Abstract
Purpose
Few data are available regarding the nephrotoxicity of immune checkpoint inhibitor (ICI) combination therapy in advanced renal cell carcinoma (RCC). This study aimed to investigate the nephrotoxicity of ICI-based combination therapy versus standard of care sunitinib in patients with advanced RCC.
Methods
We searched Embase/PubMed/Cochrane Library for relevant randomized controlled trials (RCTs). Treatment-related nephrotoxicities including increase of creatinine and proteinuria were analyzed by Review Manager 5.4 software.
Results
Seven RCTs involving 5239 patients were included. The analysis showed that ICI combination therapy had similar risks of any grade (RR = 1.03, 95% CI: 0.77–1.37, P = 0.87) and grade 3–5 (RR = 1.48, 95% CI: 0.19–11.66, P = 0.71) increased creatinine compared with sunitinib monotherapy. However, ICI combination therapy was associated with significantly higher risks of any grade (RR = 2.33, 95% CI: 1.54–3.51, P < 0.0001) and grade 3–5 proteinuria (RR = 2.25, 95% CI: 1.21–4.17, P = 0.01).
Conclusions
This meta-analysis suggests that ICI combination therapy shows more nephrotoxicity of proteinuria than sunitinib in advanced RCC, which deserves a high attention in the clinic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kidney cancer is among the 10 most common cancers in both men and women, representing 3.7% of all new cancer cases. RCC is the most common form of kidney cancer and is responsible for up to 85% of cases [1]. The treatment landscape of advanced RCC has undergone a revolution. For more than 10 years, single-agent therapy with antiangiogenic tyrosine kinase inhibitors (TKIs), including sunitinib or pazopanib, was an unchallenged gold-standard first-line approach for advanced RCC. However, with the advent of immunotherapies, immune checkpoint inhibitor (ICI) alone, double-agent ICI, or ICI combined with TKIs, has shown superior efficacy compared with TKI monotherapies [2]. A meta-analysis based on a comprehensive evaluation of current clinical trials (KEYNOTE-426, JAVELIN Renal101, CheckMate 9ER, CLEAR, CheckMate 214, Immotion151, Immotion150) reported that ICI combination therapy resulted in significantly improved tumor response and survival benefits in the first-line treatment for advanced RCC compared with sunitinib monotherapy [3]. On the basis of pivotal phase III trials, ICI–vascular endothelial growth factor (VEGF) inhibitor combinations, including nivolumab plus cabozantinib, pembrolizumab plus axitinib, lenvatinib plus pembrolizumab, and dual checkpoint blockade with ipilimumab plus nivolumab, represent new standards of treatment for treatment-naive advanced RCC patients, and were recommended by the most updated international guidelines [4].
Despite ICI combination therapy have shown superior efficacy in patients with advanced RCC, treatment-related toxicity has also attracted increasing attention from clinicians. Both VEGF ligand-inhibiting agents (bevacizumab, aflibercept) and the small molecule antiangiogenic TKIs are associated with proteinuria, which is rarely in the nephrotic range (> 3.5 g/24 h) and even more rarely associated with the nephrotic syndrome. Hypertension frequently accompanies proteinuria [5]. Not only VEGF inhibitors, but also ICIs cause kidney-related toxicity. A previous study noted that acute kidney injury (AKI) is a rare but potentially serious complication of checkpoint inhibitor immunotherapy [6]. The estimated incidence of ICI-associated AKI is approximately 1.5 to 5 percent [7]. Since anti-VEGF inhibitors (such as axitinib, sunitinib, pazopanib, cabozantinib, lenvatinib, and bevacizumab) and ICIs (such as pembrolizumab, nivolumab, atezolizumab, avelumab, and ipilimumab) are both associated with varying degrees of nephrotoxicity, the combination of these two different types of agents may have the potential to exacerbate the nephrotoxicity.
Because of the number of different therapeutic options available for clinicians and the absence of head-to-head comparisons between these combinations, currently, treatment decision-making for advanced RCC represents a major challenge. Beyond efficacy data on survival outcomes derived from trials, a comprehensive evaluation of treatment-related nephrotoxicity should also be taken seriously, and this is even more important in palliative therapy. Several previous studies had reported the common toxicity of ICI alone, double-agent ICI, or ICI combined with TKIs in cancer patients [6, 8,9,10,11,12,13,14,15,16,17,18,19]. However, there is no report aimed at systematically evaluating the nephrotoxicity of ICI combination therapy for advanced RCC. Thus, we conducted a meta-analysis of randomized controlled trials (RCTs) to investigate the nephrotoxicity of ICI combination therapy versus standard of care sunitinib in patients with advanced RCC.
Methods
Literature search
A systematical search of literature was performed in databases including Embase, PubMed, and Cochrane Library for eligible studies from inception until August 2022. Studies were identified using search terms as follows: “immune therapy OR immunotherapy OR immune checkpoint inhibitors OR immune checkpoint blockade OR PD-1 OR PD-L1 OR nivolumab OR pembrolizumab OR cemiplimab OR dostarlimab OR atezolizumab OR avelumab OR durvalumab OR ipilimumab OR tremelimumab OR toripalimab OR sintilimab OR camrelizumab OR tislelizumab” AND “renal cell carcinoma OR renal carcinoma OR kidney cancer OR renal cancer”. To avoid missing the relevant studies, the search initially involved randomized or non-randomized trials.
Inclusion and exclusion criteria
According to the prespecified protocol, the inclusion criteria were as follows: (1) participants—patients diagnosed with advanced RCC; (2) intervention—treated with ICI combination therapy; (3) comparison—standard of care sunitinib; (4) outcomes—reporting data of treatment-related nephrotoxicity; (5) RCTs; (6) studies published in English. Exclusion criteria were as follows: (1) studies less than 10 patients in either the experimental or the control group; (2) conference abstracts without published full-text original articles, commentaries, letters, reviews, editorials, duplicate reports and unfinished studies; (3) trials which not related to the subject of our study. If multiple publications reporting on the same study, the article with the most updated was selected.
Data extraction
The clinical outcomes evaluated in this analysis were all-grade and grade 3–5 treatment-related nephrotoxicity. Two authors (J.T. and D.M.) independently extracted data concerning study details. The following information was extracted from all eligible studies: first author, publication year, trial name, age, intervention and dosage in experimental and control arms, numbers of included patients in each studies, number of patients occurring all-grade and grade 3–5 treatment-related nephrotoxicity. This work was performed according to the Preferred Reported Items for Systematic Reviews and Meta-analyses (PRISMA) statement [20]. The selection of literature and data extraction were performed independently by two authors (J.T. and D.M.). Discrepancies were adjudicated by a third reviewer (K.W.) and resolved by consensus.
Risk of bias and quality assessments
The risk of bias of RCTs and methodological quality were evaluated with the Cochrane Collaboration’s risk of bias tool [21], completed by Review Manager 5.4 software. Two authors (J.T. and D.M.) independently performed this process, and disagreements were resolved by a third investigator (K.W.).
Statistical analysis
In our analysis, the outcomes of interesting included all-grade and grade 3–5 renal adverse events (including proteinuria, increase of creatinine, and AKI in advanced RCC patients treated with ICI combination therapy). Meta-analysis was conducted using statistical software of Review Manager 5.4 software. The pooled relative risk (RR) and 95% confidence interval (CI) was used to assess incidences of all-grade and grade 3–5 renal adverse events. Subgroup analyses were performed according to ICI agent types. Heterogeneity among studies was assessed according to the I-squared (I2) test in the meta-analysis. The heterogeneity was considered as high if I2 > 50%, and then the randomized-effects model was applied; otherwise, the fixed-effects model was used. P < 0.05 would be treated as statistically significant.
Results
Search results and study characteristics
The flowchart of the selection process and detailed identification is shown in Fig. 1. We identified a total of 2097 related studies by the initial search strategy, and these were subsequently restricted to 7 following independent evaluations performed by 2 authors (J.T. and D.M.). We excluded 2090 studies that did not fulfill our criteria, such as non-RCTs, retrospective studies, case reports, review articles, meta-analyses, and phase I trials.
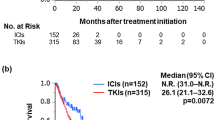
All studies included in the analysis were published between 2018 and 2022, and were judged to have a low risk of bias in separate assessments performed by two authors (J.T. and D.M.). A total of 5239 patients (ICI combinations: 3634; sunitinib monotherapy: 2605) were included in the analysis [22,23,24,25,26,27,28]. All patients were diagnosed with RCC by pathology and were adults with advanced disease, and received ICI combination therapy in the experimental group and sunitinib in the control group.
All the seven studies included in the analysis were randomized, multicenter, open-label RCTs, comparing ICI combination therapy (pembrolizumab plus lenvatinib [25], nivolumab plus cabozantinib [23], pembrolizumab plus axitinib [28], atezolizumab plus bevacizumab [24, 26], avelumab plus axitinib [22], and nivolumab plus ipilimumab [27]) with sunitinib monotherapy. Among the seven trials, six were phase 3 studies and another was phase 2 study. The main characteristics and details about the included studies are shown in Table 1.
Treatment-related nephrotoxicity
Data of proteinuria were reported in six trails, and data of creatinine increase was reported in two trails. Since the data of AKI were reported in only one trail [27], no meta-analysis was available concerning this outcome. The forest plot of these outcomes is shown in Figs. 2, 34 and 5.
The overall analysis indicated that the risks of all-grade and grade 3–5 increase of creatinine were similar between the ICI combination therapy and the sunitinib monotherapy groups (RR = 1.03, 95% CI: 0.77–1.37, P = 0.87 and RR = 1.48, 95% CI: 0.19–11.66, P = 0.71, respectively) (Figs. 4, 5).
In terms of proteinuria, ICI combination immunotherapy significantly increased the risks of any grade (RR = 2.33, 95% CI: 1.54–3.51, P < 0.0001) and grade 3–5 proteinuria (RR = 2.25, 95% CI: 1.21–4.17, P = 0.01) compared with sunitinib monotherapy (Figs. 2, 3). Subgroup analysis showed that either PD- L1 plus VEGF inhibitors or PD-1 plus VEGF inhibitors increased the risks of any grade (RR = 3.37, 95% CI: 1.96–5.78, P < 0.0001 and RR = 1.75, 95% CI: 1.26–2.42, P = 0.0009, respectively) (Fig. 2) and grade 3–5 proteinuria (RR = 3.92, 95% CI: 1.66–9.23, P = 0.002 and RR = 1.55, 95% CI: 0.83–2.87, P = 0.17, respectively) (Fig. 3).
Quality of the included studies
The risks of bias of the included studies in this meta-analysis are summarized in Fig. 6. The methodological quality was assessed as high in all the seven RCTs.
Discussion
For patients with renal cancer, the nephrotoxicity of treatment regimens is a very important and worthy indicator for physicians to pay attention to. This meta-analysis compared the nephrotoxicity of ICI combination therapy versus sunitinib monotherapy in treatment-naive patients with advanced RCC. To the best of our knowledge, this is the first meta-analysis to systematically evaluate the incidence and risk of treatment-related renal adverse events in advanced RCC patients receiving novel immune combinations versus targeted agent monotherapy.
In our study, three combined strategies (PD-1 plus VEGF inhibitors, PD-L1 plus VEGF inhibitors, and PD-1 plus CTLA-4 inhibitors) were available for analysis. The meta-analysis shows that combination immunotherapy was associated with higher risks of all-grade and grade 3–5 proteinuria compared with sunitinib monotherapy. These result are consistent with the previous study reported that the combination of ICI and an anti-VEGF inhibitor may specifically cause hypertension and proteinuria [18]. Notably, proteinuria is one of the most common manifestations of renal function impairment. Although patients with mild proteinuria may have no symptoms or mild symptoms, severe or persistent proteinuria often leads to the obvious symptoms, such as hypertension, edema and foamy urine for patients. Despite corticoid treatment or deferral of therapy may alleviate these symptoms, in severe cases, renal insufficiency or even renal failure may occur, leading to the interruption of treatment or deaths of patients. Ning et al. [29] reported that targeted therapy was associated with a significant increase in proteinuria level for patients with advanced RCC, and the use of ICIs further aggravated proteinuria for these patients. Moreover, proteinuria appears to be an effect common to all agents targeted at the VEGF pathway. VEGF ligand inhibitors (bevacizumab), and the small molecule antiangiogenic TKIs (sunitinib, sorafenib, pazopanib, ponatinib, axitinib, cabozantinib, vandetanib) produce asymptomatic albuminuria, occasionally causing the nephrotic syndrome [5]. Hypertension frequently accompanies proteinuria. However, the factors associated with the occurrence and severity of proteinuria are unknown. Preexisting renal disease (including higher baseline urine protein levels and hypertension) and RCC as compared to other malignant diseases may be predisposing factors [29]. ICI can also cause renal injury, and AKI is a rare but potentially serious complication of checkpoint inhibitor immunotherapy [14]. Since both anti-VEGF inhibitors and ICI have been associated with renal adverse effects, the combination of these two different classes of agents has the potential to aggravate the nephrotoxicity, especially in patients with advanced RCC. Therefore, proteinuria is of great significance for patients who received targeted or ICI therapies. Due to the wide application of targeted agents and ICI immunotherapy, the renal toxicity of proteinuria for RCC patients treated with ICI combination therapy deserves our special attention. In the current study, we found that ICI combination therapy showed more nephrotoxicity of proteinuria than sunitinib in advanced RCC. Therefore, our findings suggests that the incidence and risk of treatment-related proteinuria should always be considered when evaluating the risk–benefit balance, bearing in mind that treatment-related nephrotoxicity of anti-VEGF agents and ICIs may overlap. When using combination of VEGF inhibitors and ICIs, close monitoring and early recognition of proteinuria may protect patients from greater treatment-related harm.
Among the seven included trials, only CheckMate 214 reported that nivolumab plus ipilimumab may be associated with increased incidence of AKI when compared with single-agent sunitinib (2.19% vs 1.68%) (Table 1). Nivolumab plus ipilimumab was approved by the US Food and Drug Administration (FDA) for treatment-naive patients with intermediate- or poor-risk advanced RCC, with improved overall survival and complete response rates across all patient subgroups compared with sunitinib [30]. In 2016, Cortazar et al. analyzed renal toxicity of ICIs in different cancers involving 3695 patients, and they found that AKI occurred more frequently in patients who received combination therapy with ipilimumab and nivolumab than those who received monotherapy with ipilimumab, nivolumab, or pembrolizumab [9]. Despite more focused on efficacy, AKI caused by ICI combination therapy should also be taken seriously, because it may induce serious and fatal events if doctors do not recognize and treat it promptly.
Although nephrotoxicity due to ICI combination therapy is less common than other toxicities (such as hypertension, palmar-plantar erythrodysesthesia, diarrhea, hypothyroidism, and fatigue) [15] in advanced RCC patients, it can be serious and even fatal. Therefore, timely identification and treatment are very important.
This meta-analysis has both strengths and limitations. Among the strengths of this study, it used the most recent and accurate results of high-quality RCTs in terms of all-grade and grade 3–5 renal adverse events. In addition, the meta-analysis comprised a large number of treatment-naive advanced RCC patients (n = 5239). However, our study also has several limitations. First, the number of included studies is relatively small. In the PD-1 plus CTLA-4 inhibitors group, there was only one study included, which may lead to a limitation in the evaluation of subgroup results in this study. Second, patients in each study received different combination regimens, and the anti-tumor mechanisms of ICIs (including PD-1/PD-L1 and CTLA-4 inhibitors) are different, which add heterogeneity to our analysis. Third, only two treatment-related nephrotoxicities (increase of creatinine and proteinuria) were available for meta-analysis, and AKI was reported in only one trial. Because of limited available data, we could only analyze these two main nephrotoxicities based on the results of current research. Data on creatinine increase were included only in two trials, which might also lead to a heterogeneity in this study. However, despite not a high level of evidence, we believe that our research results are very important and instructive for the safety of clinical use of ICI combination therapy for patients with advanced RCC. Finally, besides creatinine increase and proteinuria, some other low incidence or unreported nephrotoxicities, such as renal failure, hyperuricemia and hepatorenal syndrome could not be extracted and further analyzed. However, we think that these nephrotoxicity indicators are also very important for the analysis of drug safety, which need to be pay more attention to in future studies. Therefore, more research is needed to further evaluate the nephrotoxicity of ICI combination therapy for patients with advanced RCC.
Conclusion
The current meta-analysis indicated that, compared with sunitinib monotherapy, ICI combination therapy was associated with similar risk of increase of creatinine, but with significantly higher risk of proteinuria for patients with advanced RCC. The toxicity of proteinuria should be fully considered when selecting therapeutic schedule for these patients, especially those with poor renal function reserve at the baseline.
Data availability
Date related to this article can be obtained from the corresponding author on request.
Abbreviations
- PD-1:
-
Programmed cell death protein-1
- PD-L1:
-
Programmed cell death 1 ligand 1
- ICI:
-
Immune checkpoint inhibitor
- CTLA-4:
-
Cytotoxic T lymphocyte antigen 4
- RR:
-
Relative risk
- RCT:
-
Randomized controlled trial
- AKI:
-
Acute kidney injury
- RCC:
-
Renal cell carcinoma
References
Barata PC, Rini BI (2017) Treatment of renal cell carcinoma: current status and future directions. CA Cancer J Clin 67(6):507–524. https://doi.org/10.3322/caac.21411
Procopio G, Nichetti F, Verzoni E (2020) Pembrolizumab plus axitinib: another step ahead in advanced renal cell carcinoma. Lancet Oncol 21(12):1538–1539. https://doi.org/10.1016/s1470-2045(20)30482-4
Mo DC, Huang JF, Luo PH, Huang SX, Wang HL (2021) Combination therapy with immune checkpoint inhibitors in advanced renal cell carcinoma: a meta-analysis of randomized controlled trials. Clin Immunol 232:108876. https://doi.org/10.1016/j.clim.2021.108876
Rassy E, Flippot R, Albiges L (2020) Tyrosine kinase inhibitors and immunotherapy combinations in renal cell carcinoma. Ther Adv Med Oncol 12:1758835920907504. https://doi.org/10.1177/1758835920907504
Zhang ZF, Wang T, Liu LH, Guo HQ (2014) Risks of proteinuria associated with vascular endothelial growth factor receptor tyrosine kinase inhibitors in cancer patients: a systematic review and meta-analysis. PLoS ONE 9(3):e90135. https://doi.org/10.1371/journal.pone.0090135
Tinawi M, Bastani B (2020) Nephrotoxicity of immune checkpoint inhibitors: acute kidney injury and beyond. Cureus. 12(12):e12204. https://doi.org/10.7759/cureus.12204
Cortazar FB, Kibbelaar ZA, Glezerman IG, Abudayyeh A, Mamlouk O et al (2020) Clinical features and outcomes of immune checkpoint inhibitor-associated AKI: a multicenter study. J Am Soc Nephrol 31(2):435–446. https://doi.org/10.1681/ASN.2019070676
Chen G, Qin Y, Fan QQ, Zhao B, Mei D, Li XM (2020) Renal adverse effects following the use of different immune checkpoint inhibitor regimens: a real-world pharmacoepidemiology study of post-marketing surveillance data. Cancer Med 9(18):6576–6585. https://doi.org/10.1002/cam4.3198
Cortazar FB, Marrone KA, Troxell ML, Ralto KM, Hoenig MP et al (2016) Clinicopathological features of acute kidney injury associated with immune checkpoint inhibitors. Kidney Int 90(3):638–647. https://doi.org/10.1016/j.kint.2016.04.008
Dolladille C, Akroun J, Morice PM, Dompmartin A, Ezine E et al (2021) Cardiovascular immunotoxicities associated with immune checkpoint inhibitors: a safety meta-analysis. Eur Heart J 42(48):4964–4977. https://doi.org/10.1093/eurheartj/ehab618
Jamal S, Hudson M, Fifi-Mah A, Ye C (2020) Immune-related adverse events associated with cancer immunotherapy: a review for the practicing rheumatologist. J Rheumatol 47(2):166–175. https://doi.org/10.3899/jrheum.190084
Perazella MA, Shirali AC (2018) Nephrotoxicity of cancer immunotherapies: past, present and future. J Am Soc Nephrol 29(8):2039–2052. https://doi.org/10.1681/ASN.2018050488
Postow MA, Sidlow R, Hellmann MD (2018) Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med 378(2):158–168. https://doi.org/10.1056/NEJMra1703481
Qu J, Ding Y, Jiang K, Hao J, Li Y et al (2021) Nephrotoxicity of immune checkpoint inhibitors: a disproportionality analysis from 2013 to 2020. Tohoku J Exp Med 254(4):275–282. https://doi.org/10.1620/tjem.254.275
Rizzo A, Mollica V, Santoni M, Rosellini M, Marchetti A, Massari F (2022) Risk of toxicity with immunotherapy-tyrosine kinase inhibitors for metastatic renal cell carcinoma: a meta-analysis of randomized controlled trials. Future Oncol 18(5):625–634. https://doi.org/10.2217/fon-2021-0888
Wanchoo R, Karam S, Uppal NN, Barta VS, Deray G et al (2017) Adverse renal effects of immune checkpoint inhibitors: a narrative review. Am J Nephrol 45(2):160–169. https://doi.org/10.1159/000455014
Wang DY, Salem J-E, Cohen JV, Chandra S, Menzer C et al (2018) Fatal toxic effects associated with immune checkpoint inhibitors. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2018.3923
Wu Z, Chen Q, Qu L, Li M, Wang L et al (2022) Adverse events of immune checkpoint inhibitors therapy for urologic cancer patients in clinical trials: a collaborative systematic review and meta-analysis. Eur Urol 81(4):414–425. https://doi.org/10.1016/j.eururo.2022.01.028
Zhou X, Yao Z, Bai H, Duan J, Wang Z et al (2021) Treatment-related adverse events of PD-1 and PD-L1 inhibitor-based combination therapies in clinical trials: a systematic review and meta-analysis. Lancet Oncol 22(9):1265–1274. https://doi.org/10.1016/s1470-2045(21)00333-8
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 134:178–189. https://doi.org/10.1016/j.jclinepi.2021.03.001
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Choueiri TK, Motzer RJ, Rini BI, Haanen J, Campbell MT et al (2020) Updated efficacy results from the JAVELIN Renal 101 trial: first-line avelumab plus axitinib versus sunitinib in patients with advanced renal cell carcinoma. Ann Oncol 31(8):1030–1039. https://doi.org/10.1016/j.annonc.2020.04.010
Choueiri TK, Powles T, Burotto M, Escudier B, Bourlon MT et al (2021) Nivolumab plus Cabozantinib versus Sunitinib for advanced renal-cell carcinoma. N Engl J Med 384(9):829–841. https://doi.org/10.1056/NEJMoa2026982
McDermott DF, Huseni MA, Atkins MB, Motzer RJ, Rini BI et al (2018) Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat Med 24(6):749–757. https://doi.org/10.1038/s41591-018-0053-3
Motzer R, Alekseev B, Rha SY, Porta C, Eto M et al (2021) Lenvatinib plus Pembrolizumab or Everolimus for advanced renal cell carcinoma. N Engl J Med 384(14):1289–1300. https://doi.org/10.1056/NEJMoa2035716
Motzer RJ, Powles T, Atkins MB, Escudier B, McDermott DF et al (2022) Final Overall survival and molecular analysis in IMmotion151, a phase 3 trial comparing atezolizumab plus Bevacizumab vs Sunitinib in patients with previously untreated metastatic renal cell carcinoma. JAMA Oncol 8(2):275–280. https://doi.org/10.1001/jamaoncol.2021.5981
Motzer RJ, Rini BI, McDermott DF, Arén Frontera O, Hammers HJ et al (2019) Nivolumab plus ipilimumab versus sunitinib in first-line treatment for advanced renal cell carcinoma: extended follow-up of efficacy and safety results from a randomised, controlled, phase 3 trial. Lancet Oncol 20(10):1370–1385. https://doi.org/10.1016/s1470-2045(19)30413-9
Powles T, Plimack ER, Soulières D, Waddell T, Stus V et al (2020) Pembrolizumab plus axitinib versus sunitinib monotherapy as first-line treatment of advanced renal cell carcinoma (KEYNOTE-426): extended follow-up from a randomised, open-label, phase 3 trial. Lancet Oncol 21(12):1563–1573. https://doi.org/10.1016/s1470-2045(20)30436-8
Ning K, Wu Z, Zou X, Liu H, Wu Y, Xiong L, Yu C, Guo S, Han H, Zhou F, Dong P, Zhang Z (2022) Immune checkpoint inhibitors further aggravate proteinuria in patients with metastatic renal cell carcinoma after long-term targeted therapy. Transl Androl Urol 11(3):386–396. https://doi.org/10.21037/tau-21-1015.PMID:35402197;PMCID:PMC898497
Tomita Y, Uemura H, Fujimoto H, Kanayama HO, Shinohara N et al (2011) Key predictive factors of axitinib (AG-013736)-induced proteinuria and efficacy: a phase II study in Japanese patients with cytokine-refractory metastatic renal cell Carcinoma. Eur J Cancer 47(17):2592–2602. https://doi.org/10.1016/j.ejca.2011.07.014
Motzer RJ, McDermott DF, Escudier B, Burotto M, Choueiri TK et al (2022) Conditional survival and long-term efficacy with nivolumab plus ipilimumab versus sunitinib in patients with advanced renal cell carcinoma. Cancer 128(11):2085–2097. https://doi.org/10.1002/cncr.34180
Acknowledgements
The authors would like to thank The Third Affiliated Hospital of Guangxi Medical University.
Funding
There is no funding for this study.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Study design, data collection and analysis were performed by A-jT, D-cM, KW and X-xX. The first draft of the manuscript was written by A-jT and D-cM, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tan, Aj., Mo, Dc., Wu, K. et al. Nephrotoxicity of immune checkpoint inhibitor combination therapy in patients with advanced renal cell carcinoma: a meta-analysis. World J Urol 41, 1563–1571 (2023). https://doi.org/10.1007/s00345-023-04407-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04407-x