Abstract
Background
Since the development of minimally invasive surgery (MIS), laparoscopic and robotic approaches have been widely adopted. However, little has been published detailing the learning curve of MIS, especially in infants.
Objective
To quantify the learning curve of laparoscopic (LP) and robot-assisted laparoscopic pyeloplasty (RAL-P) for treatment of uretero-pelvic junction obstruction (UPJO) in infants evidenced by number of cases, operative time, success and complications.
Patients and methods
Between 2009 and 2017, we retrospectively reviewed pyeloplasty cases for treatment of UPJO in infants at three academic institutions. The primary outcome was success. Secondary outcomes were UPJO recurrence, complications, and operative time as a surrogate of skill acquisition. Continuous variables were analyzed by t test, Welch-test, and one-way ANOVA. Non-continuous variables were analyzed by Chi-squared test or Fisher's exact test. Learning curves (LC) were studied by r-to-z transformation and CUSUM.
Results
Thirty-nine OP, 26 LP, and 39 RAL-P had mean operative times (OT) of 106, 121, and 151 min, respectively. LCs showed plateau in OT after 18 and 13 cases for LP and RAL-P, respectively. RAL-P showed a second phase of further improvements after 37 cases. At 16 months follow-up, there were similar rates of success and complications between the three groups.
Conclusions
Despite different duration of learning phases, proficiency was achieved in both LP and RAL-P as evidenced by stabilization of operative time and similar success rates and complications to OP. Before and after achievement of proficiency, LP and RAL-P can be safely learned and implemented for treatment of UPJO in infants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ureteropelvic junction (UPJ) obstruction is a common cause of pediatric hydronephrosis, and since 1949, the Anderson-Hynes open dismembered pyeloplasty (OP) has been the gold standard treatment [1]. First implemented in 1995 [2], laparoscopic pyeloplasty (LP) offers advantages including shorter hospitalization and decreased analgesic demand [3]. However, this approach demands a different set of technical skills, which can pose a steep learning curve (LC). In pediatric patients with smaller anatomic working space, laparoscopic instrument maneuverability can be difficult, especially during intracorporeal suturing [2,3,4,5].
The robotic interface has helped minimize this LC and increased the utilization of a minimally invasive approach [6]. Unlike laparoscopy, the robot is equipped with a more ergonomic platform, high-resolution three-dimensional (3D) view, tremor filtration with motion scaling, and wrist-like motion of instruments. In children, robot-assisted laparoscopic pyeloplasty (RAL-P) seemed to ease the execution of a minimally invasive approach while delivering similar outcomes [7,8,9,10,11,12,13,14,15]. However, data in infants is limited, especially in comparison of clinical outcomes between the three modalities. In this study, we aimed to quantify the learning curve of LP and RAL-P in infants with proficiency determined by operative time and comparison of clinical outcomes and complications of LP and RAL-P to OP.
Patients and methods
From a prospectively maintained database, we reviewed medical records of infants, defined as less than 12 months old, undergoing primary pyeloplasty for UPJ obstruction at three major academic institutions. Indications for surgical management of UPJO by pyeloplasty were similar across research sites and include increasing grade of hydronephrosis demonstrated by ultrasound and worsening renal function demonstrated by nuclear medicine studies [13]. Prior to approach selection, patients and families were counseled on the limitations and potential benefits of available pyeloplasty approaches for the treatment of UPJ obstruction. At each institution, one surgeon performed all pyeloplasty cases using one modality to assess proficiency of one surgeon using one technique. For instance, all OPs were performed by Surgeon A, all LPs were performed by Surgeon B, and all RAL-P were performed by surgeon C to assess individual attending-level surgeon learning curves. All attending surgeons had prior OP experience and Surgeon C had prior LP experience.
Inclusion criteria included patient age less than 12-months at primary diagnosis of UPJ obstruction, evaluated by ultrasound and confirmed by renal scan. Renal scan parameters were determined by the institution's pediatric radiologists. Patients with congenital malformations including vesicoureteral junction obstruction or solitary kidney, were excluded. Key variables collected include length of stay (LOS), peri-operative opioid administration, success rates, Clavien–Dindo Grade (CDG) III complications, and operative time (OT), from incision to close and including stent placement in all cases and docking time for RAL-P. Pre-operatively, retrograde pyelograms were not performed. Postoperatively, no drains were used but all patients received a JJ stent, except those under 2 months old, who received a nephroureteric stent. Success was defined as clinical resolution of hydronephrosis, with stable or improved radiographic resolution on ultrasound (US) and without need for additional interventions.
Continuous data were reported as mean with standard deviation (SD) or median with interquartile interval (IQI), defined as 25th (1st quartile) to 75th (3rd quartile) percentile intervals. F tests and D’Agostino-Pearson tests assessed variance and probability distribution, respectively. When normal distribution was rejected, logarithmic transformation precluded paired sample t test (for constant variance of error) or Welch-test (for non-constant variance of error), were used to compare means of two independent samples. One-way ANOVA compared means of three or more samples. Chi-squared test was used to study proportions with more than ten events; otherwise, Fisher's exact test was preferred [16, 17]. Fisher “r-to-z” transformation assessed the difference between Pearson’s correlation coefficients of variance between two independent samples. A CUSUM analysis was performed to identify inflection points along the learning curves for LP and RAL-P, using operative time as a surrogate of skill acquisition. CUSUM scores are the cumulative sums of the deviations of each sample value from the target value and thus detect significant changes in the mean operative time. The target value was set at the initial operative time for all three approaches. CUSUM scores are displayed on the y-axis, with consecutive cases on the x-axis. A P value < 0.05 was considered significant. The statistical software was JMP®, version 14 (SAS Institute Inc., Cary, NC, 1989–2019).
Results
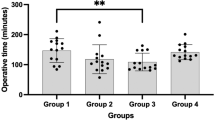
Between December 2009 and 2017, 104 infants underwent primary pyeloplasty, of which there were 39 OP, 26 LP and 39 RAL-P cases. Across all cases, operative time for the OP modality was significantly shorter compared to both minimally invasive approaches (OP = 106, LP = 121, RAL-P = 151; P < 0.001). The time to reach proficiency for LP technique was slightly longer than that of RAL-P, evidenced by a longer slope of the learning curve (LP slope = − 0.54, RAL-P slope = − 0.84; P = 0.019) (Fig. 1, Table 1). In the LP cohort, the CUSUM chart identified an inflection point at the 18th case, indicating a shift in the mean operating time and skill level of the operating surgeon (Fig. 2). RAL-P showed a multiphasic CUSUM chart with a steep learning curve during the first 13 cases, followed by stability in operating times, indicating standard proficiency level (Fig. 3). The second inflection point along the RAL-P learning curve occurred at the 37th case and represented a consolidation of learning and further improvement in operating times. No conversion to open occurred in the LP or RAL-P cohorts.
Multiphasic CUSUM analysis of OT for RAL-P with two inflection points showing a steep learning phase with the first 13 cases, followed by a consistently stable fluctuation of values around the median OT corresponding to a proficiency level. A second inflection point at the 37th case stood for the consolidation of learning plateau and the beginning of a third phase where additional OT improvements can be achieved
To further analyze proficiency evidenced by clinical outcomes we compared opioid administration, complications, and success rates between the three modalities. Of note, at baseline, the median age at surgery was significantly younger for LP and RAL-P compared to OP patients (3 vs. 4 vs. 7 months, P = 0.007). The proportion of patients who received intra- and post-operative opioids was similar between OP and RAL-P (44 vs 33%, P = 0.351) but, OP cases required a significantly higher average dose per patient compared to RAL-P cases (0.8 vs 0.5 mg/kg, P = 0.033). Five patients (13%) in the OP cohort required extended opioid administration after hospital discharge. In the LP group, no patients required post-operative opioid administration. For the LP patient cohort, details regarding intra-operative analgesia were not available within the electronic health record. No differences between all three modalities were found in the rates of CDG-III complications (OP = 7.7%, LP = 11.5%, RAL-P = 7.7%; P = 0.636). Patients with CDG-III complications included urine leak after OP, retained ureteral Double-J stent after LP, and incisional hernia after RAL-P. Recurrence of UPJ obstruction occurred in 2 OP, 2 LP, and 1 RAL-P patients, all of which required re-intervention. At a median follow-up of 16 months (min 7, max 26), success rates were similar for all three modalities (OP = 95%, LP = 92%, RAL-P = 97%; P = 0.60) (Table 1).
Discussion
Since the initial description of the technique by Anderson and Hynes in 1949, OP has been considered the gold standard for the surgical management of UPJ obstruction [1]. Since 1995, when the first LP in a child was reported [2], MIS has gradually been adopted by pediatric urologists [6]. After achievement of proficiency, studies evaluating LP in children showed equivalent success and complication rates to OP [18,19,20]. Between 2003 and 2009, there was a 12% increase RAL-P with an associated decrease in laparoscopic procedures [9], indicating a growing cohort of urologists embarking on the MIS learning curves. However, little literature exists examining the duration of learning curve for MIS and subsequent effects on success and complication rates, especially of LP and RAL-P in infants [5]. Studies that do exist have been limited by small number of MIS infant cases and to our knowledge, no study thus far has analyzed success rates and complication rates before and after LP and RAL-P proficiency relative to OP.
Thus far, it appears that most pediatric urologists have established that the use of MIS in children is beneficial but that MIS in infants still poses technical limitations. Our results show that the benefits of MIS are not limited to older children and that the learning curve of MIS utilization in infants is surmountable and safe. Within our cohort, the median age of patients undergoing LP and RAL-P was younger than that of the OP group (LP = 3, RAL-P = 4, OP = 7 months; P = 0.485). In addition, there were no differences in success rates (LP = 95%, RAL-P = 92%, OP = 97%, P = 0.634) or CDG-III complication rates (LP = 7.7%, RAL-P = 11.5%, OP = 7.7%, P = 0.833) between the three approaches. The success rates and complications rates presented capture both the learning curve and proficiency stage in LP and RAL-P, suggesting that even during the surgeon’s learning curve, neither success nor safety is compromised and is comparable to that of OP. The summation of these data describes the efficacy and safety of MIS approaches infants.
In conjunction with similar success rates and similar complication rates, the nature of the complications across all three groups further assures the safety of MIS in infants. The nature of the complications within the three groups was similar with recurrent UPJO occurring in 2 (5%) OP and 2 (8%) LP patients, all of which underwent re-intervention and 1 (3%) RAL-P patient, who underwent ureterolysis due to extrinsic compression of the uretero-pelvic anastomosis. Other than UPJO recurrence, other CDG-III complications included urine leak after OP, retained ureteral Double-J stent after LP, and 2 incisional hernias after RAL-P. Despite differences in types of complications, there is no difference in Clavien–Dindo grades across all three groups and no complications demonstrated a direct relationship to procedure approach or limitations inherent to the infant physiology or anatomical working space, suggesting that all three procedure types would be suitable in infants.
Thus far, our data have demonstrated no significant difference in success rates or complications rates across all three procedure approaches in infants both during and after surgeon MIS learning curve. However, the nature of the learning curve and its relationship to case complexity remains to be discussed. Across the study period, from 2009 to 2017, including before and after establishing LP proficiency, the average operative time (OT) for LP was 121 min with a range of 75 to 189 min (Fig. 1). The average OT for RAL-P was 151 min with a range of 86 to 176 min. The average OT for OP was 106 min with a range of 62 to 151 min. The gap in surgical times between RAL-P and OP was significant (P < 0.001) while operative times between LP and OP were comparable (P = 0.077). Longer operative times in RAL-P are likely attributable to the time required for docking the robot. Time improvements in robotic setup directly correlate with experience and proficiency levels of both surgeon and surgical team [21, 22]. The variable “operative time” can act as a surrogate for surgeon skill acquisition but also, case complexity. The range of operative times in MIS in junction with high success rates, comparable to OP, suggest that MIS can safely be implemented in cases with varying complexity. However, it must also be noted the potential confounding variable of case complexity on the variable “operative time.”
Without a tool for quantification of case complexity, we relied on the CUSUM analysis to limit confounding and detect significant changes in the cumulative mean over time to detect learning curve plateau. Based on our study, skill acquisition in laparoscopy (LP) and robotic surgery (RAL-P) is different in the rate of progression towards proficiency. The CUSUM analysis estimated that at least 18 cases were required to achieve proficiency in LP, represented by the OT inflection point (Fig. 2). In RAL-P, proficiency was achieved after 13 cases, with further improvement after 37 cases (Fig. 3). The decreased number of cases required to reach proficiency in RAL-P versus LP may be influenced by the surgeon-robot interface. The robotic interface is cognizant of ergonomics and equipped with high-resolution three-dimensional (3D) view, tremor filtration with motion scaling, and wrist-like motion of instruments. This technology may have had a hand in the relatively shorter path to proficiency in RAL-P compared to LP.
While the CUSUM analysis can help us to understand the operative learning curve and surgeon skill acquisition, it does not explicitly account for changes in surgeon confidence. One example of this may be evident in length of stay. The length of stay for LP and RAL-P patients was significantly longer than that of OP patients (LP = 2.0 ± 0.9, RAL-P = 1.5 ± 0.7, OP = 1.0 ± 0.3, P < 0.001). Increased length of stay (LOS) among MIS cases relative to OP cases is interesting within the context that success rates and complication rates are not significantly different. However, these data were not known at the time of the surgery. Therefore, we attribute longer LOS to the surgeon’s increased vigilance during the MIS learning curve with growing confidence over time.
Intra- and post-operative opioid use in milligrams per kilogram and milligrams per patient were significantly lower for RAL-P compared to OP (RAL-P = 0.08 mg/kg, OP = 0.10 mg/kg; P = 0.036; RAL-P = 0.5 mg/patient, OP = 0.8 mg/patient, P = 0.033). Five OP patients required opioids after discharge. Notably, the proportion of patients who received opioids did not significantly vary between RAL-P and OP cases (RAL-P = 33%, OP = 44%, P = 0.351). While data on intra-operative LP analgesia was not available, these patients did not require opioids during post-operative recovery. Based on these data, it is tempting to speculate that lower analgesia requirements resulted from the minimally invasive nature of LP and RAL-P. However, because the patients were infants, pain assessment may be subject to interpretive bias [23, 24]. Therefore, differences in pain management were likely primarily attributable to different institutional protocols, rather than actual analgesia requirements. Furthermore, hospital policy on opioid prescribing may vary between the study’s United States and international sites, as there may be different perspectives on the opioid epidemic and prescribing.
Limitations include those inherent to the retrospective nature of this study. We have identified four potential confounding biases regarding operative time (OT) and learning curve (LC) that warrant discussion. The first of which is that all three institutions were academic centers, in which trainees regularly take part in surgical procedures, with different degrees of involvement based on training experience. The involvement of said learners may influence individual operative times but when operative times are examined in conglomerate, the consistent involvement of trainees in all procedure approaches and in all three research sites may not influence the results seen. The second limitation is that the learning curves shown in this article may not be inclusive of urologists in early stages of training, as the attending surgeons performing the two minimally invasive approaches had already reached a proficiency level with older patients, prior to embarking on the MIS learning curve in infants. Furthermore, patient outcomes and learning curves may be subject to the practice and setting of each individual surgeon and thus, may not be identically replicated. Limited operating surgeon sample size prohibits conclusions regarding superiority of different approaches. Thirdly, for RAL-P, improvement in operative times was influenced by not only the skills of the surgeon, but also by the surgical team docking the robot. Lastly, as previously mentioned, operative times do not account for case complexity or other variables that would influence operative time.
Conclusions
In an era of technological advancements where reducing the invasiveness of surgical procedures is becoming increasingly relevant, the most suitable approach should not only be safe and effective, but also easy to learn. Despite different initial skill sets among three surgeons, the implementation of LP and RAL-P for the treatment of UPJO in infants yielded achievement of proficiency with similar success rates and complication rates to open pyeloplasty. Therefore, we believe that the learning curves for laparoscopic and robotic pyeloplasty for the treatment of UPJO in infants are safely surmountable when performed by attending-level surgeons with prior open pyeloplasty experience. This multi-institutional analysis prompts consideration of LP and RAL-P in infants, as the benefits of MIS may not be limited to older children, as previously assumed. Notably, the results presented are from early studies and we anticipate to better understand as additional experience and future proficiency is achieved. Higher quality evidence in the form of prospective observational studies and clinical trials, as well as cost-effectiveness analyses are needed to validate our conclusions.
References
Anderson JC, Hynes W (1949) Retrocaval ureter: a case diagnosed pre-operatively and treated successfully by a plastic operation. Br J Urol 21(3):209–214. https://doi.org/10.1111/j.1464-410X.1949.tb10773.x
Peters CA, Schlussel RN, Retik AB (1995) Pediatric laparoscopic dismembered pyeloplasty. J Urol 153(6):1962–1965
O’Brien ST, Shukla AR (2012) Transition from open to robotic-assisted pediatric pyeloplasty: a feasibility and outcome study. J Pediatr Urol 8(3):276–281. https://doi.org/10.1016/j.jpurol.2011.04.005
Valla JS, Breaud J, Griffin SJ et al (2009) Retroperitoneoscopic vs open dismembered pyeloplasty for ureteropelvic junction obstruction in children. J Pediatr Urol 5(5):368–373. https://doi.org/10.1016/j.jpurol.2009.02.202
Kutikov A, Resnick M, Casale P (2006) Laparoscopic pyeloplasty in the infant younger than 6 months—is it technically possible? J Urol 175(4):1477–1479. https://doi.org/10.1016/S0022-5347(05)00673-7
Monn MF, Bahler CD, Schneider EB et al (2013) Trends in robot-assisted laparoscopic pyeloplasty in pediatric patients. Urology 81(6):1336–1341. https://doi.org/10.1016/j.urology.2013.01.025
Autorino R, Eden C, El-Ghoneimi A et al (2014) Robot-assisted and laparoscopic repair of ureteropelvic junction obstruction: a systematic review and meta-analysis. Eur Urol 65(2):430–452. https://doi.org/10.1016/j.eururo.2013.06.053
Olsen LH, Jorgensen TM (2004) Computer assisted pyeloplasty in children: the retroperitoneal approach. J Urol 171(6 Pt 2):2629–2631. https://doi.org/10.1097/01.ju.0000110655.38368.56
Liu DB, Ellimoottil C, Flum AS, Casey JT, Gong EM (2014) Contemporary national comparison of open, laparoscopic, and robotic-assisted laparoscopic pediatric pyeloplasty. J Pediatr Urol 10(4):610–615. https://doi.org/10.1016/j.jpurol.2014.06.010
Sukumar S, Djahangirian O, Sood A et al (2014) Minimally invasive vs open pyeloplasty in children: the differential effect of procedure volume on operative outcomes. Urology 84(1):180–184. https://doi.org/10.1016/j.urology.2014.02.002
Kutikov A, Nguyen M, Guzzo T, Canter D, Casale P (2006) Robot assisted pyeloplasty in the infant-lessons learned. J Urol 176(5):2237–2239. https://doi.org/10.1016/j.juro.2006.07.059 (discussion 2239–2240)
Bansal D, Cost NG, DeFoor WR et al (2014) Infant robotic pyeloplasty: comparison with an open cohort. J Pediatr Urol 10(2):380–385. https://doi.org/10.1016/j.jpurol.2013.10.016
Dangle PP, Kearns J, Anderson B, Gundeti MS (2013) Outcomes of infants undergoing robot-assisted laparoscopic pyeloplasty compared to open repair. J Urol 190(6):2221–2226. https://doi.org/10.1016/j.juro.2013.07.063
Neheman A, Kord E, Zisman A, Darawsha AE, Noh PH (2018) Comparison of robotic pyeloplasty and standard laparoscopic pyeloplasty in infants: a bi-institutional study. J Laparoendosc Adv Surg Tech A 28(4):467–470. https://doi.org/10.1089/lap.2017.0262
Ebert KM, Nicassio L, Alpert SA, Ching CB, Dajusta DG, Fuchs ME, McLeod DJ, Jayanthi VR (2020) Surgical outcomes are equivalent after pure laparoscopic and robotic-assisted pyeloplasty for ureteropelvic junction obstruction. J Pediatr Urol 16(6):845.e1-845.e6. https://doi.org/10.1016/j.jpurol.2020.09.018
Campbell I (2007) Chi-squared and Fisher-Irwin tests of two-by-two tables with small sample recommendations. Stat Med 26(19):3661–3675. https://doi.org/10.1002/sim.2832
Richardson JTE (2011) The analysis of 2 × 2 contingency tables—yet again. Stat Med 30(8):890–890. https://doi.org/10.1002/sim.4116
Penn HA, Gatti JM, Hoestje SM, DeMarco RT, Snyder CL, Murphy JP (2010) Laparoscopic versus open pyeloplasty in children: preliminary report of a prospective randomized trial. J Urol 184(2):690–695. https://doi.org/10.1016/j.juro.2010.03.062
Mei H, Pu J, Yang C, Zhang H, Zheng L, Tong Q (2011) Laparoscopic versus open pyeloplasty for ureteropelvic junction obstruction in children: a systematic review and meta-analysis. J Endourol 25(5):727–736. https://doi.org/10.1089/end.2010.0544
Turner RM, Fox JA, Tomaszewski JJ, Schneck FX, Docimo SG, Ost MC (2013) Laparoscopic pyeloplasty for ureteropelvic junction obstruction in infants. J Urol 189(4):1503–1507. https://doi.org/10.1016/j.juro.2012.10.067
O’Kelly F, Farhat WA, Koyle MA (2019) Cost, training and simulation models for robotic-assisted surgery in pediatric urology. World J Urol. https://doi.org/10.1007/s00345-019-02822-7
Andolfi C, Umanskiy K (2017) Mastering robotic surgery: where does the learning curve lead us? J Laparoendosc Adv Surg Tech A 27(5):470–474. https://doi.org/10.1089/lap.2016.0641
Witt N, Coynor S, Edwards C, Bradshaw H (2016) A guide to pain assessment and management in the neonate. Curr Emerg Hosp Med Rep 4(1):1–10. https://doi.org/10.1007/s40138-016-0089-y
Cignacco E, Schenk K, Stevens B et al (2017) Individual contextual factors in the validation of the Bernese pain scale for neonates: protocol for a prospective observational study. BMC Pediatr 17(1):171. https://doi.org/10.1186/s12887-017-0914-9
Author information
Authors and Affiliations
Contributions
CA: Project development, Data management, Data analysis, Manuscript writing/editing; AL: Data collection, Manuscript writing, Manuscript editing; JA: Manuscript writing, Manuscript editing; XR: Data collection, Data management, Manuscript editing; JPW: Data management, Data analysis, Manuscript editing; NSB: Data collection, Manuscript editing; FR: Data management, Manuscript editing; PJL: Project development, Manuscript editing; DTW: Project development, Manuscript editing; MSG: Project development, Manuscript editing. All authors agree to every aspect of the work.
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Research involving human participants
Research study protocol and data use agreements were approved by each institutional review board (IRB) before de-identified and encrypted data were collected, shared, and analyzed. Informed consent for data collection was obtained according to each IRB. No identifiable data or protected health information (PHI) were shared or disclosed, therefore, no informed consent for publication was necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Andolfi, C., Lombardo, A.M., Aizen, J. et al. Laparoscopic and robotic pyeloplasty as minimally invasive alternatives to the open approach for the treatment of uretero-pelvic junction obstruction in infants: a multi-institutional comparison of outcomes and learning curves. World J Urol 40, 1049–1056 (2022). https://doi.org/10.1007/s00345-022-03929-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-03929-0