Abstract
Purpose
To evaluate the efficacy and safety of thulium-fiber laser (TFL) in laser lithotripsy during percutaneous nephrolithotomy (PCNL).
Methods
Patients with stones < 30 mm were prospectively recruited to undergo PCNL using TFL “FiberLase” (NTO IRE-Polus, Russia). Stone size, stone density, operative time, and “laser on” time (LOT) were recorded. Study included only cases managed with fragmentation. Stone-free rate and residual fragments were determined on postoperative computer tomography. Complications were classified using the Clavien–Dindo grade. Stone retropulsion and endoscopic visibility were assessed based on surgeons’ feedback using a questionnaire.
Results
A total of 120 patients were included in the study with a mean age of 52 (± 1.8) years; of these 77 (56%) were males. Mean stone size was 12.5 (± 8.8) mm with a mean density of 1019 (± 375) HU. Mean operative time was 23.4 (± 17.9) min and mean LOT was 5.0 (± 5.7) min. Most used settings were of 0.8 J/25–30 W/31–38 Hz (fragmentation). The mean total energy for stone ablation was 3.6 (± 4.3) kJ. Overall stone-free rate was 85%. The overall complication rate was 17%. Surgeons reported stone retropulsion that interfered with surgery in 2 (1.7%) cases insignificant retropulsion was noted in 16 (10.8%) cases. Poor visualization was reported in three (2.5%) cases and minor difficulties with visibility in four (3.3%) cases.
Conclusions
TFL is a safe and effective modality for lithotripsy during PCNL and results in minimal retropulsion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Currently, Holmium:YAG (Ho:YAG) laser lithotripsy is the primary laser ablation method used in the treatment of urinary calculi [1]. The Ho:YAG laser is highly efficient in stone fragmentation and dusting, and recent refinements of the Ho:YAG laser such as the Moses technology have further improved its efficacy in laboratory studies [2, 3]. Despite the well-established clinical utility of the Ho:YAG laser, next-generation, fiber-based laser systems may prove to be even safer and more efficacious. Specifically, the thulium fiber laser (TFL) offers a higher laser energy absorption in water and has been reported to cause minimal stone retropulsion in vitro [4].
The potential clinical advantages of TFL compared to the Ho:YAG laser arise from differences in laser beam generation. In solid-state lasers (Ho:YAG, LBO:YAG, KTP:YAG), a flashlamp pump emits energy through YAG crystals doped with various ions (e.g., holmium, lithium triborate or potassium titanyl phosphate), which leads to amplification and emission of the laser beam. With this method of laser generation, less than 10% of the energy is focused into the laser itself, with most energy lost in the form of heat [5]. Thus, to avoid over-heating, Ho:YAG laser devices are equipped with large water-cooling systems, contributing to their size and higher energy consumption. In contrast, TFL utilizes 30 m of thulium-doped silica fiber, which is pumped with diode lamps. This mechanism of laser production is highly efficient, and the minimal excess heat produced by TFL can be managed by a simple fan-cooling system [6].
TFL has already been shown to be an effective modality in benign prostatic hyperplasia (BPH) surgery [7,8,9], and in vitro studies have indicated great potential for TFL in laser lithotripsy for urinary stone disease [10, 11]. The objective of this study was to evaluate the efficacy and safety of TFL in the setting of PCNL. To the best of our knowledge, this is the first clinical study evaluating TFL in urinary stone disease.
Materials and methods
Patient selection and study design
After obtaining an Institutional Review Board approval for the study, we performed a prospective study to assess the safety, efficacy and retropulsion effects of TFL during PCNL. Current trial was a proof-of-concept work, therefore, no comparison group were formed. Consecutive patients (≥ 18 years) with urinary calculi were prospectively recruited for treatment with PCNL using TFL “FiberLase” (NTO IRE-Polus, Russia) between August 2017 and January 2019. For all surgeries, we used same laser machine with no changes in technical settings. Patients with a stone diameter of up to 30 mm were included, while patients on anticoagulant therapy or patients undergoing secondary simultaneous surgical intervention (e.g., for BPH, upper tract carcinoma, urethral and ureteral stricture) were excluded. Patients who refused to participate were excluded from the study and were treated with other surgical modalities (ESWL, Ho:YAG or other lithotripters). Prior to their PCNL procedure, all patients underwent contrast-enhanced computed tomography (CT) of the urinary tract for assessment of renal anatomy, and stone characteristics such as size, location, number of calyes involved and density (hounsfield units, HU). All imaging was assessed by one experienced radiologist.
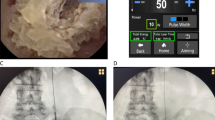
Laser settings and surgical technique
During PCNL, TFL settings were 6–40 W, 7–300 Hz, and 0.1–4.0 J. 200 mcm laser fibers were used for all cases. These settings were considered safe for surgery based on preliminary in vitro studies [12]. The operating surgeon chose the specific pulse energy regimen intraoperatively. The mode of lithotripsy was fragmentation in all cases. All PCNL procedures were performed using a 12 Fr nephroscope with MIP set (16.5–17.5 Fr) (Richard Wolf Gmbh, Germany). All procedures were performed by one of four attending surgeons, and all surgeries were completed with patients in prone position under general anesthesia. All the surgeons were highly experienced in Ho:YAG lithotripsy and perform at least 20 cases with TFL prior beginning of the study. Irrigation was passive (falling water) in all cases. A Foley catheter (16–20 Fr) was placed in all patients after surgery. The nephrostomy tube (16 Fr) was removed 2–4 days after the operation.
Outcome measures
Operative time was measured as the time from nephroscope insertion to nephroscope removal. “Laser on” time (LOT), which was automatically recorded by the laser system, was the total time that the laser was in use.
Retropulsion: Surgeon questionnaires with three-point Likert scales were used to assess stone retropulsion (0 = no retropulsion, 1 = retropulsion which does not affect stone ablation, 2 = retropulsion that interferes with stone ablation) as well as intraoperative visibility (0 = clear visibility, 1 = decrease of visibility, which does not affect procedure, 2 = poor visibility that interferes with the procedure). To exclude potential biases, inter-rater variability was assessed.
Residual stone assessment: Postoperative stone-free status was assessed in all patients on CT imaging completed within 3 months after surgery. Complications were recorded using the PCNL adaptation of the Clavien classification system [13].
Statistical analysis
Primary outcome variables included operative time, stone retropulsion, and stone-free rate. Secondary outcome variables included LOT, intraoperative visibility, and complication rate. Patient data were expressed as mean ± standard deviation (SD). Categorical variables were compared using the Pearson’s Chi-square test. For comparison of the means, analysis of variance (ANOVA) was used. Confidence intervals of the means were calculated on the basis of Student’s criterion with p = 0.05. After ANOVA, post hoc tests were used for comparisons between groups. Kruskal–Wallis test was performed for non-normally disturbed variables. For correlations assessment, Pearson’s coefficient was used. All tests were two sided, and a p value of 0.05 was considered the threshold for statistical significance. Statistical analysis was completed using SPSS Statistics 23.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 120 patients were included in this study with a mean age of 52 ± 1.8 years. Mean stone density and stone diameter were 1019 ± 375 HU and 12.5 ± 8.8 mm, respectively (Table 1). Mean follow-up time was 3 months. Most frequently used settings were of 0.8 J/25–30 W/31–38 Hz. Fragmentation settings were established during previous preclinical work and short proof-of-concept series of cases [14].
Mean operative time (without puncture time) for the entire cohort was 23.4 ± 17.9 min and LOT was 5.0 ± 5.7 min. Mean total energy for stone ablation was 3.6 ± 4.3 kJ. There was no correlation between stone density and mean LOT (Pearson correlation − 0.043, p = 0.723) (Table 2). There was a weak correlation between stone diameter and laser on time (Pearson correlation: + 0.394 (p = 0.001).
Retropulsion and visibility outcomes
Surgeons reported stone retropulsion that interfered with surgery (retropulsion score = 2) in 2 (1.7%) cases, which prolonged the operation by approximately 30 min; in these cases, the stone density was 1400 and 1072 HU, and stone diameter was 9 and 6 mm. Insignificant retropulsion (retropulsion score = 1) was noted in 13 (10.8%) cases, and in all other cases, there was no retropulsion (retropulsion score = 0) (Table 3). In retropulsion patients, we found an increased laser on time, especially in the group with extensive retropulsion (comparing both to groups of minimal and no retropulsion, p < 0.001). Surgeons reported poor visibility that interfered with the surgery (visibility score = 2) in 3 (2.5%) cases and minor difficulties with visibility in 4 (3.3%) cases (visibility score = 1); endoscopic visibility was clear (visibility score = 0) in all other cases (Table 3). We did not observe any differences in intraoperative parameters in patients with low or poor visibility or did we find an increase of intra- or postoperative complications.
Most postoperative complications were Clavien grade I–II, and none were determined to be related to the laser lithotripsy (Table 4). At 3-month follow-up, contrast-enhanced CT imaging revealed no strictures or stenosis of the upper urinary tract in any patient.
The stone-free rate at 3 months was 85% (116 patients). Residual stones’ size was < 3 mm in 10 (7%) patients, and 4 mm in the other 11 (8%) patients.
Discussion
Lasers utilizing thulium as part of the laser medium have been in use for more than a decade. For example, the Tm:YAG laser is an established tool for tissue cutting and has proven efficacy in the treatment of BPH and bladder tumor resection [7]. Unlike the Tm:YAG, which uses a solid-state crystal, TFL is a fiber laser-based technology, and has only recently appeared in clinical practice [15]. The main advantages of TFL are its significantly increased absorption in water (twice that of Tm:YAG and 4.5 times that of Ho:YAG) [10] and improved bubble formation dynamics, which is attributed to the lower peak power of TFL. In vitro studies of TFL have demonstrated better stone ablation rates compared to the Ho:YAG laser, with a dusting rate four times that of the Ho:YAG (due to a higher penetration rate) and a 1.5–2 times higher fragmentation rate due to decreased retropulsion [4, 15]. Other in vitro assessments have shown that TFL is comparable or even superior to Ho:YAG in regards to stone ablation [11]. It was found that, for uric acid and calcium oxalate monohydrate stones, TFL exhibited 2–4 times higher ablation rates than Ho:YAG [10, 16]. Similarly, Fried recently reported a higher stone ablation rate and reduced retropulsion with TFL compared to Ho:YAG [10]. In a review of the available data, Kronenberg et al. indicated that TFL may eventually rival the Ho:YAG in the treatment of urinary stone disease, but this has yet to be substantiated with clinical data [17].
The goal of this study was to evaluate the clinical efficacy and safety of using TFL as a laser lithotripter during PCNL. All the patients in our cohort were successfully treated with TFL, with a mean LOT of 6.5 min. Despite stone densities of up to 2100 HU, we did not observe a significant correlation between stone density and LOT or operative time. Our current findings suggest that TFL is equally efficient in ablating stones regardless of density. Previously, Andreeva et al. confirmed this finding in preclinical study, moreover, TFL was twice better for stone fragmentation and dusting than Ho:YAG [11, 14].
Stone retropulsion during lithotripsy frequently interferes with the efficiency and efficacy of the procedure. Standard Ho:YAG lasers are associated with high retropulsion rates. This problem has been addressed by introduction of the Moses technology, which is based on the Moses effect, present first described as early as the 1980s [10, 18]. A short, low-energy pulse creates a vapor bubble, which “parts the water,” allowing the subsequent longer, higher energy pulse to more efficiently deliver ablative energy to the stone surface. In an in vitro model, Winship et al. demonstrated that Moses technology is superior to standard Ho:YAG short- and long-pulse settings in stone ablation when the laser fiber is held 1 mm from the stone [19]. In the first clinical study using Moses technology, Elhilali et al. reported a better ablation rate and a significantly better safety profile compared to standard Ho:YAG lithotripsy [20]. In contrast to Ho:YAG, TFL should theoretically decrease retropulsion using a smaller laser fiber and operating at lower pulse energies, higher pulse rates, and longer pulse durations. Indeed, Blackmon et al. demonstrated in vitro that retropulsion increases linearly with pulse energy during Ho:YAG lithotripsy; even at pulse energies that are lower than that used clinically (i.e., 175 mJ at 10 Hz with a 270 µm fiber), the Ho:YAG laser resulted in retropulsion of > 2 mm [16]. Alternatively, TFL resulted in minimal (< 2 mm) retropulsion at pulse rates less than 150 Hz, but then drastically increased at higher rates. Taken together, the authors stated that settings designed to minimize retropulsion would result in an ablation rate of 100 µg/s for the Ho:YAG compared to 140 µg/s for TFL.
In the current study, retropulsion that interfered with the progress of the PCNL was reported in 2 (1.4%) cases, while insignificant retropulsion that did not hinder the case was reported in 16 (11.7%) cases; no retropulsion was reported in the remaining 119 (87%) cases. These data indicate that in vitro findings of less retropulsion with TFL may translate clinically, although clinical head-to-head comparisons of TFL vs. Ho:YAG lithotripsy are necessary to confirm this possibility. Previous preclinical works in the field confirmed this suggestion [11, 14].
Another interesting finding was the fact that we observed suboptimal visibility in 14.6% of cases, in most of them during surgery, we initially used high frequency settings (higher than 100 Hz), yet no statistically significant correlation between frequency and visibility was found. As for high laser powers (25–40 W) used in TFL lithotripsy in our study—we suggest that it should have no effect on urinary tissue. Previously, it has been shown by Andreeva et al. that Ho:YAG and TFL do not differ in thermal parameters [14]. Moreover, our postoperative data allows to suggest that TFL is a safe modality for lithotripsy, no cases of strictures or stenosis were found at 3 month follow-up.
Despite the benefits of Moses technology, the peak power (up to 15 kW) generated by Ho:YAG systems is much higher than that generated by TFL (500 W) [10]. The lower peak power of TFL creates a smaller vapor bubble and delivers more energy to the stone itself [10, 16, 21]. Thus, with lower energy consumption, TFL can achieve an ablation rate equivalent or superior to that of the Ho:YAG laser, which has been demonstrated for most common stone compositions including calcium oxalate monohydrate and uric acid [10, 16]. The smaller vapor bubble diameter generated by the TFL relative to the Ho:YAG (1 mm vs. 5 mm, respectively) also translates to reduced stone retropulsion as well as reduced collateral damage to tissues and endoscopic instruments [22, 23]. At the settings for lithotripsy, TFL is minimally ablative to surrounding tissues even when held in direct contact with the tissue [24].
TFL also allows for use of a smaller laser fiber diameter (as small as 100 μm) compared to Ho:YAG systems; this is attributed to the more uniform spatial beam profile of TFL [11]. This uniform beam profile is a result of using a diode laser pump as the energy source rather than a flashlamp. The smallest fiber diameter that was used in the current study was 200 μm; however, studies evaluating TFL using smaller diameter fibers are currently ongoing.
There were several limitations to this study. First, this was not a comparative study. Ideally, the TFL will soon be compared against the Ho:YAG laser (both standard and Moses) in a clinical setting. Currently, TFL is only approved for clinical use in urinary stone disease, BPH and bladder resection in Russia; the evaluation of TFL as a laser lithotripter will be enhanced as regulatory agencies in other nations approve TFL for clinical use. However, main goal of this study was to prove that TFL is an effective and safe device for stone lithotripsy. Second, the study included four surgeons, which may introduce variation in operative outcomes such as operative time; however, this did not interfere with our primary objective of assessing the safety and efficacy of TFL during PCNL. Third, the use of non-validated questionnaires (e.g., Likert scale from 0 to 2) may have been a potential source of bias, especially with four surgeons participating in the trial. One benefit of including data from multiple surgeons is demonstration of the point that SP TFL may be adaptable for surgeons of varying levels of experience and skill. Last major limitation is lack of data on TFL efficacy, current study is the first clinical work on TFL lithotripsy, therefore, we are unable to compare achieved data with any previous works in the field.
Conclusions
TFL is a safe and effective modality for lithotripsy during PCNL and results in minimal retropulsion. Further studies regarding the clinical efficacy and safety of TFL compared to Ho:YAG laser lithotripsy are required.
References
Enikeev D, Shariat SF, Taratkin M, Glybochko P (2020) The changing role of lasers in urologic surgery. Curr Opin Urol 30(1):24–29
Mullerad M, Aguinaga JRA, Aro T, Kastin A, Goldin O, Kravtsov A, Assadi A, Badaan S, Amiel GE (2017) Initial clinical experience with a modulated holmium laser pulse-moses technology: does it enhance laser lithotripsy efficacy? Rambam Maimonides Med J. https://doi.org/10.5041/RMMJ.10315
Ventimiglia E, Traxer O (2019) What is moses effect: a historical perspective. J Endourol 33(5):353–357
Glybochko P, Altshuler G, Yaroslavsky I, Vinarov A, Rapoport L, Enikeev D, Sorokin N, Dymov A, Vinnichenko V (2017) Comparative in vitro study of Ho: Yag and Tm fiber laser lithotripters in dusting mode of operation. J Urol 197(4):E815–E815
Nazif OA, Teichman JM, Glickman RD, Welch AJ (2004) Review of laser fibers: a practical guide for urologists. J Endourol 18(9):818–829
Jackson SD, Lauto A (2002) Diode-pumped fiber lasers: a new clinical tool? Lasers Surg Med 30(3):184–190
Enikeev D, Okhunov Z, Rapoport L, Taratkin M, Enikeev M, Snurnitsyna O, Capretz T, Inoyatov J, Glybochko P (2019) Novel thulium fiber laser for enucleation of prostate: a retrospective comparison with open simple prostatectomy. J Endourol 33(1):16–21
Enikeev D, Glybochko P, Rapoport L, Snurnitsyna O, Potoldykova N, Novoselova T, Laukhtina E, Taratkin M, Margulis V (2018) Need for upper urinary tract stenting in cases of ureteral orifice injury during laser enucleation of the prostate. Int Urol Nephrol 50(12):2173–2177
Glybochko PV, Rapoport LM, Enikeev ME, Enikeev DV (2017) Holmium laser enucleation of the prostate (HoLEP) for small, large and giant prostatic hyperplasia: tips and tricks. Urologia 84(3):169–173. https://doi.org/10.5301/uj.5000232
Fried NM (2018) Recent advances in infrared laser lithotripsy [Invited]. Biomed Opt Express 9(9):4552–4568
Traxer O, Keller EX (2019) Thulium fiber laser: the new player for kidney stone treatment? A comparison with Holmium: YAG laser. World J Urol. https://doi.org/10.1007/s00345-019-02654-5
Rapoport LM, Vinarov AZ, Sorokin NI, Dymov AM, Enikeev DV, Tsarichenko DG, Lekarev VY, Klimov RE, Andreeva VA, Kovalenko AA (2018) Experimental verification of thulium lithotripsy. Urologiia 5:74–80
Rosette JJ, Opondo D, Daels FP, Giusti G, Serrano A, Kandasami SV, Wolf JS Jr, Grabe M, Gravas S, Group CPS (2012) Categorisation of complications and validation of the Clavien score for percutaneous nephrolithotomy. Eur Urol 62(2):246–255
Andreeva V, Vinarov A, Yaroslavsky I, Kovalenko A, Vybornov A, Rapoport L, Enikeev D, Sorokin N, Dymov A, Tsarichenko D et al (2019) Preclinical comparison of superpulse thulium fiber laser and a holmium:YAG laser for lithotripsy. World J Urol 38:497–503
Dymov A, Glybochko P, Alyaev Y, Vinarov A, Altshuler G, Zamyatina V, Sorokin N, Enikeev D, Lekarev V, Proskura A et al (2017) Thulium lithotripsy: from experiment to clinical practice. J Urol 197(4):E1285–E1285
Blackmon RL, Irby PB, Fried NM (2011) Comparison of holmium:YAG and thulium fiber laser lithotripsy: ablation thresholds, ablation rates, and retropulsion effects. J Biomed Opt 16(7):071403
Kronenberg P, Traxer O (2019) The laser of the future: reality and expectations about the new thulium fiber laser-a systematic review. Transl Androl Urol 8(Suppl 4):S398–S417
Isner JM, Lucas AR, Fields CD (1988) Laser therapy in the treatment of cardiovascular disease. Br J Hosp Med 40(3):172–178
Winship B, Wollin D, Carlos E, Li J, Peters C, Simmons WN, Preminger GM, Lipkin M (2018) Dusting efficiency of the moses holmium laser: an automated in vitro assessment. J Endourol 32(12):1131–1135
Elhilali MM, Badaan S, Ibrahim A, Andonian S (2017) Use of the moses technology to improve holmium laser lithotripsy outcomes: a preclinical study. J Endourol 31(6):598–604
Gross A, Becker B, Taratkin M, Enikeev D, Rapoport L, Netsch C (2018) Wavelength and pulse shape effects on stone fragmentation of laser lithotripters. J Urol 199(4):E293–E294
Hardy LA, Kennedy JD, Wilson CR, Irby PB, Fried NM (2017) Analysis of thulium fiber laser induced bubble dynamics for ablation of kidney stones. J Biophoton 10(10):1240–1249
Wilson CR, Hardy LA, Irby PB, Fried NM (2015) Collateral damage to the ureter and Nitinol stone baskets during thulium fiber laser lithotripsy. Lasers Surg Med 47(5):403–410
Fried NM, Murray KE (2005) High-power thulium fiber laser ablation of urinary tissues at 1.94 microm. J Endourol 19(1):25–31
Author information
Authors and Affiliations
Contributions
DE—manuscript writting/editing; protocol development. MT—manuscript writting; protocol development; data analysis. RK—data collection; protocol development; data analysis. YA—manuscript editing; protocol development. LR—manuscript editing; protocol development. MG—manuscript editing; protocol development. DK—data collection; protocol development. SA—data collection; protocol development. GA—data collection; protocol development; DT—data collection; protocol development; IM—manuscript editing. EV—manuscript editing. EG—manuscript editing. ZO—manuscript editing; protocol development. FAJ—manuscript editing; data analysis. PG—manuscript editing; protocol development. OT—manuscript writting/editing; protocol development.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest was reported by the authors.
Ethical approval
Study was approved by the Sechenov University (Moscow, Russia) institutional review board.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Enikeev, D., Taratkin, M., Klimov, R. et al. Thulium-fiber laser for lithotripsy: first clinical experience in percutaneous nephrolithotomy. World J Urol 38, 3069–3074 (2020). https://doi.org/10.1007/s00345-020-03134-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03134-x