Abstract
Purpose
This study would like to develop a novel model similar to human prostate in terms of its texture profile, sensation upon resection, and anatomical hallmarks for resident transurethral resection of the prostate (TUR-P) training.
Methods
Ten phantom designs were proposed, using broadly available ingredients and a homemade protocol. Three steps of evaluation and development were done: objective measurement measuring texture profile (e.g. hardness, elasticity, cohesiveness/consistency, and adhesiveness/stickiness) using TA-XT2i Texture Analyzer (Llyod Instruments, Ametek Inc) to compare the designs with human prostate, finding the most similar design to prostate; expert consensus by a panel of urologist/senior residents comparing the simulation of TUR-P on the selected design with pre-existing control phantom; and anatomical design development using 3D printing for molding.
Results
Texture profile analysis for mean hardness, elasticity, cohesiveness/consistency, and adhesiveness/stickiness of human prostate was 3753.4 ± 673.4, 85 ± 1.9, 0.7 ± 0.03, and 0, respectively, and design IX was the most similar to human prostate (3660.7 ± 465.6, 87.0 ± 2.5, 0.6 ± 0.05, 0). Furthermore, expert consensus showed superiority of design IX compared with pre-existing control phantom (16.95 ± 1.36 vs 8.86 ± 3.10; P < 0.001). Most of the respondents agreed that the texture, consistency, and phantom ability to mimic human prostate upon resection were similar with human prostate, though hallmarks of the prostate e.g. veromontanum, and lobes were lacking. We used these feedbacks to develop a mold, designed to produce these important anatomical hallmarks.
Conclusion
This study developed a cost-effective prostate model from a food-based design that is similar to human prostate in terms of its texture and sensation upon TUR-P resection provided with important anatomical hallmarks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Benign prostatic hyperplasia (BPH) is a common pathological condition among adult men who have reached their sixties. Based on the data taken from Cipto Mangunkusumo National Referral Hospital (RSCM) in 1994–2013, a number of 3804 cases of BPH were reported with mean age of 66.61 years [1]. Many surgical techniques are available to treat BPH, but transurethral resection of the prostate (TUR-P) act as the gold-standard treatment for the disease [1]. Due to the high burden BPH in the country, the management of BPH, specifically TUR-P procedure, is essential for all urologists.
In the course of their training, it is important that urology residents develop surgical and technical skills for every procedure, reassuring the mature skills prior to operation on real patients [2]. This step needs consistent practice and supporting facility such as dry lab for surgical simulation [2]. Dry Lab became an integral part of surgical education, especially in urology, by offering an opportunity to practice on instrumental phantoms, preventing misconduct during the surgery, and achieving patient safety. Dry lab also enables supervisors to evaluate psychomotor skills of the residents before allowing them to proceed, performing the procedure on real patients [3]. Surgical residents may gain experience and expertise in utilizing the tools within the dry lab environment, which has lesser stressors compared with the operating room [4]. With all things considered, the application dry lab in surgical education may increase learning curve, thus benefiting the future practice relating to the specific procedure being simulated.
For TUR-P procedure, it is important for urologist to understand the basic anatomy and features available in human urinary system, especially the prostate [2, 5]. Furthermore, providing a similar simulation mimicking resection of the human prostate is the ultimate goal for dry lab training of TUR-P procedure [5]. Prostate phantom becomes an essential key instrument in TURP training, and its dimension and consistency should be able to emulate human prostate [5]. Limbs and Things Ltd. from Bristol, United Kingdom, has created a TURP trainer, which enables the trainees to perform resection on the phantom; however, the phantom in this simulator is still limited in providing similar consistency and motoric sensation during prostate resection due to its hygroscopic form, which makes it easily deformed [2, 5]. The phantom also costs around 117 euro which is not applicable to use in developing countries. Other approach is using virtual reality (VR) and haptic system, but it does not give the same feel as resecting the real human tissue [6,7,8].
In local setting, RSCM has started TUR-P training since 2010 by using a formalin-soaked tofu (bean curd) phantom. The prostate phantom is formed by soaking the tofu in 10% formalin solution for 24 h, unfortunately this prostate phantom did not produce the same sensations in the resection of human prostate, since it is considered too fragile.
To achieve better simulation experience, the objective of this study was to develop a model, most similar to prostate model composition, which will achieve the same consistency to the human prostate; inexpensive; and easy to produce; therefore, providing benefits for future urologists to train themselves while emulating the same feel as the human prostate.
Methods
A cost-efficient single-use homemade model was designed to mimic the texture and sensation of a human prostate. Ten designs/compositions were selected for further evaluation (Table 1). Evaluation for the proposed design was done in two stages, objective measurement and expert consensus. Objective measurement was done by directly comparing the texture profile parameters of the ten design models with human prostate. Expert consensus was done by a panel of expert consisting of urologists and senior residents, reviewing the selected design (the most similar to human prostate) with pre-existing control phantom for TUR-P simulation.
Objective measurement
Ten prostate designs were prepared and cooked using a uniformly made protocol. All the ingredients were mixed in a form of dough, beaten, and evenly prepared in an aluminium tray sized 7 × 7 × 5 cm. The dough was then covered with cloth and steamed for two and a half hours, in 100 °C heat. A lumen presenting the urethra was made at the center of the product using a bobba straw with approximate diameter of 2 cm. Reference texture parameter was taken from human prostate through by-products of TUR-P, and was prepared for texture analysis. All prostate samples with less than 2 cm of thickness were glued using transglutaminase (meat glue) and was rested overnight in − 20 °C. The product was made into small cubes for compression by the texture profile analyzer. Texture parameters were measured using Lloyd Texture Profile Analyzer, TA-XT2i (TA plus, Llyod Instruments, Ametek Inc.) using Texture expert software (Szczesniak, 1990) in the food science department of Institut Pertanian Bogor (IPB) (Fig. 1). Four outcome parameters obtained from the texture profile analysis curve were included, namely hardness, elasticity, cohesiveness/consistency, and adhesiveness/stickiness. Hardness is defined as the force needed to compress samples, elasticity is defined as the rapidity and degree of recovery from a deforming force, cohesiveness/consistency is defined as the degree to which the material can be deformed before it breaks, and adhesiveness/stickiness is defined as the work/force necessary to overcome the attractive forces between the surface of the product and the surface of the probe that came in contact. All parameters are internationally recognized in food science field. Each designs and prostate samples underwent two successive compression cycles performed at a constant displacement rate of 1 mm/s, using 205 g force. The material was compressed 50% of the original height, and the return height at the secondary compression was 5 mm above original height. Statistical analysis using independent T test were then done to compare all the parameters of each of the designs with the prostate as a reference.
Expert consensus
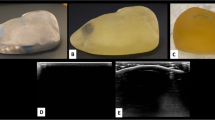
Expert consensus was done by a panel urologists’ and senior residents experience in doing TUR-P procedure on the proposed prostate model design with a control model (Fig. 2). The panel consisting of all consultant urologists and senior residents of Cipto Mangunkusumo National Referral Hospital with minimum 50 experiences of TUR-P procedure before the time of consensus. We compared the most similar design to human prostate (design IX) from the previous evaluation with a control model that is widely used for TUR-P training with similar cost to our design. The control model for this study was large potatoes that were hollowed for urethral lumen, as it is one of the commonly used affordable model worldwide. The consensus consists of four criteria, involving the similarity of texture and appearance, similarity of cohesiveness/consistency, similarity of experience on simulation, and likelihood for recommending the design model. Each of the criteria were initialy statistically evaluated using Cohen’s kappa measure for inter-rater reliability (n = 10) with a result of 0.783 (P value 0.011), 0.615 (P value 0.035), 0.615 (P value 0.035), and 1 (P value 0.002), indicating substantial to perfect agreements. Data were reported using a Likert scale, scoring each opinion/answer from the questionnaire as numbers, 1 for strongly disagree, 2 for disagree, 3 for neutral, 4 for agree, and 5 for strongly agree. An overall score was then computed, ranging from 0 to maximum score of 20. Comparison between the chosen design (design IX) model and control model was done using a statistical study of independent T test.
Results
Objective measurement
We evaluated the texture parameters of ten prostate models and human prostate. Each of the designs and human prostate was measured on a minimum of seven samples using Lloyd Texture Profile Analyzer (TA-XT2i, Llyod Instruments, Ametek Inc.) using the pre-adjusted settings. Mean hardness, elasticity, cohesiveness/consistency, and adhesiveness/stickiness of human prostate were 3753.4 ± 673.4, 85 ± 1.9, 0.7 ± 0.03, and 0, respectively. All ten designs were also measured accordingly, and results were presented on Table 2. Statistical comparison was also done to compare each of the designs with the prostate as a reference value. Among the ten designs, design number IX was objectively more similar to the human prostate samples in terms of its mean hardness, elasticity, cohesiveness/consistency, and adhesiveness/stickiness (P value 0.899, 0.751, 0.197, and 1, respectively).
Expert consensus
Following the objective measurement, the most similar design (number IX) was continued for the evaluation for expert consensus. We compared the prostate model with a commonly used affordable phantom in international setting, large potatoes, as a control. Comparison was done on the simulation of the TUR-P resection between the selected model compared with the control using the same simulator kit present in Department of Urology, Cipto Mangunkusumo National Referral Hospital (Fig. 2) and Olympus (Olympus Medical, Tokyo, Japan). 26 Fr resectoscope and 0.9% normal saline (NS) were used as an irrigant. From a panel consisting of 22 urologists and senior residents, our study reported a mean overall score of 16.95 ± 1.36 for the selected design model compared with 8.86 ± 3.10 for the control phantom. The score for our selected design model was significantly higher with P < 0.001 in comparison with the control (Fig. 3). Amongst the questions within the questionnaire, most of the respondents agreed that the texture, consistency, and phantom ability to mimic human prostate upon resection were similar to the human prostate (5 strongly agree, and 16 agree) while only one answered neutral. About 9 respondents strongly agreed to recommend the model for future use, while 13 others agreed. None of the respondents answered neutral, disagree, or strongly disagree. The complete comparison between the respondents’ answers on the selected design and control is presented in Fig. 4. Upon the feedback given, most of the feedback were to improve the anatomical hallmark of the prostate phantom, eight respondents recommend the inclusion of veromontanum, while ten respondents requested for inclusion of visible enlarged lobes.
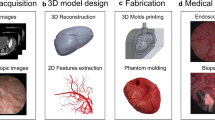
Development of anatomically similar to human phantom design
Using the feedback from the consensus, we developed a 3D mold design to create anatomical hallmarks of prostate phantom to imitate the human prostate (Fig. 5). The dimension of prostate was designed with a volume of 50 × 30 × 50 mm, urethral length of 30 mm, and diameter of 13 mm. Distinguishable veromontanum and lateral lobes were designed for the mold to better illustrate the human prostate.
Discussion
The role of dry lab training in residency module has become influential in increasing the learning curves of residents while still maintaining the safety of the patients [2]. A good model may provide sufficient opportunity to develop surgical and technical skills for every procedure, through replicating the basic anatomy and characteristics of the involved organs [2]. The development of a model that may emulate real organs, will benefit the residents to get more familiarized with the procedure; therefore, increasing the experience and mastery. Given the chance to get familiarized with the technique in dry lab where less stressors/pressures are present in comparison with the operating table will help develop a good learning curve and minimize unwanted complications, as suggested by previous studies. For transurethral resection of prostate specifically, it is important for residents to become familiarized with the consistency of the prostate, the feel and the products of TUR-P from the prostate, the manoeuvrability within the surgical field within the prostate, and the important hallmarks that may affect the technique of surgical procedure [5].
Current available simulators and phantoms for TUR-P training are limited to either being too simple and cheap [9,10,11,12] or too sophisticated and costly [7,8,9,10,11,12,13]. Simpler models, are present as varying forms, from using poultry, beef, and pork sausages [9], vegetables e.g. large potatoes [10], and cadaveric prostate from human [11]. These simpler models are affordable and may provide true resection, resulting in TUR-P products, albeit may not resembling real TUR-P products of the human prostate. Some known simple models are being used in current practice, such as apples, potatoes, sausages, and cadaveric prostate. However, these models are still unable to provide similar texture of the human prostate, as models like sausages and cadaveric prostate are too soft [9, 11], while apples and potatoes are often too hard to resect and provide luminal space which is difficult to maneuver in Ref. [8]. Furthermore, the major drawbacks of these simpler models are their inability to emulate the urinary system (specifically the prostate), in regards to the anatomical hallmarks and functional mechanisms of the urinary system [7]. On the other hand, recent development of the more sophisticated virtual reality (VR)-based simulator has enabled real time simulation of TUR-P by providing a visual imitation of the prostate anatomy and functional traits of the system such as bleeding and vital signs changes throughout the procedure [7, 8]. The advantages of these models have given residents opportunities to get familiarized with prostate anatomical hallmarks, to attempt control of fluid flow and bleeding, and to observe the effects of their handling towards vital signs of the patients [8, 13]. However, one main limitation of the VR system is its lack of material to resect on [8, 13]. The VR system consists of a void compartment with kinetic sensors connecting to the system which will convert any movements into visual output on the monitor [14]. The system does not provide any substance to be truly resected on, meaning no motoric sensation of resecting the prostate is provided [14]. It became a great loss, as the motoric sensation in prostate resection is one of the main factors that may help residents to develop skills and control in doing TUR-P procedure.
We decided to choose a food-based design for our proposed model to develop an easily made model costing less than other available factory-made models, that could be easily reproduced by all centers. Another main reason of using a food-based model consisting of animal meat in its composition is to achieve a prostate model that would simulate the resection on the human prostate, as similarly as possible. One known available commonly used model is sausages, which is said to be an affordable and effective option for TUR-P simulation [9]. The drawback of using sausage is its low availability in certain regions/country and its heterogeneous composition. We decided to create an alternative model with ingredients that are generally available in all area. We included all types of flours for our proposed designs to harden and avoid dispersion of the model upon resection, with a certain amount of elasticity and consistency. We also tried to adjust the amount of the flour included to reduce the stickiness, so the composition would simulate the resection on the prostate better. In our selected model, we found out that a recipe consisting of mackerel (fish) and starch flour with specific amount would result in a texture profile similar to those of prostate.
This study has successfully developed a prostate phantom design that is objectively and subjectively similar to human prostate upon TUR-P. The aim of this study is to develop a cost-efficient design which focuses on the kinetic aspect of the simulation, therefore, emulating the motoric sensation of resecting a real human prostate. As the first study to measure the texture of human prostate, our study has achieved most similar hardness, elasticity, cohesiveness/consistency, and adhesiveness/stickiness of a prostate phantom design to human prostate. The selected prostate phantom design was further tested for resection, while being reviewed with experienced operators, consisting of urologists and residents. This consensus resulted in an outstanding review preferring the newly developed design model. Furthermore, this phantom is ahead in its economic value, as each single use of this phantom only costs about 4 USD per unit [13].
The biggest advantages of our phantom are its ability to demonstrate the feeling and sensation of resection and to provide results of a resection as similar to TUR-P on human prostate. The review from the urologists upon resection on the phantom was all positive, mostly praising its consistency/cohesiveness and its non-stickiness on the bipolar cautery. This finding is also in accordance to our objective finding on the texture profiles of our phantom that closely resembles the prostate. The result of the resection on the phantom produced resected areas and prostatic chips that are very similar to the TUR-P in human prostate. As the resected areas imitates real prostate, the resident should be able to learn the targeted result of a TUR-P procedure, knowing when to stop and when to continue the resection. The burnt/resected chips are also easily mobilized, making it easier for the operator to manipulate the surgical field.
Although the main focus of our study is to develop a phantom that enables resident to experience the motoric sensation in resecting the prostate, our study also tried to bring the important anatomical hallmarks of human prostate to the phantom. Three important domains were covered, which are the lumen size and diameter, length, and structures of lateral lobes and veromontanum. It may not provide the exact resemblance of the human anatomy as given by the VR-based simulator; however, we concluded that the anatomical hallmarks are beneficial in accommodating the residents to be familiarized in doing the procedure using operational standards. The limitation of the study includes its short longevity and its inability of providing the physiological dynamics throughout the procedure as provided by VR system. The short longevity of the phantom is due to the composition of the phantom which is food based, specifically using mackerel as its main ingredient. It may not be as optimal if being used more than 3–5 days after production, as food-based materials are often spoiled which will affect heavily on its texture and consistency. Furthermore, providing the physiological dynamics of the simulation e.g. vital signs and bleeding requires complex programming and a robust number of funding.
There are limitations of the methodological aspects of our research. Our study was not yet able to assess the result of our design model for resident learning curve in the long run. Our study currently focused on the development of the model, and in future, it should be continued to evaluate its effect on residents learning curve on affecting the clinical outcomes to the patients. The 3D model described in the study was also still in the initial phase, and should be developed further to achieve an anatomically similar model to the human prostate. We plan to construct a mold from a 3D reconstruction of normal human prostate MRI in our next project. Because we only evaluate the prostate product of TURP for texture analysis, we currently can only provide general texture of the prostate, and could not asses or evaluate if the texture of different part of prostate would also be different. There may also be small difference of texture profile due to the resection.
As our study is an early phase of a continuing simulator system development, the current study is the first stepping stone to achieve the ideal simulator for TUR-P dry lab training. Future study in developing a simulator covering all the organs of the urinary tract, that is modeled to imitate the real human urinary tract anatomy in terms of its measurements and hallmarks. The next step is to develop the human mimicking prostate model to achieve high longevity and possibility for mass production by developing a model made from silicon composition that provides similar texture to this study. Long-term plan of the study is to incorporate an augmented reality system, with the current prostate phantom as a single use reloadable phantom and the urinary tract simulator.
Conclusion
This study has developed a cost-effective homemade prostate model that is objectively and subjectively similar to human prostate in terms of its texture and sensation upon TUR-P resection provided with important anatomical hallmarks. Future development is planned for the whole urinary system than may help emulate the procedure similarly to in real human, possibly integrating the augmented reality system in the simulation.
References
Tjahdojati, Soebadi DM, Umbas R, Purnomo BB, Widjanarko S, Mochtar CA et al (2017) Panduan penatalaksanaan klinis: pembesaran prostat jinak (benign prostatic hyperplasia/BPH). Ikatan Ahli Urologi Indonesia
Brewin J, Ahmed K, Khan MS, Jaye P, Dasgupta P (2014) Face, content, and construct validation of the Bristol TURP trainer. J Surg Educ 71(4):500–505
Kapadia MR, Da-Rosa DA, Mac-Rae HM, Dunnington GL (2007) Current assessment and future directions of surgical skills laboratories. J Surg Educ 64(5):260–265
Matsumoto ED, Hamstra SJ, Radomski SB, Cusimano MD (2001) A novel approach to endourological training: training at the surgical skills center. J Urol 166:1261–1266
Niessen WJ, Viergever MA (2001) Medical image computing and computer-assisted intervention—MICCAI 2001. In: The forth international conference Proceedings. Springer, Utrecht, pp 360–367
Burdea G, Patounakis G, Popescu V, Weiss RE (1999) Virtual reality-based training for the diagnosis of prostate cancer. IEEE Trans Biomed Eng 46(10):1253–1260
Tjiam IM, Berkers CH, Schout BM, Brinkman WM, Witjes JA, Scherpbier AJ et al (2014) Evaluation of the educational value of a virtual reality TURP simulator according to a curriculum-based approach. Simul Healthc 9(5):288–294
Källström R, Hjertberg H, Kjölhede H, Svanvik J (2005) Use of a virtual reality, real-time, simulation model for the training of urologists in transurethral resection of the prostate. Scand J Urol Nephrol 39(4):313–320
Bach T, Geavlete B, Herrmann TRW, Gross AJ (2009) Homemade” TUR-simulator for less than $40 U.S.? The “TupperTM” experience. J Endourol 23(3):509–513
Khan R, Aydin A, Khan MS, Dasgupta P, Ahmed K (2015) Simulation-based training for prostate surgery. BJU Int 116(4):665–674
Ahmad S, Byrne D, Ghulam N (2013) Training model for transurethral resection of prostate using human cadavers embalmed by Thiel's method. Videourology. https://doi.org/10.1089/vid.2013.0026
Hou S, Ross G, Tait I, Halliday P, Tang B (2017) Development and validation of a novel and cost-effective animal tissue model for training transurethral resection of the prostate. J Surg Educ 74(5):898–905
Sweet R, Porter J, Oppenheimer P et al (2002) Simulation of bleeding in endoscopic procedures using virtual reality. J Endourol 16:451–455
Ben-Zvi T, Hueber PA, Valdivieso R, Azzizi M, Tholomier C, Bienz M et al (2015) Urological resident exposure to transurethral surgical options for BPH management in 2012–2013: a pan-Canadian survey. Can Urol Assoc J 9(3–4):E236
Funding
There is no external funding done for this study. All expenses were covered by the institution and authors.
Author information
Authors and Affiliations
Contributions
NR: project design, project development, data collection, and manuscript writing. HWKP: data collection and manuscript writing. PB: manuscript writing and supervision. IW: data collection and supervision. CAM: data analysis and supervision. ARAHH: project design, supervision, and manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (The Ethics Committee of the Faculty of Medicine, University of Indonesia; Ethical Approval number 0224/UN2.F1/ETIK/2018) and with the 1964 Helsinski declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rasyid, N., Putra, H.W.K., Birowo, P. et al. TUR-P phantom for resident surgical training: food-based design as a human mimicking model of the prostate. World J Urol 38, 2907–2914 (2020). https://doi.org/10.1007/s00345-020-03085-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03085-3