Abstract
Objectives
To evaluate the effect of intensified treatment parameters on safety, functional outcomes, and PSA after MR-Guided Transurethral Ultrasound Ablation (TULSA) of prostatic tissue.
Patients and methods
Baseline and 6-month follow-up data were collected for a single-center cohort of the multicenter Phase I (n = 14/30 at 3 sites) and Pivotal (n = 15/115 at 13 sites) trials of TULSA in men with localized prostate cancer. The Pivotal study used intensified treatment parameters (increased temperature and spatial extent of ablation coverage). The reporting site recruited the most patients to both trials, minimizing the influence of physician experience on this comparison of adverse events, urinary symptoms, continence, and erectile function between subgroups of both studies.
Results
For Phase I and TACT patients, median age was 71.0 and 67.0 years, prostate volume 41.0 and 44.5 ml, and PSA 6.7 and 6.7 ng/ml, respectively. All 14 Phase I patients had low-risk prostate cancer, whereas 7 of 15 TACT patients had intermediate-risk disease. Baseline IIEF, IPSS, quality of life, and pad use were similar between groups. Pad use at 1 month and quality of life at 3 months favored Phase I patients. At 6 months, there were no significant differences in functional outcomes or adverse events.
Conclusion
TULSA demonstrated acceptable clinical safety in Phase I trial. Intensified treatment parameters in the TACT Pivotal trial increased ablation coverage from 90 to 98% of the prostate without affecting 6-month adverse events or functional outcomes. Long-term follow-up and 12-month biopsies are needed to evaluate oncological safety.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The incidence and prevalence of prostate cancer (PCa) have risen in recent decades due to changes in demographics, and improvements in diagnosis and screening [1]. For men with very low-risk PCa, active surveillance is an option to reduce overtreatment [2]. Patients who do not qualify for active surveillance or are unwilling to undergo active surveillance require definitive treatment options for localized PCa such as radical prostatectomy or radiotherapy [2]. These definitive treatment options have shown excellent tumor control and minimal adverse events in competence centers and are, therefore, considered as gold standard in the treatment of localized PCa [3]. Beside these options, alternative treatment methods have emerged aiming local tumor control with reduced procedure-related side-effects. Still in their infancy, these techniques lack long-term data, and their efficacy and safety are matter of recent studies [2].
Magnetic resonance imaging (MRI)-guided transurethral ultrasound ablation (TULSA) is a novel therapeutic tool for thermal ablation of prostatic tissue with the advantages of MRI planning and live MRI thermometry feedback/guidance. A recent Phase I trial demonstrated the clinical feasibility and safety of TULSA in 30 patients with localized PCa at three institutions [4], and the subsequent TULSA-PRO Ablation Clinical Trial (TACT) Pivotal study is investigating efficacy and safety in 115 men across 13 sites. The Phase I safety and feasibility trial intentionally used conservative treatment margins, sparing 3 mm of untreated prostate tissue at the apex, along with a 3-mm margin of untreated prostate tissue peripherally at the inside of the prostate capsule. This was expected to leave 10% of the prostate volume untreated, and the resulting risk of residual disease was willingly accepted. While not a primary endpoint of the Phase I study, 12-month biopsy identified clinically significant PCa in 31% of patients, and any disease in 55% of patients. For the TACT trial, treatment parameters were intensified towards the goal of achieving complete whole-gland ablation with reduced prostate tissue sparing, accepting the risk of increased treatment-related side effects. The results of follow-up biopsy are pending.
Here we evaluate the impact of intensified treatment parameters on treatment safety by comparing adverse events, functional outcomes, and PSA course for Phase I and TACT patients treated at an experienced single center that enrolled patients to both studies.
Patients and methods
The Phase I trial (NCT01686958) recruited 30 men ≥ 65 years with biopsy-proven PCa (Gleason score 3 + 3 or 3 + 4, PSA ≤ 10 ng/ml, clinical stage T1c–T2a, N0, M0) across three centers. The TACT Pivotal study (NCT02766543) recruited 115 patients ≥ 45 years with biopsy-proven PCa (Gleason score 3 + 3 or 3 + 4, PSA ≤ 15 ng/ml, clinical stage T1c–T2a, N0, M0) across 13 centers. In Germany, recruitment of men with Gleason 3 + 4 was not allowed for the Phase I trial. Both trials were approved by the respective ethics boards, and written informed consent was obtained from all study participants.
As the aim of this analysis was to evaluate the effect of intensified treatment parameters on safety and functional outcomes, the influence of physician experience was minimized by only including patients treated at a single experienced center (University of Heidelberg; Germany) that enrolled the most patients to both studies. All patients at this center were treated by the same physicians for both trials: 14 patients in Phase I, and 15 in the TACT study.
MRI-guided TULSA procedure
The TULSA-PRO investigational device (Profound Medical Inc., Toronto, Canada) was described previously [4,5,6,7]. All TULSA procedures were performed under general anesthesia. A suprapubic catheter was inserted before the procedure. The rigid transurethral ultrasound applicator (UA) was inserted over a nitinol guidewire and mounted to a positioning system (PS) that provided remote linear and rotational motion of the UA. The UA consisted of 10 independent ultrasound transducers that emitted directional high-intensity ultrasound for thermal ablation of prostatic tissue. To protect the prostatic urethra, the UA was cooled by flowing water to preserve 1–2 mm of tissue around the array. To protect the rectal wall, a passive endorectal cooling device was used.
Treatment took place in a 3 Tesla MRI (Phase I: Magnetom Trio, Siemens, Munich, Germany; TACT: Magnetom Prisma, Siemens, Munich, Germany). The UA was positioned within the prostatic urethra under MRI guidance. The urologist and radiologist defined treatment plans by delineating the outer boundaries of the prostate on high-resolution T2-weighted MRI images acquired in alignment with each individual UA transducer element. In both studies, treatment plans spared a 3-mm safety margin of untreated tissue towards the external rhabdosphincter. A second safety margin of spared prostate tissue along the inner edge of the prostate capsule was defined differently between the Phase I and TACT studies as described below. Treatment of the prostate was done under live MRI thermometry feedback control of ultrasound power to each element during a complete rotation of the UA [4].
Treatment differences between the Phase I study and the TACT pivotal study
In the Phase I safety and feasibility study, the treatment controller aimed to deliver temperatures ≥ 55 °C from the urethra out to a margin set 3 mm inside of the prostatic capsule. Histological studies of MRI–TULSA predict acute cell kill of tissues whose temperature measured by MR thermometry exceeds 55 °C [5, 8]. Delayed cell kill was expected to migrate outward an additional 1–3 mm [8], correlating with an isoeffective thermal dose of 240 cumulative equivalent minutes at 43 °C (CEM43) [9], a widely accepted predictor of the extent of thermal coagulation [5, 10]. With a control temperature of 55 °C set 3 mm inside the capsule, the total volume of acute and delayed cell kill was expected to cover 90% of the gland, sparing a rim of viable prostate tissue at the periphery. These controller parameters were chosen to enable MR thermometry measurement of the spatial treatment precision and the expected extent of delayed cell kill within the prostate [11].
In the TACT study, the treatment control parameters were intensified for complete prostate ablation by delivering higher temperatures closer to the capsule. As thermal dose is a function of temperature and exposure time, the controller aimed to deliver ≥ 57 °C at a margin set 2 mm inside the capsule, and the minimum rotational speed was reduced from 8 to 4 degrees per minute. Simulations predicted these changes would deliver acute cell kill ≥ 55 °C to within 1 mm of the prostate capsule [6], with the total volume of acute and delayed cell kill covering 99% of the targeted prostate volume (Fig. 1).
Evaluated parameters and follow-up
At the baseline visit, all patients underwent physical examination, transrectal ultrasound, and blood chemistry. PSA values were determined at treatment day and during follow-up. The first follow-up was after 2 weeks to evaluate micturition and remove the suprapubic catheter. Detailed follow-up visits at 1, 3, and 6 months included physical examination, blood samples including PSA values, and evaluation for adverse events using Common Terminology Criteria for Adverse Events v.4 [12]. All patients completed standardized questionnaires at the baseline visit and follow-up including the international index for erectile function (IIEF-15) questionnaire, and the international prostate symptom score (IPSS) and quality of life (QoL) questionnaire. Urinary continence was evaluated by interview and pad use. Ablation coverage (measured by MR thermometry) was calculated for all patients and compared between groups [11].
Statistical analysis
Descriptive statistics for the evaluated parameters were reported by their median and inter-quartile range. Comparisons between the Phase I and TACT study patients used Chi square tests for categorical variables, and Mann–Whitney U tests for continuous variables, with a significance threshold of p < 0.05. All statistical analyses were carried out using IBM SPSS software package version 25.
Results
Patient characteristics
Baseline clinical data are given in Table 1. In Phase I, 12/14 patients had an MRI/TRUS fusion biopsy [13] for diagnosis of PCa, and 2/14 had a transrectal, TRUS-guided biopsy. In the TACT study, 10/15 patients had a baseline MRI/TRUS fusion biopsy [13], 5/15 had a TRUS-guided biopsy. All TACT patients had a protocol-mandated pre-intervention MRI of the prostate to rule out advanced disease.
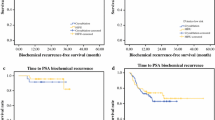
Comparison of ablation coverage measured by MR thermometry revealed that 90% (IQR 88–92%) and 98% (IQR 97–99%) of the gland reached a lethal thermal dose of 240 CEM43 in the Phase I and TACT trials, respectively (p < 0.01). The PSA nadirs in Phase I and TACT patients were 0.7 ng/ml (IQR 0.2–0.8) and 0.5 ng/ml (IQR 0.2–1.2), respectively (p > 0.05), reached in a median of 3 months (Table 2).
Functional outcomes
At 6 months, functional outcomes in patients from the Phase I and TACT studies were similar in terms of urinary symptoms, incontinence, and erectile function. The suprapubic catheter was removed 14.5 days (median; IQR 13.0–25.0) and 20.0 days (median; IQR 10.3–42.0) after treatment in Phase I and TACT patients, respectively (p = 0.18). Micturition during follow-up was evaluated by IPSS and QoL questionnaires (Table 3). Patients from both trials showed an increase in IPSS score after 1 month, with improvements from baseline at 3 and 6 months, and no statistical difference between groups (p > 0.05). None of the Phase I patients reported urinary leakage or pad use at baseline or follow-up. Among TACT patients, at the 1-month visit three patients needed 1 pad/day (significant difference to Phase I, p = 0.04) and one patient needed 2 pads/day. At the 3-month visit, one patient required 1 pad/day. At the 6-month visit, none of the TACT patients required pads. Quality of life was better in Phase I patients at 3 months (p = 0.01) and was comparable between groups at baseline, 1 month, and 6 months. Erectile function was evaluated using question two of the IIEF questionnaire (erections sufficient for penetration) as the ability to penetrate in more than 50% of attempts. At baseline, 40% and 60% of Phase I and TACT patients had good erectile function (p = 0.36). At 6 months, 29% and 47% of Phase I and TACT patients reported good erectile function, respectively (p = 0.32). IIEF scores were comparable between groups, with a decline at 1 month followed by recovery at 3 and 6 months (Table 4).
Adverse events
Adverse events of any grade were experienced by 11/14 patients in Phase I (78.5%) and 12/15 patients in TACT (80.0%). There were no intraoperative complications, no rectal injuries or fistulae, and no cases of severe urinary incontinence. There were no grade 4 or higher adverse events. In both groups, all patients were discharged 1 day after the procedure. Aside from one attributable grade 3 adverse event in Phase I, and one in TACT, all adverse events were grade 1 or 2. Both grade 3 adverse events were epididymitis, resolved with hospitalization and intravenous antibiotic therapy (Phase I and TACT) and vasectomy (TACT). Other adverse events mainly consisted of urinary tract infection [Phase I: 6/14 (43%); TACT: 10/15 (66.6%); p = 0.229], epididymitis with outpatient antibiotic treatment [Phase I: none; TACT: 3/15 (20%)], bladder outlet obstruction [Phase I: 6/14 (43%); TACT: 2/15 (13%)] or urgency [Phase I: 5/14 (36%); TACT: 3/15 (20%)]. All grade 1 and 2 adverse events could be managed with outpatient treatment, medication, or catheterization. All adverse events occurred during the first 3 months and resolved with adequate treatment (Table 5).
Discussion
MRI-guided TULSA has demonstrated clinical safety and feasibility in a Phase I trial [4]. In contrast to other ablative therapies like transrectal HIFU or cryotherapy, TULSA treatment is planned and delivered under live MRI visualization and MRI thermometry. Thereby, treatment planning, heat delivery, and ablation extent can be controlled precisely [4]. In the Phase I trial, the treatment controller was designed to deliver temperatures ≥ 55 °C up to a 3-mm margin inside of the prostate capsule. In concordance with the treatment plan, a lethal thermal dose (≥ 240 CEM43 [9]) was achieved in 90% of the gland [11]. This was confirmed by an 88% reduction in viable prostate tissue volume measured using 12-month MRI and biopsy data [11]. To increase ablation coverage, treatment parameters in the TACT study were modified to deliver higher temperatures (≥ 57 °C) closer to the prostate capsule (2 mm interior margin). In our patients, this increased the extent of lethal thermal dose from 90% of the prostate volume in Phase I, to 98% coverage in the TACT study. We observed some evidence that PSA nadir at 6 months was lower in TACT, but the difference did not reach significance in our single-center subsets. Preliminary data for the whole patient collective of the TACT trial showed a significant difference in PSA decline at 6 months compared to Phase I [14]. As previously demonstrated, PSA nadir is a prognostic parameter for disease-free survival in patients undergoing HIFU treatment [15, 16] with the lowest risk for disease recurrence in patients with the lowest PSA nadir. However, longer follow-up including prostate biopsy is mandatory to assess whether the modified treatment parameters affected oncological safety for TULSA treatment as PSA nadir is only a surrogate parameter.
The therapeutic benefits of increasing the treatment temperature and ablation extent were expected to be accompanied by an increased risk of side effects. The main purpose of this study was to evaluate whether the intensified TULSA treatment parameters in the TACT study affected the previously demonstrated clinical safety of the Phase I trial. As the experience of the physician can also have an effect on treatment outcomes, this analysis only included data from patients treated at one experienced institution [17].
There were no significant differences in treatment safety between Phase I and TACT patients. However, due to the small group sizes, some potentially important differences did not meet statistical significance. In particular, patients in TACT had to tolerate their catheter a median of 1 week longer than in Phase I. As prostate volumes were comparable between groups, we attribute this difference to increased swelling of the prostate due to the increased temperature and treatment volume. The correlation of higher obstruction rates with increased treatment volume has been described for transrectal HIFU [18]. Bladder outlet obstruction is a typical side effect of transrectal HIFU. Without prior transurethral resection, up to 50% of HIFU patients develop bladder outlet obstruction with the need for surgical intervention [19, 20], with a reported median time to bladder outlet obstruction of 6 months after a single HIFU session [20]. None of the patients treated with TULSA required surgical intervention for bladder outlet obstruction during 6 months follow-up, and the number of bladder outlet obstruction events was lower in TACT patients. Further, evaluation of IPSS scores even showed that micturition symptoms improved after 3 months, suggesting a simultaneous therapeutic effect on benign prostatic enlargement and derived symptoms. The transurethral access, non-focused delivery of thermal energy, and lower peak treatment temperature seem to have a different effect than transrectal HIFU, making TULSA more comparable to other transurethral BPH treatments like transurethral needle ablation or transurethral microwave ablation [21].
As the treatment is performed in a MRI suite under live MRI-thermometry, ablation extent can be monitored during treatment and real-time adjustments can be made for complete treatment of the intended target volume [5, 6, 22]. MRI guidance also facilitates sparing of surrounding sensitive structures. In Phase I, none of our patients experienced incontinence, and erectile function returned to baseline levels after 6 months. No significant differences were observed in TACT study patients at 6 months. However, 4 of 15 (26.6%) and 1 of 15 (6.7%) TACT patients used pads due to urgency and mild incontinence at 1 and 3 months, respectively. This may have influenced transient differences in quality of life, favoring Phase I patients at 3 months. Median IIEF scores had not yet returned to baseline in TACT patients after 6 months as in Phase I, but there were no significant differences in the number of patients with erections sufficient for penetration between groups, or between baseline and 6 months for either group. We attribute the observed differences to the reduction of the safety margin from the prostatic capsule and the subsequently increased treatment volume and delivered energy.
During the Phase I trial, a high rate of urinary tract infections across all three study centers was a matter of concern and attributed to the preoperative cystoscopy, the suprapubic catheter, or insertion of the transurethral ultrasound device [4]. At our institution infections occurred more often in TACT patients, but this difference was not statistically significant. The rate of epididymitis was also higher in TACT patients. Urinary tract infections attributed to necrosis caused by thermoablative treatments of the prostate are not uncommon and have been described extensively for transurethral needle ablation [23], transurethral microwave thermotherapy [24, 25], transurethral laser coagulation [26], and transrectal HIFU [19]. The higher rates of urinary tract infections in TACT patients may, therefore, be attributed to increased necrosis as a result of the higher energy delivered to a larger treatment volume. As infection rates are a matter of concern, action should be taken to overcome this issue. In transrectal HIFU, the combination with TURP to remove debris reduced the infection rate significantly [27], but is also used to overcome high rates of obstructive micturition and bladder neck obstructions. As described by Chaussy et al., the use of low-dose antibiotic prophylaxis also resulted in significantly lower urinary infection rates after HIFU [18]. In our collective, all patients with symptomatic urinary tract infections were treated successfully by antibiotics. To overcome the high rates of urinary tract infections observed in TULSA throughout the Phase I and TACT trials, extension of antibiotic prophylaxis from a solely perioperative course to several weeks after TULSA should be considered.
Limitations of this study include the small number of patients and the short follow-up of 6 months. Although early clinical safety can be evaluated at 6 months, evidence of oncological efficacy for TACT patients requires further follow-up including prostate biopsy at 12 months, and long-term evaluation of clinical safety is needed to rule out late toxicity.
Conclusion
TULSA is a safe and well-tolerated treatment for transurethral ablation of prostatic tissue, as demonstrated in a Phase I safety and feasibility trial. For the subsequent TACT Pivotal study of safety and efficacy, intensified treatment parameters increased ablation extent from 90 to 98% coverage of the prostate. Comparing adverse events and functional outcomes in subgroups of patients from the Phase I and TACT trials who were treated at a single experienced institution demonstrated that clinical safety was not affected by these changes to the treatment algorithm.
Abbreviations
- CEM43:
-
Cumulative equivalent minutes at 43 °C
- IIEF:
-
International index for erectile function
- IPSS:
-
International prostate symptom score
- IQR:
-
Interquartile range
- MRI:
-
Magnetic resonance imaging
- PCa:
-
Prostate cancer
- PS:
-
Positioning system
- QoL:
-
Quality of life
- TACT:
-
TULSA-PRO Ablation Clinical Trial
- TULSA:
-
Transurethral ultrasound ablation
- UA:
-
Ultrasound applicator
References
Krebs in Deutschland 2013/2014 (2017) 11. Ausgabe. Robert Koch-Institut (Hrsg) und die Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. (Hrsg). Robert Koch-Institut, Berlin. https://doi.org/10.17886/rkipubl-2017-007. ISBN: 978-3-89606-288-8
Mottet N, Bellmunt J, Briers E, Bolla M, Bourke L, Cornford P, De Santis M, Henry A, Joniau S, Lam T, Mason MD, Van den Poel H, Van den Kwast TH, Rouvière O, Wiegel T members of the EAU–ESTRO–SUR–SIOG Prostate Cancer Guidelines Panel. EAU–ESTRO–ESUR–SIOG Guidelines on Prostate Cancer. Edn. Presented at the EAU annual congress Copenhagen 2018. ISBN:978-94-92671-02-8. EAU Guidelines Office. Place published, Arnhem, The Netherlands
Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, Davis M, Peters TJ, Turner EL, Martin RM, Oxley J, Robinson M, Staffurth J, Walsh E, Bollina P, Catto J, Doble A, Doherty A, Gillatt D, Kockelbergh R, Kynaston H, Paul A, Powell P, Prescott S, Rosario DJ, Rowe E, Neal DE, Protec TSG (2016) 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 375(15):1415–1424. https://doi.org/10.1056/NEJMoa1606220
Chin JL, Billia M, Relle J, Roethke MC, Popeneciu IV, Kuru TH, Hatiboglu G, Mueller-Wolf MB, Motsch J, Romagnoli C, Kassam Z, Harle CC, Hafron J, Nandalur KR, Chronik BA, Burtnyk M, Schlemmer HP, Pahernik S (2016) Magnetic resonance imaging-guided transurethral ultrasound ablation of prostate tissue in patients with localized prostate cancer: a prospective phase 1 clinical trial. Eur Urol 70(3):447–455. https://doi.org/10.1016/j.eururo.2015.12.029
Burtnyk M, Hill T, Cadieux-Pitre H, Welch I (2015) Magnetic resonance image guided transurethral ultrasound prostate ablation: a preclinical safety and feasibility study with 28-day followup. J Urol 193(5):1669–1675. https://doi.org/10.1016/j.juro.2014.11.089
Chopra R, Burtnyk M, N’Djin WA, Bronskill M (2010) MRI-controlled transurethral ultrasound therapy for localised prostate cancer. Int J Hyperthermia 26(8):804–821. https://doi.org/10.3109/02656736.2010.503670
Partanen A, Yerram NK, Trivedi H, Dreher MR, Oila J, Hoang AN, Volkin D, Nix J, Turkbey B, Bernardo M, Haines DC, Benjamin CJ, Linehan WM, Choyke P, Wood BJ, Ehnholm GJ, Venkatesan AM, Pinto PA (2013) Magnetic resonance imaging (MRI)-guided transurethral ultrasound therapy of the prostate: a preclinical study with radiological and pathological correlation using customised MRI-based moulds. BJU Int 112(4):508–516. https://doi.org/10.1111/bju.12126
Siddiqui K, Chopra R, Vedula S, Sugar L, Haider M, Boyes A, Musquera M, Bronskill M, Klotz L (2010) MRI-guided transurethral ultrasound therapy of the prostate gland using real-time thermal mapping: initial studies. Urology 76(6):1506–1511. https://doi.org/10.1016/j.urology.2010.04.046
Sapareto SA, Dewey WC (1984) Thermal dose determination in cancer therapy. Int J Radiat Oncol Biol Phys 10(6):787–800
McDannold NJ, King RL, Jolesz FA, Hynynen KH (2000) Usefulness of MR imaging-derived thermometry and dosimetry in determining the threshold for tissue damage induced by thermal surgery in rabbits. Radiology 216(2):517–523. https://doi.org/10.1148/radiology.216.2.r00au42517
Bonekamp D, Wolf MB, Roethke MC, Pahernik S, Hadaschik BA, Hatiboglu G, Kuru TH, Popeneciu IV, Chin JL, Billia M, Relle J, Hafron J, Nandalur KR, Staruch RM, Burtnyk M, Hohenfellner M, Schlemmer HP (2018) Twelve-month prostate volume reduction after MRI-guided transurethral ultrasound ablation of the prostate. Euro Radiol 29:299–308. https://doi.org/10.1007/s00330-018-5584-y
National Cancer Institute; Common Terminology Criteria for Adverse Events (CTCAE) version 4.0; https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed 01.02.2019
Hadaschik BA, Kuru TH, Tulea C, Rieker P, Popeneciu IV, Simpfendorfer T, Huber J, Zogal P, Teber D, Pahernik S, Roethke M, Zamecnik P, Roth W, Sakas G, Schlemmer HP, Hohenfellner M (2011) A novel stereotactic prostate biopsy system integrating pre-interventional magnetic resonance imaging and live ultrasound fusion. J Urol 186(6):2214–2220. https://doi.org/10.1016/j.juro.2011.07.102
Klotz L, Penson D, Chin J, Pavlovich C, Relle J, Koch M, Hatiboglu G, Oto A, Futterer J, Raman SS, Lotan Y, Persigehl T, Heidenreich A, Suarez JF, Staruch R, Burtnyk M, Pantuck A, Sedelaar JP, Arora SS, Zagaja G, Tirkes T, Macura K, Bonekamp D, Haider M, Eggener S (2018) LBA20 MRI-guided transurethral ultrasound ablation (TULSA) in patients with localized prostate cancer: preliminary results of tact pivotal study. J Urol 199(4):e1077–e1078. https://doi.org/10.1016/j.juro.2018.03.091
Ganzer R, Robertson CN, Ward JF, Brown SC, Conti GN, Murat FJ, Pasticier G, Rebillard X, Thuroff S, Wieland WF, Blana A (2011) Correlation of prostate-specific antigen nadir and biochemical failure after high-intensity focused ultrasound of localized prostate cancer based on the stuttgart failure criteria—analysis from the @-Registry. BJU Int 108(8 Pt 2):E196–E201. https://doi.org/10.1111/j.1464-410X.2011.10091.x
Chen PY, Chiang PH, Liu YY, Chuang YC, Cheng YT (2018) Primary whole-gland ablation for localized prostate cancer with high-intensity focused ultrasound: the important predictors of biochemical recurrence. Int J Urol 25(6):615–620. https://doi.org/10.1111/iju.13581
Baumunk D, Andersen C, Heile U, Ebbing J, Cash H, Porsch M, Liehr UB, Janitzky A, Wendler JJ, Schindele D, Blaschke S, Miller K, Schostak M (2013) High-intensity focussed ultrasound in low-risk prostate cancer—oncological outcome and postinterventional quality of life of an inexperienced therapy centre in comparison with an experienced therapy centre. Aktuelle Urol 44(4):285–292. https://doi.org/10.1055/s-0033-1348253
Chaussy C, Thuroff S (2001) Results and side effects of high-intensity focused ultrasound in localized prostate cancer. J Endourol 15(4):437–440. https://doi.org/10.1089/089277901300189501
Crouzet S, Chapelon JY, Rouviere O, Mege-Lechevallier F, Colombel M, Tonoli-Catez H, Martin X, Gelet A (2014) Whole-gland ablation of localized prostate cancer with high-intensity focused ultrasound: oncologic outcomes and morbidity in 1002 patients. Eur Urol 65(5):907–914. https://doi.org/10.1016/j.eururo.2013.04.039
Netsch C, Pfeiffer D, Gross AJ (2010) Development of bladder outlet obstruction after a single treatment of prostate cancer with high-intensity focused ultrasound: experience with 226 patients. J Endourol 24(9):1399–1403. https://doi.org/10.1089/end.2009.0607
Ohigashi T, Nakamura K, Nakashima J, Baba S, Murai M (2007) Long-term results of three different minimally invasive therapies for lower urinary tract symptoms due to benign prostatic hyperplasia: comparison at a single institute. Int J Urol 14(4):326–330. https://doi.org/10.1111/j.1442-2042.2007.01692.x
Chopra R, Burtnyk M, Haider MA, Bronskill MJ (2005) Method for MRI-guided conformal thermal therapy of prostate with planar transurethral ultrasound heating applicators. Phys Med Biol 50(21):4957–4975. https://doi.org/10.1088/0031-9155/50/21/001
Steele GS, Sleep DJ (1997) Transurethral needle ablation of the prostate: a urodynamic based study with 2-year followup. J Urol 158(5):1834–1838
Gravas S, Laguna MP, de la Rosette JJ (2003) Efficacy and safety of intraprostatic temperature-controlled microwave thermotherapy in patients with benign prostatic hyperplasia: results of a prospective, open-label, single-center study with 1-year follow-up. J Endourol 17(6):425–430. https://doi.org/10.1089/089277903767923236
Vesely S, Knutson T, Dicuio M, Damber JE, Dahlstrand C (2005) Transurethral microwave thermotherapy: clinical results after 11 years of use. J Endourol 19(6):730–733. https://doi.org/10.1089/end.2005.19.730
Norby B, Nielsen HV, Frimodt-Moller PC (2002) Transurethral interstitial laser coagulation of the prostate and transurethral microwave thermotherapy vs transurethral resection or incision of the prostate: results of a randomized, controlled study in patients with symptomatic benign prostatic hyperplasia. BJU Int 90(9):853–862
Chaussy C, Thuroff S (2003) The status of high-intensity focused ultrasound in the treatment of localized prostate cancer and the impact of a combined resection. Curr Urol Rep 4(3):248–252
Funding
Profound Medical Inc. helped design and conduct the study, manage and analyze the data, and prepare and approve the manuscript.
Author information
Authors and Affiliations
Contributions
GH: project development, data collection, data analysis, manuscript writing and editing. VP: data collection, data analysis. DB: data collection, data analysis, manuscript writing and editing. MB: project development, data analysis, manuscript writing and editing. RS: project development, data analysis, manuscript writing and editing. SP: project development, data collection, data analysis. GT: data collection, data analysis. JPR: data analysis, manuscript writing and editing. JM: data collection, supervision. HPS: project development, supervision, critical revision of manuscript. MH: project development, manuscript writing and editing, supervision, critical revision of manuscript. JNN-D: data analysis, manuscript writing and editing, supervision, critical revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
R. Staruch and M. Burtnyk are employees of Profound Medical and receive a salary and stock options. The other authors declare, that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hatiboglu, G., Popeneciu, V., Bonekamp, D. et al. Magnetic resonance imaging-guided transurethral ultrasound ablation of prostate tissue in patients with localized prostate cancer: single-center evaluation of 6-month treatment safety and functional outcomes of intensified treatment parameters. World J Urol 38, 343–350 (2020). https://doi.org/10.1007/s00345-019-02784-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02784-w