Abstract
Purpose
Although the clinical significance of a diagnosis of prostate cancer for some men is debated, for many men it leads to significant morbidity and mortality. Radical treatment of clinically localized prostate cancer has been shown to improve survival in men with intermediate or high-risk disease. There is no high level evidence to support the superiority of radical prostatectomy, with or without adjuvant or salvage external beam radiotherapy in comparison to definitive radiotherapy with or without androgen deprivation, and the choice should be individualized. External beam radiation therapy practices are in constant evolution, and numerous strategies have been investigated to improve either efficacy or reduce toxicity, or both.
Methods
Randomized controlled trials investigating strategies to improve efficacy, reduce toxicity, or both of external beam radiotherapy have been reviewed in men with prostate cancer without nodal or distant metastases. These strategies include the use of neo-adjuvant and adjuvant androgen deprivation, dose-escalation, hypofractionation, whole pelvic radiation therapy, incorporation of improved imaging, image- guided radiation therapy, and adjuvant systemic therapy. The evidence to date for these strategies is discussed, noting limitations in applying the results of reported trials to men treated in contemporary settings.
Results
A number of strategies have shown improvements in biochemical control using external beam radiotherapy. To date, only with the use of androgen deprivation therapy has this translated into improvements in disease specific and overall survival. This may reflect the long natural history of prostate cancer and high incidence of competing risks. Technological advances have enabled dose escalation with reduced toxicity, of paramount importance given the long natural history.
Results
The use of external beam radiation therapy in prostate cancer is evolving with numerous strategies incorporated to improve outcomes. The optimum dose and fractionation and use of androgen deprivation or systemic adjuvants for each man is unclear based on current evidence and prognostic and predictive parameters. Patient preferences play an important role in chosen therapy. It is hoped that future studies better capture all prostate cancer- and treatment- related morbidity to clarify the optimal therapy choices for each man with prostate cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conflicting results from large randomized trials of PSA screening for prostate cancer have led to significant debate, not only about the value of screening, but about the value of treatments aimed to cure the disease [5, 132]. It is a common disease, being the second most frequently diagnosed cancer in men globally, with well over 1.2 million diagnosed in 2018 [19]. There is, however, significant debate about the clinical relevance for men of a diagnosis of prostate cancer. While it is commonly said that more men may die with prostate cancer than of prostate cancer, it is a heterogeneous disease, behaving very differently in different men. For many men, it causes significant morbidity or death and it therefore remains an important cause of morbidity and mortality globally, being the fifth most common cause of cancer death in men [19].
Much research has aimed to identify, for men diagnosed with prostate cancer that is localized to the prostate and seminal vesicles, the parameters that may predict the likelihood of significant morbidity or mortality. The most widely used risk stratification, suggests division into low, intermediate and high-risk groups according to these tumor factors (Table 1) [34, 58, 139]. More recently recognition of heterogeneity in outcomes in men within these risk groups has lead to further stratification. High-risk disease has been divided into localized and locally advanced cohorts in the EUA risk grouping shown as in Table 1 [106]. The NCCN guidelines divide low, intermediate and high risks further into very low, low, favorable intermediate, unfavorable intermediate, high and very high risk groups [109]. Additional factors such as PSA kinetics or PNI help to predict outcome [11, 31, 33]. For each man, consideration of these factors, in addition to patient factors, including estimates of life expectancy and comorbidities, allows some estimation of the likelihood of morbidity or mortality from prostate cancer, from which a decision can be made about whether attempts at curative treatment are justified.
The optimal curative treatment of clinically localized prostate cancer is unclear. Acceptable options include radical prostatectomy, external beam radiotherapy, interstitial brachytherapy, androgen deprivation therapy, combinations of these modalities, and active surveillance or watchful waiting (observation with treatment only for symptoms) [106, 130]. Radical prostatectomy, external beam radiotherapy and brachytherapy, with or without androgen deprivation therapy, are the potentially curative modalities. The most effective modality in terms of cure has not been established. Several randomized trials have aimed to measure the efficacy and toxicity of the different modalities. The early SPCG-4 randomized trial comparing radical prostatectomy with watchful waiting showed a significant improvement in overall survival, disease-specific survival and metastasis-free survival with surgery, but was conducted in an era prior to the widespread use of PSA, and thus its applicability to contemporary population of men with prostate cancer was questioned [13]. The survival benefit was largely limited to those men under 65 years of age. The subsequent PIVOT trial, also comparing radical prostatectomy with observation, was conducted in the PSA era. Although no significant difference was found in overall or prostate cancer specific survival with surgery for the entire randomized cohort, there was a reduction in the risk of bone metastases, and subset analysis identified improvements in survival in men with PSA > 10 and intermediate and high risk tumors [146]. Although these trials did not assess the efficacy of radiotherapy, they provide evidence that radical treatment can lower the risk of death or of developing metastases, particularly in men with intermediate and higher risk prostate cancer.
The recently published ProTECT trial randomized men with clinically localized prostate cancer to radical prostatectomy, external beam radiotherapy or monitoring [50]. After a median follow-up of 10 years, the risk of dying from prostate cancer was very low in all groups. Radical treatment reduced the risk of clinical progression, largely because of a reduction in the risk of metastases. Participants had predominantly low-risk prostate cancer. The median PSA under 5 ng/mL, over three quarters had a Gleason score of 6, and over three quarters had T1C disease. While this study provides justification for active surveillance, the results cannot be extrapolated to higher risk disease.
At the other end of the spectrum, locally advanced disease, defined variably although commonly accepted to describe cancer that has spread beyond the prostate capsule in the absence of clinically evident regional or distant spread, traditionally has been considered unsuitable for radical prostatectomy. Two randomized trials, outlined in Table 2 have shown a survival benefit with the addition of external beam radiation therapy to androgen deprivation compared with androgen deprivation alone [96, 143]. Both trials concluded that the combination of external beam radiotherapy and androgen deprivation should be the standard of care for locally advanced disease.
We therefore have evidence that for low-risk disease, radical treatment including RP and RT do not improve survival or reduce the risk of dying from prostate cancer compared with active surveillance. For locally advanced disease, RT improves prostate cancer specific and overall survival compared with ADT alone. For intermediate and high-risk clinically localized disease, PIVOT provides some evidence to support curative treatment, but for these men high quality randomized comparisons between surgery and radiotherapy are lacking. A number of non-randomized comparisons of surgery with external beam radiotherapy and brachytherapy have been published, and have suggested superior results for radical prostatectomy [25, 77, 134, 149]. Despite attempts to control for confounding variables, these cannot control for unknowns, including the absence of surgical staging of nodes in men receiving radiation therapy, and all comorbidities and competing risks.
Men who undergo radical prostatectomy who are found to have extracapsular extension, seminal vesicle invasion or positive surgical margins are at increased risk of recurrence, and post-operative radiotherapy has been used to reduce this risk. Three randomized trials to date have shown that adjuvant radiation therapy reduces the risk of biochemical failure [16, 140, 144]. Although the older SWOG 8794 trial found significant improvements in overall survival and metastasis-free survival, the more recent EORTC 22911 and ARO 96-02/AUO AP 09/95 trials did not, possibly reflecting effective salvage therapy for biochemical failure. There is no high-level evidence to support the superiority of a primarily surgical or radiation therapy approach. These modalities differ in the logistics of treatment, and their side effect profile, particularly if combined modality treatment is used, and both should be discussed. For each man, the choice will depend on personal consideration of relative benefits, logistics and potential side effects. Ideally treatment should be aimed at cure, with minimization of treatment related toxicity, and ideally with preservation of urinary continence and potency.
The different curative modalities cannot be compared on the basis of biochemical failure. The definition of biochemical failure definition differs following RP and RT, and ‘failure’ does not have the same implication in terms of subsequent risk of prostate cancer metastases or mortality. Traditionally, external beam radiotherapy trials have used the ASTRO definition of biochemical failure, defined as occurring after three consecutive rises in PSA after a nadir, with the date of failure being halfway between the nadir date and the first rise, or the initiation of salvage therapy [4]. This was of limited clinical relevance, correlating poorly with clinically relevant outcomes, largely due to backdating and sensitivity to the use of androgen deprivation. The RTOG-ASTRO Phoenix Consensus endorsed the adoption of the Phoenix definition of prostate cancer in 2005, defined by a rise of 2 ng/mL or more above the nadir PSA [127]. Although biochemical failure increases the risk of subsequent clinical failure, not all men who develop PSA failure will go on to develop metastases or die from prostate cancer, and there may be a significant lag between time PSA failure and metastases or death [27]. PSA is not a surrogate for prostate cancer death, and therefore, more clinically relevant outcomes are recommended [83]. As mentioned, given the variable and sometimes long natural history, long follow-up is necessary.
Although the more recently published trials have measured clinically relevant outcomes, including overall mortality, prostate cancer-specific mortality, metastasis-free survival, freedom from androgen deprivation, and comprehensive prospective assessment of toxicity and quality of life, there have been significant advances in both surgical techniques, and radiation therapy, which should be considered when applying the results of these studies to men presenting today. The strategies that have been investigated to improve outcomes with definitive external beam radiotherapy are the focus of this review.
Many strategies have been explored to improve the outcome for men undergoing external beam radiotherapy, aimed both at improving efficacy and the chance of cure or long-term growth restraint, and reducing the risk and severity of side effects. These include:
-
1.
Neoadjuvant and adjuvant androgen deprivation therapy (ADT).
-
2.
Dose-escalated radiation therapy (DERT).
-
3.
Increasing conformality.
-
(a)
CT planning—3D conformal radiotherapy (3DCRT).
-
(b)
Highly conformal techniques—IMRT, VMAT, HT.
-
(a)
-
4.
Incorporation of image guidance radiation therapy (IGRT).
-
5.
Rectal spacers.
-
6.
Whole pelvic radiation therapy (WPRT).
-
7.
Hypofractionation (HF).
-
8.
Extreme hypofractionation—SBRT.
-
9.
Incorporation of new imaging—MRI, PSMA.
-
10.
Adjuvant systemic therapy.
Androgen deprivation
Prostate cancer cell growth androgen dependence has been recognized since the work of Huggins and Hodges in the early nineteenth century [65]. It has been an effective therapy for metastatic disease for many decades. Based on its efficacy in the metastatic setting, and high rates of recurrence in localized disease with radiotherapy alone, ADT has been investigated with radiotherapy for localized disease. Neoadjuvant androgen deprivation has the potential to cytoreduce disease prior to treatment, and potentially reduces the volume needed to be treated. Preclinical studies suggest that neoadjuvant therapy may increase radiosensitivity by impairment of DNA repair, reducing the dose required for sterilization [48, 72, 117, 153]. Androgen deprivation may also act on microscopic metastatic disease. Numerous randomized trials have investigated the use of androgen deprivation therapy (ADT) in combination with radiotherapy to improve the chance of cure, either neoadjuvantly, or adjuvantly, the features of which are outlined in Table 3. The majority of these trials have been performed with doses of radiation that would be considered relatively low by current standards. To date, ADT is the only strategy which has resulted in convincing improvements in overall and disease-specific survival, without increasing radiation related toxicity. It is, however, associated with well-recognized toxicity.
Four randomized trials have compared radiotherapy alone with the use of short term neoadjuvant and concomitant ADT, showing improvements in prostate cancer-specific survival or overall survival [32, 42, 68, 124]. Three randomized trials have attempted to clarify the optimal duration of neoadjuvant ADT [26, 42, 116]. In TROG 96.10, 6 months of ADT resulted in improved overall and disease-specific survival compared with no ADT, whereas 3 months did not significantly improve outcomes compared with radiotherapy alone. In the study by Crook and colleagues, an improvement with longer duration of neoadjuvant therapy was only apparent in the subset with Gleason score of 8 or more. No clear benefit was seen with 4 months compared with 9 months in RTOG 99.10.
Three trials with predominantly high-risk participants have compared radiotherapy alone with radiotherapy and adjuvant ADT: RTOG 85.31 (median 2.2 years), EORTC 22863 (3 years), and EORTC 22991 (6 months) [15, 17, 115]. Although short-term ADT did not result in improved survival in EORTC 22991, longer term ADT (2 or 3 years) resulted in clear improvements in overall in RTOG 85.31 and EORTC 22863, with absolute improvements in 10-year survival of 10% and 18%, respectively. Subset analysis within RTOG 85.31 suggested improvements in survival were confined to the subset with Gleason score 8–10 tumors.
Three trials have assessed the effect of long term ADT when neoadjuvant therapy is given: RTOG 9202, TROG RADAR and DART [41, 61, 69, 89, 148]. TROG RADAR found improved prostate cancer-specific survival, and RTOG and DART both found significant improvements in overall survival. Importantly, men in DART were treated with dose-escalated radiation therapy, with a median dose of 78 Gy used. Most of the preceding trials used relatively low radiotherapy doses, and the effect of androgen deprivation in the setting of dose escalation was unknown.
Together the above trials support the use of neoadjuvant androgen deprivation for intermediate risk disease, and the addition of long-term androgen deprivation for high risk disease. Importantly, however, intermediate risk encompasses a heterogeneous group, and ongoing trials will be needed to identify those men for whom androgen deprivation is unlikely to be of benefit and toxicity can be avoided, either using traditional or novel parameters such as molecular profiling.
The optimal duration of ADT in men with high-risk disease is debated. Two randomized trials have compared different durations of adjuvant therapy. EORTC 22961 compared 6 months with 3 years of adjuvant therapy, and found that 3 years improved survival, with 5-year survival 85% versus 81%, suggesting that 6 months was insufficient [14]. In contrast PCS IV, which compared 36 months with 18 months of ADT after 4 months of neoadjuvant therapy found no difference in overall survival. It was, however, a superiority trial, and therefore not powered to confidently exclude inferiority of a shorter course [107].
ADT is associated with well-recognized toxicities, including reduced libido and sexual dysfunction, vasomotor symptoms, fatigue, cognitive effects, emotional effects, gynecomastia, reduced penile and testicular size, hair loss and osteoporosis. More recently, a number of studies have found an increased risk of metabolic syndrome with ADT, with an increased risk of diabetes and cardiovascular disease including myocardial infarction, heart failure and arrhythmias, cerebrovascular disease and venous thromboembolism [9, 18, 30, 52, 73, 79]. Some studies have suggested that the risks are increased only in those with preexisting cardiovascular disease [108, 112, 151]. Other studies have not identified significant increases. This may reflect differing relative risks in different patient populations, particularly in lower prostate cancer risk groups for whom ADT confers minimal benefit in terms of reducing prostate cancer death. Nguyen and colleagues performed a meta-analysis of randomized trials in men with unfavorable-risk prostate cancer, and found significant reductions in prostate cancer mortality and overall mortality, and no significant increase risk of cardiovascular mortality [110]. Despite conflicting results, there is sufficient evidence to suggest a possible increase in cardiovascular risk, and therefore for each man, baseline cardiovascular risk factors need to be considered, and weighed against the likelihood of benefit of ADT on prostate cancer morbidity and mortality. These risk factors should be monitored and managed in those men in whom ADT is initiated. There is no evidence to date that a particular intervention is indicated or will abrogate risk [92].
Dose escalation
Several randomized trials have sought to identify if an improvement in outcome can be achieved by increasing the radiotherapy dose. Prostate cancer is recognized as a relatively radio-resistant malignancy, and doses that can be given are influenced by the tolerance of adjacent normal structures, including the rectum and bladder, and prostatic urethra. Significant technical advances in radiation therapy delivery have enabled safe dose escalation to doses that are less commonly used in other tumor sites. Early radiotherapy to the prostate was delivered using estimations of prostate position based on information from plain X-ray based on correlation to bony landmarks or information from urethrography, and two-dimensional dose calculation. The introduction of 3D conformal radiotherapy was an initial advance. CT anatomical and tissue density information is incorporated for delineation of the target volume and organs and risk, 3D planning systems are used for dose calculation, and customized automated shielding using multi-leaf lead collimators within the treatment head of linear accelerators all allow reduction in the radiation field sizes with better targeting of tumor and lower doses to surrounding normal tissues. An early randomized trial showed the advantage of 3D conformal radiation therapy over 2D techniques in reducing the risk of late proctitis and bleeding, without a reduction in local control [40].
Subsequently, highly conformal techniques have been developed, including intensity modulated radiation therapy (IMRT), volumetric modulated arc therapy (VMAT) and helical tomotherapy (HT). All incorporate computer aided optimization or ‘inverse planning’ to enable greater conformality. IMRT and VMAT incorporate dynamic variation in dose intensity across beams. Concave dose distributions with steep dose gradients can be achieved. VMAT uses the same hardware (linear accelerators with multi-leaf collimators) with delivery of radiation therapy as the treatment head rotates about the patient, instead of using multiple static beams. HT uses different hardware resembling a CT scanner, with small fan beams delivering treatment while continuously rotating about the patient. These techniques have enabled higher doses to be given to the prostate and seminal vesicles, with the same or lower doses delivered to the rectum and bladder. Early non-randomized data showed that increases in dose up to 86.5 Gy could be achieved with 3D conformal radiation therapy and IMRT. Escalation of dose improved biochemical control, and the use of IMRT enabled this without increasing, or in fact reducing the risk of proctitis [150].
Several randomized trials have been published, all showing reductions in the risk of biochemical relapse with increased dose, a comparison of which is outlined in Table 4 [12, 39, 54, 81, 82, 100, 152]. The majority did not employ highly conformal techniques. In the MDACC trial, subset analysis identified reductions in clinical failure, distant metastases and death from prostate cancer in men with PSA > 10 ng/mL, or with high-risk features [81]. Apart from this subset analysis involving small numbers, none of the randomized trials have shown that improvements in biochemical control translate into an improvement in distant metastases, prostate cancer-specific survival or overall survival.
Kalbasi et al. published results of a retrospective, non-randomized comparative effectiveness study of DERT in men identified with the National Cancer Database (NCDB) [71]. It found that men with intermediate or high-risk disease had improved overall survival if they were treated with doses greater or equal to 75.6 Gy. The limitations of non-randomized trials apply, with multiple potential unknown confounders. A recent meta-analysis of the above randomized trials found significant relationship between dose and biochemical control in all risk groups, but no effect of dose on overall survival [147]. The lack of relationship between biochemical control and clinical failure or survival may be related to the prolonged lag time, effective use of secondary interventions, or competing risks.
The randomized trials of DERT have found increases in toxicity with dose escalation, however, all were conducted before the widespread use of highly conformal radiation techniques, or specified dose constraints for organs at risk. Toxicity outcomes from these trials have contributed to our understanding of dose and volume tolerances for bladder and bowel to keep toxicity acceptably low [1, 56, 114, 119]. Despite the lack of high-level evidence to show that DERT improves survival, based on improvements in biochemical failure, doses above 74 Gy are widely used, and recommended in guidelines [106]. With highly conformal techniques and attention to dose volume constraints for organs at risk, the risk of toxicity can be minimized.
An important consideration with the use of more conformal dose distributions with steep dose gradients and the use of small, tight margins to reduce the dose to the surrounding normal tissues is the risk of geographic miss, or missing the target. Two important advances have addressed this risk: the use of multiparametric MRI for accurate delineation of the prostate, seminal vesicle and organs at risk, and strategies addressing potential organ motion. Multiparametric MRI has contributed not only to better identification of high-risk lesions, but also risk group modification, with frequent upstaging of disease. It allows better identification of extracapsular extension or seminal vesicle invasion, but also better delineation of the prostate from the surrounding normal structures, allowing greater sparing of normal tissues [10, 101]. Accurate image registration with planning CT is essential to ensure these advantages can be realized.
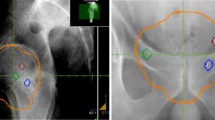
Image-guided radiation therapy (IGRT)
Numerous studies have identified and attempted to quantify interfraction and intrafraction motion of the prostate and seminal vesicles due to variations in bladder and bowel filling, and the implication of this on dose [28, 29, 78, 80, 85, 87, 113, 133, 138]. Failure to take prostate and seminal vesicle motion into consideration can compromise tumor control. A number of studies conducted prior to appreciation of organ movement have found higher relapse rates with more conformal techniques [55, 94]. Numerous studies have shown that increased rectal filling at the time of planning increases the risk of failure, presumably because the prostate moves posteriorly during the course of treatment [37, 57].
Appreciation of this movement has led to strategies to either limit movement, or accurately localize the prostate for treatment. Bowel and bladder protocols are used in an attempt to limit variation in bladder and bowel filling. Image guidance or image-guided radiation therapy (IGRT) is used to verify the position of the prostate for treatment. Various IGRT methods have been used, including the insertion of triangulated radiopaque intraprostatic fiducial markers into the prostate, transabdominal ultrasound, low dose cone-beam CT scans, insertion of electromagnetic transponders which may allow tracking or gating, or MRI guidance [35, 145]. Tight margins used in highly conformal techniques can only be used if accurate image guidance is employed [84]. Use of daily image guidance may negate the negative prognostic influence of rectal distention at the time of planning [86].
Brachytherapy boost for dose escalation
The randomized trials of dose escalation discussed above all use external beam radiation therapy alone. An alternative mean of escalating dose is with interstitial brachytherapy. Brachytherapy may be delivered either low dose rate (LDR) applications, delivered by permanent insertion of numerous radioactive seeds, including 125Iodine or 103Palladium seeds, or high dose rate applications, delivered using multiple fractions with temporary applicator placement and remote after loading with 192Iridium sources. The advantages of interstitial brachytherapy include the ability to deliver very high doses to the prostate with rapid fall off in dose, with low doses to the surrounding normal tissues, and the ability to overcome the problem of organ motion. Disadvantages include the need for specialized equipment and expertise, and operator dependence. The dose to peri-prostatic tissues, which may harbor microscopic disease, may be insufficient, and therefore it is usually used with external beam radiotherapy for men with intermediate or higher risk features. Not all men have suitable anatomy, and those with high IPSS scores are at higher risk of genitourinary toxicity.
Three randomized trials have reported outcomes of the use of a brachytherapy boost following external beam radiotherapy and are outlined in Table 5. Two relatively small randomized trials have examined the use of high dose rate brachytherapy with 192Iridium [36, 62]. Both identified improvements in biochemical control which have not translated into reductions in metastases or death. Both used suboptimal doses in the control arm by contemporary standards.
ASCENDE-RT is a recently published trial conducted in men with high and intermediate clinically localized prostate cancer. All men were to receive 12 months of neoadjuvant androgen deprivation, with whole pelvic radiotherapy to a dose of 46 Gy in 23 fractions given after 8 months. Men were randomized to receive a conformal external beam boost to 32 Gy in 16 fractions, or a LDR 125I implant to give a minimum peripheral dose of 115 Gy. After a median follow-up of 6.5 years, this has shown that the risk of biochemical failure is more than halved with an LDR boost [105]. No difference in overall survival, prostate cancer-specific or metastasis-free survival was identified. Importantly, LDR brachytherapy leads to significant increases in the risk of late genitourinary toxicity, with more men needing temporary catheterization and/or requiring incontinence pads. The 5-year cumulative incidence of ≥ grade 3 toxicity was 18.4% for LDR boost compared with 5.2% (P = 0.124) [128]. Patient-reported health-related quality of life assessments were performed, and identified more clinically significant declines in physical function and urinary function scales in the brachytherapy arm [129].
These trials highlight one of the major limitations of dose escalation alone. More conformal techniques with the use of image guidance enable dose escalation without increasing the dose to nearby rectum, and bowel toxicity may be stable. The prostatic urethra, however, is within the treatment volume, and dose escalation, regardless of the method, will increase its dose and therefore the risk of early and late genitourinary toxicity. Adjustments to seed or catheter placement may minimize the risk, but this may result in some tumor sparing.
An alternative mean of dose escalation that is enabled by newer technologies is partial organ or intra-lesional boosting, or dose-painting. Multiparametric MRI has enabled better delineation of tumor volume, and pathological studies have confirmed that local recurrences occur predominantly at the site of initial involvement [24]. FLAME is a recently published randomized trial examining this approach [103]. Between 2009 and 2015, 571 men with predominantly high risk disease with IPSS ≤ 20 and no TURP within 3 months were randomized to receive 77 Gy in 35 fractions with IMRT, with or without a boost to the tumor defined on multiparametric MRI of up to 95 Gy. Seminal vesicle dose was according to risk, 5–8 mm margins were used for the initial phase, and no margin for boost volume. ADT was permitted and given in 61%. With median follow-up of 4.6 years toxicity outcomes have been reported, showing an increase in the late ≥ Grade 2 GU toxicity, without an increase in GI toxicity. The urethra was not volumed and no dose constraints were specified. The primary outcome, biochemical failure, will be reported with longer follow-up.
With adequate image guidance and tight margins, and partial organ dose escalation, we may be able to avoid increasing rectal toxicity, but it is very difficult to escalate dose without treating prostatic urethra and trigone. These studies suggest that improving outcomes in prostate cancer will rely on more than just increasing the dose, and different approaches are needed to improve the therapeutic ratio. One such strategy aimed at reducing rectal toxicity that is currently under investigation is the insertion of a spacer, such as Space OAR® hydrogel between the prostate and rectum which can displace the anterior rectal wall outside the high dose region [102]. In a randomized trial with a median follow-up of 3 years, this has been shown to reduce the volume of rectum receiving high dose, and reduce late rectal toxicity and late quality of life declines [51, 95].
Hypofractionation
The above-mentioned trials have used conventional fractionation, with doses per fraction of 1.8–2 Gy. Conventional fractionation is based traditional understanding of the differences in radiobiological responses between most tumors, and late reacting normal tissues, which have a greater capacity to repair sub-lethal damage provided the dose per fraction is kept relatively low. These differences have been quantified by the α/β ratio, being 1-3 for late reacting normal tissues, and closer to 10 for tumors. Numerous investigators have proposed from equi-effective outcomes comparing different dose fractionation schedules that prostate cancer has an α/β ratio closer to 1.5, which is lower than that of nearby late reacting normal tissues [20, 43, 46, 75, 141]. Moderate hypofractionation with the use of larger doses per fraction may have greater biological effect on prostate cancer without increasing late toxicity. It may also significantly shorten the overall treatment time, currently 8–9 weeks for dose-escalated conventionally fractionated treatment.
Several randomized trials comparing moderate hypofractionation with conventional fractionation have been performed, and are compared in Table 6. The majority of participants are of low or intermediate risk. Three large randomized trials have recently reported 5–6-year follow-up. They have largely employed contemporary radiation therapy, with conformal techniques, central quality assurance of target coverage and organs at risk dose volume constraints, and image guidance for accuracy of delivery [23, 38, 91]. CHHIP and PROFIT used hypofractionated doses with similar EQD2 doses to conventionally fractionated control arms [23, 38]. Although both have shown an increase in acute gastrointestinal toxicity with hypofractionation, biochemical failure rates are similar, and there is no increase in late toxicity. Longer follow-up will be required to confirm these findings. Other randomized trials have assessed the effect of dose escalation with hypofractionation using higher EQD2 doses compared with the conventionally fractionated arms [6, 59, 66, 91, 118]. Although one trial found reduced biochemical failure with hypofractionation, the dose in the conventionally fractionated arm was relatively low [59]. Others have not identified reduced biochemical relapse, and importantly have found increased risk of late genitourinary or gastrointestinal toxicity [2, 3, 66, 91]. Sub-group analyses suggest that the risks of late toxicity can be minimized by patient selection and care with dose volume constraints [60, 118]. Only one trial included patients treated with pelvic nodal irradiation, treating just over 30% of participants who had high-risk disease. This was a risk factor for increased late genitourinary toxicity.
The above trials suggest that with modern radiotherapy techniques, using highly conformal techniques, using small margins and image guidance to ensure treatment accuracy and reduced dose to normal tissues, hypofractionated radiotherapy is effective with an acceptable toxicity profile, and allows a significant reduction in the overall treatment time, inconvenience and resource utilization. Bearing in mind that the larger contemporary trials report follow-up in the order of 5–6 years, and that < 20% of participants of the above trials had high risk disease, on the basis of the results reported to date, the most recent ASTRO/ASCO/AUA and AUA/ASTRO/SUO guidelines recommend that moderate hypofractionation be considered for men of any risk category who are suitable for radiotherapy [104, 130]. Although the different dose fractionations have not been compared, there is more evidence to support doses of 60 Gy in 20 fractions or 70 Gy in 28 fractions, with doses higher than these associated with greater late toxicity based on the above trials. Longer follow-up will be essential to determine the optimal fractionation, and whether efficacy and toxicity vary according to baseline characteristics.
Stereotactic radiation therapy
While the above trials have explored ‘moderate’ hypofractionation, there is interest in more extreme hypofractionation, referred to as stereotactic body radiation therapy (SBRT) or stereotactic ablative radiation (SABR). These involve the use doses per fraction closer to 6–9 Gy, with total EQD2 of 86-168 Gy, although the linear quadratic equation is unlikely to predict cell kill at such high doses per fraction [76]. It is thought that endothelial damage, and possibly immune effects contribute to the cell kill with these high doses per fractions [47]. Safe delivery of SBRT relies to an even greater degree on technological advances mentioned above, including highly conformal inverse planning techniques, improved imaging, image guidance and strategies to address intrafraction movement. Ideally additional incorporation of radiofrequency tracking technology, using implanted markers by which intrafraction movement can be monitored, is required. A number of investigators have published their experience, largely with low or intermediate risk disease, suggesting lower biopsy positivity and PSA nadirs, but with increases in GU and GI toxicity [93]. There has been insufficient follow-up for mature biochemical failure outcomes. Until adequately powered randomized trials with sufficient follow-up are reported, SBRT should be considered investigational, and enrollment to clinical trials encouraged.
There is extensive interest in the use of SBRT in the treatment of oligometastatic prostate cancer. To date, this approach has proved feasible and safe when dose volume constraints are respected, and appears to delay time to salvage androgen deprivation treatment.
Whole pelvic radiation therapy (WPRT; elective nodal irradiation)
An additional strategy employed in an attempt to improve the chance of cure with external beam radiotherapy is elective nodal irradiation of pelvic nodes, or whole pelvic radiotherapy (WPR). There are a number of theoretical arguments to support the elective treatment of pelvic nodes. Surgical lymphadenectomy studies have identified microscopic, radiologically occult, nodal metastases, especially with higher risk tumors [22]. The Roach formula, (LNI risk = 2/3 PSA + [(GS-6) × 10]) based on PSA and Gleason score was validated on surgical series and stratifies men at low or high risk of nodal metastases [126]. Lymph node drainage studies reveal the wide drainage patterns of the prostate to pelvic nodal groups including external, internal and common iliac, obturator and presacral nodes [97]. The RTOG 9202 trial confirming improved survival with long-term androgen deprivation used whole pelvic radiotherapy [89]. Finally, patterns of failure studies after prostate and seminal vesicle only radiotherapy show high incidence of pelvic node recurrence, including in common iliac nodes [135].
There are, however, a number of arguments against elective pelvic nodal irradiation. Increasing the treated volume has the potential to increase toxicity. Treatment of the whole pelvis with 3D conformal radiotherapy includes large volume of small and large bowel. Highly conformal techniques allow significant reduction in dose to bowel [111, 142]. Many debate whether nodal metastases are curable with the doses of radiation that can be employed, even with additional androgen deprivation. Finally, three randomized trials, outlined in Table 7, have failed to reveal significant effects on biochemical failure, clinical failure or survival [7, 8, 88, 120, 125].
The early RTOG 77-01 included many men with lower risk disease, including those who were pathologically node negative. The subsequent RTOG 94-13 trial was conducted in men thought to be of high risk of lymph node metastases on the basis of Roach formula LN% greater than 15%. This was a 2 × 2 randomized trial, with randomization either to prostate/seminal vesicle radiation therapy (PORT) or WPRT, and randomization to 4 months of neoadjuvant or adjuvant androgen deprivation. Although the initial analysis after a median follow-up of almost 5 years found a significant reduction in biochemical failure with WPRT, no significant difference was evident on a subsequent analysis with longer follow-up. The initial analysis had suggested an interaction between the use of WPRT and the timing and androgen deprivation, with significant reductions in failure in men receiving neoadjuvant hormones who receive WPRT compared with PORT. These differences did not remain significant with longer follow-up, and indeed the trial was not powered for comparison between the four treatment arms. The GETUG-01 was also negative, but also included many men of lower risk.
The failure to identify improvements in outcome with whole pelvic radiotherapy may be related to poor patient selection, inadequate coverage of nodes or inadequate dose. The use of highly conformal techniques necessitates accurate delineation of nodal locations at risk, and consensus guidelines have been published [53, 90]. There is ongoing debate about the adequacy of these volumes, with a recent MSKCC pattern of failure trial after prostate and seminal vesicle only found a high incidence of common iliac relapse [97].
There is concern that highly conformal dose distributions for pelvic nodes may lead to compromised coverage depending on the image guidance used. Image guidance is often based on the position of the prostate, rather than bony anatomy and pelvic nodal position. Despite this, studies suggest that the risk of failing to cover the nodal PTV due to image guidance based on fiducials is very low, although this would depend on margins used [44, 64].
The results of the ongoing RTOG 09-24, in men of moderate to high risk of recurrence, using contemporary radiotherapy techniques with IMRT, contemporary doses (to 79.2 Gy or brachytherapy implant) and 4, 6 or 32 months of androgen deprivation, and the UK prostate and pelvis versus prostate alone treatment for locally advanced prostate cancer (PIVOTAL) trial, a multicenter phase II trial, are eagerly awaited.
Although there is interest in hypofractionated whole pelvic radiotherapy, the above studies have used conventional fractionation [70]. Only the Italian randomized trial of hypofractionation used whole pelvic radiotherapy [6].
Adjuvant systemic therapy
An important reason for failure to cure prostate cancer with radiotherapy may be related to occult metastatic disease. As mentioned above, numerous studies have confirmed the benefit of the addition of ADT to radiation therapy, either because of a synergistic effect with increased radiosensitivity, or effects on micro-metastatic disease. A significant proportion of men with high-risk disease fail despite the use of DERT, neoadjuvant and long-term adjuvant ADT, and alternative strategies are required. A number of systemic agents have been investigated in an attempt to target occult metastatic disease. Based on its efficacy in the setting of metastatic castration-resistant prostate cancer (PRPC) in TAX 327 and subsequently in hormone naïve metastatic disease in CHAARTED and GETUG-AFU 15, docetaxel has been used earlier with radiation therapy and ADT with high risk, non-metastatic disease [49, 136, 137]. Four randomized trials are compared in Table 8 [45, 67, 74, 131]. Although STAMPEDE found an improvement in median survival with the addition of docetaxel, subset analysis did not show a benefit in the M0 subset. Longer follow-up is required to determine if there are significant improvements in survival that would justify the toxicity of docetaxel.
Newer agents, which act on the androgen receptor, such as enzalutamide, a potent androgen receptor inhibitor, are also being investigated, based on their activity in the metastatic setting, and more favorable side effect profile with randomized trials in progress.
Imaging advances
New staging imaging modalities such as positron emission tomography (PET) using prostate-specific membrane antigen (PSMA) ligands have shown promise in the detection of otherwise occult metastatic disease. Staging for metastatic disease for intermediate and high-risk men at initial presentation has traditionally included computed tomography (CT) scans of the abdomen and pelvis for detection of lymph node metastases, MRI for identification of local recurrence, and 99mTc bone scans for bony metastatic disease. The sensitivity and accuracy of CT, or MRI, for detection of lymph node involvement are low [21, 63]. While not yet widely available, the sensitivity, specificity and accuracy of PET imaging with PSMA ligands have been shown to be superior to morphological staging with CT or MRI using histopathological correlation of lymph node dissection [98, 99, 123], and superior to bone scan in the detection of bone metastasis, although histological confirmation of metastatic disease is often lacking [122]. Currently, early deaths in clinical trials may be the result of comorbid conditions or occult metastatic disease at presentation. More widespread use of accurate imaging for staging will better identify those with metastatic disease for whom radical local treatment will not be curative, and for whom alternative strategies are required, and those with truly localized disease for whom intensification of local therapy is justified. Improved staging will result in stage shifts that will need to be considered when comparing outcomes from contemporary series with historical controls.
Conclusion
Identifying the optimal treatment for each man with prostate cancer remains a significant challenge. Although some tumor and patient factors allow us to make some estimate of competing risks, prostate cancer behavior is heterogenous. For many men, prostate cancer has a long disease course. Identification of optimal treatment cannot rely on comparison of biochemical relapse alone. While it does provide an early marker of relapse, it is not a surrogate for prostate cancer morbidity, and provides no indicator of treatment-related morbidity. Reporting of toxicity outcomes has been incomplete and non-standardized, particularly for incontinence and sexual dysfunction. Given the long natural history of prostate cancer, efficacy and toxicity outcomes of randomized trials that have reported clinically relevant outcome data now will not have used currently available staging imaging investigations, and may have used radiation therapy techniques that do not reflect contemporary practice. For those for whom a decision to use definitive external beam radiotherapy is made, there are numerous strategies employed to optimize outcomes, either aimed at improving efficacy or reducing toxicity. The optimal strategy, or combination of strategies for each man is debatable, and hopefully will be elucidated with ongoing trials using not only efficacy outcomes and standardized toxicity measures, but patient-reported outcomes. In the meantime, presenting the different options and the evidence clearly to each man is important, if challenging, and will allow him to make an informed choice that takes into account his personal preferences.
References
Al-Mamgani A, Heemsbergen WD, Peeters STH et al (2009) Role of intensity-modulated radiotherapy in reducing toxicity in dose escalation for localized prostate cancer. Int J Radiat Oncol Biol Phys 73(3):685–691
Aluwini S, Pos F, Schimmel E et al (2015) Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (HYPRO): acute toxicity results from a randomised non-inferiority phase 3 trial. Lancet Oncol 16:274–283
Aluwini S, Pos F, Schimmel E et al (2016) Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (HYPRO): late toxicity results from a randomised, non-inferiority, phase 3 trial. Lancet Oncol 17:464–474
American Society for Therapeutic Radiology and Oncology Consensus Panel (1997) Consensus statement: guidelines for PSA following radiation therapy. Int J Radiat Oncol Biol Phys 37:1035–1041
Andriole GL, Crawford ED, Grubb RL, Buys SS et al (2009) Mortality results from a randomized prostate-cancer screening trial. N Engl J Med 360:1310–1319
Arcangeli G, Saracino B, Arcangeli S, Gomellini S, Petrongari MG, Sanguineti G, Strigari L (2017) Moderate hypofractionation in high-risk, organ-confined prostate cancer: final results of a phase III randomized trial. J Clin Oncol 35(17):1891–1897
Asbell SO, Krall JM, Pilepich MV et al (1988) Elective pelvic irradiation in stage A2, B carcinoma of the prostate: analysis of RTOG 77-06. Int J Radiat Oncol Biol Phys 15:1307–1316
Asbell SO, Martz KL, Shin KH et al (1998) Impact of surgical staging in evaluating the radiotherapeutic outcome in RTOG 77-06, a phase III study for T1BN0M0 (A2) and T2N0M0 (B) prostate carcinoma. Int J Radiat Oncol Biol Phys 40:769–782
Azoulay L, Yin H, Benayoun S, Renoux C, Boivin JF, Suissa S (2011) Androgen-deprivation therapy and the risk of stroke in patients with prostate cancer. Eur Urol 60(6):1244–1250
Barenttsz JO, Weinreb JC, Verma S et al (2016) Synopsis of the PI-RADS v2 guidelines for multiparametric prostate magnetic resonance imaging and recommendations for use. Eur Urol 69:41–49
Beard C, Schultz D, Loffredo M et al (2006) Perineural invasion associated with increased cancer-specific mortality after external beam radiation therapy for men with low and intermediate risk prostate cancer. Int J Radiat Oncol Biol Phys 66:403–407
Beckendorf V, Guerif S, Le Prise E, Cosset J-M, Bougnoux A et al (2011) 70 Gy versus 80 Gy in localized prostate cancer: 5 year results of GETUG 06 randomized trial. Int J Radiat Oncol Biol Phys 80(4):1056–1063
Bill-Axelson A, Holmberg L, Garmo H et al (2014) Radical prostatectomy or watchful waiting in early prostate cancer. NEJM 370:932–942
Bolla M, de Reijke TM, Van Tienhoven G et al (2009) Duration of androgen suppression in the treatment of prostate cancer. N Engl J Med 360(24):2516–2527
Bolla M, Maingnon P, Carrie C et al (2016) Short androgen suppression and radiation dose escalation for intermediate- and high-risk localized prostate cancer: results of EORTC Trial 22991. J Clin Oncol 34(15):1748–1756
Bolla M, van Poppel H, Tombal B et al (2012) Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer: long-term results of a randomised controlled trial (EORTC trial 22911). Lancet 380(9858):2018–2027
Bolla M, Van Tienhoven GV, Warde P et al (2010) External irradiation with or without long-term androgen suppression for prostate cancer with high metastatic risk: 10 years results of an EORTC randomised study. Lancet Oncol 11:1066–1073
Bosco C, Bosnyak Z, Malmberg A et al (2015) Quantifying observational evidence for risk of fatal and nonfatal myocardial cardiovascular disease following androgen deprivation therapy for prostate cancer: a meta-analysis. Eur Urol 68:386–396
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Brenner DJ, Martinez AA, Edmundson GK et al (2002) Direct evidence that prostate tumors show high sensitivity to fractionation (low alpha/beta ratio), similar to late-responding normal tissue. Int J Radiat Oncol Biol Phys 52:6–13
Briganti A, Abdollah F, Nini A et al (2012) Performance characteristics of computed tomography in detecting lymph node metastases in contemporary patients with prostate cancer treated with extended pelvic lymph node dissection. Eur Urol 61(6):1132–1138
Briganti A, Blute ML, Eastham JH et al (2009) Pelvic lymph node dissection in prostate cancer. Eur Urol 55:1251–1265
Catton C, Lukka H, Gu C-S, Martin J, Supiot S, Chung PW, Bauman GS et al (2017) Randomized trial of a hypofractionated radiation regimen for the treatment of localized prostate cancer. J Clin Oncol 35(17):1844–1890
Chopra S, Toi A, Taback N et al (2012) Pathological predictors for site of local recurrence after radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys 82:e441–e448
Cooperberg MR, Vickers AJ, Broering JM, Carroll PR (2010) Comparative risk-adjusted mortality outcomes following primary surgery, radiation therapy, or androgen deprivation therapy for localized prostate cancer. Cancer 116:5226–5234
Crook J, Ludgate C, Malone S et al (2009) Final report of multicenter Canadian phase III randomized trial of 3 versus 8 months of neoadjuvant androgen deprivation therapy before conventional-dose radiotherapy for clinically localized prostate cancer. Int J Radiat Oncol Biol Phys 73(2):327
Crook JM, O’Callaghan CJ, Duncan G et al (2012) Intermittent androgen suppression for rising PSA level after radiotherapy. N Engl J Med 367:895–903
Crook JM, Raymond Y, Salhani D, Yang H, Esche B (1995) Prostate motion during standard radiotherapy as assessed by fiducial markers. Radiother Oncol 37:35–42
Curtis W, Khan M, Magnelli A, Stephans K, Tendulkar R, Xia P (2013) Relationship of imaging frequency and planning margin to account for intrafraction prostate motion: analysis based on real-time monitoring data. Int J Radiat Oncol Biol Phys 85:700–706
D’Amico AV, Denham JW, Crook J et al (2007) Influence of androgen suppression therapy for prostate cancer on the frequency and timing of fatal myocardial infarctions. J Clin Oncol 25(17):2420–2425
D’Amico AV, Manola J, Loffredo M et al (2004) 6-month androgen suppression plus radiation therapy vs radiation therapy alone for patients with clinically localized prostate cancer. JAMA 292:821–827
D’Amico AV, Renshaw AA, Cote K et al (2004) Impact of percentage of positive cores on prostate cancer specific mortality for patients with low or favourable-intermediate risk disease. J Clin Oncol 22:3726–3732
D’Amico AV, Renshaw AA, Sussman B, Chen MH (2005) Pretreatment PSA velocity and risk of death following external beam radiation therapy. JAMA 294:440–447
D’Amico AV, Whittington R, Malkowicz SB et al (1998) “Biochemical outcome after radical protatectomy, external beam radiotherapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280:969–974
Dang A, Kupelian PA, Cao M et al (2018) Image-guided radiotherapy for prostate cancer. Transl Androl Urol 7(3):308–320
Dayes IS, Parpia S, Gilbert J, Julian JA, Davis IR, Levine MN, Sathya J (2017) Long-term results of a randomized trial comparing iridium implant plus external beam radiotherapy with external beam radiation therapy alone in node-negative locally advanced cancer of the prostate. Int J Radiat Oncol Biol Phys 99(1):90–93
de Crevoisier R, Tucker SL, Dong L et al (2005) Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy. Int J Radiat Oncol Biol Phys 62:965–973
Dearnaley D, Syndikus I, Mossop H, Khoo V, Birtle A, Bloomfield D, Graham J, Kirkbridge P, Logue J, Malik Z et al (2016) Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol 17:1047–1060
Dearnaley DP, Jovic G, Syndikus I et al (2014) Escalated-dose versus control-dose conformal radiotherapy for prostate cancer: long term results from the MRC RT01 randomised controlled trial. Lancet Oncol 15:464–473
Dearnaley DP, Khoo VS, Norman AR, Meyer L, Nahum A, Tait D, Yarnold J, Horwich A (1999) Comparison of radiation side-effects of conformal and conventional radiotherapy in prostate cancer: a randomised trial. Lancet 353:267–272
Denham JW, Joseph D, Lamb DS et al. (2014) Short-term androgen suppression and radiotherapy versus intermediate-term androgen suppression and radiotherapy, with or without zoledronic acid, in men with locally advanced prostate cancer (TROG 03.04 RADAR): an open-label, randomised, phase 3 factorial trial. Lancet Oncol 15(10):1076–1089
Denham JW, Steigler A, Lamb DS et al (2011) Short-term neoadjuvant androgen deprivation and radiotherapy for locally advanced prostate cancer: 10 year data from the TROG 96.01 randomised trial. Lancet Oncol 12(5):451–459
Duchesne GM, Peters LJ (1999) What is the alpha/beta ratio for prostate cancer? Rationale for hypofractionated high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys 44:747–748
Eminowicz G, Dean C, Shoffren O et al (2013) Intensity-modulated radiotherapy (IMRT) to prostate and pelvic nodes-is pelvic lymph node coverage adequate with fiducial-based image-guided radiotherapy. Br J Radiol 87:0696
Fizazi K, Faivre L, Lesaunier F et al (2015) Androgen deprivation therapy plus docetaxel and estramustine versus androgen deprivation therapy alone for high-risk localised prostate cancer (GETUG 12): a phase 3 randomised controlled trial. Lancet Oncol 16:787–794
Fowler J, Chappell R, Ritter M (2001) Is alpha/beta for prostate tumors really low? Int J Radiat Oncol Biol Phys 50:1021–1031
Garcia-Barros M, Paris F, Cordon-Cardo C et al (2003) Tumor response to radiotherapy regulated by endothelial cell apoptosis. Science 300:1155–1159
Goodwin JF, Sciewer MJ, Dean JL et al. (2013) A hormone-DNA repair circuit governs the response of genotoxic insult. Cancer Discovery 3(11):1254–1271
Gravis G, Boher JM, Joly F et al (2016) Androgen deprivation therapy (ADT) plus docetaxel versus ADT alone in metastatic non castrate prostate cancer: impact of metastatic burden and long-term survival analysis of GETUG-AFU15 trial. Eur Urol 70:256–262
Hamdy FC, Donovan JL, Lane JA et al (2016) 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. NEJM 375(15):1415–1424
Hamstra DA, Mariados N, Sylvester J et al (2017) Continued benefit to rectal separation for prostate radiation therapy: final results of a phase III trial. Int J Radiat Oncol Biol Phys 97(5):976–985
Haque R, Ulcickas Yood M, Xu X et al (2017) Cardiovascular disease risk and androgen deprivation therapy in patients with localised prostate cancer: a prospective cohort study. Br J Cancer 117(8):1233–1240
Harris V, Staffurth J, Esmail A et al (2015) Consensus guidelines and contouring atlas for pelvic node delineation in prostate and pelvic node intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys 92(4):874–883
Heemsbergen WD, Al-Magmani A, Slot A, Dielwart MFH (2014) Long-term results of the Dutch randomised prostate cancer trial: Impact of dose-escalation on local, biochemical, clinical failure, and survival. Radiother Oncol 110:1104–1109
Heemsbergen WD, Al-Magmani A, Witte MG, van Herk M, Lebesque JV (2013) Radiotherapy with rectangular fields is associated with fewer clinical failures than conformal fields in the high-risk prostate cancer subgroup: results from a randomized trial. Radiother Oncol 107:134
Heemsbergen WD, Al-Mamgani A, Witte MG et al (2010) Urinary obstruction in prostate cancer patients from the Dutch trial (68 Gy vs 78 Gy): relationships with local dose, acute effects, and baseline characteristics. Int J Radiat Oncol Biol Phys 78(1):19–25
Heemsbergen WD, Hoogeman MS, Witte MG, Peeters STH, Inroccic L, Lebesque JV (2007) Increased risk of biochemical and clinical failure for prostate cancer patient with a large rectum at radiotherapy planning: results from the Dutch trial of 68 Gy versus 78Gy. Int J Radiat Oncol Biol Phys 67(5):1418
Heidenreich A, Aus G, Bolla M et al (2008) EAU guidelines on prostate cancer. Eur Urol 53:68–80
Hoffman K, Voong R, Levy LB et al (2018) Randomized trial of hypofractionated, dose-escalated, intensity-modulated radiation therapy (IMRT) versus conventionally fractionated IMRT for localized prostate cancer. J Clin Oncol 36(29):2943–2949
Hoffman KE, Voong KR, Pugh TJ, Skinner H et al (2014) Risk of late toxicity in men receiving dose-escalated hypofractionated intensity modulated prostate radiation therapy: results from a randomized trial. Int J Radiat Oncol Biol Phys 88:1074–1084
Horwitz EM, Bae K, Hanks GE et al (2008) Ten-year follow-up of Radiation Oncology Therapy Group protocol 92-02: a phase III trial of the duration of elective androgen deprivation in locally advanced prostate cancer. J Clin Oncol 26:2497–2504
Hoskin P, Rojas AM, Bownes PJ, Lowe GJ, Ostler PJ, Bryant L (2012) Randomised trial of external beam radiotherapy alone or combined with high-dose-rate brachytherapy boost for localised prostate cancer. Radiother Oncol 103:217–222
Hovels AM, Heesakkers RA, Adang EM et al (2008) The diagnostic accuracy of CT and MRI in the staging of pelvic lymph nodes in patients with prostate cancer: a meta-analysis. Clin Radiol 63(4):387–395
Hsu A, Pawlicki T, Luxton G et al (2007) A study of image-guided intensity-modulated radiotherapy with fiducials for localized prostate cancer including pelvic nodes. Int J Radiat Oncol Biol Phys 68:898–902
Huggins C, Hodges CV (1941) Studies of prostatic cancer. The effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. J Urol 168:9–12
Incrocci L, Wortel RC, Alemayehu WG, Aluwini S, Schimmel E et al (2016) Hypofractionated versus conventionally fractionated radiotherapy for patients with localised prostate cancer (HYPRO): final efficacy results from a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol 17:1061–1069
James ND, Sydes MR, Clarke NW et al (2016) Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multi-stage, platform randomised controlled trial. Lancet 387:1163–1177
Jones CU, Hunt D, McGowan DG et al (2011) Radiotherapy and short-term androgen deperivation for localized prostate cancer. N Engl J Med 365(2):107–118
Joseph DJ, Lamb D, Denham JW et al (2018) Ten year final results of the TROG 03.04 (RADAR) randomised phase 3 trial evaluating duration of androgen suppression and zoledronate for locally advanced prostate cancer. J Clin Oncol 36(6 Suppl):1
Kaidar-Person O, Roach M 3rd, Crehange G (2013) Whole-pelvic nodal radiation therapy in the context of hypofractionation for high-risk prostate cancer patients: a step forward. Int J Radiat Oncol Biol Phys 86(4):600–605
Kalbasi A, Berman A, Swisher-McClure S et al (2015) Dose-escalated irradiation and overall survival in men with nonmetastatic prostate cancer. JAMA Oncol 1(7):897–906
Kaminski JML, Hanlon AL, Lim Joon D et al (2003) Effect of sequencing of androgen deprivation and radiotherapy on prostate cancer growth. Int J Radiat Oncol Biol Phys 57(1):24–28
Keating NL, O’Malley AJ, Smith MR (2006) Diabetes and cardiovascular disease during androgen deprivation therapy for prostate cancer. J Clin Oncol 24:4448–4456
Kellokumpu-Lehtinen P-LI, Hjalm-Eriksson M, Astrom L et al (2018) A randomized phase III trial between adjuvant docetaxel and surveillance after radical radiotherapy for intermediate and high risk prostate cancer. J Clin Oncol 36(Suppl 15):5000
King CR, Fowler JF (2001) A simple analytic derivation suggests that prostate cancer alpha/beta ratio is low. Int J Radiat Oncol Biol Phys 51:213–214
Kirkpatrick JP, Meyer JJ, Marks LB et al (2008) The linear quadratic model is inappropriate to model high dose per fraction effects in radiosurgery. Semin Radiat Oncol 18:240–243
Kishan AU, Cook RR, Ciezki JP et al (2018) Radical prostatectomy, external beam radiotherapy, or external beam radiotherapy with brachytherapy boost and disease progression and mortality in patients with Gleason score 9-10 prostate cancer. JAMA 319:896–905
Kitamura K, Shirato H, Seppenwoolde Y, Onimaru R, Oda M, Fujita K, Shimizu S, Shinohara N, Harabayashi T, Miyasaka K (2002) Three-dimensional intrafractional movement of prostate measured during real-time tumor-tracking radiotherapy in supine and prone treatment positions. Int J Radiat Oncol Biol Phys 53:1117–1123
Klil-Drori AJ, Yin H, Tagalakis V, Aprikian A, Azoulay L (2016) Androgen deprivation therapy for prostate cancer and the risk of venous thromboembolism. Eur Urol 70(1):56–61
Kotte AN, Hofman P, Lagendijk JJ, van Vulpen M, van der Heide UA (2007) Intrafraction motion of the prostate during external-beam radiotherapy: analysis of 427 patients with implanted fiducial markers. Int J Radiat Oncol Biol Phys 69:419–425
Kuban DA, Levy LB, Cheung MR et al (2011) Long-term failure patterns and survival in a randomized dose-escalation trial for prostate cancer. Who dies of disease? Int J Radiat Oncol Biol Phys 79(5):1310–1317
Kuban DA, Tucker SL, Dong L, Starkschall G, Huang EH, Cheung MR, Lee AK, Pollack A (2008) Long-term results of the M.D. Anderson randomized dose-escalation trial for prostate cancer. Int J Radiat Oncol Biol Phys 70(1):67–74
Kupelian PA, Buchsbaum JC, Patel C, Elshaikh M, Reddy CA, Zippe C, Klein EA (2002) Impact of biochemical failure on overall survival after radiation therapy for localized prostate cancer in the PSA era. Int J Radiat Oncol Biol Phys 52(3):704–711
Kupelian PA, Langen KM, Willoughby TR, Zeidan OA, Meeks SL (2008) Image-guided radiotherapy for localized prostate cancer: treating a moving target. Semin Radiat Oncol 18:58–66
Kupelian PA, Langen KM, Zeiden OA et al (2006) Daily variations in delivered doses in patients treated with radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 66:876–882
Kupelian PA, Willoughby TR, Reddy CA, Klein EA, Mahadevan A (2008) Impact of image guidance on outcomes after external beam radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 70(4):1146–1150
Langen KM, Willougby TR, Meeks SL, Santhanam A, Cunningham A, Levine L, Kupelian PA (2008) Observations of real-time prostate gland motion using electromagnetic tracking. Int J Radiat Oncol Biol Phys 71:1084–1090
Lawton C, Desilvio M, Roach M, Uhl V et al (2007) An update of the phase III trial comparing whole pelvic to prostate only radiotherapy and neoadjuvant to total androgen suppression: updated analysis of RTOG 94-13, with emphasis on unexpected hormone/radiation interactions. Int J Radiat Oncol Biol Phys 69(3):646–655
Lawton C, Lin X, Hanks G et al (2017) Duration of androgen deprivation in locally advanced prostate cancer: long term update of NRG Oncology RTOG 9202. Int J Radiat Oncol Biol Phys 98(2):296–303
Lawton CAF, Michalski J, El-Naq I, Buyyounouski MK et al (2009) RTOG GU Radiation Oncology Specialists reach consensus on pelvic lymph node volumes for high-risk prostate cancer. Int J Radiat Oncol Biol Phys 74(2):383–387
Lee WR, Dignam JJ, Amin MA, Bruner DW, Low D, Swanson GP, Shah AB, D’Souza DP, Michalski JM, Dayes IS, Seaward SA, Hall WA, Nguyen PL, Pisansky TM, Faria SL, Chen Y, Koontz BF, Paulus R, Sandler HM (2016) Randomized phase III noninferiority study comparing two radiotherapy fractionation schedules in patients with low-risk prostate cancer. J Clin Oncol 34(20):2325–2332
Levine GN, D’Amcio AV, Berger P et al (2010) Androgen deprivation therapy in prostate cancer and cardiovascular risk. A Science Advisory from the American Heart Association, American Cancer Society, and American Urological Association. Endorsed by the American Society for Radiation Oncology. CA Cancer J Clin 60:194–201
Loblaw A, Liu S, Cheung P (2018) Stereotactic ablative body radiotherapy in patients with prostate cancer. Transl Androl Urol 7(3):330–340
Marcello M, Ebert M, Haworth AM, Steigler A, Kennedy A, Joseph D, Denham J (2018) Association between treatment planning and delivery factors and disease progression in prostate cancer radiotherapy: results from the TROG 03.04 RADAR trial. Radiother Oncol 126:249–256
Mariados N, Sylvester J, Shah D, Karsch L et al (2015) Hydrogel spacer prospective multicenter randomized controlled pivotal trial: dosimetric and clinical effects of perirectal spacer application in men undergoing prostate image guided intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys 92(5):971–977
Mason MD, Parulekar WR, Sydes MR et al (2015) Final report of the Intergroup randomized study of combined androgen-deprivation therapy plus radiotherapy versus androgen-deprivation therapy alone in locally advanced prostate cancer. J Clin Oncol 33(19):2143–2149
Mattei A, Fueschel FG, Dhar NB et al (2008) The template of the primary lymphatic landing sites of the prostate should be revisited. Eur Urol 53:118–125
Maurer T, Gschwend JE, Rauscher I et al (2016) Diagnostic efficacy of gallium-PSMA Positron Emission Tomography compared to conventional imaging in lymph node staging of 130 consecutive patients with intermediate to high risk prostate cancer. J Urol 195(5):1436–1443
Maurer T, Weirich G, Schottelius M et al (2015) Prostate-specific membrane antigen-radioguided surgery for metastatic lymph nodes in prostate cancer. Eur Urol 68(3):530–534
Michalski JM, Moughan J, Purdy J, Bosch W, Bruner DW, Bahary J-P, Lau H, Duclos M, Parliament M, Morton G, Hamstra D, Seider M, Lock M, Patel M, Gay H, Vigneault E, Winter K, Sandler H (2018) Effect of standard vs dose-escalated radiation therapy for patients with intermediate-risk prostate cancer. The NRG Oncology RTOG 0126 Randomized Clinical Trial. JAMA Oncol (American Medical Association) 4(6):e180039
Moghanaki D, Turkbey B, Vapiwala N et al (2017) Advances in prostate cancer magnetic resonance imaging and positron emission tomography-computed tomography for staging and radiotherapy treatment planning. Semin Radiat Oncol 27:21–33
Mok G, Benz E, Vallee JP et al (2014) Optimization of radiation therapy techniques for prostate cancer with prostate-rectum spacers: a systematic review. Int J Radiat Oncol Biol Phys 90(2):278–288
Monninkof EM, van Loon JWL, van Vulpen M, Kerkmeijer LGW, Pos FJ, Haustermans K, van den Bergh L, Isebaert S, McColl GM, Smeenk RJ, Noteboom J, Walraven I, Peeters PHM, van der Heide UA (2018) Standard prostate gland radiotherapy with and without lesion boost in prostate cancer: toxicity in the FLAME randomized controlled trial. Radiother Oncol 127(1):74–80
Morgan SC, Hoffman K, Loblaw A et al (2018) Hypofractionated radiation therapy for localized prostate cancer: an ASTRO, ASCO, and AUA evidence based guideline. J Clin Oncol 36(34):3411–3430
Morris WJ, Tyldesley S, Rodda S, Halperin R, Pai H, McKenzie M, Duncan G, Morton G, Hamm J, Murray N (2017) Androgen Suppression Combined with Elective Nodal and Dose Escalated Radiation Therapy (the ASCENDE-RT Trial): an analysis of survival endpoints for a randomized trial comparing a low-dose rate brachytherapy boost to a dose-escalated external beam boost for high- and intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys 98(2):275–285
Mottet N, Bellmunt J, Bolla M, Briers E et al (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71:618–629
Nabid A, Carrier N, Martin A-G et al (2018) Duration of androgen deprivation therapy in high-risk prostate cancer: a randomized phase III trial. Eur Urol 74:432–441
Nanda A, Chen MH, Moran BJ et al (2014) Neoadjuvant hormonal therapy use and the risk of death in men with prostate cancer treated with brachytherapy who have no or at least a single risk factor for coronary artery disease. Eur Urol 65:177–185
National Comprehensive Cancer Network (2018) NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) Prostate Cancer. Version 4. https://wwwnccn.org/professionals/physician_gls/pdf/prostate.pdf. Accessed 9 Oct 2018
Nguyen RL, Je Y, Schutz FAB et al (2011) Association of andorgen deprivation therapy with cardiovascular death in patients with prostate cancer: a meta-analysis of randomized trials. JAMA 306(21):2359–2366
Nutting CM, Convery DJ, Cosgrove VP et al (2000) Reduction of small and large bowel irradiation using a optimized intensity-modulated pelvic radiotherapy technique in patients with prostate cancer. Int J Radiat Oncol Biol Phys 48:649–656
O’Farrell S, Gamo H, Holmberg L et al (2015) Risk and timing of cardiovascular disease after androgen-deprivation therapy in men with prostate cancer. J Clin Oncol 33(11):1243–1251
Padhani AR, Khoo VS, Suckling J, Husband JE, Leach MO, Dearnaley DP (1999) Evaluating the effect of rectal distension and rectal movement on prostate gland position using cine MRI. Int J Radiat Oncol Biol Phys 44:525–533
Peeters STH, Lebesque JV, Heemsbergen WD et al (2006) Localized volume effects for late rectal and anal toxicity after radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys 64(4):1151–1161
Pilepich MV, Winter K, Lawton CA et al (2005) Androgen suppression adjuvant to definitive radiotherapy in prostate carcinoma - long term results of phase III RTOG 85-31. Int J Radiat Oncol Biol Phys 61(5):1285–1290
Pisansky TM, Hunt D, Gomella LG et al (2015) Duration of androgen suppression before radiotherapy for localized prostate cancer: radiation Therapy Oncology Group Randomized Clinical Trial 9910. J Clin Oncol 33(4):332–339
Polkinghorn WR, Parker JS, Lee MX et al (2013) Androgen receptor signaling regulates DNA repair in prostate cancers. Cancer Discov 3(11):1245–1253
Pollack A, Walker G, Horwitz EM, Price R, Feigenberg S, Konski AA et al (2013) Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J Clin Oncol 31(31):3860–3868
Pollack A, Zagars GK, Starkschall G et al (2002) Prostate cancer radiation dose response: results of the M.D. Anderson phase III randomized trial. Int J Radiat Oncol Biol Phys 53:1097–1105
Pommier P, Chabaud S, Lagrange J, Richaud P, Le Prise E, Wagner J, Azria D, Beckendorf V, Suchaud J, Bernier V, Perol D, Carrie C (2016) Is there a role for pelvic irradiation in localized prostate adenocarcinoma? Update of the long-term survival results of the GETUG-01 randomized study. Int J Radiat Oncol Biol Phys 96(4):759–769
Pommier P, Chabaud S, Lagrange JL et al (2007) Is there a role for pelvic irradiation in localized prostate adenocarcinoma? Preliminary results of GETUG-01. J Clin Oncol 25(34):5366–5373
Pyka T, Okamoto S, Dahlbender M et al (2016) Comparison of bone scintography and 68 Ga-PSMA PET for skeletal staging in prostate cancer. Eur J Nucl Med Mol Imaging 43(12):2114–2121
Rauscher I, Maurer T, Fendler WP et al (2016) 68 Ga-PSMA ligand PET/CT in patients with prostate cancer: how we review and report. Cancer Imaging 16:14
Roach M 3rd, Bae K, Speight J et al (2008) Short-term neoadjuvant androgen deprivation therapy and external beam radiotherapy for locally advanced prostate cancer: long-term results of RTOG 8610. J Clin Oncol 26(4):585–591
Roach M 3rd, Desilvio M, Lawton C et al (2003) Phase III trial comparing whole-pelvic radiotherapy versus prostate-only radiotherapy and neoadjuvant versus adjuvant combined androgen suppression: radiation Therapy Oncology Group 9413. J Clin Oncol 21(10):1904–1911
Roach M 3rd, Marquez C, Yuo HS, Narayan P, Coleman L, Nseyo UA, Navvab Z, Carrol PR (1994) Predicting the risk of lymph node involvement using the pre-treatment prostate specific antigen and Gleason score in men with clinically localized prostate cancer. Int J Radiat Oncol Biol Phys 28(1):33–37
Roach M III, Hanks G, Thames H Jr et al (2006) Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: Recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys 65:965–974
Rodda A, Morris WJ, Hamm J, Duncan G (2017) ASCENDE-RT: an analysis of health-related quality of life for a randomized trial comparing low-dose-rate brachytherapy boost with dose-escalated external beam boost for high- and intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys 98(3):581–589
Rodda S, Tyldesley S, Morris WJ, Keyes M, Halperin R, Pai H, McKenzie M, Duncan G, Morton G, Hamm J, Murray N (2017) ASCENDE-RT: an analysis of treatment-related morbidity for a randomized trial comparing a low-dose-rate brachytherapy boost with a dose-escalated external beam boost for high- and intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys 98(2):286–295
Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, Freedland SJ, Greene K, Klotz LH, Makarov DV, Nelson JB, Rodrigues G, Sandler H, Taplin ME, Treadwell JR (2018) Clinically localized prostate cancer: aUA/ASTRO/SUO Guideline. Part II: Recommended approaches and detailed specific care options. J Urol 199:990–997
Sandler HM, Hu C, Rosenthal SA et al (2015) A phase III protocol of androgen suppression (AS) and 3DCRT/IMRT versus AS and 3DCRT/IMRT followed by chemotherapy (CT) with docetaxel and prednisone for localized, high-risk prostate cancer (RTOG 0521). J Clin Oncol 33(suppl 18):abstr LBA5002
Schroder FH, Hugosson J, Roobol MJ et al (2009) Screening and prostate-cancer mortality in a randomized European study. N Engl J Med 360:1320–1328
Shelton J, Rossi PJ, Chen H, Liu Y, Master VA, Jani AB (2011) Observations on prostate intrafraction motion and the effect of reduced treatment time using volumetric modulated arc therapy. Pract Radiat Oncol 1:243–250
Sooriakuman P, Nyberg T, Akre O, Haendler L, Heus I, Olsson M, Carlsson S, Roobol MJ, Steineck G, Wikland P (2014) Comparative effectiveness of radical prostatectomy and radiotherapy in prostate cancer: observational study of mortality outcomes. BMJ (Clinical Research Ed) 348:g1502
Spratt DE, Vargas HA, Zumsetg ZS et al (2017) Patterns of lymph node failure after dose-escalated radiotherapy: implications for extended pelvic node coverage. Eur Urol 71:37–43
Sweeney CJ, Chen YH, Carducci M et al (2015) Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med 373:737–746
Tannock IF, de Wit R, Berry WR et al (2004) Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 351:1502–1512
Byrne TE (2005) A review of prostate motion with considerations for the treatment of prostate cancer. Med Dosim 30:155–161
Thompson I, Thrasher JB, Aus G et al (2007) Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol 177(2007):2106–2131
Thompson IM, Tangen CM, Paradelo J et al (2006) Adjuvant radiotherapy for pathologically advanced prostate cancer. JAMA 296(19):1329–1335
Vogelius IR, Bentzen SM (2018) Dose response and fractionation sensitivity of prostate cancer after external beam radiation therapy: a meta-analysis of randomized trials. Int J Radiat Oncol Biol Phys 100(4):858–865
Wang-chesebro A, Xia P, Coleman J et al (2006) Intensity-modulated radiotherapy improves lymph node coverage and dose to critical structures compared with three-dimensional conformal radiotherapy in clinically localized prostate cancer. Int J Radiat Oncol Biol Phys 66:654–662
Widmark A, Klepp O, Solberg A, Damber J-E, Angelsen A, Fransson P, Lund J-A, Tasdemir I, Hoyer M, Wiklund F, Fossa SD, For the Scandinavian Prostate Cancer Group Study 7 and the Swedish Association for Urological Oncology 3 (2009) Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): and open randomised phase III trial. Lancet 373:301–308
Wiegel T, Bottke D, Steiner U et al (2009) Phase III postoperative adjuvant radiotherapy after radical prostatectomy compared with radical prostatectomy alone in pT3 prostate cancer with post-operative undetectable prostate-specific antigen: ARO 96-02/AOU AP 09/95. J Clin Oncol 27(18):2924–2930
Willougby TR, Kupelian PA, Pouliot J et al (2006) Target localization and real-time tracking using Calypso 4D localization system in patients with localized prostate cancer. Int J Radiat Oncol Biol Phys 65:528–534
Wilt TJ, Brawer MK, Jones KM et al (2012) Radical prostatectomy versus observation for localized prostate cancer. NEJM 367:203–213
Zaorsky NG, Keith SW, Shaikh T et al (2016) Impact of radiation therapy dose escalation on prostate cancer outcomes and toxicities. Am J Clin Oncol 41(4):409–415
Zapatero A, Guerrero A, Maldonado X et al (2015) High-dose radiotherapy with short-term or long-term androgen deprivation in localised prostate cancer (DART01/05 GICOR): a randomised, controlled, phase 3 trial. Lancet Oncol 16:320–327
Zelefsky MJ, Eastham JA, Cronin AM et al (2010) Metastasis after radical prostatectomy or external beam radiotherapy for patients with clinically localized prostate cancer: a comparison of clinical cohorts adjusted for case mix. J Clin Oncol 28:1508–1513
Zelefsky MJ, Fuks Z, Hunt M, Lee HJ, Lombardi D, Ling CC et al (2001) High dose radiation delivered by intensity modulated conformal radiotherapy improves the outcome of localized prostate cancer. J Urol 166(3):876–881
Ziehr DR, Chen MH, Zhang D et al (2015) Association of androgen-deprivation therapy with excess cardiac-specific mortality. BJU Int 116:358–365
Zietman AL, Bae K, Slater JD et al (2010) Randomized trial comparing conventional-dose with high-dose conformal radiation therapy in early-stage adenocarcinoma of the prostate: long term results from Proton Radiation Oncology Group/American College of Radiology 95-09. J Clin Oncol 28(7):1106–1111
Zietman AL, Nakfoor BM, Prince EA et al (1997) The effect of androgen deprivation and radiation therapy on an androgen-sensitive murine tumour: an in vitro and in vivo study. Cancer J Sci Am 3:31–36
Author information
Authors and Affiliations
Contributions
The author was solely responsible for the preparation of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflict of interest to declare.
Ethical standards
This review includes no person-level information and therefore no consent or ethical committee review was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Daly, T. Evolution of definitive external beam radiation therapy in the treatment of prostate cancer. World J Urol 38, 565–591 (2020). https://doi.org/10.1007/s00345-019-02661-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02661-6