Abstract
Objective
To compare the outcomes of robotic radical nephrectomy (RRN) to those of laparoscopic radical nephrectomy (LRN) for large renal masses.
Methods
This was a retrospective analysis of RRN and LRN cases performed for large (≥ cT2) renal masses from 2004 to 2017 and collected in the multi-institutional international database (ROSULA: RObotic SUrgery for LArge renal masses). Peri-operative, functional, and oncologic outcomes were compared between each approach. Descriptive analyses were performed and presented as medians with interquartile ranges. Inverse probability of treatment weighting-adjusted multivariable analyses were used to identify predictors of peri-operative complications. Kaplan–Meier analysis and Cox regression models were used to assess survival outcomes.
Results
A total of 941 patients (RRN = 404, LRN = 537) were identified. There was no difference in terms of gender, age, and clinical tumor size. Over the study period, RRN had an annual increase of 11.75% (95% CI [7.34, 17.01] p < 0.001) and LRN had an annual decline of 5.39% (95% CI [−6.94, −3.86] p < 0.001). Patients undergoing RRN had higher BMI (27.6 [IQR 24.8–31.1] vs. 26.5 [24.1–30.0] kg/m2, p < 0.01). Operative duration was longer for RRN (185.0 [150.0–237.2] vs. 126 [90.8–180.0] min, p < 0.001). Length of stay was shorter for RRN (3.0 [2.0–4.0] vs. 5.0 [4.0–7.0] days, p < 0.001). RRN cases presented more advanced disease (higher pathologic staging [pT3–4 52.5 vs. 24.2%, p < 0.001], histologic grade [high grade 49.3 vs. 30.4%, p < 0.001], and rate of nodal disease [pN1 5.4 vs. 1.9%, p < 0.01]). Surgical approach did not represent an independent risk factor for peri-operative complications (OR 1.81 95% CI [0.97–3.39], adjusted p = 0.2). The main study limitation is the retrospective design.
Conclusions
This study represents the largest known multi-center comparison between RRN and LRN. The two procedures seem to offer similar peri-operative outcomes. Notably, RRN has been increasingly utilized, especially in the setting of more advanced and surgically challenging disease without increasing the risk of peri-operative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical nephrectomy remains the standard of care for management of large renal tumors [1, 2]. The introduction of the laparoscopic approach has offered significant advantages over the open approach, mainly in terms of lower peri-operative morbidity and faster post-operative recovery. Nonetheless, the open approach has remained the preferred option in the setting of larger, locally advanced tumors with venous extension [3, 4]. Over the past decade, robotic surgery has been increasingly adopted in many urologic procedures including radical nephrectomy, as it can facilitate the surgeon in overcoming certain technical challenges and because of the steep learning curve of standard laparoscopy [5, 6].
Although studies have sought to evaluate robotic radical nephrectomy (RRN), few have adequately characterized and compared this technique with the established laparoscopic radical nephrectomy (LRN) [3, 7, 8]. In a recent large population-based study, Jeong et al. concluded that the use of robotic assistance for radical nephrectomy is not associated with increased risk of complications, but translates into prolonged operating time and higher hospital costs [3]. The findings of this study and its limitations have generated an ongoing debate [9, 10].
The aim of our study was to perform a comparative outcome analysis of RRN vs. LRN for large (≥ T2) renal masses in a “real-life” scenario using a large multi-institutional database.
Methods
Study design
We developed the multi-center, multi-national RObotic SUrgery for LArge (ROSULA) renal masses database involving 22 surgical centers worldwide. Using this database, we identified cases with ≥ cT2 renal masses [11] who underwent radical nephrectomy by a robotic-assisted or purely laparoscopic approach from 2004 to 2017. These cases were reviewed for baseline characteristics, peri-operative, and oncologic parameters.
Parameters
Baseline characteristics included age, gender, race, body mass index (BMI), American Society of Anesthesiologists (ASA) score; presence of diabetes mellitus, hypertension, or pre-operative chronic kidney disease (CKD) stage ≥ 3; pre-operative hemoglobin, estimated glomerular filtration rate (eGFR) [12], clinical tumor size, hilar location (determined by location within renal hilum and contact with hilar vessels on radiographic imaging) [13], tumor stage, nodal involvement, and metastasis.
Peri-operative variables included operative duration, estimated blood loss (EBL), intra-operative transfusions, intra-operative complications, 30-day post-operative complications (graded according to the Clavien–Dindo system with ≥ 3 considered major) [14], length of stay, change in hemoglobin at discharge, and change in eGFR at discharge.
Data analysis
In the first step of analyses, we evaluated rate of change in use of laparoscopic and robotic radical nephrectomy over time. Temporal trends were quantified using the estimated annual percentage change (EAPC).
In the second step of analyses, descriptive statistics including frequencies and proportions for categorical variables, means, medians, and ranges were reported for continuously coded variables. The Chi square tested the statistical significance in proportions’ differences. The t test evaluated for statistically significant differences between means.
In the third step of analyses, we relied on univariable and multivariable logistic regression models to test the effect of laparoscopic vs. robotic radical nephrectomy on any complication rates within the entire cohort of patients in whom radical nephrectomy was performed. An odds ratio (OR) was then determined for each significant factor.
In the fourth step of analyses, Kaplan–Meier (KM) plots graphically depicted the overall mortality and recurrence or metastasis-free survival rates after stratification according to laparoscopic vs. robotic radical nephrectomy within the cohort of patients with pT2M0 tumors. Then, a hazard ratio (HR) was derived using univariable and multivariable Cox regression models (CRMs) which were tested for differences in recurrence or metastases rates.
Covariates included in the multivariable models were those that were statistically significant in univariable models (p < 0.05). Moreover, to reduce the effect of selection bias, in multivariable models, we used a propensity score adjustment that relied on weighting based on inverse probability of treatment (IPTW) [15]. Since multiple different and independent hypotheses were tested, the Benjamini–Hochberg method was applied to control the false discovery rate for independent test statistics [16].
All tests were two-sided, and the level of significance was set at p < 0.05. Analyses were performed using the R software environment for statistical computing and graphics (version 3.5.0; http://www.r-project.org/).
Results
Baseline demographics
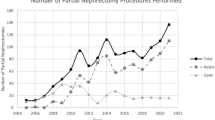
A cohort of 941 patients were identified as undergoing RRN (n = 404 [42.9%]) or LRN (n = 537 [57.1%]) for ≥ cT2 renal masses over the 14-year study period. Approximately, 2.8% (24/861) underwent a retroperitoneal surgical approach. An increasing number of robotic procedures were performed at participating centers with an EAPC of 11.75% (95% CI [7.34, 17.01] p < 0.001) for RRN and − 5.39% (95% CI [− 6.94, − 3.86] p < 0.001) for LRN (Fig. 1).
Patient demographics and baseline characteristics are listed in Table 1. Patients undergoing RRN had a higher median BMI compared to LRN (27.6 vs. 26.5 kg/m2, p < 0.01). There was no significant difference in terms of age, gender, or co-morbidities (hypertension or diabetes). However, nearly twice as many patients with CKD ≥ 3 underwent LRN compared to RRN (p < 0.01). There was no difference in clinical tumor size between groups (median 8.6 cm for RRN and 8.6 cm for LRN, p = 0.1). However, the robotic group included more metastatic patients (13.4% vs. 6.3%, p < 0.001) and had a higher proportion of masses with hilar location (27.5% vs. 10.4%, p < 0.001) (Fig. 2).
Peri-operative outcomes
Peri-operative outcomes are detailed in Table 2. Median operative duration was longer in RRN vs. LRN (185 vs. 126 min, p < 0.001). There was no significant difference in the median estimated blood loss and rate of intra-operative blood transfusion between the two approaches. Similarly, there was no significant difference in the overall rate of peri-operative complications between RRN (21.0%) vs. LRN (15.3%). Furthermore, there was no significant difference in the rate of major post-operative complications (Clavien grade ≥ 3) (3.5% vs. 1.9%).
Pathologic and oncologic outcomes
Approximately 97% of the clinical T2 masses demonstrated a malignant pathology, with no significant difference between RRN and LRN (Table 3). There was a higher rate of positive nodes among RRN vs. LRN (5.9% vs. 1.9%, p < 0.01). Subgroup analysis did not demonstrate a difference among groups comparing RRN vs. LRN approaches regarding rates of sarcomatoid differentiation (p = 0.6). However, RRN cases were found to have higher pathologic staging (p < 0.001), histologic grade (p < 0.001), and rate of positive surgical margin (p < 0.01).
Risk factors for peri-operative, surgical, and oncologic outcomes
At univariable analysis, BMI, ASA, pre-operative hemoglobin, pathologic stage, and hilar location were selected as potential factors in the occurrence of peri-operative complications (Table 4). On IPTW-adjusted multivariable analysis, BMI (OR = 1.06, 95% CI [1.02–1.12] p = 0.03), pre-operative hemoglobin (OR = 0.75, 95% CI [0.62–0.91] p = 0.003), and hilar location (OR = 1.89, 95% CI [1.00–3.56] p = 0.04) remained statistically significant predictors of peri-operative complications. However, only pre-operative hemoglobin remained significant after adjustment for multiple comparisons.
Variables assessed in the analysis of recurrence or metastasis are specified in Table 5. Positive surgical margins and all-cause mortality were not analyzed in the multivariable models due to the low number of events available.
Survival outcomes
Figure 3a, b demonstrates the Kaplan–Meier analyses for overall survival and disease-free survival. The median follow-up time was approximately 15 months for RRN and 20 months for LRN among malignant cases (p = 0.001) (Table 3). No difference was found in overall survival between groups (p = 0.06) (Fig. 3a); however, there was a higher disease-free survival among patients undergoing LRN (Fig. 3b).
On IPTW-adjusted CRM, surgical technique was not a risk factor for disease recurrence (Table 5).
Discussion
To the best of our knowledge, we report herein the largest multi-center comparison between RRN and LRN to date. Although multiple studies have compared open and laparoscopic radical nephrectomy approaches [17,18,19,20,21,22], few have comparatively investigated robotic and laparoscopic techniques, and none have exclusively examined large renal masses on such a considerable scale [3, 7, 23, 24]. Previous comparative studies in this field were done on population-based datasets, which carry some intrinsic limitations, such as the lack of a more granular analysis of outcomes [3]. Therefore, we believe that our study findings, based on real-life data, can fill an existing literature gap and fuel further critical discussion.
Over the past decade, robotic technology has been largely adopted for those major urologic procedures requiring “reconstructive” steps, primarily radical prostatectomy, but also partial nephrectomy and pyeloplasty [25]. On the other hand, its implementation for purely extirpative procedures, such as radical nephrectomy or adrenalectomy, has remained more limited given a debatable advantage over standard laparoscopy and concerns of higher costs [26].
First and foremost, it was interesting to note that over the 14-year study period an increasing number of robotic procedures were performed at participating centers. This mirrors findings from a recent trend analysis based on the Premier Health Care database, where Jeong et al. found that the use of robotic-assisted surgery was increased from 1.5% (39 of 2676 RN procedures in 2003) to 27.0% (862 of 3194 RN procedures) in 2015 (p < 0.001) [3].
In the current study, we found that patients undergoing RRN presented with higher BMI, higher rate of hilar tumors, and higher rate of metastatic disease and node involvement. Following resection, these patients were found to have a higher rate of positive margins as well as higher pathologic grade and stage. These differences suggest that surgeons used the robot to manage those bulkier, more complex tumors posing a higher level of surgical risk. Interestingly, Leow et al. identified a similar trend in a large comparative meta-analysis of nearly 5000 patients undergoing nephron-sparing surgery [27]. They discovered that the robotic approach was more often associated with larger and more complex renal tumors. RRN not only facilitates management of larger and higher stage tumors [28], but has also demonstrated the feasibility and safety of performing associated challenging procedures such as inferior vena cava thrombectomy, additional partial organ excision, or extensive dissection of retroperitoneal lymph nodes—procedures that otherwise would likely be performed via an open approach [29]. Taken together, these findings can be explained by the unique features of the robotic platform that allow for improved surgical dexterity, range of movement, three-dimensional visualization, tremor filtration, and motion scaling compared to pure laparoscopy [29].
Not surprisingly, the operative duration was significantly longer for RRN compared to LRN, with approximately 60 min in increased median operative time (p < 0.001). This difference can be in part explained by robot docking, and in part by the fact that robotic cases presented more advanced disease. In the study by Jeong et al., there was a higher rate of prolonged operating time (> 4 h) for patients undergoing RRN (46.3% vs. 25.8%; risk difference, 20.5%), and this difference partially accounted for the higher cost attributed to robotics [3]. Interestingly, our open conversion rates of 3% in RRN and 1.9% in LRN were significantly lower than the seemingly high rates identified by Jeong et al. (13.6% in RRN and 34.7% in LRN) [3]. This is likely attributable to our participating institutions being high volume referral centers with considerable minimal invasive surgery expertise compared to the national data set used by Jeong et al.
The nearly 20% peri-operative complication rate and 3% major complication rate were similar to previous studies characterizing minimally invasive radical nephrectomy [17, 23, 24, 30,31,32,33,34,35,36]. Interestingly, there was no significant difference between the two approaches regarding peri-operative complication rates, even after accounting for potential confounding variables. Moreover, in all our analyses we relied on IPTW adjustment to reduce the inherent selection bias within retrospective cohorts. Remarkably, results after IPTW adjustment were consistent with the results after multivariable adjustment only.
In the multivariable model, baseline patient characteristics, such as BMI, pre-operative hemoglobin levels, and hilar tumor location were found to be independent predictors of risk for peri-operative complications; however, only pre-operative hemoglobin levels remained significant after adjustment. The expected increased risk associated with decreased hemoglobin found in this study compares favorably with the increased risk of peri-operative blood transfusion, a peri-operative complication described by Abu-Ghanem et al. [37]. The analysis by Jeong et al. on a large health-care database also showed a similar rate of all post-operative complications and major complications, with no difference between surgical approaches [3]. Similarly, using SEER-Medicare data, Golombos et al. did not find any difference in major adverse events [38]. Also, Helmers et al. performed a single-center comparative analysis, and despite identifying higher rate of lymph node dissection, operative conversion, and EBL for RRN compared to LRN, they did not find differences in complication rates between approaches [7]. Nazemi et al. evaluated outcomes between open, laparoscopic, and robotic surgical approaches and reported similar median EBL, length of stay, and complication rates [8]. Although these studies offer details regarding patient and tumor characteristics, their limited sample size and single-center nature limit their generalizability.
The median hospital stay was shorter for RRN (3 versus 5 days; p < 0.001). Kates et al. also reported a shorter hospital stay for RRN compared with LRN (3.52 vs. 3.98, p = 0.049) in a cost analysis of hospital data from Maryland [39]. From a clinical standpoint, it is unlikely that the two procedures result in significant difference, and practice patterns at participating institutions might have contributed to this finding. However, it can be speculated that shorter hospital stay in the RRN group could have translated into a lower overall cost in our study population. Indeed, this topic deserves further investigation.
Given the limited available follow-up (median 15 and 20 months for RRN and LRN, respectively), an assessment of the oncologic outcomes did not represent a primary end point of our study. Additionally, the RRN group presented an overall higher positive margin rate (5.9% vs. 1.9%, p < 0.01). We suspect that this is likely to be related to the more advanced/progressed disease in that group; however, this could not be assessed with multivariable analysis due to the low number of these events available. Furthermore, after adjustment, surgical approach was not an independent predictive factor for disease recurrence.
Limitations of this study include its retrospective design; however, this was mitigated with use of IPTW. Although we did not assess the learning curve or surgeon/hospital experience, we adjusted our analysis for the year of surgery in an effort to address some of the disparities in surgeon expertise and practice patterns over time. As already mentioned, the median follow-up period in this study was relatively short and, consequently, further insight into valuable oncologic outcomes was necessarily limited. Finally, this study did not evaluate economic outcomes such as direct hospital costs and supply costs of these approaches which may represent a significant factor in adoption of surgical approach. In this regard, few studies have investigated this issue and have generally reported higher hospitals costs or charges for RRN, primarily using population-based analyses [3, 38,39,40]. However, a review of 150 nephrectomies from a single center revealed that RRN did not incur significantly higher costs than LRN if a robot was already available and fixed costs of the robot were excluded [41]. Additionally, decreased length of stay, which was observed here among RRN in our series, subsequently lowers the overall admission costs and thus may negate some of the higher costs associated with robotic surgery [3, 29]. Nevertheless, a specific cost analysis was beyond the scope of the current investigation. Certainly, this remains an issue requiring further scrutiny.
Conclusion
Herein, we report the largest known multi-center comparison between RRN and LRN. The present analysis of “real-life” data shows an increasing utilization of the robotic platform, which was associated with higher proportions of hilar and advanced tumors, with a similar morbidity profile to laparoscopic approach. The robotic approach may be a reasonable option for tumors, which may not have been tackled via minimally invasive surgery; however, further study comparing an open approach is necessary. In centers where robotic technology is available, RRN certainly represents an additional tool in the surgical armamentarium. Ideally, further investigation should be pursued within the framework of prospective randomized studies, incorporating a cost-effectiveness analysis.
References
Campbell S, Uzzo RG, Allaf ME, Bass EB, Cadeddu JA, Chang A, Clark PE, Davis BJ, Derweesh IH, Giambarresi L, Gervais DA, Hu SL, Lane BR, Leibovich BC, Pierorazio PM (2017) Renal mass and localized renal cancer: AUA guideline. J Urol 198(3):520–529. https://doi.org/10.1016/j.juro.2017.04.100
Ljungberg B, Bensalah K, Canfield S, Dabestani S, Hofmann F, Hora M, Kuczyk MA, Lam T, Marconi L, Merseburger AS, Mulders P, Powles T, Staehler M, Volpe A, Bex A (2015) EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol 67(5):913–924. https://doi.org/10.1016/j.eururo.2015.01.005
Jeong IG, Khandwala YS, Kim JH, Han DH, Li S, Wang Y, Chang SL, Chung BI (2017) Association of robotic-assisted vs laparoscopic radical nephrectomy with perioperative outcomes and health care costs, 2003 to 2015. JAMA 318(16):1561–1568. https://doi.org/10.1001/jama.2017.14586
Berger AD, Kanofsky JA, O’Malley RL, Hyams ES, Chang C, Taneja SS, Stifelman MD (2008) Transperitoneal laparoscopic radical nephrectomy for large (more than 7 cm) renal masses. Urology 71(3):421–424. https://doi.org/10.1016/j.urology.2007.10.057
Barbash GI, Glied SA (2010) New technology and health care costs–the case of robot-assisted surgery. N Engl J Med 363(8):701–704. https://doi.org/10.1056/NEJMp1006602
Klingler DW, Hemstreet GP, Balaji KC (2005) Feasibility of robotic radical nephrectomy–initial results of single-institution pilot study. Urology 65(6):1086–1089. https://doi.org/10.1016/j.urology.2004.12.020
Helmers MR, Ball MW, Gorin MA, Pierorazio PM, Allaf ME (2016) Robotic versus laparoscopic radical nephrectomy: comparative analysis and cost considerations. Can J Urol 23(5):8435–8440
Nazemi T, Galich A, Sterrett S, Klingler D, Smith L, Balaji KC (2006) Radical nephrectomy performed by open, laparoscopy with or without hand-assistance or robotic methods by the same surgeon produces comparable perioperative results. Int Braz J Urol 32(1):15–22
Lubin MA, Tewari A, Badani KK (2018) Robotic-assisted vs laparoscopic radical nephrectomy. JAMA 319(11):1165–1166. https://doi.org/10.1001/jama.2017.21860
Cacciamani GE, Desai MM, Gill IS (2018) A larger perspective study is needed when judging robotic radical nephrectomy. Eur Urol 74(1):123–124. https://doi.org/10.1016/j.eururo.2018.03.014
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474. https://doi.org/10.1245/s10434-010-0985-4
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, Ckd EPI (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Gill IS, Colombo JR Jr, Frank I, Moinzadeh A, Kaouk J, Desai M (2005) Laparoscopic partial nephrectomy for hilar tumors. J Urol 174(3):850–853. https://doi.org/10.1097/01.ju.0000169493.05498.c3 (discussion 853–854)
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46(3):399–424. https://doi.org/10.1080/00273171.2011.568786
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B (Methodol) 57(1):289–300
Bragayrac LA, Abbotoy D, Attwood K, Darwiche F, Hoffmeyer J, Kauffman EC, Schwaab T (2016) Outcomes of minimal invasive vs open radical nephrectomy for the treatment of locally advanced renal-cell carcinoma. J Endourol 30(8):871–876. https://doi.org/10.1089/end.2016.0082
Golombos DM, Chughtai B, Trinh QD, Thomas D, Mao J, Te A, O’Malley P, Scherr DS, Del Pizzo J, Hu JC, Sedrakyan A (2017) Minimally invasive vs open nephrectomy in the modern era: does approach matter? World J Urol 35(10):1557–1568. https://doi.org/10.1007/s00345-017-2040-6
Hemal AK, Kumar A, Kumar R, Wadhwa P, Seth A, Gupta NP (2007) Laparoscopic versus open radical nephrectomy for large renal tumors: a long-term prospective comparison. J Urol 177(3):862–866. https://doi.org/10.1016/j.juro.2006.10.053
Jeon SH, Kwon TG, Rha KH, Sung GT, Lee W, Lim JS, Jeong YB, Hong SH, Kim HH, Byun SS (2011) Comparison of laparoscopic versus open radical nephrectomy for large renal tumors: a retrospective analysis of multi-center results. BJU Int 107(5):817–821. https://doi.org/10.1111/j.1464-410X.2010.09688.x
Kercher KW, Heniford BT, Matthews BD, Smith TI, Lincourt AE, Hayes DH, Eskind LB, Irby PB, Teigland CM (2003) Laparoscopic versus open nephrectomy in 210 consecutive patients: outcomes, cost, and changes in practice patterns. Surg Endosc 17(12):1889–1895. https://doi.org/10.1007/s00464-003-8808-3
Liu G, Ma Y, Wang S, Han X, Gao D (2017) Laparoscopic versus open radical nephrectomy for renal cell carcinoma: a systematic review and meta-analysis. Transl Oncol 10(4):501–510. https://doi.org/10.1016/j.tranon.2017.03.004
Liu JJ, Leppert JT, Maxwell BG, Panousis P, Chung BI (2014) Trends and perioperative outcomes for laparoscopic and robotic nephrectomy using the National Surgical Quality Improvement Program (NSQIP) database. Urol Oncol 32(4):473–479. https://doi.org/10.1016/j.urolonc.2013.09.012
Hemal AK, Kumar A (2009) A prospective comparison of laparoscopic and robotic radical nephrectomy for T1-2N0M0 renal cell carcinoma. World J Urol 27(1):89–94. https://doi.org/10.1007/s00345-008-0321-9
Autorino R, Zargar H, Kaouk JH (2014) Robotic-assisted laparoscopic surgery: recent advances in urology. Fertil Steril 102(4):939–949. https://doi.org/10.1016/j.fertnstert.2014.05.033
Dobbs RW, Magnan BP, Abhyankar N, Hemal AK, Challacombe B, Hu J, Dasgupta P, Porpiglia F, Crivellaro S (2017) Cost effectiveness and robot-assisted urologic surgery: does it make dollars and sense? Minerva Urol Nefrol 69(4):313–323. https://doi.org/10.23736/S0393-2249.16.02866-6
Leow JJ, Heah NH, Chang SL, Chong YL, Png KS (2016) Outcomes of robotic versus laparoscopic partial nephrectomy: an updated meta-analysis of 4,919 patients. J Urol 196(5):1371–1377. https://doi.org/10.1016/j.juro.2016.06.011
Malthouse T, Hart A, Lam W, Kadirvelarasan A, Doeuk N, Challacombe B (2015) Robotic versus laparoscopic nephrectomy from a single centre: comparing apples with oranges? J Endourol 29:A240
Lam W, Chakravorty M, Challacombe B (2016) If the robot is there, why not use it? Why we should use the robot for laparoscopic nephrectomy. BJU Int 118(6):852–854. https://doi.org/10.1111/bju.13509
Pierorazio PM, Hyams ES, Lin BM, Mullins JK, Allaf ME (2012) Laparoscopic radical nephrectomy for large renal masses: critical assessment of perioperative and oncologic outcomes of stage T2a and T2b tumors. Urology 79(3):570–575. https://doi.org/10.1016/j.urology.2011.10.065
Gong EM, Lyon MB, Orvieto MA, Lucioni A, Gerber GS, Shalhav AL (2006) Laparoscopic radical nephrectomy: comparison of clinical Stage T1 and T2 renal tumors. Urology 68(6):1183–1187. https://doi.org/10.1016/j.urology.2006.08.1077
Steinberg AP, Finelli A, Desai MM, Abreu SC, Ramani AP, Spaliviero M, Rybicki L, Kaouk J, Novick AC, Gill IS (2004) Laparoscopic radical nephrectomy for large (greater than 7 cm, T2) renal tumors. J Urol 172(6 Pt 1):2172–2176
Bird VG, Shields JM, Aziz M, Ayyathurai R, De Los Santos R, Roeter DH (2009) Laparoscopic radical nephrectomy for patients with T2 and T3 renal-cell carcinoma: evaluation of perioperative outcomes. J Endourol 23(9):1527–1533. https://doi.org/10.1089/end.2009.0399
Rosoff JS, Raman JD, Sosa RE, Del Pizzo JJ (2009) Laparoscopic radical nephrectomy for renal masses 7 centimeters or larger. JSLS 13(2):148–153
Conley SP, Humphreys MR, Desai PJ, Castle EP, Dueck AC, Ferrigni RG, Andrews PE (2009) Laparoscopic radical nephrectomy for very large renal tumors (> or = 10 cm): is there a size limit? J Endourol 23(1):57–61. https://doi.org/10.1089/end.2008.0263
Hattori R, Osamu K, Yoshino Y, Tsuchiya F, Fujita T, Yamada S, Funahashi Y, Ono Y, Gotoh M (2009) Laparoscopic radical nephrectomy for large renal-cell carcinomas. J Endourol 23(9):1523–1526. https://doi.org/10.1089/end.2009.0393
Abu-Ghanem Y, Zilberman DE, Dotan Z, Kaver I, Ramon J (2018) Perioperative blood transfusion adversely affects prognosis after nephrectomy for renal cell carcinoma. Urol Oncol 36(1):12. https://doi.org/10.1016/j.urolonc.2017.09.006 (e15–12e20)
Golombos DM, Chughtai B, Trinh QD, Mao J, Te A, O’Malley P, Scherr DS, Del Pizzo J, Hu JC, Sedrakyan A (2017) Adoption of technology and its impact on nephrectomy outcomes, a U.S. population-based analysis (2008-2012). J Endourol 31(1):91–99. https://doi.org/10.1089/end.2016.0643
Kates M, Ball MW, Patel HD, Gorin MA, Pierorazio PM, Allaf ME (2015) The financial impact of robotic technology for partial and radical nephrectomy. J Endourol 29(3):317–322. https://doi.org/10.1089/end.2014.0559
Yang DY, Monn MF, Bahler CD, Sundaram CP (2014) Does robotic assistance confer an economic benefit during laparoscopic radical nephrectomy? J Urol 192(3):671–676. https://doi.org/10.1016/j.juro.2014.04.018
Abaza R, Gonsenhauser I, Box G, Sharp D, Sabsigh A (2015) Robotic nephrectomy is not costlier than standard laparoscopy when a robot is available. J Urol 193(4):e388
Author information
Authors and Affiliations
Contributions
Protocol/project development: RA, UAA, ID, FP. Data collection or management: UAA, MCM, NL, AM, KC, CF, JS, WW, GQ, AB, AA, FB, CZ, AL, PK, ML. Data analysis: UAA, MM. Manuscript writing: RA, UAA, ID. Manuscript editing: BY, GS, RGU, CL, MCM, UC, JP, AM, WW, SP, LS, MG, MR-B, CPS, AM, AK, KHR, PD, BC, LJH, FP, MA.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Research involving human participants and/or animals
The ROSULA database is an IRB-approved study at the participating centers.
Informed consent
Patients included in this retrospective analysis had signed an informed consent at the time of surgery.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anele, U.A., Marchioni, M., Yang, B. et al. Robotic versus laparoscopic radical nephrectomy: a large multi-institutional analysis (ROSULA Collaborative Group). World J Urol 37, 2439–2450 (2019). https://doi.org/10.1007/s00345-019-02657-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02657-2