Abstract
Objective
To evaluate whether elderly patients aged ≥ 75 years with locally advanced prostate cancer (LAPC) may benefit from local treatment (LT).
Methods
Elderly patients aged ≥ 75 years with non-metastatic cT3–4 LAPC who were treated with LT [radical prostatectomy (RP), radiation therapy (RT)] or non-LT (NLT) were identified. After propensity score matching (PSM), cancer-specific mortality (CSM) and other-cause mortality (OCM) rates were assessed. In the assessment of LT vs. NLT and RP vs. RT, multivariable competing risk regression (MVA CRR) analysis was used.
Results
368 and 482 paired patients were matched for LT vs. NLT and RP vs. RT, respectively. 5 and 10 years CSM rates were 9.4 vs. 18.5% in LT and 24.9 vs. 29.3% in NLT-treated patients, respectively (P < 0.0001). 5 and 10 years CSM rates were 3.4% vs. 8.6% in RP and 6.7% vs. 15.1% in RT-treated patients, respectively (P = 0.10). In the MVA CRR model, after PSM, NLT resulted in higher CSM rates in Gleason score 8–10 [subhazard ratio (sHR) = 2.83, P < 0.001], cT3b/4 (sHR = 3.97/2.56, P = 0.003/0.002), cN0 (sHR = 2.52, P < 0.001) or PSA > 10 ng/ml [sHR (PSA = 10.1–20 ng/ml) = 4.59, P = 0.03; sHR (PSA > 20 ng/ml) = 2.77, P = 0.001] patients compared with LT. However, no statistically significant difference in CSM was observed between RP and RT, except for cT3a patients in whom higher CSM rates were noted for RT compared with RP (sHR = 3.91, P = 0.02).
Conclusion
LAPC patients may benefit from local treatment despite advanced age. However, this benefit was only seen in patients with cT3b/4, Gleason score 8–10, cN0 or PSA > 10 ng/ml.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recommendations of treatment for elderly patients with locally advanced prostate cancer (LAPC) are vague. To date, two large randomized clinical trials (RCTs) have shown the superiority of radiation therapy (RT) combined with androgen deprivation therapy (ADT) over ADT alone in LAPC patients [1, 2]. However, one trial excluded patients over 75 years, and the other excluded patients over 80 years. To the best of our knowledge, no RCT was ever published evaluating the role of radical prostatectomy (RP) in the treatment of LAPC. Some observational studies tried to shed light on this issue [3,4,5,6,7]. The vast majority of studies published showed favorable results for RP in the treatment of LAPC; these data were derived from uncontrolled studies. In addition, patients aged ≥ 75 years were poorly represented. Hence, it is difficult to speculate the effectiveness of local treatment (LT) in the contemporary elderly patients aged ≥ 75 years with LAPC.
In view of this, we aimed to assess the cancer-specific mortality (CSM) in elderly patients aged ≥ 75 years, who were diagnosed with LAPC (cT3–T4, M0) and were treated with LT vs. non-LT (NLT) as initial therapy. Additionally, we performed an exploratory analysis to determine if there was a difference in outcomes between RP and RT.
Patients and methods
Study population
Within the Surveillance, Epidemiology, and End Results (SEER) database (18 cancer registries, accounting for 26% of the US population, 2004–2014), patients diagnosed with histologically confirmed adenocarcinoma of the prostate [International Classification of Disease for Oncology (site code: 61.9); histological code: 8140] were identified. Other inclusion criteria were: (1) age ≥ 75 years; (2) clinical stage T3–T4 or/and N+, M0 [sixth edition of American Joint Committee on Cancer (AJCC) Cancer Staging Manual]; (3) patients who chose RP (surgery site codes: 50 and 70), RT (external beam radiotherapy; radiation-specific codes: 1 and 4) or NLT (no surgery or radiation therapy) as initial treatment. Exclusion criteria were: (1) patients who chose surgery other than RP, for example, transurethral resection of the prostate; (2) patients treated with both RP and RT; (3) patients who chose brachytherapy as first therapy; (4) patients diagnosed by autopsy or death certificate only; (5) patients who have not done PSA test or Gleason score analysis; (6) patients with incomplete dates of follow-up. The patient selection and exclusion process is described in supplementary Fig. 1. CSM was defined according to the SEER mortality code (code 28010). All other competing deaths were considered as other-cause mortality (OCM). In addition, newly validated prostate-specific antigen (PSA) data were also included in the analysis [8].
Covariates and study outcomes
Race, age at diagnosis, marital status, PSA value, Gleason score and clinical T and N stages were selected as covariates. Primary outcome was the CSM rate in LT- and NLT-treated patients. Secondary outcome was the CSM rate in RP- and RT-treated patients. Patients who died due to other causes were included in the OCM rate [9].
Statistical analyses
Mean, median and interquartile ranges were reported for the continuous variable. Frequency and proportion were reported for the categorical variable. Mann–Whitney U test and Pearson x2 test or Fisher’s exact test were used to compare means and proportions, respectively.
Propensity score matching methods [1:1 ratio, using nearest neighbor matching method, with a maximum tolerated difference (caliper) of 0.005; MatchIt package in R] were used before analysis to balance covariates in control and treatment groups, thus reducing possible bias [10].
According to treatment type, patients were categorized into two comparison groups: LT vs. NLT and RP vs. RT. Cumulative incidence rates (CSM rate and OCM rate) were obtained and compared using the Gray test for each treatment group [11]. Multivariable competing risk regression (MVA CRR) analysis was performed to compare CSM rates in each comparison group (LT vs. NLT and RP vs. RT) after accounting for confounders.
All statistical tests were two-sided, and statistical significance was defined as P < 0.05. Analyses were performed using the R statistical package (version 3.3.0; the R foundation for Statistical Computing, Vienna, Austria).
Results
Demographic and clinical characteristics
Overall, 2796 elderly patients (≥ 75 years) diagnosed with LAPC (cT3–T4, M0) were identified. Among them, 2145 patients were treated with LT (1210 with RP, 935 with RT) and 651 patients were treated with NLT. Median age was 77 years [interquartile range (IQR) 76–80] in the LT group and 82 years (IQR 78–86) in the NLT group. In RP and RT cohorts, median age was 78 years (IQR 76–81) and 76 years (IQR 75–78), respectively. After dividing age into two categories, the highest rate for the group older than 80 years was found in NLT-treated patients (65.3%); followed by patients treated with RT (37.8%) and RP (15.2%). Most patients in both groups were Caucasian. After categorizing patients by each year, over time, the rate for the number of cases was decreasing in NLT group (9.8–6.8% from 2004 to 2014) and increasing in RP group (5.1–10.8% from 2004 to 2014), whereas, relatively stable in RT group. The rate of biopsy Gleason score 8–10 was highest in the NLT group (64.7%), followed by the RT (64.6%) and RP (37.2%) group. The same situation occurred in the rate for T4 and PSA > 20 ng/ml patients, with the highest rate detected in the NLT group (48.2% for T4; 48.1% for PSA > 20 ng/ml), followed by the RT (13.5% for T4; 29.5% for PSA > 20 ng/ml) and the RP (7.4% for T4; 8.1% for PSA > 20 ng/ml) group. The highest rate for cN1 was found in the RP group (12.0%), followed by NLT (11.7%) and RT (6.5%) group. The details are depicted in Tables 1 and 2.
Propensity score matching
Before propensity score matching, all demographic and clinical characteristics were significantly different in each comparison group. After propensity score matching, 368 and 482 paired patients were matched for NLT vs. LT and RP vs. RT, respectively (Tables 1, 2). No significant difference was found for every covariate in each comparison group after matching, except for the “year of diagnosis” in NLT vs. LT cohorts (P = 0.05; Table 1). Jitter plots for each PSM are shown in supplementary Figs. 2 and 3, respectively.
Survival analyses
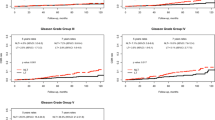
LT vs. NLT
Overall, 5 and 10 years CSM rates were 9.4 vs. 18.5% in LT and 24.9 vs. 29.3% in NLT-treated patients, respectively (Fig. 1a; P < 0.0001). The absolute risk reductions were 15.5 and 10.8% at 5 and 10 years, respectively. The OCM rates at 5 and 10 years were 25.1 vs. 56.6% in LT and 31.1 vs. 58.4% in NLT-treated patients, respectively (Fig. 1b; P = 0.09).
In the MVA CRR model, patients with NLT had a 2.66-fold higher probability of dying from prostate cancer (PCa) compared to those treated with LT (Table 3; P < 0.001). Specifically, NLT resulted in higher CSM rates in Gleason score 8–10 [subhazard ratios (sHR) = 2.83, confidence interval (CI) 1.77–4.53, P < 0.001], cT3b/4 (sHR = 3.97/2.56, 95% CI 1.58–9.98/1.49–4.94, P = 0.003/0.002), cN0 (sHR = 2.52, 95% CI 1.58–4.03, P < 0.001) or PSA > 10 ng/ml [sHR (PSA = 10.1–20 ng/ml) = 4.59, 95% CI 2.57–6.25, P = 0.03; sHR (PSA > 20 ng/ml) = 2.77, 95% CI 1.23–4.12, P = 0.001] patients compared with LT.
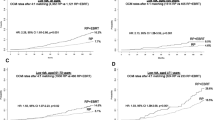
RP vs. RT
5 and 10 years CSM rates were 3.4 vs. 8.6% in RP and 6.7 vs. 15.1% in RT-treated patients, respectively (Fig. 2a; P = 0.10). 5 and 10 years OCM rates were 12.3% vs. 37.4% in RP and 17.1 vs. 45.3% in RT-treated patients, respectively (Fig. 2b; P = 0.10).
In the MVA CRR model, no statistically significant difference was found between RP and RT cohorts with regard to CSM rates, except for T3a patients in whom higher CSM rates were noted for RT compared with RP (sHR = 3.91, 95% IC 1.99–5.23, P = 0.02; Table 3).
Discussion
Treatment of LAPC has been a controversial topic in recent decades. No general consensus concerning the most appropriate treatment options was ever reached. This is especially true in elderly patients. Elderly patients are more prone to presenting with advanced diseases; have a greater risk of death from PCa compared with the younger counterparts (age < 75 years; [12]). This makes planning of treatment much more complex. To date, RT combined with ADT is still regarded as a cornerstone treatment providing one of the most efficient multimodality therapies compared with either monotherapy in the treatment of LAPC. This has already been verified by two landmark RCTs [1, 2]. However, studies regarding to a treatment strategy for elderly patients aged ≥ 75 years with LAPC are still lacking.
The role of RP as one of the primary LT treatment options is controversial in the treatment of LAPC. Several observational studies reported a high risk of relapse and clinical progression after RP in patients with LAPC [13, 14]. This is probably the main reason for the limited application of surgery in these patients. Nevertheless, an increasing number of studies showed favorable results in LAPC patients treated with RP [3,4,5,6,7]. In a previous SEER-based study, Giorgio et al. evaluated the survival benefit of RP in patients with cT3–T4 disease. They concluded that RP led to a significant survival advantage over observation group [15]. However, patients older than 80 years were excluded. Furthermore, the analysis was based on a relatively older database (1995–2009), which might not be fully applicable to the contemporary elderly patients.
In our analysis, some results were noteworthy. First, we identified some important differences in clinically relevant demographics between LT (RP and RT) and NLT cohorts. For instance, a shift of treatment modalities in each year, over time, we found that the rate for the number of cases was decreasing in NLT cohort and increasing in RP cohort, whereas, relatively stable in RT cohort. That means RP has been growing to play a more significant role in the contemporary treatment of elderly patients aged ≥ 75 years with LAPC. This trend is in line with another database study from Weiner et al., which showed the likelihood of receiving RP as primary therapy for high-risk PCa dramatically increased over time [16]. It also implied a notion that advanced age might not be a limiting factor for receiving RP in relatively healthy patients with LAPC as they might benefit. In a multi-institutional cohort study of 266 patients, it was reported that CSM rates did not differ among age groups even in LAPC (cT3b–4) patients with few comorbidities who were treated surgically, suggesting RP may be appropriate even at older age [5].
Second, a 15.5 and 10.8% overall CSM reduction at 5 and 10 years in the LT cohort compared with NLT cohort was observed. This suggests the potential benefit of LT for elderly patients aged ≥ 75 years with LAPC. However, no significant difference was found between RP and RT cohorts. These results match with those of the study from Stephen et al., which showed that there was no significant difference in CSM between RP and RT in the treatment of high-risk PCa, despite younger participants and lower rates of more advanced disease were included in their study [17].
Third, in the MVA CRR model, patients were stratified according to clinical T and N stage, Gleason score and PSA value. After considering confounders, patients with cT3/T4, cN0, Gleason score 8–10 or PSA > 10 ng/ml may benefit from LT. Unlike our study, a previous SEER-based analysis—only stratified according to Gleason score and clinical T stage—showed that NLT resulted in higher CSM rates in all stratified subgroups compared with RP [15]. The discrepancy between their and the herein studies could be due to different experimental groups (RP + RT vs. RP) and different age compositions (≥ 75 vs. 65–80 years). It is interesting that they concluded the highest benefit from RP was observed in patients with cT3b/T4 or Gleason score 8–10 disease. In our analysis, patients with cT3b/T4 or Gleason score 8–10 disease could benefit from LT. It suggests that those older than 65 years, with more aggressive features, would harbor the highest survival benefit from LT. Moreover, elderly patients aged ≥ 75 years with cN0 or PSA > 10 ng/ml would benefit from LT. The possible explanation is that lymph node-positive patients have a higher death rate than lymph node-negative patients [18]. In addition, elderly LAPC patients also tend to have a higher chance of distant metastasis [12]. The benefit of LT diminishes under these circumstances. Contradictory to our results, Poppel H et al. showed that T3 PCa patients with PSA < 10 ng/ml would yield significant benefit from RP than those with PSA > 10 ng/ml [19]. Their study, however, was not controlled, and most importantly, age groups were different compared to our study. This may contribute to the reported difference.
Interestingly, RT led to higher CSM rates in patients with T3a disease compared with RP (P = 0.02) in the MVA CRR model. That means RP could be a better option for T3a elderly patients aged ≥ 75 years. However, in LT vs. NLT cohorts, LT did not show a significant advantage over NLT regarding CSM in T3a patients (P = 0.14). Therefore, how T3a elderly patients aged ≥ 75 years may benefit from RP should be further discussed.
Fourth, elderly patients normally suffer from comorbidities [20]. Consequently, they have a higher chance of dying of other diseases compared to younger ones (< 75 years). CSM benefits from LT are only meaningful if patients live long enough to enjoy a CSM reduction. Hence, we also examined the OCM rate in each cohort. The results indicated that no obvious difference existed between LT and NLT cohorts (Fig. 2). LT cohort even tended to be lower (25.1 vs. 31.1%), although not statistically significant, at the 5 years OCM. This suggests that elderly patients aged ≥ 75 years who were treated with LT have enough time to enjoy the CSM reduction compared with the NLT-treated counterparts.
Fifth, life expectancy is often crucial in selecting treatment modalities, especially in elderly patients. The European Association of Urology (EAU)—European Society for Radiotherapy & Oncology (ESTRO)—International Society of Geriatric Oncology (SIOG) Guidelines recommend that RP should be offered to medium- and high-risk localized PCa patients with a life expectancy > 10 years [21]. However, a recent published article showed a 16% under-treatment rate in medium- or high-risk PCa patients (aged > 75 years) without any significant comorbidity [22]. Another article reported that only 10% of men at the age of 75–80 years without obvious comorbidity received radical treatment in spite of their 52% probability of a 10-year life expectancy [23]. We believe that there could also be some potential under-treatment in LAPC patients aged ≥ 75 years in our daily clinical practice, especially in those with fewer comorbidities. Here, we suggested that treatment decisions should be made based on functional age, not chronological age, which can be assessed by some geriatric assessment tools.
There are some limitations which should be noted in this study. First and foremost, although SEER is a comprehensive population-based database in the US, it lacks information about patient baseline performance status and comorbidities. We tried to obliterate the influence of these confounders using PSM methods and MVA CRR models, which took OCM and other covariates into account when analyzing. However, due to the retrospective nature of this study, a potential selection bias caused by baseline performance status and comorbidities in each patient might still occur, and that is the reason why we did not include the overall survival in our analysis. Second, the database only records the initial treatment. It is, therefore, unknown how potential later following treatment would affect CSM. Likewise, the database does not provide information about the usage of RT dose as well as RP type (open vs. robotic). Third, the MVR CRR analysis was not applied to cNx patients due to the limitation of sample size. Last but not least, the database lacks information on ADT and chemotherapy, especially ADT, which is a basic treatment for PCa patients. Given the limitations above, the results should be treated cautiously.
Conclusion
Our analysis showed that LT yielded significantly lower CSM compared to NLT in elderly patients aged ≥ 75 years with LAPC. Consequently, LAPC patients may also benefit from LT in spite of advanced age, but the benefit was only seen in patients with cT3b/4, Gleason score 8–10, cN0, or PSA > 10 ng/ml. No evidence indicated that there was any significant difference between RT and RP regarding CSM, except for cT3a patients in whom higher CSM rates were noted for RT compared with RP.
References
Warde P, Mason M, Ding K et al (2011) Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: a randomised, phase 3 trial. Lancet 378(9809):2104–2111. https://doi.org/10.1016/S0140-6736(11)61095-7
Widmark A, Klepp O, Solberg A et al (2009) Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): an open randomised phase III trial. Lancet 373(9660):301–308. https://doi.org/10.1016/S0140-6736(08)61815-2
Mitchell CR, Boorjian SA, Umbreit EC et al (2012) 20-Year survival after radical prostatectomy as initial treatment for cT3 prostate cancer. BJU Int 110(11):1709–1713. https://doi.org/10.1111/j.1464-410X.2012.11372.x
Loeb S, Smith ND, Roehl KA, Catalona WJ (2007) Intermediate-term potency, continence, and survival outcomes of radical prostatectomy for clinically high-risk or locally advanced prostate cancer. Urology 69(6):1170–1175. https://doi.org/10.1016/j.urology.2007.02.054
Moltzahn F, Karnes J, Gontero P et al (2015) Predicting prostate cancer-specific outcome after radical prostatectomy among men with very high-risk cT3b/4 PCa: a multi-institutional outcome study of 266 patients. Prostate Cancer Prostatic Dis 18(1):31–37. https://doi.org/10.1038/pcan.2014.41
Van Poppel H, Vekemans K, Da Pozzo L et al (2006) Radical prostatectomy for locally advanced prostate cancer: results of a feasibility study (EORTC 30001). Eur J Cancer 42(8):1062–1067. https://doi.org/10.1016/j.ejca.2005.11.030
Carver BS, Bianco FJ Jr, Scardino PT, Eastham JA (2006) Long-term outcome following radical prostatectomy in men with clinical stage T3 prostate cancer. J Urol 176(2):564–568. https://doi.org/10.1016/j.juro.2006.03.093
National Cancer Institute Surveillance, Epidemiology, and EndResults Prostate-Specific Antigen Working Group, Adamo MP, Boten JA et al (2017) Validation of prostate-specific antigen laboratory values recorded in surveillance, epidemiology, and end results registries. Cancer 123:697–703. https://doi.org/10.1002/cncr.30401
Hu CY, Xing Y, Cormier JN, Chang GJ (2013) Assessing the utility of cancer-registry-processed cause of death in calculating cancer-specific survival. Cancer 119:1900–1907. https://doi.org/10.1002/cncr.27968
D’Agostino RB Jr (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17:2265–2281. https://doi.org/10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b
Gray R (1988) A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 6:1140–1154. http://www.jstor.org/stable/2241622
Scosyrev E, Messing EM, Mohile S, Golijanin D, Wu G (2012) Prostate cancer in the elderly: frequency of advanced disease at presentation and disease-specific mortality. Cancer 118(12):3062–3070. https://doi.org/10.1002/cncr.26392
Thompson I, Thrasher JB, Aus G et al (2007) Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol 177:2106–2131. https://doi.org/10.1016/j.juro.2007.03.003
Mottet N, Bellmunt J, Bolla M et al (2011) EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol 59:572–583. https://doi.org/10.1016/j.eururo.2011.01.025
Gandaglia G, Sun M, Trinh QD et al (2014) Survival benefit of definitive therapy in patients with clinically advanced prostate cancer: estimations of the number needed to treat based on competing-risks analysis. BJU Int 114(6b):E62–E69. https://doi.org/10.1111/bju.12645
Weiner AB, Matulewicz RS, Schaeffer EM et al (2017) Contemporary management of men with high-risk localized prostate cancer in the United States. Prostate Cancer Prostatic Dis 20(3):283–288. https://doi.org/10.1038/pcan.2017.5
Boorjian Stephen A, Jeffrey Karnes R, Viterbo Rosalia et al (2011) Long-term survival after radical prostatectomy versus external beam radiotherapy for patients with high-risk prostate cancer. Cancer 117(13):2883–2891. https://doi.org/10.1002/cncr.25900
Cheng L1, Zincke H, Blute ML et al (2001) Risk of prostate carcinoma death in patients with lymph node metastasis. Cancer 91(1):66–73. https://doi.org/10.1002/1097-0142(20010101)91:1<66::AID-CNCR9>3.0.CO;2-P
Van Poppel H, Goethuys H, Callewaert P et al (2000) Radical prostatectomy can provide a cure for well-selected clinical stage T3 prostate cancer. Eur Urol 38:372–379. https://doi.org/10.1159/000020311
Piccirillo JF, Vlahiotis A, Barrett LB et al (2008) The changing prevalence of comorbidity across the age spectrum. Crit Rev Oncol Hematol 67(2):124–132. https://doi.org/10.1016/j.critrevonc.2008.01.013
Mottet N, Bellmunt J, Bolla M et al (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 71:618–629. https://doi.org/10.1016/j.eururo.2016.08.003
Lunardi P, Ploussard G, Grosclaude P et al (2017) Current impact of age and comorbidity assessment on prostate cancer treatment choice and over/undertreatment risk. World J Urol 35(4):587–593. https://doi.org/10.1007/s00345-016-1900-9
Bratt O, Folkvaljon Y, Hjälm Eriksson M et al (2015) Undertreatment of men in their seventies with high-risk nonmetastatic prostate cancer. Eur Urol 68(1):53–58. https://doi.org/10.1016/j.eururo.2014.12.026
Acknowledgements
Wei Sheng is grateful for the funding from the China Scholarship Council (201608080204).
Author information
Authors and Affiliations
Contributions
Protocol/project development: WS, HWZ; data collection or management: WS; manuscript writing/editing: WS, RK.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no actual or potential conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
345_2018_2389_MOESM2_ESM.tif
Supplementary Fig. 2. The jitter plot for local treatment vs. non-local treatment in propensity score matching (TIFF 714 kb)
345_2018_2389_MOESM3_ESM.tif
Supplementary Fig. 3. The jitter plot for radical prostatectomy vs. radiation therapy in propensity score matching (TIFF 819 kb)
Rights and permissions
About this article
Cite this article
Sheng, W., Kirschner-Hermanns, R. & Zhang, H. Elderly patients aged ≥ 75 years with locally advanced prostate cancer may benefit from local treatment: a population-based propensity score-adjusted analysis. World J Urol 37, 317–325 (2019). https://doi.org/10.1007/s00345-018-2389-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2389-1