Abstract
Purpose
To assess the current status and future potential of multiparametric MRI (mpMRI) and MRI-targeted biopsy (MRI-TBx) on the pretherapeutic risk assessment in prostate cancer patients’ candidates for radical prostatectomy.
Methods
A literature search of the MEDLINE/PubMed and Scopus database was performed. English-language original and review articles were analyzed and summarized after an interactive peer-review process of the panel.
Results
Pretherapeutic risk assessment tools should be based on target plus systematic biopsies, where the addition of systematic biopsy (TRUS-Bx) to the mpMRI-target cores is associated with a lower rate of upgrading at final pathology. The combination of mpMRI findings with clinical parameters outperforms models based on clinical parameters alone in the prediction of adverse pathological outcomes and oncological results. This is particularly true when a specialized radiologist is present.
Conclusion
The combination of mpMRI findings and clinical parameters should be considered to improve patient stratification in the pretherapeutic risk assessment. There is an urgent need to develop or include MRI data and MRI-TBx findings in available preoperative risk tools. This will allow improving the pretherapeutic risk assessment, providing important additional information for patient-tailored treatment planning and optimizing outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radical prostatectomy (RP) represents the most commonly used therapeutic approach in patients with a diagnosis of clinically localized prostate cancer (PCa) [1, 2]. Pretherapeutic risk assessment plays a key role in the planning of the surgical approach. Indeed, risk stratification based on individual disease characteristics is key to plan the extent of the preservation of the neurovascular bundles, which is associated with improved erectile function recovery, as well as to decide whether to perform a pelvic lymph node dissection (PLND) and its extension [1,2,3,4,5]. Due to the low accuracy of the conventional imaging in the prediction of extracapsular extension (ECE), seminal vesicle invasion (SVI) [6], and the identification of patients with lymph node invasion (LNI) [7], preoperative risk stratification was historically based on multivariable models that included clinical variables such as serum prostate-specific antigen (PSA), clinical stage, the number of positive cores, and biopsy Gleason score [8,9,10,11].
Over the last few years, the introduction of mpMRI in the diagnostic pathway of PCa led to substantial changes in the diagnosis of localized disease. In particular, the use of mpMRI is associated with an improved detection of clinically significant PCa (csPCa) with a reduction of the risk of overdiagnosis [12,13,14]. Moreover, the availability of MRI images led to the development of mpMRI-based targeted biopsies (MRI-TBx), which are associated with an increase in the detection of csPCa reducing the rates of insignificant disease relative to standard systematic biopsy approaches (TRUS-Bx) [15,16,17,18,19]. This led to a paradigm shift in the pretherapeutic risk assessment of PCa patients, where more accurate preoperative information on disease characteristics based on imaging and MRI-TBx should be incorporated in available models to improve our ability to predict pathological outcomes.
The aim of this narrative review was to summarize the available evidence on the current status and future potential of MRI and MRI-TBx on the pretherapeutic risk assessment of PCa.
Methods
A literature search of the MEDLINE/PubMed and Scopus database was performed using the following keywords in combination with both medical subject headings terms and text words: prostate cancer, MRI, targeted biopsy, risk tools, staging, and risk assessment. Only English-language original and review articles published between May 2007 and March 2018 were included. The relevant studies selected were analyzed and summarized after an interactive peer-review process of the panel.
mpMRI in risk assessment at diagnosis
Even though mpMRI, together with MRI-TBx, has demonstrated to significantly improve the accuracy in detecting csPCa [15,16,17,18,19], the combination of this radiologic test with available clinical information and biomarkers seems to return the best diagnostic risk estimate. Indeed, several risk models have been developed showing an increase in mpMRI accuracy in detecting csPCa and spare prostate biopsies in patients more likely to be diagnosed with low-risk disease [20,21,22,23,24]. The diagnostic risk assessment is of crucial importance to reduce overtreatment rate and restrict active treatment to significant diseases only. A summary of the current available risk tools is presented in Table 1. All these risk models were developed on series of patients underwent mpMRI and subsequent MRI-TBx using either software assisted-registration (fusion) or visual registration (cognitive) approach. The majority of these studies utilized transperineal systematic template biopsies as their reference standard. Distler et al. [20] developed a nomogram to predict the risk of csPCa relying on PI-RADS and PSA density. The authors observed that PSA density increases the NPV of negative mpMRI (79 vs. 89%) for exclusion of csPCa when PSA density was 0.15 ng/ml/ml or less. These findings were confirmed in the previous negative biopsy setting (83 vs. 93%) [20]. Radtke et al. [21] developed novel risk models for prediction of csPCa for biopsy naïve men and after the previous biopsy and compared these with the ERSPC risk calculators and PI-RADS. The novel risk models, incorporating clinical parameters (age, PSA, DRE, and prostate volume) and PI-RADS, performed significantly better compared with those without PI-RADS and those with only PI-RADS, and were found to be more helpful in making the decision to biopsy men at a suspicion of PCa [21]. However, these models lack of an external validation. To overcome this issue, Van Leeuwen et al. [22] demonstrated that a model combining age, PSA, DRE, prostate volume, previous biopsy, and PI-RADS outperform the model of clinical parameters alone, and the accuracy of this model in the external validation cohort was 86%. The clinical application of this model would allow sparing 28% of prostate biopsies at the cost of missing 1.6% of csPCa [22]. In conclusion, all these risk models [20,21,22,23,24] demonstrated that combining clinical parameters with mpMRI improved the accuracy of the decision to perform a biopsy in a patient with suspicion of PCa in comparison with models based on clinical parameter or PI-RADS alone both in biopsy naïve and previous negative biopsy setting. This allows a considerable reduction in the number of unnecessary prostate biopsies at the cost of missing a very small number of csPCa and leads to a reduction in overtreatment. As such, mpMRI should be considered within the clinical context before surgery to achieve an accurate therapeutic strategy decision.
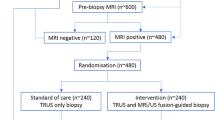
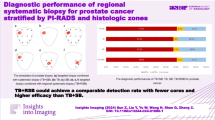
Current role of a “targeted biopsy approach” in preoperative risk assessment
The increase in the use of MRI-TBx in clinical practice has redefined the current biopsy strategies, and the introduction of a targeted biopsy approach in the diagnostic pathway of PCa has been evaluated [25]. In this context, it is also important to evaluate how targeted biopsies without systematic cores might affect the preoperative risk assessment as compared to other biopsy strategies. Although a recent RCT reported the superiority of the MRI-TBx alone as compared to 12-core TRUS-Bx alone [25], the question about whether or not we should quit performing systematic sampling, in addition to MRI-TBx, still remains without an answer [26,27,28,29]. The current role of systematic sampling resides both in avoiding csPCa misdiagnosis as well as in providing an accurate mapping of the prostate in the view of an eventual subsequent treatment. First, the combination of both TRUS-Bx and MRI-TBx has been shown to provide the highest detection rate of significant disease at the cost of a sharp increase in the detection of non-significant PCa in patients with positive mpMRI, with TRUS-Bx being 79% better than MRI-TBx in detecting non-significant disease [15]. The concordance between the two techniques in detecting PCa is quite high [65% (CI 54–74%)] [15]; nonetheless, the addition of TRUS-Bx still allowed to detect 15% csPCa more as compared to the use of MRI-TBx alone [15]. Second, in the PROMIS trial [13], which provided promising results regarding the use of mpMRI as a triage test for the detection of csPCa, the accuracy of imaging in defining csPCa multifocality was not provided. The presence of multiple csPCa foci within the prostatic tissue is crucial when a targeted biopsy alone strategy is considered. In this context, Le et al. [30], in a study comparing mpMRI to RP specimen, reported that mpMRI missed non-index lesions with Gleason grade ≥ 3 + 4 in 20% of men. In further studies comparing targeted and systematic approach with RP specimen, Borkowetz et al. [31] reported that 16% of tumor foci would have been detected by TRUS-Bx alone, with 81% of those being csPCa. Radtke et al. [32], in a similar study, demonstrated that the addition of TRUS-Bx to MRI-TBx would have increased the detection rate of csPCa from 79 to 97%. In both aforementioned studies [31, 32], the combination of MRI-TBx and TRUS-Bx provided the highest significant index lesions detection. In this context, an important issue that must be taken into account is the precision of MRI-TBx in correctly sampling the lesion reported by mpMRI. Indeed, MRI-TBx failed to target the mpMRI lesion in approximately 20% of suspicious lesions harbouring PCa at final pathology [30,31,32]. Furthermore, the use of both systematic and targeted approach was demonstrated to provide the lowest rate of upgrading at RP, ranging from 18 up to 29% [31, 33]. In conclusion, the combination of MRI-TBx and TRUS-Bx is associated with the lowest probability of significant disease misdiagnosis. Moreover, the addition of systematic cores to targeted ones provides the best reflection of PCa multifocality within the prostate gland and the most reliable PCa grading. With the aim to provide an as reliable as possible preoperative risk assessment, the combination of both biopsy strategies must be considered, so far, the best available approach until future risk tools will allow to safely identify which patients might avoid systematic prostate biopsy in addiction to MRI-TBx.
Are we ready to use information from mpMRI and MRI-targeted biopsy in available preoperative models?
Prediction of adverse pathological outcomes
The role of mpMRI in PCa staging is still a matter of debate. A recent systematic review and meta-analysis [6] demonstrated that MRI has a high specificity but a poor and heterogeneous sensitivity for local PCa staging. The pooled sensitivity for ECE, SVI, and overall stage T3 were 57, 58, and 61%, respectively [6]. Despite the sensitivity of MRI increases with the addiction of functional imaging to T2-weighted imaging [6], it is still low and this limits the preoperative surgical planning which could be modified based on minimizing the risk of positive surgical margins (PSMs) and optimizing the likelihood of complete extirpation via image-directed guidance for wide resection. Evidence coming from a RCT suggests that preoperative MRI alone do not reduce the overall risk of PSMs [34]. Specifically, Rud et al. [34] randomized 216 patients to non-MRI vs. 222 to MRI prior to robotic-assisted RP and observed that despite MRI changed the surgical procedure in the direction of a more radical excision in 27% of the patients, the rate of PSMs was 23 vs. 19% in non-MRI vs. MRI group (p = 0.4), respectively. However, surprisingly, when a subgroup analysis was performed in those patients with cT1 disease, there was a statistically significant difference in terms of PSMs between non-MRI and MRI groups (27 vs. 16%, respectively; p = 0.035). The relative and absolute reduction was 41 and 11%, respectively. This suggests that the use of mpMRI for preoperative staging might reduce the risk of PSMs in patients with impalpable disease at DRE.
Other authors assessed the added value of mpMRI data to clinical parameters to predict adverse pathological outcomes (Table 2). For example, Feng et al. [35] observed that mpMRI results (positive/negative for ECE) might predict pathological ECE and significantly increase the diagnostic accuracy of clinical-based models (Partin Table and Memorial Sloan-Kettering [MSK] nomogram). The authors [35] developed also a risk tool that integrates ECE status at mpMRI with clinical-based models to estimate pathological ECE risk. A similar designed study [36] analyzed the incremental value of preoperative MRI in addiction to clinical-based models [Partin Table and the cancer of the prostate risk assessment (CAPRA) score] in predicting adverse outcomes at RP. The authors [36] observed that when MRI results (i.e., negative vs. positive mpMRI) were added to each model predicting pathological ECE and SVI, they were significantly associated with the outcome of interest. Moreover, they provided evidence that MRI combined with clinical models outperformed clinical-based models alone for prediction of adverse outcomes at RP [36] (Table 2). The largest study available to date that assessed the added value of mpMRI to clinical parameters was published by Grivas et al. [37]. In a cohort of 527 patients who underwent 3-T mpMRI and subsequent robotic-assisted RP, the authors observed that MRI finding was a highly significant predictor of SVI, after accounting for clinical parameters (Table 2). Furthermore, the combination of MRI data with Partin model overwhelmingly increased the AUC (from 83.7 to 92.9%) and the net benefit. In a sub-analysis in 379 patients where mpMRI were assessed by only one expert radiologist, the sensitivity of mpMRI for SVI detection increased from 75.9 to 84.4% [37]. On the same direction, Tay et al. [38] evaluated the incremental utility of mpMRI over clinical parameters in predicting ECE interpreted in a standard radiologic setting (standard read) and when further over-read by a specialized reader (specialized read). The authors observed that the sensitivity of clinical parameters-only model vs. clinical parameters + MRI standard read vs. clinical parameters + MRI specialized read was 60 vs. 68 vs. 88%, respectively (Table 2). Moreover, the addition of mpMRI standard read led to a small but not significant increase in the AUC (72 vs. 69%). Conversely, the addition of mpMRI specialized reading significantly increases the AUC relative to the clinical baseline model (91 vs. 69%; Table 2) [38], suggesting that specific radiologic training is mandatory to improve the preoperative surgical planning. Recently, Weaver et al. [39] failed to observe a significant increase of the diagnostic accuracy in predicting ECE and SVI when mpMRI data were added to MSK nomogram. This discrepancy between the previous studies may reside in the high number of radiologist (9) who evaluated mpMRI findings [39].
To summarize, the majority of the available studies provided evidence that mpMRI findings are significant related to ECE [35, 36, 39], SVI [36, 37] and significantly increased the diagnostic accuracy of clinical parameters [38] and of clinical-based model alone (Partin table [35, 36], Memorial Sloan–Kettering (MSK) nomogram [35], and Cancer of the Prostate Risk Assessment (CAPRA) score [36]) to predict adverse RP outcomes. However, some considerations of the aforementioned studies should be underlined. First, only one of these studies [35] developed a risk tool allowing individual pretherapeutic risk assessment. Second, only two of these studies reported the sensitivity of the mpMRI data combined with clinical parameters to predict adverse pathological outcomes [35, 38]. This is surprising given that sensitivity is mandatory to understand whether mpMRI incorporated with clinical data might be reliable used in preoperative planning. Tay et al. reported that, except in case of specialized reader, the sensitivity is low 68% [38]. The high sensitivity reported by Feng et al. [35] (84–91%, and 83–94% considering cutoff between 15 and 40% according to Partin table and MSK nomogram, respectively; Table 2) is questionable, because the authors did not report how many adverse pathological outcomes will be missed below the proposed high cutoff. In consequence, these findings are not applicable during clinical practice. Third, all the aforementioned studies only considered MRI results in terms of negative or positive exam for the outcome of interest (ECE/SVI) without including other MRI data. There is evidence that apparent diffusion coefficient (ADC) from DWI and lesion volume at mpMRI are independent predictors of ECE at final pathology [40, 41]. Moreover, the first nomogram incorporating DWI information outperforms those without DWI [40]. Few studies [42, 43] assessed the potential role of PI-RADS score in the pretherapeutic risk assessment, suggesting that MRI information should be combined with other risk factors to properly assess non-organ confined disease. Future reports are needed to assess this area of research to understand whether PI-RADS score should be included into new risk tools to improve presurgical planning. Interestingly, the recently released PI-RADS v.2 [44] no longer contains the criteria for standard assessment of non-organ confined disease of the previous PI-RADS v.1 which relied on a dedicated scale system proposed by the European society of urogenital radiology (ESUR) [45]. This standardized system, dedicated to staging included within PI-RADS v.1, was demonstrated to be significantly associated with pathological ECE and to improve the sensitivity and the overall accuracy for ECE relative to non-standardized reporting system [41, 46]. Differently, PI-RADS v.2 provides a brief overview of the major MRI findings regarding ECE and SVI [44]. The absence of a formal standardized reporting system for staging might explain the high interobserver variability in the interpretation of MRI in staging assessment [47]. This emphasizes the need to improve standardization of imaging criteria that define ECE and SVI. Last but not least, none of the aforementioned studies took into account the value of MRI-TBx findings. Therefore, their results cannot be applicable in daily clinical practice given the widespread use of MRI-TBx. MRI-TBx might help to recognize in which cases preoperative planning and surgical dissection warrant added caution, because it can correctly identify aggressive PCa that are missed by TRUS-Bx and that are most likely to lead to adverse pathological outcomes. Recently, Raskolnikov et al. [48] observed that MRI-TBx Gleason score is significantly related with pathological ECE in patients who harbour preoperative negative MRI for ECE and in consequence could help to identify which patients with PCa have occult adverse RP outcomes not detectable by mpMRI. However, the authors did not provide an individual risk tool and observed a slightly increase of the AUC (from 0.83 to 0.86) of the model incorporating MRI-TBx Gleason score relative to the basic one (age, PSA and random biopsy Gleason score) [48]. All these considerations strongly suggest that there is an urgent need of new preoperative risk tools that reliable detect and localize adverse RP outcomes including not only MRI data but also MRI-TBx findings.
Prediction of lymph node invasion
The role of mpMRI was also assessed for preoperative nodal staging. A meta-analysis [7] reported a low pooled sensitivity for MRI also in this setting, probably because the definition of nodal metastasis on imaging relies on size criteria. The advent of the mpMRI allowed obtaining information regarding the anatomy of the prostate gland and its functional behaviour. Indeed, mpMRI data combined with clinical parameters increased the ability of existing clinical-based model to predict nodal metastases (LNI) [36, 39], despite this increase is not overwhelmingly as when ECE and SVI were chosen as outcome of interest (Table 2). There is also evidence that MRI T stage [49,50,51] and tumor volume at MRI [51] should be considered to predict the risk of LNI. The combination of these parameters to the clinical one showed an AUC of 95.6% and a sensitivity of 82.6%, strongly suggesting the inclusion of MRI T stage and tumor volume into the preoperative risk assessment [51]. However, the authors did not include MRI-TBx findings into the multivariable model and did not develop a risk tool due to the low number of events in terms of LNI [51]. The importance of MRI T stage was confirmed by other authors in addiction with predominant Gleason Pattern 4 [52]. To date, several risk tools are used to predict the risk of LNI [10, 11]. All these risk tools were tailored to patients undergoing standard TRUS biopsies who did not undergo preoperative mpMRI. In consequence, they may not be applicable to patients who underwent preoperative mpMRI and MRI-TBx. For example, if we consider the most popular one of these risk tools [11], there is evidence that the role of mpMRI is crucial when the predicted risk of LNI is < 5% [52]. If the patients undergo extended PLND (ePLND) according to the findings of mpMRI despite the risk of LNI is less than 5%, the risk of harbouring LNI is up to 15% [52]. Moreover, applying the findings of MRI-TBx to the Briganti nomogram [11], it might lead to an overestimation of the risk of LNI due to the higher percentage of positive cores. Hence, the available risk tools require being updated and validated utilizing MRI data and MRI-TBx findings to allow a better selection of candidates to ePLND.
Prediction of oncologic outcomes
There is also evidence that mpMRI can help the physicians to preoperatively assess the risk of biochemical recurrence (BCR) after RP [53,54,55,56,57]. Some studies demonstrated that the addition of mpMRI data significantly improves the ability of clinical parameters to predict the risk of BCR after RP [54,55,56] (Table 2). For example, Ho et al. [54] developed a nomogram to predict 3-year BCR after RP incorporating clinical data (preoperative PSA and Gleason score at biopsy) with mpMRI parameters (mpMRI suspicion score and ECE). The c-index of the nomogram with or without mpMRI data was 84 vs. 74%, respectively. More recently, Zhang et al. [56] developed a risk model using patient age, first preoperative PSA level, and six MRI parameters: (1) tumor location; (2) maximum diameter of leading lesion, (3) ADCs of leading lesion; (4) PI-RADS score; (5) DCE type; (6) MRI T stage. This nomogram performed better than the D’Amico and CAPRA score alone in predicting 3-year BCR after RP (91 vs. 79 vs. 81%, respectively). The performance of D’Amico and CAPRA scores was significantly improved by adding these MRI findings (Table 2). These studies strongly suggest that the performance of clinical parameters can be significantly increased adding mpMRI findings. However, future risk tools need to be developed incorporating other MRI findings [57] and data from MRI-TBx.
Conclusions
Over the last few years the advent of mpMRI and MRI-TBx significantly changed the diagnostic pathway of PCa. The combination of mpMRI findings and clinical parameters should always be considered in the pretherapeutic risk assessment to better risk-stratify and counsel the patients in daily clinical practice. However, there is an impending need to develop or include in the available preoperative risk tools MRI data and MRI-TBx findings to be applicable during clinical decision-making. This would allow for improving the pretherapeutic risk assessment providing important additional information for patient-tailored treatment planning, optimizing pathological and oncological outcomes.
References
Guidelines on prostate cancer (2018) European Association of Urology. http://uroweb.org/guideline/prostate-cancer/. Accessed Mar 2018
National Comprehensive Cancer Network (2017) Clinical practice guidelines in oncology (NCCN Guidelines®). Prostate cancer. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed Mar 2018
Gontero P, Kirby RS (2005) Nerve-sparing radical retropubic prostatectomy: techniques and clinical considerations. Prostate Cancer Prostatic Dis 8:133–139
Sokoloff MH, Brendler CB (2001) Indications and contraindications for nerve-sparing radical prostatectomy. Urol Clin North Am 28:535–543
Suardi N, Larcher A, Haese A et al (2014) Indication for and extension of pelvic lymph node dissection during robot-assisted radical prostatectomy: an analysis of five European institutions. Eur Urol 66:635–643
de Rooij M, Hamoen EH, Witjes JA, Barentsz JO, Rovers MM (2016) Accuracy of magnetic resonance imaging for local staging of prostate cancer: a diagnostic Meta-analysis. Eur Urol 70:233–245
Hovels AM, Heesakkers RA, Adang EM et al (2008) The diagnostic accuracy of CT and MRI in the staging of pelvic lymph nodes in patients with prostate cancer: a meta-analysis. Clin Radiol 63:387–395
Steuber T, Graefen M, Haese A et al (2006) Validation of a nomogram for prediction of side specific extracapsular extension at radical prostatectomy. J Urol 175:939–944 [discussion 44]
Eifler JB, Feng Z, Lin BM et al (2013) An updated prostate cancer staging nomogram (Partin tables) based on cases from 2006 to 2011. BJU Int 111:22–29
Memorial sloan kettering cancer center. Prostate cancer nomograms pre-radical prostatectomy. http://www.mskcc.org/nomograms/prostate/pre_op. Accessed Feb 2018
Briganti A, Larcher A, Abdollah F et al (2012) Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol 61:480–487
Futterer JJ, Briganti A, De Visschere P et al (2015) Can clinically significant prostate cancer be detected with multiparametric magnetic resonance imaging? A systematic review of the literature. Eur Urol 68:1045–1053
Ahmed HU, El-Shater Bosaily A, Brown LC et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389:815–822
Simmons LAM, Kanthabalan A, Arya M et al (2017) The PICTURE study: diagnostic accuracy of multiparametric MRI in men requiring a repeat prostate biopsy. Br J Cancer 116:1159–1165
Schoots IG, Roobol MJ, Nieboer D, Bangma CH, Steyerberg EW, Hunink MG (2015) Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol 68:438–450
Siddiqui MM, Rais-Bahrami S, Turkbey B et al (2015) Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 313:390–397
van Hove A, Savoie PH, Maurin C et al (2014) Comparison of image-guided targeted biopsies versus systematic randomized biopsies in the detection of prostate cancer: a systematic literature review of well-designed studies. World J Urol 32:847–858
Valerio M, Donaldson I, Emberton M et al (2015) Detection of clinically significant prostate cancer using magnetic resonance imaging-ultrasound fusion targeted biopsy: a systematic review. Eur Urol 68:8–19
Wegelin O, van Melick HHE, Hooft L et al (2017) Comparing three different techniques for magnetic resonance imaging-targeted prostate biopsies: a systematic review of in-bore versus magnetic resonance imaging-transrectal ultrasound fusion versus cognitive registration. is there a preferred technique? Eur Urol 71:517–531
Distler FA, Radtke JP, Bonekamp D et al (2017) The value of PSA density in combination with PI-RADS for the accuracy of prostate cancer prediction. J Urol 198:575–582
Radtke JP, Wiesenfarth M, Kesch C et al (2017) Combined clinical parameters and multiparametric magnetic resonance imaging for advanced risk modeling of prostate cancer-patient-tailored risk stratification can reduce unnecessary biopsies. Eur Urol 72:888–896
van Leeuwen PJ, Hayen A, Thompson JE et al (2017) A multiparametric magnetic resonance imaging-based risk model to determine the risk of significant prostate cancer prior to biopsy. BJU Int 120:774–781
Bjurlin MA, Rosenkrantz AB, Sarkar S et al (2018) Prediction of prostate cancer risk among men undergoing combined MRI-targeted and systematic biopsy using novel pre-biopsy nomograms that incorporate MRI findings. Urology 112:112–120
Mehralivand S, Shih JH, Rais-Bahrami S et al (2018) A magnetic resonance imaging-based prediction model for prostate biopsy risk stratification. JAMA Oncol 4:678–685
Kasivisvanathan V, Rannikko AS, Borghi M et al (2018) MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N Engl J Med. 378:1767–1777
Porpiglia F, Manfredi M, Mele F et al (2017) Diagnostic pathway with multiparametric magnetic resonance imaging versus standard pathway: results from a randomized prospective study in biopsy-naive patients with suspected prostate cancer. Eur Urol 72:282–288
Tonttila PP, Lantto J, Paakko E et al (2016) Prebiopsy multiparametric magnetic resonance imaging for prostate cancer diagnosis in biopsy-naive men with suspected prostate cancer based on elevated prostate-specific antigen values: results from a randomized prospective blinded controlled trial. Eur Urol 69:419–425
Baco E, Rud E, Eri LM et al (2016) A randomized controlled trial to assess and compare the outcomes of two-core prostate biopsy guided by fused magnetic resonance and transrectal ultrasound images and traditional 12-core systematic biopsy. Eur Urol 69:149–156
Arsov C, Rabenalt R, Blondin D et al (2015) Prospective randomized trial comparing magnetic resonance imaging (MRI)-guided in-bore biopsy to MRI-ultrasound fusion and transrectal ultrasound-guided prostate biopsy in patients with prior negative biopsies. Eur Urol 68:713–720
Le JD, Tan N, Shkolyar E et al (2015) Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol 67:569–576
Borkowetz A, Platzek I, Toma M et al (2016) Direct comparison of multiparametric magnetic resonance imaging (MRI) results with final histopathology in patients with proven prostate cancer in MRI/ultrasonography-fusion biopsy. BJU Int 118:213–220
Radtke JP, Schwab C, Wolf MB et al (2016) Multiparametric magnetic resonance imaging (MRI) and MRI-transrectal ultrasound fusion biopsy for index tumor detection: correlation with radical prostatectomy specimen. Eur Urol 70:846–853
Arsov C, Becker N, Rabenalt R et al (2015) The use of targeted MR-guided prostate biopsy reduces the risk of Gleason upgrading on radical prostatectomy. J Cancer Res Clin Oncol 141:2061–2068
Rud E, Baco E, Klotz D et al (2015) Does preoperative magnetic resonance imaging reduce the rate of positive surgical margins at radical prostatectomy in a randomised clinical trial? Eur Urol 68:487–496
Feng TS, Sharif-Afshar AR, Wu J et al (2015) Multiparametric MRI improves accuracy of clinical nomograms for predicting extracapsular extension of prostate cancer. Urology. 86:332–337
Morlacco A, Sharma V, Viers BR et al (2017) The incremental role of magnetic resonance imaging for prostate cancer staging before radical prostatectomy. Eur Urol 71:701–704
Grivas N, Hinnen K, de Jong J et al (2018) Seminal vesicle invasion on multi-parametric magnetic resonance imaging: correlation with histopathology. Eur J Radiol 98:107–112
Tay KJ, Gupta RT, Brown AF, Silverman RK, Polascik TJ (2016) Defining the incremental utility of prostate multiparametric magnetic resonance imaging at standard and specialized read in predicting extracapsular extension of prostate cancer. Eur Urol 70:211–213
Weaver JK, Kim EH, Vetter JM et al (2018) Prostate magnetic resonance imaging provides limited incremental value over the memorial sloan kettering cancer center preradical prostatectomy nomogram. Urology 113:119–128
Giganti F, Coppola A, Ambrosi A et al (2016) Apparent diffusion coefficient in the evaluation of side-specific extracapsular extension in prostate cancer: development and external validation of a nomogram of clinical use. Urol Oncol 34(291):e9–e17
Woo S, Cho JY, Kim SY, Kim SH (2015) Extracapsular extension in prostate cancer: added value of diffusion-weighted MRI in patients with equivocal findings on T2-weighted imaging. AJR Am J Roentgenol 204:W168–W175
Toner L, Papa N, Perera M et al (2017) Multiparametric magnetic resonance imaging for prostate cancer-a comparative study including radical prostatectomy specimens. World J Urol 35:935–941
Park SY, Jung DC, Oh YT et al (2016) Prostate cancer: PI-RADS version 2 helps preoperatively predict clinically significant cancers. Radiology 280:108–116
Weinreb JC, Barentsz JO, Choyke PL et al (2016) PI-RADS prostate imaging—reporting and data system: 2015, version 2. Eur Urol 69:16–40
Barentsz JO, Richenberg J, Clements R et al (2012) ESUR prostate MR guidelines 2012. Eur Radiol 22:746–757
Schieda N, Quon JS, Lim C et al (2015) Evaluation of the european society of urogenital radiology (ESUR) PI-RADS scoring system for assessment of extra-prostatic extension in prostatic carcinoma. Eur J Radiol 84:1843–1848
Riney JC, Sarwani NE, Siddique S, Raman JD (2018) Prostate magnetic resonance imaging: the truth lies in the eye of the beholder. Urologic oncology. 36(159):e1–e5
Raskolnikov D, George AK, Rais-Bahrami S et al (2015) The Role of Magnetic Resonance Image Guided Prostate Biopsy in Stratifying Men for Risk of Extracapsular Extension at Radical Prostatectomy. J Urol 194:105–111
Wang L, Hricak H, Kattan MW et al (2006) Combined endorectal and phased-array MRI in the prediction of pelvic lymph node metastasis in prostate cancer. AJR Am J Roentgenol 186:743–748
Park SY, Oh YT, Jung DC, Cho NH, Choi YD, Rha KH (2015) Prediction of micrometastasis (< 1 cm) to pelvic lymph nodes in prostate cancer: role of preoperative MRI. AJR Am J Roentgenol 205:W328–W334
Brembilla G, Dell’Oglio P, Stabile A et al (2017) Preoperative multiparametric MRI of the prostate for the prediction of lymph node metastases in prostate cancer patients treated with extended pelvic lymph node dissection. Eur Radiol 28:1969–1976
Porpiglia F, Manfredi M, Mele F et al (2018) Indication to pelvic lymph nodes dissection for prostate cancer: the role of multiparametric magnetic resonance imaging when the risk of lymph nodes invasion according to Briganti updated nomogram is < 5. Prostate cancer prostatic Dis 21:85–91
Park JJ, Kim CK, Park SY, Park BK, Lee HM, Cho SW (2014) Prostate cancer: role of pretreatment multiparametric 3-T MRI in predicting biochemical recurrence after radical prostatectomy. AJR Am J Roentgenol 202:W459–W465
Ho R, Siddiqui MM, George AK et al (2016) Preoperative multiparametric magnetic resonance imaging predicts biochemical recurrence in prostate cancer after radical prostatectomy. PLoS One 11:e0157313
Zhang YD, Wang J, Wu CJ et al (2016) An imaging-based approach predicts clinical outcomes in prostate cancer through a novel support vector machine classification. Oncotarget 7:78140–78151
Zhang YD, Wu CJ, Bao ML et al (2017) MR-based prognostic nomogram for prostate cancer after radical prostatectomy. J Magn Reson Imaging JMRI 45:586–596
Tan N, Shen L, Khoshnoodi P et al (2017) Pathological and 3 Tesla Volumetric Magnetic Resonance Imaging Predictors of Biochemical Recurrence after Robotic Assisted Radical Prostatectomy: Correlation with Whole Mount Histopathology. J Urol 199:1218–1223
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
PD: data collection and manuscript writing; AS: data collection and manuscript writing; BHD: data collection and manuscript writing; GG: manuscript editing and critical revision for important intellectual content; EM: manuscript editing and critical revision for important intellectual content; NF: manuscript editing and critical revision for important intellectual content; VC: manuscript editing and critical revision for important intellectual content; EZ: manuscript editing and critical revision for important intellectual content; VM: manuscript editing and critical revision for important intellectual content;NS: supervision and critical revision for important intellectual content; AM: supervision and critical revision for important intellectual content; FM: supervision and critical revision for important intellectual content; AB: supervision, manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Dell’Oglio, P., Stabile, A., Dias, B.H. et al. Impact of multiparametric MRI and MRI-targeted biopsy on pre-therapeutic risk assessment in prostate cancer patients candidate for radical prostatectomy. World J Urol 37, 221–234 (2019). https://doi.org/10.1007/s00345-018-2360-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2360-1