Abstract
Background
Currently, it is accepted that risk assessment of clinical stage I (CS I) nonseminomatous germ cell tumors (NSGCT) patient is mainly dependent on the presence of lymphovascular invasion (LVI). Initial active surveillance, adjuvant chemotherapy and retroperitoneal lymph node dissection (RPLND) are acceptable treatment options for these patients, but there is no uniform consensus. The purpose of this study was to compare outcomes of active surveillance with adjuvant chemotherapy.
Methods
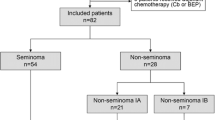
A total of 201 patients with CS I NSGCT after orchiectomy were included. Outcomes of active surveillance and adjuvant chemotherapy were retrospectively analyzed. The prognostic significance of risk factors for survival and relapse was evaluated.
Results
Of the 201 patients, 110 (54.7%) received adjuvant chemotherapy, while the remaining 91 patients (45.3%) underwent surveillance. Relapses were significantly higher for patients underwent surveillance compared to adjuvant chemotherapy group (18.3 vs. 1.2%, p < 0.001). The 5-year relapse-free survival (RFS) rate for patients who were treated with adjuvant chemotherapy was significantly better than those of patients underwent surveillance (97.6 vs. 80.8%, respectively; p < 0.001). Univariate analysis showed that the presence of LVI (p = 0.01) and treatment option (p < 0.001) were prognostic factors for RFS and pT stage (p = 0.004) and invasion of rete testis (p = 0.004) and the presence of relapse (p < 0.001) were significant prognostic factors for OS. Multivariate analysis revealed that the treatment strategy was an independent prognostic factor for RFS (p < 0.001, HR 0.54). A logistic regression analysis demonstrated that treatment options (p = 0.031), embryonal carcinoma (EC) >50% (p = 0.013) and tumor diameter (p = 0.016) were found to be independent factors for predicting relapse.
Conclusions
Our results indicate that adjuvant chemotherapy is associated with improved RFS compared with surveillance for CS I NSGCT patients. Moreover, the treatment strategy is an important prognostic indicator for RFS and a predictive factor for relapse. Although adjuvant chemotherapy seems to be a suitable treatment for patients with risk factors for relapse, surveillance is still preferred management option.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Approximately 40–50% of patients with testicular cancer are diagnosed as nonseminomatous germ cell tumors (NSGCT) and about 50–60% of these present with clinical stage I (CS I), which have not the persistence of increased postoperative tumor markers and without distant metastases (stage IA and IB) [1–3]. The risk of relapse of CS I NSGCT is substantially associated with lymphovascular invasion (LVI) in tumor. In addition, LVI detects in about one-third of the CS I NSGCT [4, 5], and these patients have high recurrence risk compared to those without LVI (about 30–50 vs. 15–20%) [6–8]. Therefore, currently, it is accepted that risk assessment of CS I NSGCT patient is mainly dependent on the presence of LVI [3]. However, if the component of embryonal carcinoma (EC) is found as >50% in the orchiectomy specimen, the rate of metastatic retroperitoneal lymph nodes (RPLN) is reached as 40–50%. Moreover, RPLN metastases are also diagnosed in most patients with pure EC plus LVI, which results in increased recurrence risk [9].
Initial active surveillance, adjuvant chemotherapy, and RPLND are acceptable treatment options for patients with CS I NSGCT, but there is no uniform consensus. In addition, the available data show that cancer-specific survival for CS I NSGCT reaches 100% and almost all patients are cured, regardless of treatment preference after orchiectomy [2, 10, 11]. Active surveillance has nearly same overall survival rate as the other two treatment modalities, especially in patients with low-relapse risk patients and is a safe and noninvasive option. Thus, systemic treatment may reserve for relapse, because high cure rates may achieve with salvage chemotherapy including three or four cycles of bleomycin, etoposide, and cisplatin (BEP) [3, 7, 8].
Although RPNLD has been commonly applied and provided both for diagnosis and therapeutic option, but it may cause some complications, such as perioperative morbidity and loss of antegrade ejaculation. Furthermore there are up to 30% recurrence risk despite the procedure [7, 9, 12]. Therefore, RPNLD is not primarily recommended in several guidelines [10, 13]. Previous studies showed that adjuvant chemotherapy with two cycles of BEP is effective management approach to prevent risk of relapse [13–15], and it is recommended for patients with high-risk CS I NSGCT with relapse-free survival (RFS) in greater than 95% of patients. The most important concerns with respect to adjuvant chemotherapy are toxicity including increased risk for cardiovascular disease, impaired renal function, hearing impairment, and peripheral neuropathy. A single cycle of BEP as an alternative adjuvant protocol has been studied to decrease these toxicities [16–19]. It found that adjuvant chemotherapy with one cycles of BEP was a feasible and safe treatment for patients with CS I NSGCT at high risk of relapse.
No randomized trials have directly compared the survival rates and late toxicity of the three treatment options. The purpose of this study was to evaluate management options and compare outcomes of active surveillance with adjuvant chemotherapy for patients with CS I NSGCT in Turkey. Moreover, the determination of prognostic factors in decision making for postorchiectomy treatment in CS I NSGCT patients with high risk of relapse was also aimed.
Material and methods
A total of 201 patients with histologically confirmed CS I NSGCT who had undergone radical orchiectomy and follow-up at 15 medical oncology centers in Turkey, between October 1999 and November 2013 were included in the this study. Eligibility was limited to patients with only stage IA and IB NSGCT following orchiectomy. Patients were re-staged clinically by clinical examination, abdominopelvic CT and thoracic CT scans following orchiectomy. Elevated tumors markers, β-human chorionic gonadotropin (β-HCG), and α-fetoprotein (AFP) were measured weekly until normalization after orchiectomy. Patients with the persistence of increased postoperative β-HCG levels or postoperative elevation of AFP and those who had insufficient disease information were excluded from data analysis.
After initial diagnosis by the primary pathologist, all pathological slides were reevaluated to confirm the histopathological subtypes by an experienced neuropathologist in all centers. A predominant percentage of embryonal carcinoma was determined as the embryonal carcinoma consisting of more than 50% of the tumor. The age of patients at diagnosis, tumor location, histopathological type, tumor stage, tumor size, the presence of rete testis invasion, vascular invasion, tunica albuginea and vaginalis invasion, preoperative or postoperative β-HCG and AFP levels, cycles of adjuvant treatment, response to treatment, and survival were retrospectively obtained from patient charts after written informed consent was obtained from patients or their relatives. The decision of adjuvant chemotherapy or surveillance was made according to the physicians’ preference for stage IA and IB NSGCT patients in all centers.
Adjuvant treatment
Of the 201 patients with CS I NSGCT, 110 patients (54.7%) were received one or two cycles adjuvant BEP chemotherapy regimen consisting of bleomycin 30 mg daily, day 1, 8, 15, cisplatin 20 mg/m2 daily day 1–5, and etoposide 100 mg/m2 daily day 1–5, every three weekly. Premedication with dexamethasone 8 mg i.v., diphenhydramine 50 mg i.v. and granisetron 3 mg i.v. was given on day 1–5 to prevent emesis on an outpatient basis. Complete blood cell counts, serum biochemistry, and toxicity were evaluated periodically. The majority of patients were treated two cycles BEP regimen (n = 92, 83.6%).
Surveillance and follow-up strategy
Patients on surveillance strategy were followed up with clinical history and physical examination (H&P), AFP and β-HCG every 2 months for first year, every 3 months for second year, and every 6 months for 3–5 years, then annually. Chest X-rays and abdominopelvic CT scan were performed every 6 months for years 2, every 6–12 months for years 3, and then annually for years 4–5. On the other hand, in patients treated with adjuvant chemotherapy, H&P, tumor markers were scheduled every 3 months for first 2 years, every 6 months for up to 5 years, and then annually. Abdominopelvic CT scan was also scheduled every 6 months in the first 2 years, and then annually. Chest X-ray was performed every 6 months for first year, annually for second years, and then was ordered as clinically indicated.
Statistical analysis
The clinicopathological factors of the patients with CS I NSGCT were compared using a Chi-square and Fisher’s exact tests according to the treatment options. The survival analyses and curves were determined using the Kaplan–Meier method and compared with the log-rank test. RFS was defined as the time from orchiectomy to recurrence, or to the date of death or loss to follow-up. Overall survival (OS) was described as the time from diagnosis to the date of the patient’s death or loss to follow-up. Univariate analysis was used to evaluate the significance of clinicopathological indicators as prognostic factors. Thereafter, multivariate analysis with the Cox proportional hazards model was also used in order to find the independent prognostic factors for both RFS and OS. Logistic regression analysis was performed to determine predictive factors for relapse. A 95% confidence interval (CI) was used to quantify the relationship between survival time and each independent factor. All p values were two-sided, and p < 0.05 were considered statistically significant. All data were analyzed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA) software.
Results
Totally, 201 patients with CS I NSGCT, with the median age of patients was 28 years (range 16–59 years), were retrospectively analyzed. The majority of patients were younger than 30 years (62.7%). One-hundred and eight (53.7%) tumors were right-sided, and 92 tumors (45.8%) were left-sided, whereas only one patient presented with a synchronous bilateral NSGCT. The median of maximum tumor diameter was 4 cm (range 0.5–15 cm). Preoperative β-HCG levels were elevated in 79 patients (39.3%; median 10.8 mU/L; range 8.44–5387), and preoperative AFP levels were increased in 44.3% of patients (median 30 ng/mL; 14–6737). After orchiectomy, 150 patients (74.6%) were diagnosed with mixed germ cell tumor and the remaining patients had embryonal carcinoma (15.4%), immature teratoma (5.9%), yolk sac tumor (3.4%) and choriocarcinoma (0.7%), respectively. Sixty-one patients (30.3%) showed a predominant percentage of embryonal carcinoma >50%. The majority of patients (66.2%) were classified as stage IA, while 33.8% of patients were staged as IB at the time of diagnosis. Vascular invasion was detected in 66 patients (33.7%).
Of the 201 patients with CS I NSGCT, 110 (54.7%) received adjuvant chemotherapy, while the remaining 91 patients (45.3%) underwent surveillance. Significant differences were determined between treatment groups with respect to invasion of the tunica albuginea, the presence of predominant embryonal carcinoma component >50%, increased preoperative β-HCG levels, pT stage, clinical stage, the presence of vascular invasion, and relapse (p < 0.001). The prevalence of tunica albuginea involvement (p = 0.002), patients with increased preoperative β-HCG levels (p = 0.004), advanced pT stage (p < 0.001), the rate of clinical stage IB (p < 0.001), the presence of vascular invasion (p < 0.001), and the presence of predominant embryonal carcinoma component >50% (p < 0.001) were significantly higher for adjuvant chemotherapy group than for patients on surveillance. The comparisons of clinicopathological factors with respect to the treatment approaches are shown in Table 1.
At the time of analysis, with a median follow-up period of 34 months (range 8–162 months), relapses were observed in 17 patients (18.3%) on surveillance (47% of cases with the component of embryonal carcinoma >50 and 23.5% of those with vascular invasion) and in one patient (1.2%) treated with adjuvant chemotherapy (with vascular invasion). Relapses were significantly higher for patients underwent surveillance compared to patients treated with adjuvant chemotherapy (18.3 vs. 1.2%, p < 0.001, Table 1).
The majority of relapses were diagnosed in RPLDs (66.6%), while in 27.9% of patients, recurrences were detected as distant metastases. Only marker relapse was detected in one patients (5.5%). The median time to relapse was 14.08 months (range 4–109.6 months). One patient received salvage chemotherapy (TIP; paclitaxel, ifosfamide, cisplatin) who had treated with adjuvant chemotherapy, while 17 patients were treated with BEP chemotherapy in surveillance group. RPLND was performed in seven patients after chemotherapy. Histopathological examination of RPLND specimens revealed necrosis or teratoma. All relapse patients were considered disease-free, except for three patients. These patients received second- or third-line and high-dose chemotherapy, but they died due to disease progression.
The five-year RFS rates for patients who were treated with adjuvant chemotherapy were significantly better than those of patients underwent surveillance (97.6 vs. 80.8%, respectively, p < 0.001, Fig. 1). However, the five-year OS rate for patients on surveillance was not statistically different from adjuvant chemotherapy group (96.1 vs. 100%, p = 0.12). In the univariate analysis for the entire cohort, the presence of vascular invasion (p = 0.01) and treatment option (p < 0.001) were significant prognostic factor for RFS. For OS, the univariate analysis indicated that pT stage (p = 0.004), invasion of rete testis (p = 0.004), and the presence of relapse (p < 0.001) were important prognostic indicators. A multivariate analysis with the Cox proportional hazards model was carried out in order to further evaluate all of the significant prognostic factors that were found in the univariate analysis for RFS. It revealed that the treatment strategy (surveillance vs. adjuvant chemotherapy) was an independent prognostic factor for RFS (p < 0.001, HR 0.54). After that, the multivariate analysis was carried out for OS; any independent prognostic factor could not be found. The results of the univariate and multivariate analyses for RFS are summarized in Tables 2.
A logistic regression analysis was performed in order to further evaluate all of the significant prognostic factors that might predict relapse in patients with CS I NSGCT. It demonstrated that treatment options (p = 0.031, odds ratio (OR): 1.03), EC > 50% (p = 0.013, OR 0.69), and tumor diameter (p = 0.016, OR 1.44) were found to be an independent factor for predicting relapse. Table 3 shows the results of logistic regression analysis.
Discussion
After radical orchiectomy, patients with CS I NSGCT have a relapse risk. On the other hand, some subgroup of these have an increased risk for recurrence [6–8, 20]. These relapses can be successfully managed with chemotherapy or RPNLD, and the majority of patients are cured. In the USA and many European countries, these patients who have an increased risk for relapse are treated with RPLND following orchiectomy, but a randomized trial demonstrated that RPLND resulted in inferior outcomes compared with adjuvant chemotherapy for relapse [13, 21, 22]. Moreover, surveillance, chemotherapy or RPLND for treatment of CS I NSGCT for patients yield similar cancer-specific survival, but there is no uniform consensus [2, 11, 12]. On the other hand, because of the complications of RPLND and the toxicity of chemotherapy, active surveillance policy is a safe and noninvasive approach associated with an excellent cure rate and nearly similar OS rate, especially in patients with low-relapse risk [23, 24].
It has shown that the risk of relapse in CS I NSGCT is substantially related to the presence of LVI. Tumor with LVI has 30–50% of recurrence risk [4–8]. In addition, several retrospective studies have been reported the predominance of EC as a predictive factor for relapse [25, 26]. The rate of metastatic RPLN is reached as 40–50% in patients who has the component of EC >50% in the orchiectomy specimen. RPLN metastases are also diagnosed in most patients with pure EC plus LVI, which results in more recurrence risk [10]. The efficacy of adjuvant chemotherapy with two or one cycles of BEP has been previously documented to prevent risk of relapse, and it is recommended for patients with high-risk CS I NSGCT [14–16]. Therefore, a risk-adapted adjuvant treatment has previously been used [15]. In the present study, the prevalence of patients without LVI was commonly seen in patients who underwent surveillance compared with adjuvant chemotherapy groups, whereas tumors with LVI and the predominant EC component >50% were significantly higher in the adjuvant chemotherapy groups. Our results are thus compatible with the literature [19, 25, 26].
In our study, of the 201 patients with CS I NSGCT, 110 (54.7%) received adjuvant chemotherapy, while the remaining 91 patients (45.3%) underwent active surveillance. Relapse rates were significantly lower for patients treated with adjuvant chemotherapy compared to patients on surveillance (1.2 vs. 18.3%, respectively). The five-year RFS rate for patients who underwent surveillance was worse than that of patients treated with adjuvant chemotherapy (97.6 vs. 80.8%, respectively). However, the five-year OS rate in adjuvant chemotherapy group was also better than that of patients on surveillance (100 vs. 96.1%, respectively), and the difference was not statistically significant. Our results are in accordance with the literature [17, 19, 23, 24].
We detected that the presence of LVI (p = 0.01) and treatment option (p < 0.001) were significant prognostic factors for RFS in the univariate analysis for the entire cohort, whereas pT stage (p = 0.004), invasion of the rete testis (p = 0.004) and the presence of relapse (p < 0.001) were important prognostic indicators for OS. Furthermore, the multivariate analysis showed that only the treatment strategy (surveillance vs. adjuvant chemotherapy) was an independent prognostic factor for RFS (p < 0.001, HR 0.54). But, any independent prognostic factor could not be found for OS in the multivariate analysis. Daugaard et al., in their study, observed 1226 CS I NSGCT, including high-risk patients with LVI [23]. They identified that LVI, presence of EC, and rete testis invasion were three risk factors associated with relapse. In their analysis, presence of LVI together with EC and rete testis invasion was associated with a relapse risk of 50%, whereas if none of the risk factors were present, relapse rate was 12% [23]. They found that 5-year disease-specific survival was 99.3%. Relapse rates in previous studies with respect to surveillance are compatible with our findings [8, 9, 23]. In contrast to their and present studies, in a study carried out by Li et al., prognostic importance of LVI and predominant presence of yolk sac tumor was proved, but not EC predominance [24]. In contrast, only treatment strategy for RFS was found to be an adverse prognostic factor, but any independent prognostic factor could not be found for OS in the multivariate analysis. This might be related to the relatively small and heterogeneous sample size. In the present study, logistic regression analysis identified that treatment options (p = 0.031, OR 1.03), EC >%50 (p = 0.013, OR 0.69), and tumor diameter (p = 0.016, OR 1.44) were a significant predictive factor for relapse in patients with CS I NSGCT.
Previous studies recommend active surveillance for all CS I NSGCT patients irrespective of risk factors [26, 27]. Surveillance remains an acceptable management for patients without LVI, because 85% of them are cured after orchiectomy. However, the disadvantage of surveillance is possible overtreatment in relapse time due to requiring of 3 or 4 cycles of salvage chemotherapy. Therefore, one or two course of BEP chemotherapy is recommended for patients with high-risk CS I NSGCT [14–16]. Although the gain is less in patients without LVI, one cycle of BEP chemotherapy close to eradicate the risk of relapse later being exposed to salvage chemotherapy. Recently, SWENOTECA group reported mature and expanded results of one course of adjuvant BEP in patients with CS I NSGCT [17]. They found that the relapse rate was 3.2% for patients with LVI and 1.6% in patients without LVI at 5 years. Thereafter, the authors recommended that one course of adjuvant BEP should be considered standard treatment in CS NSGCT with LVI; in addition, it is also a management option together with surveillance for patients without LVI [17]. In our study, after one or two cycles of adjuvant BEP, the relapse rate was 1.2% in accordance with the literature [17, 19].
The current study has several limitations. The retrospective nature and short follow-up interval are important limitation, which might have influenced the results. The other limitation of this study is also the relatively small sample size. Although our findings need confirmation by further investigations including larger sample sizes that compare two treatment options for CS I NSGCT, we believe that our study is noteworthy and these results contribute to the knowledge of this disease because distinct prognostic factors were for predicting relapse by logistic regression analysis, as a different from previous results in the literature.
In conclusion, our study indicates that adjuvant BEP chemotherapy is associated with significant improvement in RFS compared with active surveillance in CS I NSGCT after orchiectomy. Moreover, treatment preference is an important prognostic factor for RFS and treatment preference; EC predominance and tumor diameter are predictive factor for relapse. Although adjuvant chemotherapy provides the significant advantage for RFS, the OS rates were similar for the two treatment options. Therefore, the surveillance strategy is still safe and feasible management approach with an excellent cure rate after radical orchiectomy in men with CS I NSGCT, especially without risk factors. Further studies are needed that analyze new risk factors for relapse and compare all treatment options according to the risk-adapted approach.
References
Bhardwa JM, Powles T, Berney D, Baithun S, Nargund VH, Oliver RT (2005) Assessing the size and stage of testicular germ cell tumours: 1984–2003. BJU Int 96:819–821
Cohn-Cedermark G, Stahl O, Tandstad T (2015) Surveillance vs. adjuvant therapy of clinical stage I testicular tumors—a review and the SWENOTECA experience. Andrology 3:102–110
Vergouwe Y, Steyerberg EW, Eijkemans MJ, Albers P, Habbema JD (2003) External validity of a prediction rule for residual mass histology in testicular cancer: an evaluation for good prognosis patients. Br J Cancer 88:843–847
Klepp O, Olsson AM, Ous S, Nilsson S, Høisaether PA, Tveter K (1991) Early clinical stages of nonseminomatous testis cancer. Evaluation of the primary treatment and follow-up procedures of the SWENOTECA project. Scand J Urol Nephrol 25:179–190
Pont J, Albrecht W, Postner G, Sellner F, Angel K, Höltl W (1996) Adjuvant chemotherapy for high-risk clinical stage I nonseminomatous testicular germ cell cancer: long-term results of a prospective trial. J Clin Oncol 14:441–448
Daugaard G, Petersen PM, Rørth M (2003) Surveillance in stage I testicular cancer. APMIS 111:76–83 (discussion 83-5)
Kollmannsberger C, Moore C, Chi KN, Murray N, Daneshmand S, Gleave M, Hayes-Lattin B, Nichols CR (2010) Non-risk-adapted surveillance for patients with stage I nonseminomatous testicular germ-cell tumors: diminishing treatment-related morbidity while maintaining efficacy. Ann Oncol 21:1296–1301
Sturgeon JF, Moore MJ, Kakiashvili DM, Duran I, Anson-Cartwright LC, Berthold DR, Warde PR, Gospodarowicz MK, Alison RE, Liu J, Ma C, Pond GR, Jewett MA (2011) Non-risk-adapted surveillance in clinical stage I nonseminomatous germ cell tumors: the Princess Margaret Hospital’s experience. Eur Urol 59:556–562
Hermans BP, Sweeney CJ, Foster RS, Einhorn LE, Donohue JP (2000) Risk of systemic metastases in clinical stage I nonseminoma germ cell testis tumor managed by retroperitoneal lymph node dissection. J Urol 163:1721–1724
Albers P, Albrecht W, Algaba F, Bokemeyer C, Cohn-Cedermark G, Fizazi K, Horwich A, Laguna MP, Nicolai N, Oldenburg J (2015) Guidelines on testicular cancer: 2015 update. Eur Urol 68:1054–1068
Nallu A, Mannuel HD, Hussain A (2013) Testicular germ cell tumors: biology and clinical update. Curr Opin Oncol 25:266–272
Rassweiler JJ, Scheitlin W, Heidenreich A, Laguna MP, Janetschek G (2008) Laparoscopic retroperitoneal lymph node dissection: does it still have a role in the management of clinical stage I nonseminomatous testis cancer? A European perspective. Eur Urol 54:1004–1015
Beyer J, Albers P, Altena R, Aparicio J, Bokemeyer C, Busch J, Cathomas R, Cavallin-Stahl E, Clarke NW, Claßen J, Cohn-Cedermark G, Dahl AA, Daugaard G, De Giorgi U, De Santis M, De Wit M, De Wit R, Dieckmann KP, Fenner M, Fizazi K, Flechon A, Fossa SD, Germá Lluch JR, Gietema JA, Gillessen S, Giwercman A, Hartmann JT, Heidenreich A, Hentrich M, Honecker F, Horwich A, Huddart RA, Kliesch S, Kollmannsberger C, Krege S, Laguna MP, Looijenga LH, Lorch A, Lotz JP, Mayer F, Necchi A, Nicolai N, Nuver J, Oechsle K, Oldenburg J, Oosterhuis JW, Powles T, Rajpert-De Meyts E, Rick O, Rosti G, Salvioni R, Schrader M, Schweyer S, Sedlmayer F, Sohaib A, Souchon R, Tandstad T, Winter C, Wittekind C (2013) Maintaining success, reducing treatment burden, focusing on survivorship: highlights from the third European consensus conference on diagnosis and treatment of germ-cell cancer. Ann Oncol 24:878–888
Cullen MH, Stenning SP, Parkinson MC, Fossa SD, Kaye SB, Horwich AH, Harland SJ, Williams MV, Jakes R (1996) Short-course adjuvant chemotherapy in high-risk stage I nonseminomatous germ cell tumors of the testis: a Medical Research Council report. J Clin Oncol 14:1106–1113
Tandstad T, Dahl O, Cohn-Cedermark G, Cavallin-Stahl E, Stierner U, Solberg A, Langberg C, Bremnes RM, Laurell A, Wijkstrøm H, Klepp O (2009) Risk-adapted treatment in clinical stage I nonseminomatous germ cell testicular cancer: the SWENOTECA management program. J Clin Oncol 27:2122–2128
Cullen M (2012) Surveillance or adjuvant treatments in stage 1 testis germ-cell tumours. Ann Oncol 23(Suppl 10):x342–x348
Tandstad T, Ståhl O, Håkansson U, Dahl O, Haugnes HS, Klepp OH, Langberg CW, Laurell A, Oldenburg J, Solberg A, Söderström K, Cavallin-Ståhl E, Stierner U, Wahlquist R, Wall N, Cohn-Cedermark G (2014) SWENOTECA. One course of adjuvant BEP in clinical stage I nonseminoma mature and expanded results from the SWENOTECA group. Ann Oncol 25:2167–2172
Westermann DH, Schefer H, Thalmann GN, Karamitopoulou-Diamantis E, Fey MF, Studer UE (2008) Long-term followup results of 1 cycle of adjuvant bleomycin, etoposide and cisplatin chemotherapy for high risk clinical stage I nonseminomatous germ cell tumors of the testis. J Urol 179:163–166
Vidal AD, Thalmann GN, Karamitopoulou-Diamantis E, Fey MF, Studer UE (2015) Long-term outcome of patients with clinical stage I high-risk nonseminomatous germ-cell tumors 15 years after one adjuvant cycle of bleomycin, etoposide, and cisplatin chemotherapy. Ann Oncol 26:374–377
Shin YS, Kim HJ (2013) Current management of testicular cancer. Korean J Urol 54:2–10
Stephenson AJ, Bosl GJ, Motzer RJ, Kattan MW, Stasi J, Bajorin DF, Sheinfeld J (2005) Retroperitoneal lymph node dissection for nonseminomatous germ cell testicular cancer: impact of patient selection factors on outcome. J Clin Oncol 23:2781–2788
Albers P, Siener R, Krege S, Schmelz HU, Dieckmann KP, Heidenreich A, Kwasny P, Pechoel M, Lehmann J, Kliesch S, Köhrmann KU, Fimmers R, Weissbach L, Loy V, Wittekind C, Hartmann M (2008) Randomized phase III trial comparing retroperitoneal lymph node dissection with one course of bleomycin and etoposide plus cisplatin chemotherapy in the adjuvant treatment of clinical stage I Nonseminomatous testicular germ cell tumors: AUO trial AH 01/94 by the German Testicular Cancer Study Group. J Clin Oncol 26:2966–2972
Daugaard G, Gundgaard MG, Mortensen MS, Agerbæk M, Holm NV, Rørth M, von der Maase H, Christensen IJ, Lauritsen J (2014) Surveillance for stage I nonseminoma testicular cancer: outcomes and long-term follow-up in a population-based cohort. J Clin Oncol 32:3817–3823
Li X, Guo S, Wu Z, Dong P, Li Y, Zhang Z, Yao K, Han H, Qin Z, Zhou F, Liu Z (2015) Surveillance for patients with clinical stage I nonseminomatous testicular germ cell tumors. World J Urol 33:1351–1357
Groll RJ, Warde P, Jewett MA (2007) A comprehensive systematic review of testicular germ cell tumor surveillance. Crit Rev Oncol Hematol 64:182–197
Atsü N, Eskiçorapçi S, Uner A, Ekici S, Güngen Y, Erkan I, Uygur MC, Ozen H (2003) A novel surveillance protocol for stage I nonseminomatous germ cell testicular tumours. BJU Int 92:32–35
Nichols CR, Roth B, Albers P, Einhorn LH, Foster R, Daneshmand S, Jewett M, Warde P, Sweeney CJ, Beard C, Powles T, Tyldesley S, So A, Porter C, Olgac S, Fizazi K, Hayes-Lattin B, Grimison P, Toner G, Cathomas R, Bokemeyer C, Kollmannsberger C (2013) Active surveillance is the preferred approach to clinical stage I testicular cancer. J Clin Oncol 31:3490–3493
Authors’ contribution
A. B. involved in protocol/project development. All authors helped for data collection or management. A. B. and M. G. involved in data analysis, wrote the manuscript, and edited the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This manuscript was not supported by any financial or other relationships. The authors declare that they have no conflict of interest.
Ethical standards
The study was approved by the local ethics committee of hospitals, and the informed written consents were obtained from each patient or their relatives.
Rights and permissions
About this article
Cite this article
Gumus, M., Bilici, A., Odabas, H. et al. Outcomes of surveillance versus adjuvant chemotherapy for patients with stage IA and IB nonseminomatous testicular germ cell tumors. World J Urol 35, 1103–1110 (2017). https://doi.org/10.1007/s00345-016-1964-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1964-6