Abstract
Purpose
To evaluate the factors affecting complication rates of flexible ureteroscopy and laser lithotripsy (FURSL).
Materials and methods
Data on a total of 1395 patients, with 1411 renal units underwent 1571 procedures with FURSL for renal and/or proximal ureteral stones between April 2012 and January 2016, were retrospectively analyzed. Complications were assessed using the Satava and modified Clavien systems. Univariate and multivariate analyses were done to determine predictive factors affecting complication rates.
Results
The mean patient age in the total procedures was 45.68 ± 14.00 years (range 2–86 years), and the mean stone size was 15.15 ± 8.32 mm (range 5–75 mm). The overall success rate was 95.6 %. A total of 209 (13.3 %) cases suffered from complications with intraoperative complications rates of 5.9 % and postoperative complication rates of 7.3 %. Univariate analysis revealed no significant difference in complication rates in respect of age, gender, body mass index, use of ureteral access sheath, operation time, bleeding disorder, solitary kidney, preoperative stenting, American Society of Anesthesiologists score, repeated procedure or location of stones (all p value >0.05). Complication rates were determined to be significantly affected by stone size (p = 0.026), multiplicity (p = 0.028) and the presence of congenital renal abnormality (p < 0.01). The only significant factor in multivariate analysis was the presence of congenital renal abnormalities (p = 0.02).
Conclusions
The results of the current study indicated that stone size, stone number and the presence of congenital renal abnormalities were factors affecting complication rates after FURSL, although congenital renal abnormality was the only independent predictor among these risk factors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the last quarter of the twentieth century, treatment options for upper urinary tract stones shifted from open to minimally invasive techniques. Developments in technology and in minimally invasive treatment modalities have enabled a stone-free status to be achieved more rapidly, with greater patient comfort. The miniaturization of endoscopic devices, the increased quality of optic systems, the advent of holmium laser use and increased experience in endoscopic surgery have all played an important role in this change [1].
In recent years worldwide, flexible ureteroscopy and laser lithotripsy (FURSL) has gradually become a very impressive treatment option for the majority of upper urinary tract stones. FURSL is currently approved as an effective and minimally invasive procedure, achieving higher stone-free rates than extracorporeal shock wave lithotripsy (SWL) and lower morbidity than percutaneous nephrolithotomy (PNL), and therefore, the use of FURSL has been increasing continuously independent of stone size and position [2]. Moreover, a number of recent studies have reported that FURSL provides a higher stone-free rate with low morbidity, shorter hospital stay, better patient comfort, a faster return to daily activities in larger calculi and in some urology departments it is used as the first-choice treatment in renal stones requiring active treatment [3–5].
However, minimally invasive a treatment option ureteroscopic stone removal (URS) may be, and complication rates of 9–25 % have been reported in literature [6–8]. Although semirigid URS complications have been reported in several large retrospective series [6, 7], there have been few prospective studies of the outcomes and complications of both semirigid and FURSL [9] and only one study [10] (on a limited number of patients) that focused on FURSL complications only. In addition, most of these reported studies have been multi-institutional and multisurgeon applications with no standardized complication classification methods. Some have reported these complications in chronological order (intraoperative and postoperative), while others have recorded them by severity (minor and major). In the present study, the FURSL experience (in proximal ureteral and renal stones) in our clinic is presented primarily focusing on factors affecting complication rates in a single-center large patient population, using the validated classification system of Satava [11] and the modified Clavien system [12].
Materials and methods
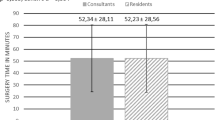
Patients
Approval for the study was granted by the Local Ethics Committee of Dıskapı Yıldırım Beyazıt Training and Research Hospital (decision no. 29/21). A total of 1395 patients in our clinical department, with 1411 renal units, underwent 1571 procedures with flexible ureterorenoscopy and laser lithotripsy for renal and/or proximal ureteral stones between April 2012 and January 2016. This study was conducted in a single center with multisurgeons including experienced urologists and those in training. Data were collected retrospectively from the hospital medical databases. All patients were evaluated according to the following criteria: medical history, physical examination, complete blood count, plasma urea and creatinine values, coagulation profiles, urinalysis and urine cultures, and imaging methods (plain radiograph, ultrasonography, intravenous urography and/or computed tomography). A preoperative negative urine culture was required before surgery, so any positive urine cultures were treated with the appropriate antibiotics. Antibiotic prophylaxis was routinely given in all cases. Stone size was recorded as the maximum length of the stone. In cases of multiple calculi, stone size was defined as the sum of the longest axis of each stone.
Data on baseline characteristics, intraoperative details and postoperative outcomes were evaluated, and analysis was focused on complications (either intraoperative or postoperative). Intraoperative complications were assessed using the Satava classification system [11], and postoperative complications were graded according to the modified Clavien system [12]. Patients undergoing diagnostic ureteroscopy, therapeutic procedures other than urinary stones and ureteroscopic procedures using a semirigid device only were excluded from the study.
Surgical technique
All procedures were performed under general anesthesia using the technique previously described by the authors [13]. Rigid ureteroscopy was routinely performed before flexible ureteroscopy for the optical dilatation. The use of ureteral access sheaths (9.5/11.5 F or 11/13 F) depended on the surgeon’s preference according to patient and stone characteristics. If the rigid/flexible ureteroscope could not be advanced easily, a JJ stent was placed for approximately 1–2 weeks before repeating the procedure. Active ureteral orifice dilation was not applied to any patient. Standard retrograde FURSL was applied with a 7.5 F flexible ureteroscope (Karl Storz, Flex X2, GmbH, Tuttlingen, Germany). Stone fragmentation was achieved using a holmium laser (Dornier MedTech GmbH, Medilas H20 or H30, Wessling, Germany) with 200- or 365-μm laser fibers. During the period of the study, 16 flexible ureteroscopes and 64 laser fibers were used. Any JJ stent placed at the end of the procedure based on the surgeon’s discretion was removed approximately 7–21 days postoperatively.
Follow-up
Patients were assessed with plain radiography and/or ultrasound or computed tomography abdominal scan. Asymptomatic stones <3 mm in size were considered to be clinically insignificant urolithiasis (CIRFs). Patients who were stone-free 1 month postoperatively were evaluated as successful.
Statistical analysis
Analysis of the study data was applied using SPSS 16.0 package program. All data were descriptive based on frequencies and calculated based on the total procedures. Factors possibly affecting complications were analyzed with the Chi-square test and the independent samples t test. Parameters that were statistically significant on univariate analysis were evaluated by multivariate logistic regression analysis. A value of p < 0.05 was accepted as statistically significant.
Results
Patient and stone characteristics
A total of 1395 patients with 1411 renal units underwent 1571 procedures. A single procedure was applied to 1284 (91 %) renal units, 2 sessions were indicated in 94 (6.7 %), and 3 sessions were indicated in 33 (2.3 %). The male/female ratio in the total procedures was 1023 (65.12 %)/548 (34.88 %), the mean patient age was 45.68 ± 14.00 years (range 2–86 years), and the mean stone size was 15.15 ± 8.32 mm (range 5–75 mm). From the total 1571 procedures, 1167 (74.29 %) had only renal stones, 329 (20.94 %) had only ureteral stones, and 75 (4.77 %) had both types of stone. The most frequent primary location of the stones was in the lower calix (26.0 %), followed by the proximal ureter (20.9 %), pelvis (19.2 %), multicaliceal (11.7 %), middle calix (11.2 %), upper calix (6.0 %) and both kidney and ureter (4.77 %). The incidence of congenital renal abnormality was low at 2.9 %. Surgery was applied to five patients during antiplatelet therapy, and bleeding diathesis was determined in six patients. The baseline demographics, stone characteristics and clinical details of the patients are presented in Table 1.
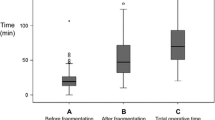
Operative findings
The mean operating time was 45.86 ± 16.46 min (range 10–150 min), and the mean fluoroscopy screening time was 41.62 ± 49.65 s (range 0–480 s). A JJ stent was placed preoperatively in 152 (9.6 %) cases, and ureteral access sheaths were used in 1255 (79.8 %) cases. In the majority of cases (80.9 %), a JJ stent was inserted at the end of the procedure. The mean hospital stay was 1.05 ± 0.48 days (range 1–14 days). The overall success rate was 95.6, 86.4 % of cases were stone-free, and 9.2 % had CIRFs. Perioperative and postoperative outcomes are summarized in Table 2.
Complications
A total of 209 (13.3 %) cases suffered from complications in 1571 procedures (Table 3). The overall incidence of intraoperative complications was 5.9 %. The most common complications were bleeding (2.5 %) and mucosal injury (2.3 %). Severe bleeding occured in nine (0.5 %) cases, necessitating a secondary ureteroscopy because of the premature termination of the procedure. Perforation (which required JJ stent insertion) and malfunctioning or breakage of instruments were determined at a low incidence of 0.3 and 0.1 %, respectively. According to the modified Satava classification system, there were 5 % grade I and 0.9 % grade IIb complications. There were no grade III complications in this series.
The postoperative complication rate was 7.3 %. The majority of complications were Clavien grade I or II (5.8 % of patients). Major complications developed in 25 (1.6 %) patients. Perirenal abscess requiring percutaneous drainage (one case; 0.06 %) (Clavien IIIa), stent migration (eleven cases; 0.7 %) (Clavien IIIb), steinstrasse (nine cases; 0.6 %) (Clavien IIIb), sepsis (one case; 0.06 %) (Clavien IV) and death (one case; 0.06 %) (Clavien V) due to urosepsis were the major complications. Late complications included ureteral stenosis (Clavien IIIb) in two cases. One of these cases was determined at 6 months postoperatively on readmission due to flank pain and detected ureteropelvic stenosis. This case was treated with laser ureteroscopic endopyelotomy. The other case was treated with open ureteroneocystostomy due to ureterovesical junction stenosis which was detected at postoperative 12 months.
Data analysis
The procedure and stone characteristics were compared according to the presence or absence of complications. Univariate analysis revealed no significant difference in complication rates in respect of age, gender, body mass index (BMI), use of ureteral access sheath, operation time, bleeding disorder, solitary kidney, preoperative stenting, American Society of Anesthesiologists (ASA) score, repeated procedure or location of stones (all p value >0.05). Complication rates were determined to be significantly affected by stone size (p = 0.026), multiplicity (p = 0.028) and the presence of congenital renal abnormality (p < 0.01) (Table 4). The only significant factor in multivariate analysis was the presence of congenital renal abnormalities (p = 0.02). Complications with congenital abnormalities are summarized in Table 5.
Discussion
The results of the current study indicated that stone size, stone number and the presence of congenital renal abnormalities were factors affecting complication rates after FURSL, although congenital renal abnormality was the only independent predictor among these risk factors. Other prognostic factors of patient age, gender, BMI, ASA status, solitary kidney, operation time or location of stones were not determined as significant predictors of complications rates. A larger stone size (especially >30 mm) was observed to be associated with a higher complication rate. In addition, multiple procedures may be required for larger stones. However, the need for repeated procedures was not a significant predictor of complications rates. These results were consistent with current literature [14–17]. However, the URS complication rates reported in literature have generally been based on series where semirigid URS has been applied ureter stones [6–8]. To the best of our knowledge, there has been no large study focusing on the factors that affect complications in FURSL. Therefore, this is the first large single-center study on this topic.
In the current series, the overall success rate was 95.6 %, which is similar to published series [4, 9, 10, 17]. A total of 209 (13.3 %) cases suffered from complications in this series with intraoperative complications rates of 5.9 % and postoperative complication rates of 7.3 %. In a recent study by the Clinical Research Office of the Endourological Society, a prospective examination was made of the data of 11,885 patients (1852 had only renal stones, 8676 had only ureteral stones, and 1145 patients had both types of stone) to whom ureteroscopy was applied in 114 centers in 32 countries [9]. However, in that study, semirigid URS was primarily used (73.9 %), followed by flexible URS (15.0 %) or a combination of both techniques (10.7 %). The postoperative complication rate was reported as 3.5 %, and the majority of which were Clavien grade I or II (2.8 % of patients). Intraoperative complications were also reported separately, including bleeding (1.4 %), perforation (1.0 %), ureteral avulsion (0.1 %) and conversion to open surgery (0.1 %). The most frequent complication in that series was fever (1.8 %). Bleeding was reported at 0.4 %, and a blood transfusion was required in 0.2 % of patients. In addition, urinary tract infection (UTI) was observed in 116 (1 %) patients, sepsis in 38 (0.3 %), and mortality was reported in 5 patients for various other reasons.
In the current series, mucosal injury (Satava grade I) was detected in 37 (2.3 %) patients. Ureteral perforation (Satava grade IIb), which was treated successfully with the placement of a JJ stent, was also observed in five (0.3 %) patients. The most common intraoperative complication observed in the current study was bleeding (2.5 %), although transfusion was not required. However, in nine (0.6 %) patients, severe bleeding (Satava grade IIb) was observed which impaired the intraoperative view and as the procedure was terminated early, a second application session was required. The most frequently observed postoperative complication in the current study was fever (5.3 %) (Clavien grade I). UTI (Clavien grade II) was observed in 42 (2.7 %) patients, which was similar to rates reported in literature.
Although the vast majority of complications were minor and the majority of these were observed to be successfully treated, major complications also developed in the current series. Steinstrasse was observed in nine (0.6 %) cases (Clavien IIIb) and one (0.06 %) patient required percutaneous drainage due to perirenal abscess (Clavien IIIa). Urosepsis and death are the most serious complications of this procedure. In the current series, urosepsis was observed in two patients and this resulted in death in one case. Avulsion and strictures are rare (<1 %) following FURSL [18]. No ureteral avulsion was observed in any patient in the current study, but ureteral narrowness developed in two patients. In the first of these cases, ureteropelvic junction stenosis was determined in tests applied at 6 months postoperatively due to symptomatic flank pain and was treated with retrograde laser endopyelotomy. In the other case, ureterovesical stenosis which developed 1 year postoperatively was treated with ureteroneocystostomy.
In the current study, postoperative JJ stent was used in 80.9 % of cases and this result was similar to current literature [19, 20]. Routine stenting after an uncomplicated procedure is not mandatory, and it might be associated with higher postoperative morbidity (stent-related symptoms). Another reason for questioning routine postoperative stenting is that anesthesia is required for removal, particularly in children. There may also sometimes be migration which then needs a secondary procedure. Stent migration was observed in 11 cases (0.7 %) in the current study. However, stent-related complications were not reported in this series, owing to the retrospective nature as a limitation.
The FURSL procedure can be safely used in difficult cases such as those with horseshoe kidney, pelvic kidney and calix diverticular stones which severely limit or prevent the application of other minimally invasive treatment options [21–23]. Atis et al. [21] applied FURSL to 25 stones of 20 patients with horseshoe kidney and reported a total complication rate of 25 %, all of which were minor. In another series where FURSL was applied to 26 pelvic ectopic kidneys, minor postoperative complications were observed in 5 patients (renal colic (n = 2), persistent hematuria (n = 1), fever (n = 1) and UTI (n = 1)) [23]. In a multicenter FURSL series of 25 patients with calix diverticular stones, the complication rate was reported as 20 % [22]. In the current study, FURSL was applied to 47 units of congenital renal abnormality (bifid pelvis (n = 1), complete ureteral duplication (n = 9), calyceal diverticula (n = 18), horseshoe kidney (n = 15), pelvic ectopia (n = 2) and malrotation (n = 2)). In this series, congenital renal abnormality was determined to be the only significant predictor of FURSL complications in multivariate logistic regression analysis. Similarly, Resorlu et al. [17] reported that congenital renal anomaly had negative effect on FURSL results.
In patients with uncorrected bleeding diathesis, FURSL remains the only potential surgical treatment alternative due to the absolute contraindication to other minimally invasive treatment options. Watterson et al. [24] applied FURSL to the kidney stones of 25 patients with bleeding diathesis or who were receiving anticoagulant treatment, and it was reported that retroperitoneal hematoma developed at a level requiring transfusion in only 1 patient and no additional intervention was required. Turna et al. [25] compared the results of FURSL applied for kidney stones to 37 patients who were receiving anticoagulant treatment with those of 37 patients not receiving any anticoagulant treatment, and no difference was determined between the two groups in respect of treatment success, and intraoperative and postoperative complications with hemorrhagic or thromboembolic events. In the current study, FURSL was applied to five patients receiving anticoagulant treatment and six patients with bleeding diathesis, and similar to the previous studies, no increase was observed in the complication rates. In the univariate analysis applied, no correlation was determined between complications and bleeding diathesis.
The use of ureteral access sheaths is recommended as it facilitates repeated ureteroscopic interventions, reduces trauma to a minimum, reduces costs by extending the life of the flexible ureterorenoscope, reduces pressure within the kidney and shortens operating time [26, 27]. Traxer and Thomas [28] applied FURSL to a series of 359 cases in 2 centers using ureteral access sheaths of 12/14 Fr diameter with a digital ureteroscope and reported that ureteral wall injury developed in 167 (46.5 %) patients. While male gender and elderly age were determined as risk factors of severe ureteral wall damage, the most significant risk factor was reported to be absence of preoperative stenting and patients with not pre-stenting were determined to be at a sevenfold greater risk of ureteral wall damage. In another study where digital ureteroscope was used, a slight increase in complications was observed associated with overuse of a guide for ureteral access [29].
In the current study, ureteral access sheaths were used in 80 % of cases and not in 20 %. In contrast to the above-mentioned studies, no relationship was determined in the current study between the use of ureteral access sheaths and complications. However, in the previous studies, all the procedures were applied with relatively wider diameter digital ureteroscopes and large diameter (12/14 Fr) ureteral access guides compatible with these thicker ureteroscopes. In addition, during the FURSL procedure, the guide wires were placed using cystoscopy only, ureteral dilatation was achieved using a semirigid ureteroscope, and it must be taken into consideration that potential concomitant pathologies such as ureteral folds and narrowness were not evaluated. On the other hand, although some studies have shown that the preoperative placement of a stent reduced complications [28, 30], no difference was determined in the current study. This can be attributed to the finer instruments used and the above-mentioned reasons.
However, the results are dependent on the retrospective application, which constitutes the major limitation of the present study. Other limitations are unknown stone composition, information about the HU of the stones and the absence of long-term follow-up. Additionally, there is heterogeneity in imaging used to determine stone-free status. Despite the limitations, the current study was the largest series on this topic and these results provide useful insight for clinicians and patients about the complications of this procedure.
Conclusions
For daily endourological routine, FURSL is an effective and safe procedure for upper urinary tract stones treatment. However, it should be noted that the complication rate increases with high stone burden and multiple stones. Additionally, a higher incidence of complication rates should not be overlooked in patients with congenital renal abnormalities.
The results of this study demonstrate that stone size, stone numbers and the presence of congenital renal abnormalities were determined as factors affecting complication rates after FURSL. Of these risk factors, congenital renal abnormality was the only independent predictor. Nonetheless, there is a need for further, large prospective studies to confirm these findings.
Abbreviations
- FURSL:
-
Flexible ureterorenoscopy and laser lithotripsy
- SWL:
-
Shock wave lithotripsy
- PNL:
-
Percutaneous nephrolithotomy
- URS:
-
Ureteroscopic stone removal
- CIRFs:
-
Clinically insignificant urolithiasis
- BMI:
-
Body mass index
- ASA:
-
American Society of Anesthesiologists
- UTI:
-
Urinary tract infection
References
Breda A, Ogunyemi O, Leppert JT, Lam JS, Schulam PG (2008) Flexible ureteroscopy and laser lithotripsy for single intrarenal stones 2 cm or greater–is this the new frontier? J Urol 179(3):981–984. doi:10.1016/j.juro.2007.10.083
Unsal A, Resorlu B, Atmaca AF, Diri A, Goktug HN, Can CE, Gok B, Tuygun C, Germiyonoglu C (2012) Prediction of morbidity and mortality after percutaneous nephrolithotomy by using the Charlson Comorbidity Index. Urology 79(1):55–60. doi:10.1016/j.urology.2011.06.038
Aboumarzouk OM, Monga M, Kata SG, Traxer O, Somani BK (2012) Flexible ureteroscopy and laser lithotripsy for stones >2 cm: a systematic review and meta-analysis. J Endourol 26(10):1257–1263. doi:10.1089/end.2012.0217
Breda A, Ogunyemi O, Leppert JT, Schulam PG (2009) Flexible ureteroscopy and laser lithotripsy for multiple unilateral intrarenal stones. Eur Urol 55(5):1190–1196. doi:10.1016/j.eururo.2008.06.019
Giusti G, Proietti S, Luciani LG, Peschechera R, Giannantoni A, Taverna G, Sortino G, Graziotti P (2014) Is retrograde intrarenal surgery for the treatment of renal stones with diameters exceeding 2 cm still a hazard? Can J Urol 21(2):7207–7212
Geavlete P, Georgescu D, Nita G, Mirciulescu V, Cauni V (2006) Complications of 2735 retrograde semirigid ureteroscopy procedures: a single-center experience. J Endourol 20(3):179–185. doi:10.1089/end.2006.20.179
PerezCastro E, Osther PJ, Jinga V, Razvi H, Stravodimos KG, Parikh K, Kural AR, de la Rosette JJ, Group CUGS (2014) Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global study. Eur Urol 66(1):102–109. doi:10.1016/j.juro.2007.09.107
Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, Knoll T, Lingeman JE, Nakada SY, Pearle MS, Sarica K, Turk C, Wolf JS Jr, Panel EANG (2007) 2007 guideline for the management of ureteral calculi. J Urol 178(6):2418–2434. doi:10.1016/j.juro.2007.09.107
DelaRosette J, Denstedt J, Geavlete P, Keeley F, Matsuda T, Pearle M, Preminger G, Traxer O, Group CUS (2014) The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. J Endourol 28(2):131–139. doi:10.1089/end.2013.0436
Oguz U, Resorlu B, Ozyuvali E, Bozkurt OF, Senocak C, Unsal A (2014) Categorizing intraoperative complications of retrograde intrarenal surgery. Urol Int 92(2):164–168. doi:10.1159/000354623
Satava RM (2005) Identification and reduction of surgical error using simulation. Minim Invasive Ther Allied Technol 14(4):257–261. doi:10.1080/13645700500274112
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bas O, Bakirtas H, Sener NC, Ozturk U, Tuygun C, Goktug HN, Imamoglu MA (2014) Comparison of shock wave lithotripsy, flexible ureterorenoscopy and percutaneous nephrolithotripsy on moderate size renal pelvis stones. Urolithiasis 42(2):115–120. doi:10.1007/s00240-013-0615-2
Best SL, Nakada SY (2011) Flexible ureteroscopy is effective for proximal ureteral stones in both obese and nonobese patients: a two-year, single-surgeon experience. Urology 77(1):36–39. doi:10.1016/j.urology.2010.05.001
Giusti G, Proietti S, Cindolo L, Peschechera R, Sortino G, Berardinelli F, Taverna G (2015) Is retrograde intrarenal surgery a viable treatment option for renal stones in patients with solitary kidney? World J Urol 33(3):309–314. doi:10.1007/s00345-014-1305-6
Guzel O, Tuncel A, Balci M, Karakoyunlu N, Aslan Y, Erkan A, Senel C (2016) Retrograde intrarenal surgery is equally efficient and safe in patients with different American Society of Anesthesia physical status. Ren Fail 38(4):503–507. doi:10.3109/0886022X.2016.1144248
Resorlu B, Unsal A, Gulec H, Oztuna D (2012) A new scoring system for predicting stone-free rate after retrograde intrarenal surgery: the “resorlu-unsal stone score”. Urology 80(3):512–518. doi:10.1016/j.urology.2012.02.072
Türk C, Knoll T, Petrik A, Sarica K, Skolarikos A, Straub M, Seitz C (2012) Guidelines on urolithiasis. European Association of Urology, Arnhem
Nabi G, Cook J, N’Dow J, McClinton S (2007) Outcomes of stenting after uncomplicated ureteroscopy: systematic review and meta-analysis. BMJ 334(7593):572. doi:10.1136/bmj.39119.595081.55
Song T, Liao B, Zheng S, Wei Q (2012) Meta-analysis of postoperatively stenting or not in patients underwent ureteroscopic lithotripsy. Urol Res 40(1):67–77. doi:10.1007/s00240-011-0385-7
Atis G, Resorlu B, Gurbuz C, Arikan O, Ozyuvali E, Unsal A, Caskurlu T (2013) Retrograde intrarenal surgery in patients with horseshoe kidneys. Urolithiasis 41(1):79–83. doi:10.1007/s00240-012-0534-7
Bas O, Ozyuvali E, Aydogmus Y, Sener NC, Dede O, Ozgun S, Hizli F, Senocak C, Bozkurt OF, Basar H, Imamoglu A (2015) Management of calyceal diverticular calculi: a comparison of percutaneous nephrolithotomy and flexible ureterorenoscopy. Urolithiasis 43(2):155–161. doi:10.1007/s00240-014-0725-5
Bozkurt OF, Tepeler A, Sninsky B, Ozyuvali E, Ziypak T, Atis G, Daggulli M, Resorlu B, Caskurlu T, Unsal A (2014) Flexible ureterorenoscopy for the treatment of kidney stone within pelvic ectopic kidney. Urology 84(6):1285–1289. doi:10.1016/j.urology.2014.07.041
Watterson JD, Girvan AR, Cook AJ, Beiko DT, Nott L, Auge BK, Preminger GM, Denstedt JD (2002) Safety and efficacy of holmium: YAG laser lithotripsy in patients with bleeding diatheses. J Urol 168(2):442–445
Turna B, Stein RJ, Smaldone MC, Santos BR, Kefer JC, Jackman SV, Averch TD, Desai MM (2008) Safety and efficacy of flexible ureterorenoscopy and holmium: YAG lithotripsy for intrarenal stones in anticoagulated cases. J Urol 179(4):1415–1419. doi:10.1016/j.juro.2007.11.076
L’Esperance JO, Ekeruo WO, Scales CD Jr, Marguet CG, Springhart WP, Maloney ME, Albala DM, Preminger GM (2005) Effect of ureteral access sheath on stone-free rates in patients undergoing ureteroscopic management of renal calculi. Urology 66(2):252–255. doi:10.1016/j.urology.2005.03.019
Stern JM, Yiee J, Park S (2007) Safety and efficacy of ureteral access sheaths. J Endourol 21(2):119–123. doi:10.1089/end.2007.9997
Traxer O, Thomas A (2013) Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J Urol 189(2):580–584. doi:10.1016/j.juro.2012.08.197
Bach C, Nesar S, Kumar P, Goyal A, Kachrilas S, Papatsoris A, Masood J, Buchholz N (2012) The new digital flexible ureteroscopes: ‘size does matter’–increased ureteric access sheath use! Urol Int 89(4):408–411. doi:10.1159/000341429
Jessen JP, Breda A, Brehmer M, Liatsikos EN, Millan Rodriguez F, Osther PJ, Scoffone CM, Knoll T (2016) International collaboration in endourology: multicenter evaluation of prestenting for ureterorenoscopy. J Endourol 30(3):268–273. doi:10.1089/end.2015.0109
Author’s contribution
O Bas participated in protocol/project development, data analysis and manuscript writing. C Tuygun performed the protocol/project development and data collection or management. O Dede contributed to protocol/project development and data analysis. S Sarı, MÇ Çakıcı, U Öztürk and G Göktuğ were involved in data collection or management and data analysis. A İmamoğlu participated in protocol/project development and manuscript editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they had no conflicts of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Baş, O., Tuygun, C., Dede, O. et al. Factors affecting complication rates of retrograde flexible ureterorenoscopy: analysis of 1571 procedures—a single-center experience. World J Urol 35, 819–826 (2017). https://doi.org/10.1007/s00345-016-1930-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1930-3