Abstract
Objective
To describe a modified surgical technique for treatment of highly recurrent bladder neck contracture (BNC) after transurethral surgery for benign hyperplasia and to evaluate success rate and patient satisfaction of this novel technique.
Methods
Ten patients with highly recurrent BNC and multiple prior attempts of endoscopic treatment underwent the T-plasty. Perioperative complications were recorded and classified according to the Clavien classification. Patient reported functional outcomes were retrospectively analysed using a standardized questionnaire assessing recurrence of stenosis, incontinence, satisfaction and changes in quality of life (QoL). The questionnaires included validated IPSS and SF-8-health survey items.
Results
Mean age at the time of surgery was 69.2 years (range 61–79), and the mean follow-up was 26 months (range 3–46). No complications grade 3 or higher according to the Clavien classification occurred. Success rate was 100 %. No de novo stress incontinence occurred. Urinary stream was described as very strong to moderate by 80 % of the patients, mean post-operative IPSS-score was 11.3 (range 4–29), and mean post-operative IPSS-QoL was 2.4 (range 1–5). Patients satisfaction was very high or high in 90 %, and QoL improved in 90 %. The SF-8-health survey showed values comparable to the reference population.
Conclusion
The T-plasty represents a safe and valuable option in treating highly recurrent BNC after surgery for benign hyperplasia. It offers multiple advantages compared to other techniques such as a single-staged approach and the opportunity for reconstruction of a reliable wide bladder neck by usage of two well-vascularized flaps. Success rate, low rate of complications and preservation of continence are highly encouraging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For symptomatic benign hyperplasia of the prostate, transurethral resection of the prostate (TURP) is regarded as the gold standard in treatment. Besides classical TURP, other transurethral techniques are acknowledged as at least equally [1–3]. The incidence of bladder neck contracture (BNC) after surgery for benign hyperplasia of the prostate varies in the literature from 0 up to 20 % with similar rates of occurrence after all types of transurethral procedures [2, 4–10]. Potential risk factors for BNC include a low adenoma weight, extensive resection of the bladder neck and use of a large resecting loop [8, 9, 11–13]. Usually, BNC occurs early after surgery within the first 2 years [8].
Endoscopic treatment is widely accepted as initial treatment of BNC [14]. Success rates of endoscopic bladder neck incision (BNI) or bladder neck resection (BNR) are approximately 90 % [14, 15]. Even after a second transurethral procedure success rates up to 92 % were described [14]. However, different studies showed a declining success rate after repeated transurethral surgery [14, 16].
BNC is often defined as highly recurrent in case of stricture recurrence after three or more failed endoscopic treatment attempts. Highly recurrent BNC is therefore a rare but troublesome condition in which there is no standard treatment defined. Described therapeutic options are intermittent dilatation, intermittent BNI or BNR, permanently suprapubic drainage, urinary diversion or an open reconstruction [6, 17–19], depending on patients age, condition and patients request. Many authors advocate an urethrovesical anastomosis after failure of endoscopic treatments [17, 18, 20]. Young first described an YV-reconstruction of the bladder neck [21]. Still, the YV-plasty represents one of the most widely used techniques for BN reconstruction offering high success rates by enabling reconstruction of a wide reanastomosis with a flap of healthy tissue. However, vascularization of the YV-flap may be impaired by extensive mobilization and tension during suturing, potentially leading to insufficiency of anastomosis and restructure of the BN. To improve vascularity and mobility of the utilized flaps, we enhanced this technique.
This study represents the first description of this procedure: The T-plasty. We reviewed the clinical outcome and the patient satisfaction of this modified technique.
Materials and methods
Patients
Between December 2008 and July 2012, ten patients underwent T-plasty of the bladder neck for highly recurrent BNC after transurethral surgery of benign hyperplasia of the prostate. According to Pansadoro and Emiliozzi [14], all our patients had prostatic urethral strictures type I: Fibrous tissue involving the bladder neck only with a wide prostatic fossa and a verumontanum that is present at urethroscopy. All patients had at least two failures of endoscopic treatment.
Preoperative workup included uroflowmetric assessment and measurement of residual urine. A simultaneous retrograde and voiding cystourethrography (VCUG) and a cystoscopy were performed to define length and dimension of the stenosis as well as relation to the external sphincter. In selected patients with suspicious history or signs of detrusor overactivity or compliance abnormalities, an urodynamic investigation was performed. For retrospective analysis, at the time of follow-up, a standardized questionnaire was sent to all patients inquiring for recurrence of the stricture, incontinence, satisfaction and changes in quality of life after institutional review board approval. As validated questionnaires, the IPSS and SF-8 health survey were included.
Stricture recurrence after T-plasty was determined as no need for further instrumentation such as catheterization, dilatation, internal urethrotomy or open surgery.
Statistical software SPSS 20.0 (SPSS Inc.) was used for all analysis.
Surgical technique
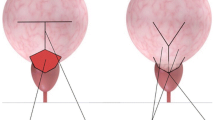
Patients were placed in a supine position. Access was gained through an abdominal midline incision. Afterwards, the perivesical space and the bladder neck were defined using the typical retropubic approach. After proper exposition of the bladder neck, the scar tissue was excised and the anterior bladder wall was incised in a T-shaped manner. Ureteral stents were placed routinely. Using the T-shaped incision instead of the traditional Y-shaped incision, two well-vascularized and tension-free flaps are created, which offer the possibility to reconstruct a wide bladder neck and anterior prostatic urethra.
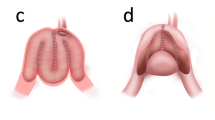
The two flaps are sutured in a V-shape, thus widening the bladder outlet. Interrupted 3/0 polygalactic acid sutures were placed from distal to proximal and tied under direct visual control (see Figs. 1, 2, 3, 4).
Schematic presentation of the type of incision. (a/marked red) represents the T-shaped incision at the anterior bladder wall, and (b) shows both flaps. (c/marked yellow) is the dorsal muco-mucosal anastomosis of trigone and prostate cavity. (d/marked blue) represents the anterior prostate wall and the resected scar tissue
After control for leak tightness, a transurethral and a suprapubic catheter was placed and the bladder was closed in layers.
A single shot of cefuroxime 1.5 g (i.v.) was given at the time of surgery; afterwards, patients did not routinely receive antibiotic prophylaxis. After discharge, testing and eventually treatment for urinary tract infection were left to the general practitioner.
Ureteral stents were routinely removed on day ten and eleven after surgery. Removal of the transurethral catheter was performed 21 days after surgery followed by a VCUG. In the absence of urinary extravasation and sufficient spontaneous micturation, voiding was allowed and the suprapubic catheter removed. As our institution represents a tertiary referral centre, routine follow-up for eventual stricture recurrence was left to the general practitioner.
Results
The mean age at the time of T-plasty was 69.2 years (range 61–79), and the mean follow-up was 26 months (range 3–46). All patients had multiple previous transurethral surgeries (mean 3.5; range 2–5). Aetiology of the stricture was TURP in 80 % and holmium laser enucleation of the prostate in 20 %.
Mean time of operation was 112 min. (range 83–158 min.), and no relevant blood loss was documented. Mean hospital stay was 13 days (range 8–21 days).
At twenty-first post-operative day, the VCUG showed a wide anastomosis in all patients. At the time of follow-up, success rate, defined as no need for further instrumentation, was 100 %. The urinary stream was described as very strong by 50 % of the patients, and 30 % reported a moderate and 20 % a weak urinary stream. Mean post-operative IPSS-score was 11.3 (range 4–29), and mean post-operative IPSS-QoL was 2.4 (range 1–5).
Patients satisfaction was very high in 70 %, high in 20 % and undecided in 10 %. Underlining these findings, quality of life improved clinically significantly in 90 % of the patients, and one patient reported no change.
No de novo stress incontinence was reported. One patient had a preoperative urge incontinence due to an overactive bladder that persisted post-operatively.
Analysing the results of the SF-8-health survey, the mean value of the physical component summary (PCS) was 43.8, and mean value of the mental component summary (MCS) was 41.8.
Two patients had a post-operative urinary tract infection detected by routine urine culture which could be treated by antibiotics without further problems. No other complications more than grade II according to the Clavien–Dindo grading system were reported.
Discussion
The discussion on treatment options for recurrent BNC remains controversial. Stricture dilation, cold knife incision or transurethral resection have been proposed with varying success rates. Different studies showed a declining success rate after repeated transurethral surgery [14, 16]. Even the use of intralesional mitomycin C after BNI could not rule out a number of cases that have been treated unsuccessfully [22, 23]. For those patients, urinary diversion is often considered as a last resort for permanent recurrence-free survival [19].
Besides that, the literature that focuses on recurrent BNC caused by surgery for benign hyperplasia of the prostate is rare. Some authors propose the same therapy for both reasons of recurrent BNC, transurethral surgery or radical prostatectomy [18]. These two causes should not be lumped together due to completely different aetiology and anatomical predispositions. Usually, BNC occurring after TURP is of shorter length [14] and relation to the external sphincter is different.
In this regard, a more differentiated therapeutic strategy should be conducted depending on the aetiology of stenosis.
Whereas transperineal reanastomosis is our therapy of choice for highly recurrent BNC after radical retropubic prostatectomy [24], we prefer a different therapy for BNC caused by transurethral surgery: The T-plasty as described above.
Theodorou [17] proposed an abdomino-perineal repair, performing an excision of the stenotic area and an end-to-end anastomosis. Simultaneously, an artificial urinary sphincter implantation was performed.
From our point of view, this approach brings different disadvantages compared to the T-plasty. Besides the more extensive combined abdomino-perineal approach, the operating time is way longer (mean 4.1 h) compared to our technique (mean 112 min.). Hospital stay was shorter in our group (15.6 vs 13 days), too.
A further disadvantage of the transperineal techniques as described by Theodorou and Simonato [18] is the extreme positioning of the patient which is needed to have a proper transperineal exposition. Furthermore and most important, transsphincteric mobilization of the urethra results in aggravated urinary incontinence. In our patient group, no de novo incontinence was noted. Therefore, implantation of an AUS is not necessary, and early problems caused by the AUS as reported by Theodorou or known late complications [25] can be avoided.
The T-plasty is leaned to the YV-plasty, first described by Young in 1953 [21]. Later Colabawalla [26] published a larger study, finding satisfactory results for the YV-plasty.
In comparison with this technique, the T-plasty offers several advantages by the utilization of two well-vascularized flaps. Using these two instead of one flap, a wider bladder neck can be reconstructed. Furthermore, less tension is impacting on the flaps. Therefore, the potential risk of a recurrence seems to be declined.
These are theoretical considerations. Due to the high account of failed previous operations and the strong resulting psychological strain for the patients, it is an attempt to ensure best results possible. Knowing that the YV-plasty is an efficient established technique, the T-plasty should be seen more as an improvement rather than a replacement of the technique.
The results of our patient group prove these considerations true: Success rate, defined as no need for further instrumentation, is high. Concordantly 80 % of the patients estimate the subjective strength of urinary stream as moderate to very strong.
Patient satisfaction is reasonable as well. The IPSS-QoL of mean 2.4 is satisfying. Though not validate for bladder neck contracture but only for anterior urethral stricture disease [27], correlation between IPSS and voiding symptoms can be taken as reliable. The results of the SF-8 show reasonable results: PCS is 43.8 which is close to the age- and sex-adjusted value of 60- to 69-year-old man of the German population (average PCS 45.01). Considering that the mean age of our study population is 69.2 and therefore at the very end of the age adjusted group (60–69 years), we take it as satisfactory results. MCS is 41.8 and thus lower than the age- and sex-adjusted value of the German population (average MCS 50.72). From our point of view, this may be due to the long medical history and repeated surgery with a consecutive mental burden.
Limitations of this study are the retrospective design of the study as well as the relatively small number of patients and limited follow-up.
Furthermore, success was defined as the absence of need for further instrumentation, and no objective measurement such as uroflowmetric, cystoscopic or radiographic assessment for recurrence-free patency of the bladder neck at the time of follow-up was available.
However, compared to the literature, the number of patients is not that small at all, giving a good insight on the results of this new technique. Moreover, this study points out the technique of T-plasty as a valuable treatment option for highly recurrent BNC compared to other more invasive techniques.
Conclusion
Highly recurrent BNC represents a challenging therapeutic condition. After repeated transurethral treatment failures, the T-plasty is a valuable option in treatment for highly recurrent BNC caused by transurethral surgery of the prostate, which offers multiple advantages compared to other approaches and techniques. Success rate, low rate of complications and no de novo incontinence are highly satisfactorily.
Abbreviations
- AUS:
-
Artificial urinary sphincter
- BNC:
-
Bladder neck contracture
- BNI:
-
Bladder neck incision
- BNR:
-
Bladder neck resection
- IPSS:
-
International prostate symptom score
- MCS:
-
Mental component summary
- PCS:
-
Physical component summary
- QoL:
-
Quality of life
- RUG:
-
Retrograde urethrography
- SF-8:
-
Short form-8 health survey
- TURP:
-
Transurethral resection of the prostate
- VCUG:
-
Voiding cystourethrography
References
Ahyai SA, Lehrich K, Kuntz RM (2007) Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. Eur Urol 52(5):1456–1463
Kuntz RM, Lehrich K, Ahyai S (2004) Transurethral holmium laser enucleation of the prostate compared with transvesical open prostatectomy: 18-month follow-up of a randomized trial. J Endourol 18(2):189–191
Madersbacher S et al (2004) EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol 46(5):547–554
Wettlaufer JN, Kronmiller P (1976) The management of post-prostatectomy vesical neck contracture. J Urol 116(4):482–483
Chiu AW et al (1990) Prophylactic bladder neck incision in the treatment of small benign prostatic hyperplasia. Zhonghua Yi Xue Za Zhi (Taipei) 45(1):22–25
Edwards LE et al (1985) Transurethral resection of the prostate and bladder neck incision: a review of 700 cases. Br J Urol 57(2):168–171
Orandi A (1985) Transurethral incision of prostate (TUIP): 646 cases in 15 years–a chronological appraisal. Br J Urol 57(6):703–707
Lee YH, Chiu AW, Huang JK (2005) Comprehensive study of bladder neck contracture after transurethral resection of prostate. Urology 65(3):498–503 (Discussion 503)
Rassweiler J et al (2006) Complications of transurethral resection of the prostate (TURP)–incidence, management, and prevention. Eur Urol 50(5):969–979 (Discussion 980)
Ahyai SA et al (2010) Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol 58(3):384–397
Robinson HP, Greene LF (1962) Postoperative contracture of the vesical neck. II. Experimental production of contractures in dogs: transurethral series. J Urol 87:610–616
Jonas U, Petri E, Hohenfellner R (1979) Indication and value of bladder neck incision. Urol Int 34(4):260–265
Greene LF, Robinson HP (1965) Postoperative contracture of the vesical neck. V. Clinical findings, symptoms and diagnosis. J Urol 94:141–147
Pansadoro V, Emiliozzi P (1999) Iatrogenic prostatic urethral strictures: classification and endoscopic treatment. Urology 53(4):784–789
Herrando C et al (1994) [Bladder neck sclerosis after transurethral resection of the prostate. “Study Group of the Puigvert Foundation”]. Actas Urol Esp 18(2):85–89
Popken G et al (1998) Anastomotic stricture after radical prostatectomy. Incidence, findings and treatment. Eur Urol 33(4):382–386
Theodorou C et al (2000) Abdomino–perineal repair of recurrent and complex bladder neck-prostatic urethra contractures. Eur Urol 38(6):734–740 (Discussion 740-1)
Simonato A et al (2007) Two-stage transperineal management of posterior urethral strictures or bladder neck contractures associated with urinary incontinence after prostate surgery and endoscopic treatment failures. Eur Urol 52(5):1499–1504
Spahn M et al (2010) Last resort in devastated bladder outlet: bladder neck closure and continent vesicostomy–long-term results and comparison of different techniques. Urology 75(5):1185–1192
Simonato A et al (2012) Comparison between two different two-stage transperineal approaches to treat urethral strictures or bladder neck contracture associated with severe urinary incontinence that occurred after pelvic surgery: report of our experience. Adv Urol 2012:481943
Young BW (1953) The retropubic approach to vesical neck obstruction in children. Surg Gynecol Obstet 96(2):150–154
Sikafi Z et al (1985) Bladder neck contracture following prostatectomy. Br J Urol 57(3):308–310
Vanni AJ, Zinman LN, Buckley JC (2011) Radial urethrotomy and intralesional mitomycin C for the management of recurrent bladder neck contractures. J Urol 186(1):156–160
Pfalzgraf D et al (2011) Open retropubic reanastomosis for highly recurrent and complex bladder neck stenosis. J Urol 186(5):1944–1947
James MH, McCammon KA (2014) Artificial urinary sphincter for post-prostatectomy incontinence: a review. Int J Urol 21(6):536–543. doi:10.1111/iju.12392
Colabawalla BN (1969) Adult bladder neck contracture–100 Y-V plasties. Br J Urol 41(5):601
Jackson MJ, Sciberras J, Mangera A et al (2011) Defining a patient-reported outcome measure for urethral stricture surgery. Eur Urol 60:60–68
Authors contribution
C.P. Reiss, P. Schriefer, R. Dahlem and M. Fisch were involved in protocol/project development; C.P. Reiss, C.M. Rosenbaum and P. Schriefer were involved in data collection or management; C.P. Reiss, C.M. Rosenbaum, A. Becker and T. Ludwig analysed the data; C.P. Reiss, C.M. Rosenbaum, A. Becker, T. Ludwig, O. Engel, S. Riechardt, M. Fisch and R. Dahlem wrote and edited the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
C. P. Reiss and C. M. Rosenbaum have contributed equally as first authors.
Rights and permissions
About this article
Cite this article
Reiss, C.P., Rosenbaum, C.M., Becker, A. et al. The T-plasty: a modified YV-plasty for highly recurrent bladder neck contracture after transurethral surgery for benign hyperplasia of the prostate: clinical outcome and patient satisfaction. World J Urol 34, 1437–1442 (2016). https://doi.org/10.1007/s00345-016-1779-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1779-5