Abstract
Purpose
To identify predictive factors for immediate continence after radical prostatectomy.
Patients and methods
A total of 1553 patients underwent radical prostatectomy in a single institution (670 RRP, 883 RARP), had complete perioperative data and follow-up for urinary continence and were included in this prospective analysis. Immediate continence was defined as no pad usage after catheter removal. Evaluated parameters included age, body mass index, ECOG performance status, erectile function, prostate volume, PSA, Gleason score, tumor stage and D’Amico risk groups, as well as surgical approach (RRP, RARP), surgeon volume, nerve-sparing, lymphadenectomy, blood transfusions and duration of catheterization.
Results
A total of 240 men (15.5 %) did not require any pads 1 day or later after removal of the transurethral catheter. Correlation of parameters with immediate continence revealed significance for age (p < 0.001), ECOG-score (p = 0.025), erectile function (p = 0.001), nerve-sparing (p = 0.022), Gleason score (p = 0.002) and surgeon volume (p ≤ 0.022). Multivariate analyses identified IIEF-score >21 (p = 0.031), ECOG (p < 0.05), bilateral nerve-sparing (p = 0.049), Gleason score <3 + 4 (p ≤ 0.028), less blood transfusion (p ≤ 0.044) and surgeon volume (p ≤ 0.042) as the remaining prognostic parameters for immediate continence after radical prostatectomy. The type of surgical approach (robotic vs. open radical prostatectomy) did not yield significant influence.
Conclusion
Evaluating continence in a contemporary prospective cohort revealed 15.5 % of patients never requiring a pad postoperatively. Predictive parameters for immediate continence were erectile function, ECOG, bilateral nerve-sparing, less blood transfusion and Gleason score. Furthermore, the surgeon’s experience but not his operative technique had a significant impact on immediate postoperative continence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radical prostatectomy is a standard treatment option for patients with localized prostate cancer [1]. Assessing patient preferences revealed that continence is the most important factor of postoperative quality of life [2]. Formerly, it was accepted that return of continence after radical prostatectomy took up to 12 months [3]. With modification of surgical techniques, this time-frame has dropped significantly [4, 5]. These improvements led to the introduction of an “early continence” group after radical prostatectomy, defined as return of urinary continence within 3 months after surgery. Early continence after radical prostatectomy has been extensively evaluated for both robot-assisted (RARP) and retropubic (RRP) prostatectomy taking into account that urinary leakage after radical prostatectomy for a certain timeframe may be acceptable. However, with regard to decreased quality of life due to post-prostatectomy incontinence, the main goal after radical prostatectomy should include immediate continence [6] besides cancer control. Clinical routine has shown that a certain percentage of patients are continent immediately after catheter removal and therefore never need a pad. There is only limited number of publications examining this issue. Sammon et al. [7] examined a patient cohort that underwent RARP and found that nerve-sparing and placement of a suprapubic catheter significantly influenced immediate continence. However, immediate continence is not limited to RARP as shown by Campodonico et al. [8] who determine the rate of immediate continence in a small group of patients undergoing RRP. Although RARP is considered to result in faster recovery of urinary continence than RRP [9, 10], a direct comparison between the two surgical techniques in regard to immediate continence has not been evaluated to date.
For better preoperative patient counseling, it is important to identify factors that are associated with improved continence outcomes. Therefore, the aim of this study is to evaluate both pre- and perioperative parameters and surgical factors for their prognostic value in predicting immediate continence after radical prostatectomy.
Patients and methods
Study population
All patients undergoing radical prostatectomy at our institution between January 2005 and August 2013 were followed up in a prospectively conducted database. Complete data were available for 1553 patients. The study protocol was approved by the local ethics committee.
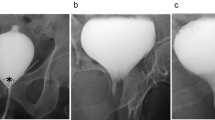
Prostatectomy procedure
Radical prostatectomy was performed by different surgeons with varying experience. RARP was performed transperitoneally, using a three-arm DaVinci system (Intuitive Surgical, Sunnyvale, CA). Lymphadenectomy was performed in all patients. Nerve-sparing was performed whenever oncological control permitted and patient reported good erectile function preoperatively (measured by IIEF5 score). Anastomosis was done as running suture in RARP [11] and with 8–10 stitches in RRP using monofilament suture. Anastomosis was tested for watertightness by intraoperative methylene blue test [12]. A 20Ch Foley catheter was placed during surgery. Routine radiological assessment of the anastomosis was performed by cystography before removal of the catheter.
Follow-up
After removal of the catheter, patients were routinely admitted overnight. They were evaluated for continence after catheter removal by micturition/pad-use diary and interview at discharge. Additionally, patients were followed up prospectively by outpatient visits and written or telephone interviews every 3 months. During the follow-up, oncological and functional results were noted. Patients were considered continent when they reported no more pad use. All collected results were entered into a prospectively conducted database [13].
Collected variables
Collected data included the following preoperative parameters: patient age, body mass index, ECOG (eastern cooperative oncology group) performance status, IIEF5 score, prostate volume, PSA value, clinical stage, and risk classification (according to D’Amico et al. [14, 15]). Further intra-/postoperative characteristics noted were as follows: surgical approach (RRP, RARP), number of harvested lymph nodes, nerve-sparing (none, uni- or bilateral), watertightness of anastomosis, necessity for or number of blood transfusions, tumor stage and grading in prostatectomy specimen, surgical margin, performing surgeon, duration of catheterization.
Statistical analyses
Patients reporting immediate continence, i.e., no pad use 1 day or later after catheter removal were identified and compared to the rest of the collective. Surgeon volume was categorized for further analysis. Median, range, mean and standard deviation (SD) were calculated for the above-mentioned variables. As a first step, the single prognostic value for immediate continence was evaluated by univariate analysis (Chi-square test for categorical variables and Mann–Whitney U test for continuous variables) where the responsible levels of significant variables were identified by univariate logistic regression. As a second step, multivariate analysis of all variables (logistic regression) was performed in order to determine the odds ratio for each variable by the possible presence of correlation effects between the focused variable and the remaining variables. A p value <0.05 was considered statistically significant. All statistical analyses were carried out using IBM SPSS software package version 20.
Results
A total of 1553 patients with complete data and a mean follow-up of 29.3 months (range 0–98; SD 24.3) underwent radical prostatectomy between January 2005 and August 2013. Mean age in all patients was 64.3 (range 38–80; SD 7.1).
Clinical examination revealed that 832 (53.6 %) patients presented with clinical stage T1. Preoperative risk stratification according to D’Amico et al. [15] revealed 496 low-risk (31.9 %), 678 intermediate-risk (43.7 %) and 379 high-risk (24.4 %) prostate cancer cases in the cohort. Regarding tumor stage, histology indicated localized prostate cancer (pT2) in 890 (57.3 %) patients and advanced prostate cancer (≥pT3) in 663 (42.7 %) patients. In the pT2 group, 190 patients (21.3 %) had positive surgical margins and adjuvant radiation therapy was performed in 39 (4.4 %) of these cases. Seventy-one (8.0 %) of pT2 patients developed biochemical recurrence during mean follow-up of 30.5 months (range 0–92; SD 24.2). In the advanced cancer group (≥pT3), 417 patients (62.9 %) had positive surgical margins and adjuvant radiation therapy was performed in 242 patients (36.5 %). In this group, 175 patients (26.4 %) had biochemical recurrence during mean follow-up of 27.7 months (range 0–98; SD 24.4).
Surgery was performed by 16 different surgeons of varying experience. In all, RRP was performed in 670 patients and RARP in 883 patients. Regarding postoperative continence, 240 (15.5 %) patients never required a pad 1 day or later after catheter removal. Of these 240 cases, 107 underwent RRP and 133 RARP and none of the patients experienced urinary retention or strictures during follow-up. Patients’ continence did not change during follow-up.
All collected patient characteristics, preoperative and perioperative parameters are listed in Table 1.
Significant correlation between the mentioned variables and immediate continence after catheter removal was detected for the following variables: patient age (p < 0.001), ECOG performance status (p = 0.025), IIEF-5 score (p = 0.001), nerve-sparing (p = 0.022) and Gleason score (p = 0.002). Regarding surgeon’s experience, significant correlation to immediate continence was seen for surgeons performing more than 100 procedures during the study period (p < 0.022).
In order to identify prognostic parameters and their significance levels for no pad usage, as well the influence of correlation between parameters, data were further analyzed by univariate and multivariate logistic regression. Univariate analysis identified age (p = 0.002; OR 0.97), ECOG performance status 1 (p = 0.008; OR 0.53; ECOG 0 as referent), IIEF-5 score >21 (meaning no erectile dysfunction) (p = 0.001; OR 1.82; severe erectile dysfunction as referent), bilateral nerve-sparing (p = 0.006; OR 1.52; no nerve-sparing as referent), number of perioperative blood transfusion (p = 0.049, OR 0.87), Gleason score (p < 0.015; OR < 0.56) and surgeons volume >100 cases (p = 0.019; OR 1.44) and >150 cases (p = 0.004; OR 1.51) as prognostic parameters.
Multivariate analysis was performed according to surgeon volume (<50 vs. >50 cases; <100 vs. >100 cases; <150 vs. >150 cases) and revealed that no erectile dysfunction by IIEF-5 score (p = 0.03; OR 1.6; severe erectile dysfunction as referent) had an impact on immediate continence in all groups. In addition, the number of blood transfusions given (p = 0.04; OR 0.85), Gleason score 3 + 4 (p < 0.01; OR 0.54) and Gleason score 4 + 3 (p < 0.03; OR 0.58) in comparison with Gleason 3 + 3 as referent and ECOG performance status 1 (ECOG 0 as referent; p < 0.05 for surgeon volume <50 vs. >50 and <150 vs. >150; p = 0.05 for <100 vs. >100) was associated with a worse outcome for immediate continence in all groups. Surgeon volume greater than 100 cases had significant impact on immediate continence (p = 0.04; OR 1.40 for >100 performed cases; p = 0.003; OR 1.16 for >150 performed cases). The surgeon’s operating volume also impacted the effect of bilateral nerve-sparing on immediate continence after 100 performed cases (p = 0.049, OR 1.52 for >100 performed cases; p = 0.039, OR 1.55 for >150 performed cases).
There was no difference for surgical procedure with regard to immediate continence (p > 0.11). Results of these analyses are displayed in Tables 1, 2 and 3.
Discussion
Continence after radical prostatectomy has extensively been evaluated in various publications. However, there is no standard definition of continence after radical prostatectomy, therefore accepting different degrees of incontinence following a certain period after surgery. From the patient’s point of view, any type of incontinence decreases quality of life [6]. Although time to recovery of urinary function has been shortened by improvement in different surgical techniques that preserve and reconstruct anatomical structures [16], not all patients will reach immediate continence after catheter removal.
The aim of this study was to identify preoperative and perioperative parameters that predict immediate continence (defined as no pad usage after catheter removal) in a cohort of men with prostate cancer undergoing either RRP or RARP. This allowed us for the first time, to directly evaluate whether surgical approach alone influences immediate continence. In contrast to many other publications which evaluate only the outcome of a single high-volume surgeon, radical prostatectomy was performed by different surgeons with varying experience in this study, allowing the evaluation of surgeon experience impact in regard to immediate continence. In addition, the cohort was not limited to only localized and low-risk prostate cancer but also included 42.7 % of patients with TNM stage ≥pT3. Rounding out the cohort, 43.7 and 24.4 % of patients had intermediate- and high-risk prostate cancer, respectively. We believe that this reflects a more realistic profile of patients and therefore the results of this study are more applicable for everyday clinical practice.
Overall, 15.5 % of patients (240 of 1553) in this study had immediate continence following surgery (never wore a pad 1 day or later after catheter removal). Multivariate analysis for patients with immediate continence identified preoperative IIEF-5 score >21, favorable ECOG performance score, Gleason score <3 + 4, bilateral nerve-sparing, less blood transfusion and surgeon experience as independent prognostic factors for immediate continence. None of the other evaluated parameters including surgical approach (RRP vs. RARP) had any significant prognostic impact on immediate continence in univariate or multivariate analyses.
Other studies that have evaluated prognostic parameters for only one surgical approach, either for RARP or RRP, have determined that suprapubic urinary drainage, age, potency and nerve-sparing are positive prognostic factors for immediate continence [7, 8]. We are in agreement with these previous studies that bilateral nerve-sparing is significantly associated with immediate continence [7, 8]. Nelson et al. [17] recently found that intraoperative nerval stimulation of the neurovascular bundles (NVB) increases urethral sphincter pressure. Furthermore, anatomical studies have found that a part of the innervation of the external urethral sphincter runs within the NVB [18]. This most likely explains why bilateral nerve-sparing is associated with better urinary continence and a faster regaining of sphincter control after radical prostatectomy as has been previously shown [19] and further confirmed in this study.
We could also confirm that preoperative IIEF5 score, reflecting erectile function and therefore the status of NVBs, had an impact on immediate continence. We found that a preoperative IIEF5 score greater than 21 is significantly associated with immediate continence. As shown previously by various authors, preoperative erectile function has an impact on postoperative urinary continence recovery [20–22].
We could show that increased prostate cancer aggressiveness, reflected by a Gleason score ≥3 + 4, is associated with worse urinary continence outcome. As shown by Weidner et al. [23], increasing tumor aggressiveness is associated with cancer-induced angiogenesis that could cause changes in cancer microenvironment and alteration to surrounding tissue. In contrast to this, tumor stage and surgical margins were without predictive value. Although 21.3 % of patients with pT2 tumors had positive surgical margins, biochemical recurrence occurred in only 8.0 %. As expected, the biochemical recurrence rate in ≥pT3 was higher. Evaluation of positive surgical margins shows great variation between different publications. As stated by Preston et al. [24], this is due to multiple influencing factors, including varying definition of positive surgical margins and variable pathologic specimen handling and reporting. Therefore reporting of biochemical recurrence seems more reliable.
Reviewing literature independently evaluating immediate continence after RARP or RRP, most authors favor RARP and attribute their results to magnified intraoperative view and less operative trauma [5, 9, 10, 25, 26]. However, in these studies, mainly high-volume surgeons performed RARP on mostly low-risk prostate cancer patients. In contrast, our study consisted of surgeries that were performed by various surgeons with various volumes of surgical experience. This allowed us to determine that immediate continence outcome is not dependent on surgical approach. RARP and RRP showed equal results with regard to immediate continence. In contrast, the performing surgeons experience affected immediate continence significantly. When surgery was performed by experienced surgeons (surgeons who had performed more than 100 cases), immediate continence was achieved in significantly more cases. This was even more significant for surgeons who had performed more than 150 cases. This is in accordance with previous studies that evaluated the impact of surgeon experience on postoperative outcome after radical prostatectomy [5, 27].
A limitation of this study is missing pad weight test or questionnaires for objective evaluation of continence instead of patient interviews and micturition diaries. As this represents a retrospective, single-center study, further analysis by prospective multicenter trials should be performed to confirm the results found here.
References
Heidenreich A, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V, Mottet N, Schmid HP, van der Kwast T, Wiegel T, Zattoni F (2011) EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. Eur Urol 59(1):61–71. doi:10.1016/j.eururo.2010.10.039
Albertsen PC, Nease RF Jr, Potosky AL (1998) Assessment of patient preferences among men with prostate cancer. J Urol 159(1):158–163
Walsh PC, Marschke P, Ricker D, Burnett AL (2000) Patient-reported urinary continence and sexual function after anatomic radical prostatectomy. Urology 55(1):58–61
Dev HS, Sooriakumaran P, Srivastava A, Tewari AK (2012) Optimizing radical prostatectomy for the early recovery of urinary continence. Nat Rev Urol 9(4):189–195. doi:10.1038/nrurol.2012.2
Ficarra V, Novara G, Rosen RC, Artibani W, Carroll PR, Costello A, Menon M, Montorsi F, Patel VR, Stolzenburg JU, Van der Poel H, Wilson TG, Zattoni F, Mottrie A (2012) Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 62(3):405–417. doi:10.1016/j.eururo.2012.05.045
Liss MA, Osann K, Canvasser N, Chu W, Chang A, Gan J, Li R, Santos R, Skarecky D, Finley DS, Ahlering TE (2010) Continence definition after radical prostatectomy using urinary quality of life: evaluation of patient reported validated questionnaires. J Urol 183(4):1464–1468. doi:10.1016/j.juro.2009.12.009
Sammon JD, Sharma P, Trinh Q-D, Ghani KR, Sukumar S, Menon M (2012) Predictors of immediate continence following robot-assisted radical prostatectomy. J Endourol. doi:10.1089/end.2012.0312
Campodonico F, Manuputty EE, Campora S, Puntoni M, Maffezzini M (2013) Age is predictive of immediate postoperative urinary continence after radical retropubic prostatectomy. Urol Int. doi:10.1159/000353414
Geraerts I, Van Poppel H, Devoogdt N, Van Cleynenbreugel B, Joniau S, Van Kampen M (2013) Prospective evaluation of urinary incontinence, voiding symptoms and quality of life after open and robot-assisted radical prostatectomy. BJU Int 112(7):936–943. doi:10.1111/bju.12258
Jeong SJ, Yeon JS, Lee JK, Cha WH, Jeong JW, Lee BK, Lee SC, Jeong CW, Kim JH, Hong SK, Byun SS, Lee SE (2013) Development and validation of nomograms to predict the recovery of urinary continence after radical prostatectomy: comparisons between immediate, early, and late continence. World J Urol. doi:10.1007/s00345-013-1127-y
Van Velthoven RF, Ahlering TE, Peltier A, Skarecky DW, Clayman RV (2003) Technique for laparoscopic running urethrovesical anastomosis: the single knot method. Urology 61(4):699–702
Nyarangi-Dix JN, Pahernik S, Bermejo JL, Prado L, Hohenfellner M (2012) Significance of the intraoperative methylene blue test for postoperative evaluation of the vesicourethral anastomosis. Adv Urol. doi:10.1155/2012/702412
Huber J, Herpel E, Jakobi H, Hadaschik BA, Pahernik S, Hohenfellner M (2013) Two decades’ experience with a prospective biobank for urologic oncology: research, clinical care, and the patients’ view. Urol Oncol 31(7):990–996. doi:10.1016/j.urolonc.2012.01.016
D’Amico AV, Moul J, Carroll PR, Sun L, Lubeck D, Chen MH (2003) Cancer-specific mortality after surgery or radiation for patients with clinically localized prostate cancer managed during the prostate-specific antigen era. J Clin Oncol 21(11):2163–2172. doi:10.1200/JCO.2003.01.075
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, Tomaszewski JE, Renshaw AA, Kaplan I, Beard CJ, Wein A (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280(11):969–974
Kojima Y, Takahashi N, Haga N, Nomiya M, Yanagida T, Ishibashi K, Aikawa K, Lee DI (2013) Urinary incontinence after robot-assisted radical prostatectomy: pathophysiology and intraoperative techniques to improve surgical outcome. Int J Urol 20(11):1052–1063. doi:10.1111/iju.12214
Nelson CP, Montie JE, McGuire EJ, Wedemeyer G, Wei JT (2003) Intraoperative nerve stimulation with measurement of urethral sphincter pressure changes during radical retropubic prostatectomy: a feasibility study. J Urol 169(6):2225–2228. doi:10.1097/01.ju.0000058213.15524.90
Walz J, Burnett AL, Costello AJ, Eastham JA, Graefen M, Guillonneau B, Menon M, Montorsi F, Myers RP, Rocco B, Villers A (2010) A critical analysis of the current knowledge of surgical anatomy related to optimization of cancer control and preservation of continence and erection in candidates for radical prostatectomy. Eur Urol 57(2):179–192. doi:10.1016/j.eururo.2009.11.009
Srivastava A, Chopra S, Pham A, Sooriakumaran P, Durand M, Chughtai B, Gruschow S, Peyser A, Harneja N, Leung R, Lee R, Herman M, Robinson B, Shevchuk M, Tewari A (2013) Effect of a risk-stratified grade of nerve-sparing technique on early return of continence after robot-assisted laparoscopic radical prostatectomy. Eur Urol 63(3):438–444. doi:10.1016/j.eururo.2012.07.009
Gandaglia G, Suardi N, Gallina A, Capitanio U, Abdollah F, Salonia A, Nava L, Colombo R, Guazzoni G, Rigatti P, Montorsi F, Briganti A (2012) Preoperative erectile function represents a significant predictor of postoperative urinary continence recovery in patients treated with bilateral nerve sparing radical prostatectomy. J Urol 187(2):569–574. doi:10.1016/j.juro.2011.10.034
Ficarra V, Borghesi M, Suardi N, De Naeyer G, Novara G, Schatteman P, De Groote R, Carpentier P, Mottrie A (2013) Long-term evaluation of survival, continence and potency (SCP) outcomes after robot-assisted radical prostatectomy (RARP). BJU Int 112(3):338–345. doi:10.1111/bju.12001
Takenaka A, Soga H, Sakai I, Nakano Y, Miyake H, Tanaka K, Fujisawa M (2009) Influence of nerve-sparing procedure on early recovery of urinary continence after laparoscopic radical prostatectomy. J Endourol 23(7):1115–1119. doi:10.1089/end.2008.0512
Weidner N, Carroll PR, Flax J, Blumenfeld W, Folkman J (1993) Tumor angiogenesis correlates with metastasis in invasive prostate carcinoma. Am J Pathol 143(2):401–409
Preston MA, Blute ML (2014) Positive surgical margins after radical prostatectomy: does it matter? Eur Urol 65(2):314–315. doi:10.1016/j.eururo.2013.08.037
Son SJ, Lee SC, Jeong CW, Jeong SJ, Byun SS, Lee SE (2013) Comparison of continence recovery between robot-assisted laparoscopic prostatectomy and open radical retropubic prostatectomy: a single surgeon experience. Korean J Urol 54(9):598–602. doi:10.4111/kju.2013.54.9.598
Kim SC, Song C, Kim W, Kang T, Park J, Jeong IG, Lee S, Cho YM, Ahn H (2011) Factors determining functional outcomes after radical prostatectomy: robot-assisted versus retropubic. Eur Urol 60(3):413–419. doi:10.1016/j.eururo.2011.05.011
Abboudi H, Khan MS, Guru KA, Froghi S, de Win G, Van Poppel H, Dasgupta P, Ahmed K (2013) Learning curves for urological procedures: a systematic review. BJU Int. doi:10.1111/bju.12315
Conflict of interest
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Nyarangi-Dix and M. Hohenfellner have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Hatiboglu, G., Teber, D., Tichy, D. et al. Predictive factors for immediate continence after radical prostatectomy. World J Urol 34, 113–120 (2016). https://doi.org/10.1007/s00345-015-1594-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1594-4