Abstract
Objectives
To evaluate the long-term safety (primary objective) and efficacy/impact on quality of life (QoL, secondary objectives) of silodosin 8 mg once daily in men with LUTS/BPH.
Patients and Methods
Men who completed the 12-week double-blind study with silodosin 8 mg, tamsulosin 0.4 mg, or placebo were offered to continue with the 9-month open-label study during which all patients received silodosin 8 mg once daily. Safety was assessed by analysing vital signs, electrocardiograms, laboratory tests, and adverse events. Efficacy was evaluated with the International Prostate Symptom Score (IPSS), IPSS voiding and storage sub-scores, IPSS–QoL, and maximum urinary flow rate (Q max).
Results
A total of 500 patients (mean age 66 years) entered the 9-month open-label study. Treatment-emergent adverse events (TEAE) were experienced by 33.4 % patients. Ejaculation dysfunction was the most common TEAE (9.0 %) but led to study discontinuations in only 1.6 % of patients. Dizziness without orthostatic hypotension occurred in 0.8 %. A marked reduction in total IPSS (−2.7 ± 3.8) was documented at the first visit of this extension phase in patients having de novo silodosin compared with lesser improvement in patients previously treated with silodosin (−0.82 ± 4.2) or tamsulosin (−0.83 ± 3.8). Improvements were maintained throughout the open-label phase. QoL also improved, with the greatest improvement in de novo silodosin patients. No relevant changes in Q max occurred.
Conclusions
Long-term treatment with silodosin was safe and efficacious. Abnormal ejaculation was the most common TEAE, but led to treatment discontinuation in only 1.6 % of patients. Orthostatic hypotension was not seen, and only a few patients experienced dizziness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower urinary tract symptoms (LUTS) are prevalent in the male population, increase with age, and are often bothersome [1]. Benign prostatic hyperplasia (BPH), the microscopic changes of the epithelial and/or stromal cells of the prostate, also increases with age and is often associated with LUTS [2]. Men with LUTS suggestive of BPH (LUTS/BPH) usually present with a combination of storage LUTS (e.g. urgency, frequency, and nocturia) and voiding LUTS (e.g. hesitancy, weak stream, and intermittency) [3]. Voiding LUTS are commonly attributed to benign prostatic obstruction (BPO) and caused by protrusion of the enlarged prostatic gland into the urethra, but may also occur due to detrusor underactivity caused by reduced detrusor contraction power or duration [4]. Storage LUTS may occur secondary to BPO [5] or may be entirely unrelated to coexistent BPH [6].
α-Blockers are an established drug class for the treatment of LUTS/BPH and often used as first-line therapy [7]. They work by ameliorating the dynamic component of BPO which is mediated by α1A-adrenoreceptors (α1A-AR). Subtype-nonselective α-blockers (e.g. doxazosin and terazosin) are often associated with vasodilatation and cardiovascular adverse events (e.g. dizziness, asthenia, fatigue, somnolence, and orthostatic hypotension) [8–10] due to the antagonism of the α1B-AR sub-type found in blood vessels [11, 12]. Due to the risk of falls and fall-related morbidity or mortality, such adverse events are particularly undesirable in elderly men who often have cardiovascular comorbidities and take antihypertensive medication [13, 14].
The development of uro-selective α-blockers with increased affinity for the α1A-AR over other subtypes has provided the possibility to maximize efficacy and minimize undesirable cardiovascular adverse events [15, 16]. Silodosin is a new α-blocker with high α1A-AR but low α1B-AR selectivity. Silodosin has been licensed for LUTS/BPH in more than 50 countries, including USA, Europe, and Japan. Silodosin is approximately 160 times more selective for the α1A-AR, whereas the other widely available uro-selective α-blocker tamsulosin has only tenfold selectivity for the α1A-AR [17]. Randomized, controlled, 12-week phase III trials have demonstrated the efficacy and cardiovascular safety of silodosin in comparison with placebo or tamsulosin [18–20]. A consequence of the uro-selectivity of silodosin is its antagonism of α1A-AR in the ejaculatory apparatus which results in a higher incidence of ejaculation disorders (14–33 %) [21]. Due to the above-mentioned drug characteristics, silodosin treatment seems to be especially suitable in older men who often take antihypertensive drugs but are less likely to be concerned or bothered by ejaculatory dysfunction [22].
The primary aim of this open-label, 9-month extension study was to evaluate the long-term safety of silodosin 8 mg administered once daily for the treatment of men with LUTS/BPH. Secondary objectives were the evaluations of long-term clinical efficacy and quality of life (QoL) in men treated for LUTS/BPH with silodosin 8 mg once daily.
Patients and methods
Patients and study design
This prospective, multicentre, open-label study was conducted in Europe between October 2006 and January 2008 (clinical trials registration number NCT00359905). Men aged ≥50 years with signs and symptoms of BPH, who had successfully completed the 12-week double-blind study in which they were randomized to silodosin 8 mg, tamsulosin 0.4 mg, or placebo [18], were included. Patients had no relevant medical conditions or drug therapy that would exclude concomitant use of silodosin.
Patients who chose to enter the open-label extension study were all treated with silodosin 8 mg once daily. For those who had previously received double-blind treatment with silodosin 8 mg, the total treatment duration with silodosin was 12 months (i.e. 3 months of double-blind treatment and 9 months of open-label treatment), while for patients who previously received double-blind treatment with tamsulosin 0.4 mg or placebo, the treatment duration with silodosin therapy was 9 months. During open-label treatment, four follow-up visits (visits 9–12) were scheduled at week 2, 14, 27, and 40 (Fig. 1).
Safety parameters included vital signs (blood pressure and heart rate), electrocardiograms, laboratory tests, and physical examination. Patient-reported treatment-emergent adverse events (TEAEs) were recorded and classified based on the terminology of the Medical Dictionary for Regulatory Activities (MedDRA).
Efficacy variables included the change from baseline in the total International Prostate Symptom Score (IPSS, sum of questions 1–7), IPSS storage sub-score (sum of questions 2, 4, and 7), and IPSS voiding sub-score (sum of questions 1, 3, 5, and 6). Responses to IPSS questions 1–7 were measured on a six-point scale, ranging from 0 (not at all/none) to 5 (almost always/≥5 times). Additionally, the change from baseline in IPSS–QoL (question 8) was documented. Responses to IPSS question eight were measured on a seven-point scale, ranging from 0 (delighted) to 6 (terrible). Furthermore, change from baseline in maximum urinary flow rate (Q max) was measured by using free uroflowmetry.
Local ethics committee approval was obtained by each centre before patient recruitment. All study participants signed a new informed consent before entering the open-label extension study. The study was conducted in accordance with the guidelines of the International Conference on Harmonization for Good Clinical Practice and the Declaration of Helsinki.
Statistical analyses
No formal inferential statistics were performed for the open-label extension phase data; only descriptive statistics are presented. Continuous variables were expressed as mean ± SD or as percentage in case of frequency or categorical variables. Patients entered in the open-label extension study were also listed in the tables and grouped according to the treatment assigned at the randomization in the double-blind phase.
Results
Patient disposition
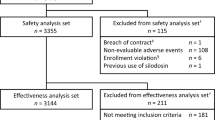
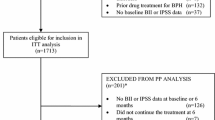
A total of 892 patients completed the 12-week, double-blind phase of the study, and 500 men chose to continue with the open-label extension study. Of the study participants who entered the 9-month open-label phase, 197 men received silodosin 8 mg, 204 men tamsulosin 0.4 mg, and 99 men placebo during the double-blind phase (Fig. 2). Of the 500 patients recruited in the open-label phase of the study, 466 (93.3 %) completed ≥6 months of silodosin treatment; 173/197 (87.8 %) completed 12 months since they were already treated with silodosin for 3 months during the double-blind phase. The mean age (SD) of men in the open-label phase was 66 (7.2) years. Other demographic characteristics are shown in Table 1. Approximately 42 % of patients had arterial hypertension, and the majority of these study participants took cardiovascular drugs. Specifically, 24 % of men entered in the open-label study used drugs acting on the renin-angiotensin system and 12 % were on β-blockers, 9 % on calcium channel antagonists, and 6 % on diuretics. Some patients (96, 19.2 %) took more than one antihypertensive drug.
Long-term safety
In total, 167 patients (33.4 %) experienced TEAEs in the open-label safety population. The most frequently reported TEAEs were “retrograde ejaculation” occurring in 9.0 % and influenza-like symptoms occurring in 2.8 % of patients (Table 2). All other TEAEs occurred in <2.0 % of patients. Dizziness was reported by only a few patients (0.8 %), and orthostatic (postural) hypotension was not reported at all.
Nine patients (1.8 %) experienced a total of nine serious TEAE during the open-label extension phase; all but one were considered to be unrelated to silodosin administration. One patient had a myocardial infarction; this man previously had silodosin 8 mg in the double-blind treatment phase in which he did not experience any adverse effect on blood pressure or heart rate. Due to the absence of any other risk factors for a cardiac event, this SAE was considered possibly related to silodosin administration. One patient died from a serious TEAE during the open-label extension phase; this TEAE was first reported during the double-blind period but unrelated to silodosin use.
A total of 13 patients (2.6 %) prematurely discontinued the open-label extension study due to 14 TEAEs. Twelve of these TEAEs were classified as definitely, probably or possibly related to silodosin administration. Eight patients (1.6 %) discontinued during the open-label extension phase due to “retrograde ejaculation”, and nine patients (1.8 %) discontinued due to the lack of efficacy (two patients reported both “retrograde ejaculation” and lack of efficacy). However, no patient discontinued the study due to dizziness or orthostatic hypotension. In terms of vital signs, laboratory parameters or 12-lead electrocardiograms, no clinical changes were found. Table 3 demonstrates systolic and diastolic blood pressures as well as heart rates for the different treatment groups and the overall study population.
The overall safety population, i.e. patients exposed to silodosin in the double-blind or open-label phase, was very similar to that of the open-label safety population. For this overall group, “retrograde ejaculation” was the most frequent TEAE (98/684 patients, 14.3 %). Dizziness occurred in only a few patients (10/684 men, 1.5 %). Overall, “retrograde ejaculation” infrequently led to patient discontinuation from the study (13/684 men, 1.9 %).
Long-term efficacy
The improvement seen in total IPSS as well as in storage and voiding sub-scores in patients who had previously received silodosin 8 mg or tamsulosin 0.4 mg during the double-blind phase maintained during the open-label extension phase (Fig. 3). In terms of total IPSS, a notable decrease (−2.7 ± 3.8) was found after week 14 of the open-label treatment phase in patients who previously received placebo in the double-blind period (Fig. 3a). A less pronounced improvement was seen in patients who were previously treated with silodosin (−0.82 ± 4.2) or tamsulosin (−0.83 ± 3.8) (Table 4).
Change of symptoms during the 9-month open-label phase during which all patients, who were previously treated with silodosin 8 mg, tamsulosin 0.4 mg, or placebo for 3 months (double-blind phase), received silodosin 8 mg once daily. Graphs illustrate absolute changes of a total IPSS, b IPSS storage sub-score, c IPSS voiding sub-score, d quality of life. Pre-random IPSS score at baseline (before 3-month double-blind phase); DB double blind, IPSS International Prostate Symptom Score, QoL quality of life
A similar pattern was observed for the IPSS storage sub-score. Patients who previously took silodosin 8 mg or tamsulosin 0.4 mg had a further slight improvement after week 14 of the open-label extension phase which was then sustained until the end of treatment (Fig. 3b). Patients who previously took placebo had a notable improvement with a change from baseline of −1.15 ± 1.9 after week 14 of the open-label extension phase.
Improvements of the IPSS voiding sub-score in patients who were previously treated with silodosin or tamsulosin were maintained throughout the open-label phase. Patients who previously used placebo showed an improvement in the IPSS voiding sub-score (Fig. 3c). The change from baseline was −1.54 ± 2.7 after week 14 of the open-label extension phase, and there was a trend towards a gradual improvement during the open-label extension phase.
IPSS–QoL showed a slight additional improvement in all three treatment groups during the open-label extension phase with silodosin therapy (Fig. 3d). Patients who previously received placebo showed the greatest improvement. The mean changes of IPSS–QoL from the beginning until the end of double-blind period were −0.41 ± 1.0 for previously with silodosin 8 mg treated, −0.31 ± 1.1 for previously with tamsulosin 0.4 mg treated, and −0.72 ± 1.0 for previously with placebo-treated patients.
Q max only changed marginally during the open-label extension phase. Patients who were treated with silodosin or placebo during the double-blind phase improved slightly by week 52 (mean changes +0.63 ± 4.9 and +0.47 ± 5.7 ml/s, respectively), whereas Q max in patients who were treated with tamsulosin during the double-blind phase remained nearly unchanged (+0.01 ± 4.7 ml/s).
Discussion
This is the first long-term study in European patients with LUTS/BPH, confirming the safety and efficacy of silodosin 8 mg once daily during a 9-month open-label treatment period. Only 33.4 % of patients reported any TEAE, most being mild or moderate in severity. There were no relevant changes in vital signs, laboratory parameters, or 12-lead electrocardiograms confirming the excellent efficacy of silodosin in long-term users.
Patient demographics of this study appear to be representative of men with LUTS/BPH seen in real clinical practice [30]. These patients are usually older than 60 years of age, have arterial hypertension, take concomitant antihypertensive agents, and frequently suffer of cardiac comorbidities. A major treatment concern in prescribing α-blockers for LUTS/BPH in this patient group is the potential decrease of arterial blood pressure which may manifest in orthostatic hypotension, dizziness, or falls. These TEAEs were the main concerns of primary care physicians when prescribing drugs for this group of patients, as demonstrated in a recent European survey [23]. In the present study, 42 % of patients had arterial hypertension and the majority were on antihypertensive agents. Dizziness was rarely reported, and orthostatic hypotension was not seen at all, confirming results of a previously published North American phase III open-label extension study with silodosin 8 mg once daily [24].
The most commonly reported TEAE was ejaculatory dysfunction which was previously thought to be and classified as “retrograde ejaculation” [25]. Anejaculation, together with other ejaculation disorders (e.g. reduced semen quantity, reduced seminal emission force, and no semen), is generally classified as ejaculatory dysfunction. These disorders are fully reversible after treatment discontinuation and are not a safety concern as there is no impact on spermatogenesis. Ejaculation disorders are a consequence of the high selectivity of silodosin and occurred in 9.0 % of patients of our study, especially in men who received placebo in the double-blind study phase.
Evidence from two 12-week studies in the USA and one 12-week study in Japan suggests that patients with silodosin-related ejaculatory dysfunction have a greater symptomatic response and IPSS improvement [26, 27]. In line with previous silodosin studies, the discontinuation rate due to ejaculation disorders during our open-label phase was low (0.8 %), confirming the high treatment persistence even in long-term silodosin studies. A more pronounced efficacy profile of silodosin in patients with ejaculatory dysfunction combined with a minor importance for sexually related TEAEs in a cohort of elderly men, who often have preexistent ejaculatory problems [28, 29], may explain why ejaculation disorders have rarely resulted in treatment discontinuations.
Although the absence of a placebo control group is a limitation of any open-label study, it became evident that the efficacy observed during the double-blind treatment period for patients treated with α-blockers in terms of total IPSS and IPSS sub-scores was similar or even more pronounced in the open-label extension phase of the study. These findings are consistent with results of three 12-week randomized, double-blind studies demonstrating that silodosin significantly improved IPSS compared with placebo (mean reduction in total IPSS −6.4 to −8.3 vs. −3.5 to −5.3) [18–20]. Patients who previously received placebo during the double-blind period showed a rapid improvement of symptoms during the open-label phase, achieving a mean decrease in total IPSS of approximately three points which is likely to be perceptible for the patients. Furthermore, all treatment groups irrespective of the previous treatment in the open-label phase showed an additional improvement in IPSS–QoL question, with the greatest improvement in patients previously treated with placebo.
Conclusions
The results of this 9-months open-label extension study with silodosin 8 mg once daily demonstrate that this highly uro-selective α1A–blocker is safe and efficacious in men with LUTS/BPH. Silodosin rarely led to dizziness and was not associated with orthostatic hypotension, especially in the patient cohort who used antihypertensive medication. Ejaculation disorders were reported as significant in 9.0 % of patients, but were the reason for study discontinuation in only 1.6 %.
References
Kupelian V, Wei JT, O’Leary MP, Kusek JW, Litman HJ, Link CL, McKinlay JB, BACH survey investigators (2006) Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) Survey. Arch Int Med 166:2381–2387
Berry SJ, Coffey DS, Walsh PC, Ewing LL (1984) The development of human benign prostatic hyperplasia with age. J Urol 132:474–479
Sexton CC, Coyne KS, Kopp ZS, Irwin DE, Milsom I, Aiyer LP, Tubaro A, Chapple CR, Wein AJ, EpiLUTS Team (2009) The overlap of storage, voiding and postmicturition symptoms and implications for treatment seeking in the USA UK and Sweden: EpiLUTS. BJU Int 103(Suppl 3):12–23
van Koeveringe GA, Vahabi B, Andersson KE, Kirschner-Hermanns R, Oelke M (2011) Detrusor underactivity: a plea for new approaches to a common bladder dysfunction. Neurourol Urodyn 30:723–728
Oelke M, Baard J, Wijkstra H, de la Rosette JJ, Jonas U, Höfner K (2008) Age and bladder outlet obstruction are independently associated with detrusor overactivity in patients with benign prostatic hyperplasia. Eur Urol 54:419–426
Chapple CR, Roehrborn CG (2006) A shifted paradigm for the further understanding, evaluation, and treatment of lower urinary tract symptoms in men: focus on the bladder. Eur Urol 49:651–658
Oelke M, Bachmann A, Descazeaud A, Emberton M, Gravas S, Michel MC, N’Dow J, Nordling J, de la Rosette J, European Association of Urology (2013) EAU Guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms, including benign prostatic obstruction. Eur Urol 64:118–140
Chapple CR (2004) Pharmacological therapy of benign prostatic hyperplasia/lower urinary tract symptoms: an overview for the practising clinician. BJU Int 94:738–744
Lepor H, Auerbach S, Puras-Baez A, Narayan P, Soloway M, Lowe F, Moon T, Leifer G, Madsen P (1992) A randomized, placebo-controlled multicenter study of the efficacy and safety of terazosin in the treatment of benign prostatic hyperplasia. J Urol 148:1467–1474
Chapple CR, Carter P, Christmas TJ et al (1994) A three month double-blind study of doxazosin as treatment for benign prostatic bladder outlet obstruction. Br J Urol 74:50–56
Fine SR, Ginsberg P (2008) Alpha-adrenergic receptor antagonists in older patients with benign prostatic hyperplasia: issues and potential complications. J Am Osteopath Assoc 108:333–337
Lowe FC (2004) Role of the newer alpha, -adrenergic-receptor antagonists in the treatment of benign prostatic hyperplasia-related lower urinary tract symptoms. Clin Ther 26:1701–1713
Souverein PC, Van Staa TP, Egberts AC, De la Rosette JJ, Cooper C, Leufkens HG (2003) Use of alpha-blockers and the risk of hip/femur fractures. J Intern Med 254:548–554
Thorpe A, Neal D (2003) Benign prostatic hyperplasia. Lancet 361:1359–1367
Michel MC, Grübbel B, Möllhoff S et al (1994) 1-Adrenoceptor affinities of drugs for the treatment of benign prostatic hyperplasia in human prostate, rat tissues and at cloned subtypes. Abstract presented at: 23rd Congress of the Société Internationale d’Urologie; September 18–24, Sydney, Australia. Abstract 649
Hatano A, Takahashi H, Tamaki M, Komeyama T, Koizumi T, Takeda M (1994) Pharmacological evidence of distinct alpha 1-adrenoceptor subtypes mediating the contraction of human prostatic urethra and peripheral artery. Br J Pharmacol 113:723–728
Tatemichi S, Kobayashi K, Maezawa A, Kobayashi M, Yamazaki Y, Shibata N (2006) Alpha1-adrenoceptor subtype selectivity and organ specificity of silodosin (KMD-3213). Yakugaku Zasshi 126:209–216
Chapple CR, Montorsi F, Tammela TL, Wirth M, Koldewijn E, Fernandez EF, European Silodosin Study Group (2011) Silodosin therapy for lower urinary tract symptoms in men with suspected benign prostatic hyperplasia: results of an international, randomized, double-blind, placebo- and active-controlled clinical trial performed in Europe. Eur Urol 59:342–352
Kawabe K, Yoshida M, Homma Y, Silodosin Clinical Study Group (2006) Silodosin, a new alpha1A-adrenoceptor-selective antagonist for treating benign prostatic hyperplasia: results of a phase III randomized, placebo-controlled, double-blind study in Japanese men. BJU Int 98:1019–1024
Marks LS, Gittelman MC, Hill LA, Volinn W, Hoel G (2009) Rapid efficacy of the highly selective alpha1A-adrenoceptor antagonist silodosin in men with signs and symptoms of benign prostatic hyperplasia: pooled results of 2 phase 3 studies. J Urol 181:2634–2640
Miller J, Carson CC (2007) Alpha blockers and ejaculatory function: a state of the art review. Curr Sex Health Rep. 4:141–144
Osman NI, Chapple CR, Cruz F, Desgrandchamps F, Llorente C, Montorsi F (2012) Silodosin: a new subtype selective alpha-1 antagonist for the treatment of lower urinary tract symptoms in patients with benign prostatic hyperplasia. Expert Opin Pharmacother 13:2085–2096
Montorsi F, Mercadante D (2013) Diagnosis of BPH and treatment of LUTS among GPs: a European survey. Int J Clin Pract 67:114–119
Marks LS, Gittelman MC, Hill LA, Volinn W, Hoel G (2009) Silodosin in the treatment of the signs and symptoms of benign prostatic hyperplasia: a 9-month, open-label extension study. Urology 74:1318–1322
van Dijk MM, de la Rosette JJ, Michel MC (2006) Effects of α1-adrenoceptor antagonists on male sexual function. Drugs 66:287–301
Roehrborn CG, Kaplan SA, Lepor H, Volinn W (2011) Symptomatic and urodynamic responses in patients with reduced or no seminal emission during silodosin treatment for LUTS and BPH. Prostate Cancer Prostatic Dis. 14:143–148
Homma Y, Kawabe K, Takeda M, Yoshida M (2010) Ejaculation disorder is associated with increased efficacy of silodosin for benign prostatic hyperplasia. Urology 76:1446–1450
Hellstrom WJ, Giuliano F, Rosen RC (2009) Ejaculatory dysfunction and its association with lower urinary tract symptoms of benign prostatic hyperplasia and BPH treatment. Urology 74:15–21
Blanker MH, Bosch JL, Groeneveld FP, Bohnen AM, Prins A, Thomas S, Hop WC (2001) Erectile and ejaculatory dysfunction in a community-based sample of men 50 to 78 years old: prevalence, concern, and relation to sexual activity. Urology 57:763–768
Hutchison A, Farmer R, Chapple C, Berges R, Pientka L, Teillac P, Borkowski A, Dobronski P (2006) Characteristics of patients presenting with LUTS/BPH in six European countries. Eur Urol 50:555–561
Acknowledgments
This study was initiated and supported by Recordati Industria Chimica e Farmaceutica SpA, Milan, Italy. The authors would like to thank Mr. Alessandro Antonellini and Mr. Massimo Casi for their valuable support with regard to study monitoring, data summary, and proof reading.
Conflicts of interest
Nadir I. Osman has no conflict of interest. Christopher R. Chapple is a consultant and researcher for Allergan, Astellas, Pfizer, and Recordati. Teuvo L. Tammela is a consultant and researcher for Astellas, Pfizer, and Recordati. Andreas Eisenhardt is speaker, advisor and/or trial participant of Berlin-Chemie, Ipsen, Janssen-Cilag, Lilly, Recordati, and Takeda. Matthias Oelke is speaker, advisor and/or trial participant of Apogepha, Astellas, GlaxoSmithKline, Lilly, Mundipharma, Pfizer, Recordati, and Sophiris.
Ethical standard
The trial was registered under clinical trials registration number NCT00359905. Ethics committee approval was obtained for each centre, and written informed consent was obtained from all study participants. The study was designed and performed according to the GCP recommendations and the 1964 Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Osman, N.I., Chapple, C.R., Tammela, T.L. et al. Open-label, 9-month extension study investigating the uro-selective alpha-blocker silodosin in men with LUTS associated with BPH. World J Urol 33, 697–706 (2015). https://doi.org/10.1007/s00345-015-1519-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1519-2