Abstract
Objectives
Women are under-represented in Radiology, both globally and in Ireland. An annual review of the medical workforce in Ireland for the year 2021–2022 revealed that although the overall gender breakdown of trainees is similar, with 56% female and 44% male trainees, certain specialities have disproportionate numbers of a given gender. Females only account for 38% of Irish Radiology trainees, one of the lowest of all the specialties. The cause for this disparity is likely multifactorial, but a lack of interest in applying for Radiology training by female doctors is a possible cause. The objectives of this study were to identify specific factors that attract or deter intern doctors from considering a career in Radiology and to identify underlying gender-specific differences.
Materials and methods
Anonymous online surveys were distributed to 50% of the intern population in Ireland between May and June 2022. The survey included questions on demographics, prior radiology exposure, and dedicated multiple-choice questions for those either considering or not considering radiology, which were subdivided into potentially influencing factors.
Results
Two-hundred-seven interns responded giving a response rate of 48.3%, which totalled almost 25% of the interns in Ireland. For those interns considering radiology, significantly more male interns (n = 24/67, 35.8%) are considering radiology compared with females (n = 26/139, 18.71%), (p < 0.009). Significantly more females were deterred by the perception of radiology as a male-based speciality (p < 0.004).
Conclusion
Significantly fewer females are considering radiology, deterred by physics knowledge, use of technology, and, significantly, by the perception of radiology as a male-dominated speciality.
Clinical relevance statement
This survey highlights important reasons that female interns are deterred from radiology. It will help direct future medical training and doctor recruitment policies, with a view to addressing the ongoing gender disparity in the Irish radiology workforce.
Key Points
-
Women are under-represented in the Irish and global Radiology workforce.
-
Female interns are dissuaded from Radiology as a career by their perception of Radiology as male-dominated.
-
This survey will shape medical training and doctor recruitment policies to improve gender diversity in radiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The importance of diversity, including gender diversity, in the medical sector cannot be overstated. It impacts patient outcomes [1,2,3], reduces bias in patient care [4], and in a myriad of situations trumps ability when solving complex problems [5]. Gender diversity is lacking in Radiology where women are under-represented, accounting for 33.5% of Radiologists globally [6]. Although, encouragingly, when stratified for age, there is increasing representation of female Radiology consultants with successive generations, increasing to 48%, for Radiologists aged under 35 years globally [6], a lack of gender diversity persists within the Irish Radiology workforce with female Radiology consultants only accounting for 39% of the workforce, one of the lowest of all the specialities [7].
Causes for the under-representation of female consultants in Radiology are likely multifactorial and may relate to barriers identified in both healthcare and corporate sectors. These barriers relate to ‘glass ceilings’ referring to invisible barriers to career advancement, such as institutional culture and bias, and ‘leaky pipelines’, referring to the loss of women along their career path [2, 8]. It may also be, in part, due to fewer females in Radiology training, given that of all the training specialities, the Radiology training scheme in Ireland has the second lowest proportion of female trainees, with females accounting for 40% [7]. This too may be multifactorial, with the potential for bias at the application stage, during the appointment, and loss of females along their training path. It may also relate to lower numbers of female doctors applying to Radiology training schemes in the first place.
A wealth of literature, including systematic reviews and meta-analyses [9,10,11,12,13,14,15,16], addresses factors influencing medical student’s career choices, but fewer studies assess doctor’s career choices. Intern year is the first mandatory clinical year immediately following medical school graduation and is typically the starting point for doctors in Ireland to consider planning speciality career choices.
Insights into what attracts, dissuades, and motivates doctors, particularly female doctors in Ireland to pursue Radiology is vital to address the gender disparity and shape both medical training and recruitment policies. The aims of this research were as follows:
-
1.
To identify specific factors that attract or deter intern doctors from considering a career in Radiology.
-
2.
To identify if there are gender-specific differences in those influential factors.
Materials and methods
Ethical approval
The aim of this study was to assess factors that attract or discourage interns in Ireland from considering a career in Radiology, by means of an anonymous online survey. At the time of this study, there were 854 interns located across six intern networks in Ireland, comprising over 50 hospital sites. Requests for ethical approval were sent to each hospitals’ Research Ethics Committee (REC), and at the time of survey dissemination, ethical approval had been granted by sufficient RECs to disseminate the survey to three of the six intern networks.
Inclusion and exclusion criteria
Inclusion criteria: interns in training in the Republic of Ireland were invited to participate.
Exclusion criteria: none.
Date range and data retrieval
An anonymous online survey, hosted on the online platform ‘Survey Monkey’ was disseminated to interns in Ireland inviting them to participate. The survey was disseminated between May–July 2022, based on successful ethical approval at individual clinical sites. Dissemination of the survey in May of the clinical year meant participating interns had at least ten months of exposure to, and interactions with, a Radiology Department.
The invitation to participate was accompanied by an information leaflet and links, both HTML and a QR code to the online survey. The information leaflet contained information regarding the purpose of the survey, that it was anonymous, and that it was voluntary without obligation to participate.
Survey questionnaire
-
All participants were asked to provide demographic data including:
-
Gender: (female, male, transgender female, transgender male, non-binary, other, prefer not to say).
-
-
All participants were asked to select their type, if any, of previous radiology exposure (none, didactic lectures, medical school placement within a radiology department, elective placement within a radiology department, interaction with a radiology department as part of their job, attendance at a radiology conference, family member or friend is a radiologist).
-
All participants were asked to answer a multiple-choice question (MCQ), selecting overall factors that they considered important when choosing a career speciality. These factors were broadly grouped into categories of influential factors.
-
Training scheme factors (duration, geographical location in one site).
-
Job factors (job flexibility, part-time or remote work, job satisfaction, intellectual stimulation, use of technology).
-
Patient-related factors (direct patient contact, impact on patient care).
-
Prestige and income (perception of the speciality by others, recognition, high income).
-
Other factors (availability of jobs, having a mentor, research opportunities, compatibility with childcare needs).
-
An open text box for additional comments.
-
-
Participants were asked to answer either one of two MCQ stems, depending on whether they were or were not considering a career in radiology.
Those considering radiology as a career were asked to answer an MCQ, selecting factors that attracted them to radiology, broadly grouped into:
-
Training scheme factors (duration, location primarily in one geographic centre).
-
Previous exposure (formal medical school exposure, previous mentorship).
-
Job factors (broad range of knowledge in lots of specialties, interest in anatomy, interest in physics, interest in technology, intellectually stimulating, interventional procedures, having a clearly defined, task-based workday, minimal paperwork, job flexibility, remote or part-time work, job opportunities, potential for research, high income).
-
Patient factors (impact on patient care, reduced patient interactions).
-
Perception of radiology (positive perception personally, positive perception by peers, positive experience within a department).
-
An open text box for additional comments.
Those not considering radiology were asked to answer an MCQ, selecting factors that deterred them from radiology, broadly grouped into:
-
Training scheme factors (formal examinations throughout the scheme, primarily training in one geographic centre).
-
Previous exposure (lack of formal exposure in medical school, lack of exposure to a radiology department in general, lack of a mentor).
-
Job factors (physics knowledge, anatomy knowledge, requiring a broad range of knowledge in lots of specialities, being a consultant to other consultants, radiation exposure, working in the dark, using technology, having a task-based structured day, interventional procedures, lack of job flexibility, lack of job availability).
-
Patient factors (lack of patient contact, lack of acknowledgment).
-
Perception of radiology (negative perception personally, negative perception by colleagues, previous negative experience with a department, perception as a male-dominated speciality, lack of job satisfaction).
-
An open text box for additional comments.
-
All participants were invited to answer an MCQ regarding the social media/ television portrayal of Radiologists (in a negative light, as isolated, socially awkward individuals working in the dark, as a predominantly male-based speciality).
-
All participants were invited to leave any other insightful comments.
Data analysis and statistical tests
This survey asked participants to select factors that attract or dissuade them from choosing radiology, to gain an overall insight into trends regarding workforce disparity. Anonymous raw data from SurveyMonkey were entered into Microsoft Excel and transferred to the software package GraphPad Prism to perform statistical analysis.
A single transgender male intern responded to this survey. Their responses were included in any ‘overall’ analysis, but excluded from the gender-specific sub-group analyses, as inclusion may potentially identify them, and anonymity was our priority.
Demographic data were translated into percentages for descriptive purposes. Categorical variables were described using a contingency table and analysed with Chi-squared tests or Fischer’s exact test. For all statistical tests, a p-value < 0.05 was considered statistically significant.
Results
Intern demographics
There were 854 interns in Ireland between 2021–2022. The survey was distributed to 3 of the 6 intern networks, totalling approximately 50% of the intern cohort (n = 427 approximately), requesting their participation in the study. From this population, there were 207 respondents, yielding a response rate of 48.5% which is felt to be a representative sample. Of the 207 intern respondents; 67.1% were female (n = 139/207) 32.4% were male (n = 67/207) and 0.48% identified as transgender male (n = 1/207) (Fig. 1). None of the interns felt that transgender female or non-binary described them best, nor did any intern select the ‘prefer not to say’ option.
General career choice
Of the potential factors influencing general career choice (Fig. 2), the most frequently chosen factor for all interns was ‘job satisfaction’, selected by 88.8%. This was closely followed by intellectual stimulation (67.9%), training duration (57.7%), job availability (57.8%), and direct patient contact (57.3%). When these general factors were stratified by gender (Fig. 3), differences in influential factors became apparent. Significantly more males (n = 18/67, 26.9%) than females (n = 17/138, 12.3%) selected the ‘use of technology’ as an important factor, (p < 0.016). Significantly more females (n = 52/138, 88.1%) than males (n = 7/67, 11.9%) selected a job being ‘compatible with childcare’ as an influential factor when choosing a career (p < 0.001).
Consideration of Radiology as a career
Of the 50 interns considering radiology, (n = 24/67, 35.8%) were male and (n = 26/139, 18.7%) were female (Fig. 4). Chi-squared Test of Independence revealed gender was associated with choice of radiology as a career (x2 (1, n = 207) = 7.549, p = 0.02) and analysis with Fischer’s exact test revealed significantly more male interns (n = 24/67, 35.8%) are considering radiology compared with females (n = 26/139, 18.7%) (p < 0.01).
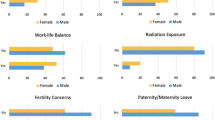
The factors for not considering radiology are stratified by gender and displayed as % for graphical purposes in Fig. 5. The commonest deterring factors for both genders were ‘lack of patient contact’ and ‘lack of medical school exposure’. Sub-group analysis with Fischer’s exact test revealed statistically significant gender differences in the perception of Radiology as a male-dominated speciality (p = 0.004) with significantly more females than males citing this perception as a deterring factor. There was a trend for a greater percentage of females to select ‘physics knowledge’ and ‘use of technology’ as deterring factors, although they did not reach statistical significance.
Discussion
Almost one-quarter of Irish interns in this study are considering radiology, which parallels the results of a recent single-centre study, where 30.5% of Irish medical students are considering radiology as a career [16]. Of concern is that significantly fewer female interns are considering radiology as a career (18.7%), compared with male interns (35.8%). This gender-related difference in radiology interest has been reported in a cohort of Irish medical students [16], United Kingdom medical graduates [12], and a meta-analysis involving > 26,000 students globally [17]. How are we to reduce gender disparity in the radiology workforce, partially attributed to the ‘leaky pipeline’ of loss of women along their career path, if we have fewer female doctors considering radiology as a career to begin with?
‘Job satisfaction’ was the most frequently chosen factor influencing general career choice, for both male and female interns, which correlates with a meta-analysis of over 800,000 medical students [10]. When stratified by gender, differences emerged regarding motivating factors influencing overall career choice, with significantly more males (26.9%) than females (12.3%) selecting ‘use of technology’ as an influential factor when choosing a career. Significantly more female interns (88%) selected ‘compatibility with childcare’ as an influential factor when considering a career. This gender inequity around career choice mirrors the literature which shows that more female doctors state that career choice is influenced by children [18, 19] and female doctors delay childbearing due to career demands [20]. Reasons underpinning this gender inequity around childcare are multifactorial and fall outside the scope of this discussion. However, if we acknowledge that female career choices are disproportionally affected by child-rearing, we can showcase radiology as an attractive career for balancing both work and childcare, with its task-based workday and the potential to work flexibly and remotely. Notably, in Ireland, radiology training is one of the few training schemes to occur in primarily one training centre, reducing geographical upheaval on families.
The top two deterrents from pursuing radiology, by both male and female interns, were ‘lack of patient contact’ and ‘lack of previous exposure to radiology’. When stratified by gender, significantly more females cited ‘perception as a male-dominated speciality’ as a deterring factor. This troubling trend in perception has been documented previously [21] and contributes to a challenging cycle where a lack of gender diversity discourages females from pursuing radiology, which in turn compounds the gender disparity. More female interns were deterred from radiology by both ‘physics knowledge’ and ‘use of technology’, in contrast to the significantly higher proportion of male interns who selected ‘use of technology’ as an attractive factor in considering general career choice. This tendency for males to pursue and remain within technical specialities is well-documented in the literature, with surgery having higher male representation [7, 17] and is even seen in sub-specialities, with interventional radiology having only 16% female radiologists [22].
One limitation of this study was the discrepancy in the gender of the 207 intern respondents. Data relating to survey response behaviour is complex [23, 24] but females tend to respond more frequently than men [25], and our higher female response rate: 67.1% females (n = 139/207), 32.4% males (n = 67/207) and 0.48% transgender male (n = 1/207), parallels a recently published survey regarding consideration of radiology as a career by medical students, which had a female response rate of 62% [16]. Another limitation is that only 50% of the intern networks in Ireland could be surveyed due to the available ethical committee approval. Nonetheless, this represents a large cohort of participants and is considered representative of national trends.
This is the first Irish survey providing insight into motivating and deterring factors for doctors when considering radiology as a career. The results are profound, revealing significantly fewer female interns are considering radiology, but also identifying specific, potentially addressable factors for this. Female interns, in addition to considering childcare when selecting a career in general, are dissuaded from radiology by a lack of patient contact, lack of exposure to the speciality in medical school, physics knowledge, use of technology, and significantly, their perception of radiology as a male-dominated speciality. Strategies to address these concerns could centre around female radiologists and trainees speaking to intern cohorts, assuaging concerns around the physics curriculum, highlighting subspecialty areas within radiology with proportionally more patient contact, and the ability to work remotely, and also to train in one geographic location. In addition, the visibility of female radiology staff improves gender representation, provides interns with role models, fosters interest in the speciality, and establishes mentor-mentee relationships, which are valued by female doctors [19]. The benefits of diversity are far-reaching, reducing implicit bias in patient care [3, 4] and improving innovation [26]. Although the gender gap is closing, women are still notably under-represented in Radiology, and active steps must be taken by educators, employers, and leaders in radiology to promote an inclusive environment, attractive to female doctors.
Abbreviations
- MCQ:
-
Multiple-choice questions
- REC:
-
Research Ethics Committee
References
Cooper-Patrick L, Gallo J, Gonzales J (1999) Race, gender, and partnership in the patient-physician relationship. J Am Med Assoc 282:583–589
Surawicz C (2016) Women in leadership: why so few and what to do about it. J Am Coll Radiol 13:1433–1437
Wallis C, Jerath A, Coburn N et al (2022) Association of surgeon-patient sex concordance with postoperative outcomes. JAMA Surg 157:146–156
Davenport D, Alvarez S, Natesan M et al (2022) Faculty recruitment, retention, and representation in leadership: an evidence-based guide to best practices for diversity, equity, and inclusion from the council of residency directors in emergency medicine. West J Emerg Med 23:62–71
Page S (1993) The difference. How the power of diversity creates better groups, firms. Princeton University Press
Cater S, Yoon S, Lowell D et al (2018) Bridging the gap: identifying global trends in gender disparity among the radiology physician workforce. Acad Radiol 25:1052–1061
NDTP (2022–2023) NDTP HSE Medical Workforce Report (2022–2023) https://www.hse.ie/eng/staff/leadership-education-development/met/plan/ndtp-medical-workforce-report-2023.pdf
Weigel K, Kubik-Huch R, Gebhard C (2020) Women in radiology: why is the pipeline still leaking and how can we plug it? Acta Radiol 61:743–748
Arleo E, Bluth E, Francavilla M, Straus C, Reddy S, Recht M (2016) Surveying fourth-year medical students regarding the choice of diagnostic radiology as a specialty. J Am Coll Radiol 13:188–195
Yang Y, Li J, Wu X et al (2019) Factors influencing subspecialty choice among medical students: a systematic review and meta-analysis. BMJ Open 9:e022097
Fielding J, Major N, Mullan B et al (2007) Choosing a specialty in medicine: female medical students and radiology. AJR Am J Roentgenol 188:897–900
Lambert T, Smith F, Goldacre M (2018) Career specialty choices of UK medical graduates of 2015 compared with earlier cohorts: questionnaire surveys. Postgrad Med J 94:191–197
Murias Quintana E, Sánchez Lasheras F, Fernández-Somoano A et al (2017) Choice of the specialty of diagnostic radiology by results of the competitive examination to assign residency positions from 2006 to 2015. Radiologia 59:232–246
Pyatigorskaya N, Madson M, Di Marco L (2017) Women’s career choices in radiology in France. Diagn Inter Imaging 98:775–783
Abduljabbar A, Alnajjar S, Alshamrani H et al (2020) The influence of gender on the choice of radiology as a specialty among medical students in Saudi Arabia: cross-sectional study. Interact J Med Res 9:e14666
Lynch T, Bockhold S, McNulty J (2022) Factors influencing the choice of radiology as a medical specialty in Ireland. Eur J Radiol 151:110297
Levaillant M, Levaillant L, Lerolle N, Vallet B, Hamel-Broza J (2020) Factors influencing medical students’ choice of specialization: a gender based systematic review. EClinicalMedicine 28:100589
Lambert T, Smith F, Goldacre M (2017) Combining parenthood with a medical career: questionnaire survey of the UK medical graduates of 2002 covering some influences and experiences. BMJ Open 7:e016822
Simpson A, Cusiamno M, Baxter N (2021) The inconvenience of motherhood during a medical career. CMAJ 193:1465–1466
Shen M, Tzioumis E, Anderen E et al (2022) Impact of mentoring on academic career success for women in medicine: a systematic review. Acad Med 97:444–458
Grimm L, Lowell D, Cater S, Yoon S (2017) Differential motivations for pursuing diagnostic radiology by gender: implications for residency recruitment. Acad Radiol 24:1312–1317
Theodoulou I, Dost S et al (2022) The interventional radiology gender gap: perspectives from the international IR training survey. Br J Radiol 95:20210726
Brüggen E, Wetzels M, De Ruyter K, Schillewaert N (2011) Individual differences in motivation to participate in online panels: the effect on response rate and response quality perceptions. Int J Mark Res 53:369–390
Smith G (2008) Does gender influence online survey participation?: A record-linkage analysis of university faculty online survey response behavior. ERIC document reproduction service no. ED 501717
Porter S, Whitcomb M (2005) Non-response in student surveys: the role of demographics, engagement and personality. Res High Educ 46:127–152
Hewlett S, Marshall M, Sherbin L (2013) How diversity can drive innovation. Harv Bus Rev 91:30–30
Acknowledgements
National University of Ireland Galway, NUIG, Radiology Dept. Interns in Ireland who participated and provided invaluable career insights.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Lorraine Murray.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have not been previously reported.
Methodology
-
Observational
-
Multicentre study
Additional information
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Murray, L., Ni Mhuircheartaigh, J. Female interns are not choosing radiology as a career—national survey providing insights into gender imbalance. Eur Radiol (2024). https://doi.org/10.1007/s00330-024-10943-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-024-10943-w