Abstract
Objectives
It is unclear which selection strategy, plain CT vs. CT perfusion (CTP), is more powerful in predicting outcome after mechanical thrombectomy (MT). We aimed to compare the effect of plain CT and CTP in predicting outcome after MT within 6 h.
Methods
We conducted a prospective analysis of a retrospective cohort from our single-center study, which had occlusion of the internal carotid artery and middle cerebral artery up to the proximal M2 segment and received MT within 6 h. According to the Alberta Stroke Program Early CT Score (ASPECTS), patients were divided into a high-ASPECTS group (≥ 6) and a low ASPECTS group (< 6). Similarly, patients were divided into mismatch and no-mismatch groups according to the DEFUSE3 criteria for CTP. A good outcome was defined as a 90-day modified Rankin Scale (mRS) score of ≤ 3. Univariate and binary logistic regression analyses were used to investigate the association between different imaging modality and 90-day mRS score, and mortalities, respectively.
Results
The high ASPECTS group included 307 patients (89.2%). The mismatch group included 189 (54.9%) patients meeting the DEFUSE3 criterion. Compared to the low ASPECTS group, the high ASPECTS group had a good outcome (odds ratio (OR), 2.285; [95% confidence interval (CI) (1.106, 4.723)], p = 0.026) and lower mortality (OR, 0.350; [95% CI (0.163, 0.752)], p = 0.007). However, there were no significant differences in good outcomes and mortality between the mismatch and no-mismatch groups.
Conclusions
Compared with plain CT, CTP does not provide additional benefits in the selection of patients suitable for MT within 6 h.
Clinical relevance statement
CT perfusion is not superior to plain CT for the prediction of clinical outcomes when selecting patients for mechanical thrombectomy in the first 6 h. In that clinical setting, plain CT may be safe in the absence of perfusion data.
Key Points
• The advantage of CT perfusion (CTP) over CT in pre-mechanical thrombectomy (MT) screening has not been proven for patients with a large infarct core.
• CTP is not better than plain CT in predicting good outcome following MT within 6 h.
• Plain CT is sufficient for selecting patients suitable for MT within 6 h of large artery occlusion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Large vessel occlusive stroke accounts for approximately one-third of acute ischemic stroke (AIS) and can lead to severe disability and high mortality [1]. A number of randomized controlled trials have demonstrated that MT was an effective treatment for patients with large vessel occlusion (LVO) within 6 h by saving salvageable tissue [2,3,4,5,6,7,8,9]. However, patients with large core infarcts tend to have poor outcomes despite successful recanalization. The Alberta Stroke Program Early CT Score (ASPECTS) evaluated on plain CT is the most commonly used method to exclude large core infarcts in RCTs because of its convenience and simplicity.
CTP is an advanced imaging modality that can provide more accurate information about infarct core volumes before MT. CTP had been used in several clinical trials to enroll patients who might benefit from MT beyond the 6-h time window, such as the DEFUSE3 (Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke 3), DAWN (Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo), and BAOCHE (Basilar Artery Occlusion Chinese Endovascular) trials [10,11,12].
However, it is still unclear which selection strategy, plain CT or CTP, is more powerful for predicting MT outcomes within the 6-h time window. Previous investigations conducted by Nogueira RG et al [13] and Jadhav AP et al [14] have provided invaluable insights and information regarding this matter. Their studies both categorize patients into groups based on the presence or absence of CTP examination and compare the differences in their prognoses. However, this study design possesses certain limitations. For instance, Jadhav AP et al’s study encompassed the analysis of data from seven randomized controlled trials (RCTs). It is noteworthy that only two RCTs (the EXTEND-IA and SWIFT-PRIME studies) explicitly indicated the utilization of CTP for patient selection [2, 6]. As a result, many patients underwent CTP without consistent criteria for inclusion or exclusion based on CTP, and some patients were not selected based on CTP at all, leading to substantial bias. Additionally, even within the same SWIFT-PRIME study, there were differences in CTP criteria between the first 71 patients and the later patients [2].
Hence, there are still unresolved aspects that necessitate the implementation of additional research designs. Based on these considerations, we designed this study to compare plain CT with CTP in predicting outcomes after MT with 6 h of LVO.
Methods
The study protocol was approved by the ethics committee of the Second Affiliated Hospital of Zhejiang University, School of Medicine. The study was conducted according to the principles expressed in the Declaration of Helsinki. Written informed consent for MT was obtained from all patients or their legally authorized representatives. Because patient information was deidentified and anonymized before being released to the researchers, the informed consent requirement for this study was waived by the Institutional Review Board.
We conducted a prospective analysis of a retrospective cohort from our single-center study involving a cohort of consecutive AIS patients (n = 390) who had occlusion of the internal carotid artery, middle cerebral artery up to the proximal M2 segment and underwent MT from October 2013 to December 2021. According to our protocol, all the patients received the plain CT to exclude hemorrhage and the CTP to determine LVO routinely on admission. For patients within a 4.5-h time window, if they met the criteria for intravenous recombinant tissue plasminogen activator (rtPA), they initially received intravenous rtPA [15]. These patients also underwent concurrent MT, without waiting for the effects of intravenous thrombolysis. Notably, our center consistently utilized the Solitaire stent retriever and aspiration catheters from October 2013 to December 2021. Iodixanol and iohexol were the contrast agents used.
Patients and clinical data
We enrolled patients who had (1) complete occlusion of the internal artery including internal carotid artery, middle cerebral artery up to the proximal M2 segment; (2) had an onset-to-puncture time within 6 h and underwent MT; and (3) had a recorded follow-up modified Rankin Scale (mRS) score at 3 months. We excluded patients who had only undergone no-contrast CT or CTP. We retrieved demographic, clinical, and imaging data including age and sex, risk factors: smoking, comorbid conditions such as history of hypertension, diabetes mellitus, atrial fibrillation, and stroke or transient ischemic attack history; previous medication history: antiplatelet usage, strain usage, baseline systolic/diastolic blood pressure, onset-puncture-treatment time, National Institutes of Health Stroke Scale (NIHSS) score [16] at admission, ASPECTS [17] at admission, thrombolysis before MT arterial occlusion lesion (AOL) [18] score, sICH, PH, mortality, and 90d-mRS score.
Patient groups
According to ASPECTS, patients were divided into high ASPECTS group (ASPECTS ≥ 6) and low ASPECTS group (ASPECTS < 6) [15]. We also divided the patients into mismatch group who meet DEFUSE3 criteria and no-mismatch group based on CTP data. The DEFUSE3 criterion included initial infarct volume (ischemic core) less than 70 ml, and a ratio of ischemic tissue volume to initial infarct volume of 1.8 or more, whereas the absolute volume of potentially reversible ischemia (penumbra) was 15 ml or more [10].
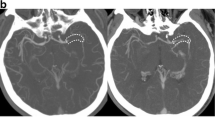
Imaging protocol
CTP was performed on a 64-slice CT scanner (SOMATOM Definition Flash; Siemens Healthcare Sector), including plain CT (120 kV, 320 mA, contiguous 5-mm axial slices, acquisition time 7 s) and volume CTP (100 mm in the z-axis, 4-s delay after the start of contrast medium injection, 74.5 s total imaging duration, 80 kV, 120 mA, slice thickness 1.5 mm, collimation 32 × 1.2 mm). Volume CTP consisted of 26 consecutive spiral acquisitions of the brain. All 26 scans were divided into 4 parts: (1) 2 scans with 3-s cycle time; (2) 15 scans with 1.5-s cycle time; (3) 4 scans with 3-s cycle time; and (4) 5 scans with 6-s cycle time. Axial slice coverage was 150 mm. A 60-ml bolus of contrast medium (iopamidol; Bracco Sine) with a single injection was used at a flow rate of 6 ml/s followed by a 20-ml saline chaser at 6 ml/s.
Imaging analysis
All perfusion images were retrospectively postprocessed using commercial software (MIStar; Apollo Medical Imaging Technology). The time to maximum of tissue residue function (Tmax) map was produced using standard singular value deconvolution without arterial input function (AIF) delay. The AIF was automatically selected, which was a global AIF from normal artery. Previously validated thresholds were applied in order to measure the baseline volume of hypoperfusion lesion (Tmax > 6 s) and infarct core (relative cerebral blood flow (rCBF) < 30% on CT. The ASPECTS [17] was assessed by Y.P. and W.Z. In the cases of any disagreements between the two, Z.C. was consulted for confirmation.
Outcome measures
Clinical outcome at 3 months was assessed with modified Rankin Score (mRS) ranging from 0, indicating no symptoms to 6, indicating death. Good outcome was defined as mRS 0–3 after MT. Safety outcomes were in-hospital mortality, PH (PH1: < 30% of the infarcted area with mild space-occupying effect; PH2: > 30% of the infarcted area with obvious mass effect), and sICH (hemorrhagic transformation was accompanied by worsening clinical symptoms or an increase in NIHSS score of ≥ 4 points) according to ECASS (European Collaborative Acute Stroke Study) II [9]. The assessment of hemorrhage transformation after MT was carried out by P.Y. and W.Z. In the case of any disagreements between the two researchers, Z.C. was consulted for confirmation.
Statistical analysis
Normally dismally distributed data were expressed as means ± s, and the average values between the two groups were compared using the t-test. Data with non-normal distributions are expressed as medians and quartiles (M (Q1, Q3)), and pairwise comparisons were performed using the Mann–Whitney U-test. Categorical data are expressed as percentages and were compared using the χ2 test. Associations of plain CT or CTP and outcome were determined using binary logistic regression models adjusted by baseline characteristics with a p < 0.1 in univariate analyses. All statistical analyses were performed using SPSS, version 22.0 (IBM). A p value < 0.05 was considered to indicate statistical significance. Y.P. completed the statistical analysis of the data and was responsible for it.
Results
There are a total of 390 patients with AIS within 6 h who had occlusion of the cerebral artery and underwent MT within 6 h from October 2013 to December 2021. Among the 390 patients, 46 patients underwent either plain CT or CTP. A total of 344 patients were enrolled in the final cohort for analysis (Fig. 1).
The predictive ability of ASPECTS within 6 h
The high ASPECTS group included 307 (89.2%) patients who underwent plain CT and low ASPECTS included 37 (10.8%) patients. The high ASPECTS group had shorter onset-to-puncture time (180 [126–245] versus 253 [168–304], p = 0.001), lower rate of smoking (83 (27%) versus 15 (40.5%), p = 0.086), and higher percentage of prior antiplatelet usage (59 (19.2%) versus 3 (8.1%), p = 0.097) than the low ASPECTS group.
For outcome variables, univariate analysis showed the high ASPECTS group had higher rate of good outcome (90d-mRS score ≤ 3, 178 (58.0%) versus 14 (37.8%), p = 0.020), and a lower rate of mortality (55 (17.9%) versus 14 (37.8%), p = 0.004) and sICH (33 (11.3%) versus 9 (25.0%), p = 0.020) than the low ASPECTS group. There were no significant differences in other variables including age, sex, the NIHSS score on admission, the rate of hypertension, diabetes, atrial fibrillation, previous stroke, intravenous thrombolysis (IVT), occlusion site, and AOL score (Table 1).
After adjusting for onset-to-puncture time, smoking, and antiplatelet drugs, the high ASPECTS group still had a better outcome (90d-mRS score ≤ 3, odds ratio (OR), 2.285, [95% confidence interval (CI) (1.106, 4.723)], p = 0.026), and lower rate of mortality (OR, 0.350, [95% CI (0.163, 0.752)], p = 0.007) and sICH (OR, 0.346, [95% CI (0.144,0.831)], p = 0.018). However, there were no significant differences in outcome (90d-mRS score ≤ 2) and rate of PH (Table 3, Fig. 2a).
The predictive ability of CTP within 6 h
The mismatch group included 189 (54.9%) patients who met the DEFUSE3 criterion on the basis of CTP and the no-mismatch group included 155 (45.1%) patients. The mismatch group had a higher ASPECTS on admission (8 [7,8,9] versus 8 [6,7,8,9], p = 0.003), lower NIHSS score on admission (14 [10,11,12,13,14,15,16,17,18] versus 16 [13,14,15,16,17,18,19,20], p = 0.003), and higher rate of diabetes (40 (21.2%) versus 22 (14.2%), p = 0.094). For clinical outcome, in univariate analysis, the mismatch group had higher rate of outcome (90d-mRS score ≤ 2, 86 (45.5%) versus 54 (34.8%), p = 0.045), and lower rate of mortality (29 (15.3%) versus 40 (25.8%), p = 0.016) and sICH (16 (8.9%) versus 26 (17.4%), p = 0.021). The two groups showed no significant differences in age, sex, the rate of hypertension, diabetes, atrial fibrillation, previous stroke, smoking, percentage of use of antiplatelet drugs and stain drugs, IVT, occlusion site, or ALO score (Table 2).
However, after adjusting for ASPECTS on admission, NIHSS score on admission, and diabetes, the mismatch group still had a lower rate of sICH (OR, 0.395, [95% CI (0.186, 0.839)], p = 0.016). There were no significant differences in outcome (90d-mRS score ≤ 2 or 90d-mRS score ≤ 3), rate of PH, or mortality rate in the multivariate analysis (Table 3, Fig. 2b).
Discussion
In our study, we found patient selection by plain CT was associated with good outcome and low mortality, whereas utilizing CTP for patient selection was not associated with good outcome and low mortality.
To date, there is no consensus about the effect of CT and CTP on outcome after MT. Nogueira et al [13] divided patients into CT group (n = 332) and CTP group (n = 372) according to the examination before MT and found that the CTP group did not have better outcome than the CT group. Dhillon et al [19] compared the CT group (n = 2610) with the CTP group (n = 593) in a larger study sample and found that the CTP group had improvement in functional disability at discharge compared with the CT group. A meta-analysis including 7 RCTs compared a CT group (n = 610) and CTP group (n = 738). The results showed similar good outcomes in patients with and without CTP before MT within 6 h [14].
One reason for the different results is that the criteria for excluding patients from MT by CTP are different. Therefore, we used the criteria of DEFFUSE3, which were tested in patient selection for MT beyond 6 h. In addition, different centers have their own clinical habits when choosing different examinations before MT, and CTP will increase the door-to-puncture time compared with CT, which causes selection bias. In the SWIFT-PRIME trial (a single card with thrombectomy as the primary endovascular treatment), CTP before MT could increase onset-to-puncture time due to time delay [20, 21]. In our center, we routinely performed both plain CT and CTP simultaneously during clinical work. CTP was used to reconstruct angiography, but not to select patients for MT within 6 h, to reduce bias. As a result, we found that it was not helpful to select to patients for MT based on DEFUSE3 standard comparing with ASPECTS.
The DEFUSE3 trial relied solely on the use of advanced imaging such as CT/MR perfusion or diffusion-weighted imaging for patient selection. Unfortunately, due to technical, logistical, and financial constraints, this poses significant challenges for many centers around the world [10]. In addition, in our data, nearly half of patients who benefited similarly from MT comparing with meet DEFUSE3 group would be excluded basing on the criteria of DEFUSE3.
The ASPECTS evaluated on plain CT is the most commonly used method to exclude large core infarcts because of its convenience and simplicity. It provides a semi-quantitative estimate of the identified core volume using visible low density as an alternative metric for core volume. Moreover, there are also several RCTs with the criterion of an ASPECTS ≥ 6 proving that MT was associated with good outcome only basing on plain CT [3,4,5]. Bhuva et al [22] also put forward that higher ASPECTS was associated with greater benefit from MT in DAWN. Interestingly, studies found that, in extend window (6–24 h), in which CTP had been proven useful in selecting patients, there were also no significant differences in the clinical outcomes of patients selected based on plain CT compared with those selected with CTP or magnetic resonance imaging (MRI) [23]. Basing on the above analysis and our data, there is reason to believe that using CTP to select patients for MT within 6 h is meaningless and may exclude many patients who could benefit from MT. Our data added evidence to current guidelines.
Our study has several limitations. Firstly, this was a retrospective design with potential risk of selection bias, although the data were collected prospectively. Secondly, we were a single-center study, and our conclusion only applies to patients who underwent MT within 6 h. Thirdly, the plain CT scan group and CTP group have the same population due to small sample size. Utilizing different grouping methods based on various trial specifications is better recommended in prospective trials to determine the suitability of these methods for patient selection. A randomized controlled trial providing definite data is needed.
Conclusion
Our data add evidence to current guidelines that the use of CTP in early time window (onset-to-puncture time within 6 h) is not helpful in selecting patients benefiting from MT and suggests that plain CT may be safe in the absence of CTP data. However, because our data was based on retrospective study, these findings must be properly confirmed in a prospective randomized controlled trial.
Abbreviations
- AIS:
-
Acute ischemic stroke
- AOL:
-
Arterial occlusive lesion
- ASPECTS:
-
Alberta Stroke Program Early CT Score
- CI:
-
Confidence interval
- CTP:
-
CT perfusion
- IQR:
-
Interquartile range
- IVT:
-
Intravenous thrombolysis
- LVO:
-
Large vessel occlusion
- mRS:
-
Modified Rankin Scale
- MT:
-
Mechanical thrombectomy
- NIHSS:
-
National Institutes of Health Stroke Scale
- OR:
-
Odds ratio
- PH:
-
Parenchymal hematoma
- RCTs:
-
Randomized controlled trials
- SD:
-
Standard deviation
- sICH:
-
Symptomatic intracerebral hemorrhage
- TIA:
-
Transient ischemic attack
References
Chen Z, Zhang M, Shi F et al (2018) Pseudo-occlusion of the internal carotid artery predicts poor outcome after reperfusion therapy. Stroke 49:1204–1209
Saver JL, Goyal M, Bonafe A et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372:2285–2295
Berkhemer OA, Fransen PS, Beumer D et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11–20
Goyal M, Demchuk AM, Menon BK et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372:1019–1030
Jovin TG, Chamorro A, Cobo E et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306
Campbell BC, Mitchell PJ, Kleinig TJ et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009–1018
Bracard S, Ducrocq X, Mas JL et al (2016) Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 15:1138–1147
Martins SO, Mont’Alverne F, Rebello LC et al (2020) Thrombectomy for stroke in the public health care system of Brazil. N Engl J Med 382:2316–2326
von Kummer R, Broderick JP, Campbell BC et al (2015) The Heidelberg Bleeding Classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke 46:2981–2986
Albers GW, Marks MP, Kemp S et al (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378:708–718
Nogueira RG, Jadhav AP, Haussen DC et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21
Jovin TG, Li C, Wu L et al (2022) Trial of thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med 387:1373–1384
Nogueira RG, Haussen DC, Liebeskind D et al (2021) Stroke imaging selection modality and endovascular therapy outcomes in the early and extended time windows. Stroke 52:491–497
Jadhav AP, Goyal M, Ospel J et al (2022) Thrombectomy with and without computed tomography perfusion imaging in the early time window: a pooled analysis of patient-level data. Stroke 53:1348–1353
Powers WJ, Rabinstein AA, Ackerson T et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50:e344–e418
Brott T, Adams HP Jr, Olinger CP et al (1989) Measurements of acute cerebral infarction: a clinical examination scale. Stroke 20:864–870
Pexman JH, Barber PA, Hill MD et al (2001) Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol 22:1534–1542
Bang OY, Saver JL, Kim SJ et al (2011) Collateral flow predicts response to endovascular therapy for acute ischemic stroke. Stroke 42:693–699
Dhillon PS, Butt W, Podlasek A et al (2022) Perfusion imaging for endovascular thrombectomy in acute ischemic stroke is associated with improved functional outcomes in the early and late time windows. Stroke 53:2770–2778
Goyal M, Menon BK, van Zwam WH et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387:1723–1731
Mokin M, Pendurthi A, Ljubimov V et al (2018) ASPECTS, large vessel occlusion, and time of symptom onset: estimation of eligibility for endovascular therapy. Neurosurgery 83:122–127
Bhuva P, Yoo AJ, Jadhav AP et al (2019) Noncontrast computed tomography Alberta Stroke Program Early CT Score may modify intra-arterial treatment effect in DAWN. Stroke 50:2404–2412
Nguyen TN, Abdalkader M, Nagel S et al (2022) Noncontrast computed tomography vs computed tomography perfusion or magnetic resonance imaging selection in late presentation of stroke with large-vessel occlusion. JAMA Neurol 79:22–31
Acknowledgements
Z.C. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Z.C. designed the whole study and supervised the whole project, monitored data collection, drafted the manuscript, and approved the final version of the manuscript. Concept and design: Y.P. and Z.C. Acquisition, analysis, or interpretation of data: Y.P., YC. Critical revision of the manuscript for important intellectual content: Y.P., YC, WZ, YH, YZ, ML. Statistical analysis: Y.P., YC. Obtained funding: Z.C., ML. All authors contributed to the development of the manuscript and approved the final draft. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding
This study was supported by the National Natural Science Foundation of China (81971101, 82171276).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Zhicai Chen.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent for MT was obtained from all patients or their legally authorized representatives. Because patient information was de-identified and anonymized before being released to the researchers, the informed consent requirement for this study was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained. The study protocol was approved by the ethics committee of the Second Affiliated Hospital of Zhejiang University, School of Medicine. The study was conducted according to the principle expressed in the Declaration of Helsinki.
Study subjects or cohorts overlap
None of the study subjects or cohorts has been previously reported.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pei, Y., Chen, Y., Zhong, W. et al. Effect of computed tomography vs. computed tomography perfusion on mechanical thrombectomy outcomes within 6 hours. Eur Radiol 34, 5331–5338 (2024). https://doi.org/10.1007/s00330-023-10545-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10545-y