Abstract
Objective
To assess success and safety of CT-guided procedures with narrow window access for biopsy.
Methods
Three hundred ninety-six consecutive patients undergoing abdominal or pelvic CT-guided biopsy or fiducial placement between 01/2015 and 12/2018 were included (183 women, mean age 63 ± 14 years). Procedures were classified into “wide window” (width of the needle path between structures > 15 mm) and “narrow window” (≤ 15 mm) based on intraprocedural images. Clinical information, complications, technical and clinical success, and outcomes were collected. The blunt needle approach is preferred by our interventional radiology team for narrow window access.
Results
There were 323 (81.5%) wide window procedures and 73 (18.5%) narrow window procedures with blunt needle approach. The median depth for the narrow window group was greater (97 mm, interquartile range (IQR) 82–113 mm) compared to the wide window group (84 mm, IQR 60–106 mm); p = 0.0017. Technical success was reached in 100% (73/73) of the narrow window and 99.7% (322/323) of the wide window procedures. There was no difference in clinical success rate between the two groups (narrow: 86.4%, 57/66; wide: 89.5%, 265/296; p = 0.46). There was no difference in immediate complication rate (narrow: 1.3%, 1/73; wide: 1.2%, 4/323; p = 0.73) or delayed complication rate (narrow: 1.3%, 1/73; wide: 0.6%, 1/323; p = 0.50).
Conclusion
Narrow window (< 15 mm) access biopsy and fiducial placement with blunt needle approach under CT guidance is safe and successful.
Clinical relevance statement
CT-guided biopsy and fiducial placement can be performed through narrow window access of less than 15 mm utilizing the blunt-tip technique.
Key Points
• A narrow window for CT-guided abdominal and pelvic biopsies and fiducial placements was considered when width of the needle path between vital structures was ≤ 15 mm.
• Seventy-three biopsies and fiducial placements performed through a narrow window with blunt needle approach had a similar rate of technical and clinical success and complications compared to 323 procedures performed through a wide window approach, with traditional approach (> 15 mm).
• This study confirmed the safety of the CT-guided percutaneous procedures through < 15 mm window with blunt-tip technique.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Percutaneous image-guided biopsies and drain placement are routinely performed for diagnosis and management of a broad spectrum of pathologies. Due to the high technical success and excellent safety profile, CT-guided biopsies are widely used to obtain pathologic diagnosis [1]. The overall safety profile of these procedures is very good, with rate of major adverse events < 2% [2]. Many factors contribute to the technical success and safety profile of CT-guided biopsies, such as vascularity of the lesion, type and gauge of biopsy needle used, benign or malignant nature of the lesion, and the experience of radiologists and pathologists [2, 3].
The high success rate of percutaneous imaging-guided biopsy may result in increased requests for “difficult” CT-guided biopsies, for example, targeting lesions in close proximity to vital structures or when the lesion location or the surrounding structures is variable depending on patient position, bowel motion, breathing, etc. [4]. These circumstances are challenging as the access window to the lesion is either narrow or movable. Given the implications of declining image-guided procedures, such as either suboptimal conservative treatment or more morbid surgical management, an approach that would allow sampling in the setting of the narrow window is necessary.
The identification of a safe needle trajectory, also known as a safe window, is a cornerstone of percutaneous intervention. Different techniques have been adopted to gain access to these narrow window target lesions, including patient positioning, hydrodissection, and curved and blunt-tip needles [5,6,7,8,9,10,11,12]. In our institution, we use the “blunt-tip” technique, which is used by several interventional teams, but has not been described in the literature. Furthermore, the available data so far does not evaluate the safety of and technical success in the narrow window access biopsies specifically and not explicitly considered in the most recent Society of Interventional Radiology guidelines in regard to percutaneous biopsies [2].
The purpose of this study was to assess the success rate and safety profile of CT-guided procedures performed in patients with narrow window access, with blunt needle approach, compared to the procedures performed with wide window access.
Materials and methods
This is a retrospective HIPAA-compliant study of consecutive patients who underwent CT-guided biopsy or fiducial placement in the abdomen and pelvis at our institution between January 2015 and December 2018. The institutional review board approved the study with a waiver for informed consent. Written informed consent was obtained prior to all CT-guided procedures per the institutional protocol. Our institution is a teaching hospital where trainees actively participate in the procedures. In our institution, we have availability and substantial expertise in both CT-guided and US-guided percutaneous procedures. For each biopsy request from a referring physician, an interventional radiologist thoroughly reviews the case using imaging and clinical information. Based on this evaluation, the interventional radiologist decides whether to proceed with CT or US guidance, and the patient is then scheduled accordingly.
Study patients
In this retrospective study, 410 consecutive abdominal and pelvic CT-guided procedures performed between January 2015 and December 2018, including core needle biopsy (CNB) and fiducial placement, were identified through the institutional database. Fourteen procedures were excluded from the study due to the absence of available images (5 cases), no pathology report available for evaluation of clinical outcomes (8 cases), and trans-organ approach (1 case) (Fig. 1). Since 2018, the procedure technique for narrow window has not changed, with new staff being trained to follow blunt needle technique for narrow window cases.
Procedure technique
CT-guided procedures were performed under intermittent CT fluoroscopy guidance (AS Definition 32 detector (64 slice), Siemens). Procedures were performed with moderate sedation (intravenous midazolam and fentanyl), administered by registered radiology nursing staff who continuously monitored the cardiac and respiratory status of the patient per institutional protocol. Patients were screened for coagulopathy, and appropriate corrections were made, including cessation of anti-coagulation as feasible as per Society of Intervention Radiology (SIR) guidelines [2]. Procedures were performed by radiology residents or abdominal imaging fellows under the direct supervision of experienced board-certified interventional or abdominal radiologists.
The attending radiologist decided on appropriate patient positioning based on the available prior cross-sectional imaging to ensure the safest approach to the target to increase the access window as feasible by utilizing a variety of decubitus approaches. The patient then underwent a non-contrast CT scan of the target area. Intravenous contrast was administered at the discretion of the attending radiologist for better visualization of the lesion, vascular structures, and ureters. The biopsies were performed using a 17G coaxial /18G biopsy system (Mission, Bard). Similarly, for fiducial placement alone, an 18G sharply beveled needle with wax at the tip (Brachystar needle, Bard) was placed through the 17G coaxial needle.
The target for a core needle biopsy (CNB) or fiducial placement was localized, and the optimal window, defined as the shortest tract between the skin and the target lesion with the minimum number of vital structures in between, was chosen.
Although a formal protocol to approach cases with narrow access window is not formalized in our institution, the blunt needle approach is usually preferred due to the protection against penetration of visceral structures and vessels. The encapsulated structures, fascia, and bowel require either a significant force or a sharp needle to penetrate. In contrast, within the fat, the blunt needle can glide by different structures, in our experience. Therefore, by consensus, a blunt needle is used to navigate the fat-containing narrow window component of the tract after the sharp needle (stylet) penetrates the skin, subcutaneous tissues, muscle, and parietal peritoneum. The procedure sequence is as follows: after traversing the fascia, the sharp stylet is replaced by the blunt-tip stylet to advance through the narrow window. The blunt needle is used to navigate within the peritoneum to avoid damage to intraperitoneal organs, such as small vessels. Next, when the needle is at the target, a sharp needle is used to advance the system into the target organ for obtaining biopsies or placing fiducials.
A limited unenhanced CT scan was performed after the biopsy or fiducial placement to screen for post-procedure complications. A radiology nurse monitored patients to detect signs and symptoms of post-procedural complications and sedation recovery. The length of post-procedure observation time varied from 1 h in cases for sedation recovery only to up to 4 h in visceral biopsy and fiducial placement cases per departmental protocol. In case of a procedure at increased risk for complication, the monitoring period is extended at the discretion of the interventional radiologist.
Procedure review
Procedure images were reviewed on PACS by an abdominal imaging fellow (ACh). Within the needle trajectory, the window width was defined as the minimum distance between the vital structures, such as visceral organs, bowel loops, vessels, ureters, and bones along the path of the needle, as measured in three-dimensional planes (Figs. 2 and 3). A consensus among the radiologists performing procedures in our department deemed 15 mm window width a safe threshold to perform CNB with the standard technique. Procedures were classified according to the smallest window width between nearby structures along the needle path into “narrow window” (≤ 15 mm [sub-categorized as < 5 mm, 5–10 mm, 11–15 mm]) and “wide window” (> 15 mm). Depth was defined as the distance between the skin to the tip of the coaxial/core needle within the target organ (Figs. 2, 3, and 4). The closest structures to the needle path, such as visceral organs, bowel loops, major vessels (including aorta, iliac, celiac, and superior mesenteric arteries, vena cava, portal, hepatic, and mesenteric veins), small vessels (including mesenteric branches, inferior epigastric), ureters, and bones, were considered adjacent to the trajectory. The time needed to perform the biopsy, from the preprocedural scan to the last sampling, was reported.
Example of wide window approach. Seventy-year-old man with history of chronic lymphocytic leukemia presents with CT diagnosis of abdominal mass concerning for malignancy (a). A CT-guided biopsy was ordered. b The intraprocedural images show coaxial needle in correct position at the edge of the lesion. The window width in this patient (yellow line) was measured 45 mm and the depth was 89 mm (blue line). This was classified as wide window
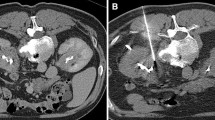
Example of narrow window approach. A 43-year-old woman underwent CT for suspected chronic lymphocytic leukemia or lymphoma. a The images reveal the presence of a celiac lymphadenopathy that is targeted for biopsy (arrow). b The intraprocedural images show coaxial needle in correct position at the edge of the lesion. The window width in this patient was measured 0 mm and the depth was 82 mm. This was classified as narrow window. During the procedure, a small amount of intraperitoneal free air was noted, likely an expected consequence of the removal of the sharp stylet followed by the introduction of the blunt stylet
Example of narrow window approach. A 63-year-old man with history of distal pancreatectomy for pancreatic adenocarcinoma underwent abdominal MRI for follow-up a, with evidence of a retrocrural lymphadenopathy (arrow). A biopsy was requested. b Intraprocedural CT images show coaxial needle at the edge of the target lesion. The pathology result showed “Lymph node tissue with no carcinoma seen.” The window width in this patient was measured 4 mm and the depth was 96 mm. This was classified as narrow window
Complications
Incidence of immediate and delayed (30 days) complications was obtained through a review of the patient’s radiology studies, radiology reports, and medical records by an abdominal research fellow. The complications were classified as major, requiring inpatient treatment, or minor, self-resolving, according to the Society of Intervention Radiology (SIR) guidelines [2].
Outcomes
Technical success was defined as obtaining adequate tissue samples from the target during the biopsy or adequate position of fiducials on post-procedural imaging. For CNB and CNB followed by fiducial placement, clinical success was defined by concordant pathology results with imaging findings as deemed by the group consensus review by procedural radiologists during routine clinical weekly radiology-pathology correlation meetings.
In addition, the results of the biopsy, with or without fiducial placement, were compared to the reference standard (surgical pathology or imaging follow-up, minimum of 6 months), to calculate sensitivity, specificity, and accuracy. True positive results were defined as malignant result confirmed on surgery or radiological or clinical follow-up, true negative as non-malignant pathology result confirmed on surgical sample or imaging follow-up, and false negative as non-malignant result that was proved malignant on surgery or imaging follow-up.
Statistical analysis
Descriptive statistics were provided. The chi-square test and the Yates’ chi-square test were used to analyze the difference in prevalence between the two groups. The Kruskal-Wallis test was used to assess differences in the window width and depth medians. The level of statistical significance was set at p < 0.05.
Results
The study cohort included 396 CT-guided procedures in 378 patients, with 183 (48%) women and mean age of 62.9 years (SD 13.6, range 21–92 years) (Table 1). There were 350/396 CNB (88.4%), 14/396 CNB followed by fiducial placement (3.5%), and 32/396 fiducial placement only (8.1%). A total of 323/396 (81.5%) CT-guided procedures were performed with wide window (> 15 mm) and 73/396 (18.5%) with narrow window with blunt-tip needle, including equal or less than 5 mm width (17/73, 23%), width 6–10 mm (22/73, 30%), and width of 11–15 mm (34/73, 47%). None of the cases with narrow window access were performed with hydrodissection technique. Median depth for narrow window was greater (97 mm, IQR 82–113 mm, 95% CI 91–104 mm) compared to wide window group (84 mm, IQR 60–106 mm, 95% CI 80–88 mm); p = 0.002.
Bowel was the most common organ adjacent to the needle path in both narrow and wide window groups (44/73, 60% and 218/323, 68%, respectively) (Table 3). In the narrow window group, major and small vessels were noted adjacent to the needle path in 31/73, 43% and in 30/73 41% cases, respectively, compared to only 53/323, 16% and 59/323, 18% for the wide window group; p < 0.0001.
The median time to perform the procedure was 30 min (interquartile range 23–40 min), without difference between procedures with narrow (median 29, IQR 21–38 min) and wide (median 30, IQR 23–40 min) window; p = 0.23.
Complications
No major complications were noted in the whole study cohort. There was one minor immediate complication (1.3%; 1/73) in the narrow window group, seen in a patient undergoing pancreatic biopsy complicated by post-procedural hematoma for which the patient required hospitalization for observation (Fig. 5). Four minor immediate complications (1.2%; 4/323) were noted in the wide window group (4 small post-procedural hematomas); p = 0.73. No interventions or treatments were required for the management of these complications. In the wide window group, one patient presented to the emergency department within 30 days after the procedure for minor complications (1/323, 0.6%). The patient, who suffered from peritoneal carcinomatosis, ascites, and ovarian mass, presented to ED with leakage of serous fluid from the site of ovarian mass biopsy. This was treated conservatively with no hospitalization or intervention. In the narrow window group, one patient presented to the emergency department within 30 days after the procedure for minor complications (1/73, 1.3%); p = 0.50. The patient, who suffered from retroperitoneal fibrosis targeted for biopsy, presented with flank pain secondary to retroperitoneal hematoma that was treated conservatively without the need for hospitalization or intervention (Fig. 6).
Narrow window approach with immediate complication. Sixty-seven-year-old man with a history of diffuse B-cell and pancreatic cysts present with clustered cystic lesions in the head of the pancreas, with diameter of 2.9 × 1.8 × 3.6 cm seen on MRCP (a). b Percutaneous CT-guided sampling was performed, with narrow window between mesenteric vessels. c During the procedure, there was evidence of bleeding. A CTA was performed without evidence of active extravasation. Patient was hemodynamically stable and was admitted overnight to monitor clinical condition
Narrow window approach with delayed complication. An 82-year-old woman presented to the ED with abdominal pain and fever. a An abdominal CT ordered for suspected diverticulitis revealed the presence of retroperitoneal lymphadenopathy. b A CT-guided percutaneous biopsy was ordered. The intraprocedural images showed narrow window, with needle trajectory between the inferior vena cava and the aorta. c After 2 days, the patient presented to the ED with fever and abdominal pain. A CT scan showed presence of small amount of retroperitoneal hematoma. After monitoring for 24 h, the fever did not recur and the patient was discharged without treatment
Outcomes
Technical success was achieved in 100% (73/73) of the cases in the narrow window group and 99.7% (322/323) in the wide window group.
After the exclusion of 33 fiducial placement procedures and 1 technically unsuccessful CNB, 89.5% (322/362) of CNBs were deemed clinically successful. There was no difference in the clinical success rate between the “narrow window” group (86.4%; 57/66) and the ‘'wide window” group (89.5%; 265/296); p = 0.46.
For the comparison with the reference standard, 12 biopsies (2 with narrow window and 10 with wide window) were excluded due to insufficient follow-up. There was a sensitivity of 88% for the narrow window approach (51/58) and 92% for the wide window approach (227/248). For both groups, the specificity was 100%. The overall accuracy was 89% for the narrow window (57/64) and 93% for the wide window (265/286) (Table 2).
Discussion
Image-guided percutaneous procedures are generally safe and highly successful. However, a narrow window between vital organs along the biopsy access is perceived as a significant safety challenge. Hydrodissection is one method suggested to avoid vital structures along the needle path; however, its utilization may be limited by difficulty maintaining fluid within a specified space for the duration of the biopsy, and therefore additional alternative solutions are needed [13,14,15,16,17]. In our institution, we routinely adopt a technique which includes blunt-tip stylet through a coaxial needle system to navigate areas with narrow access window and avoid sharp trauma to other structures. This retrospective analysis of our patient population showed that performing CT-guided biopsy through a narrow access window (< 15 mm) is as safe as through a wide window access with similar technical and clinical success (Table 3).
The blunt-tip technique was first introduced in radiological literature by Akins and Hawkins in 1989 when they examined the safety of the blunt-tip needle (made by filing down the sharp inner stylet of the standard 18G Cook needle) in an open evaluation in dogs, followed by use in patients (predominantly nephrostomies and biliary drainages with 12 abscess drainages and 2 biopsies) [10]. The authors have shown that the “blunt tip displaced loops of bowel without laceration or entry into the intestines.” Furthermore, the “blunt tip needle … bounced off kidney capsule when the pass was not perpendicular to the kidney” and “parenchymal entry … required jabbing action at the capsule.” Lastly, “blunt needle … could not be forced to penetrate barium filled renal artery despite at least 100 direct forceful attempts.” This served as the basis for the commercial development of the Hawkins (Argon Medical devices) and Hawkins-Akins (Cook Medical) blunt needles [18, 19]. The authors also safely used a blunt-tip needle for 12 percutaneous abscess drainages when vascular structures or bowel were present in the procedural trajectory under fluoroscopy. In 2009, the blunt-tip needle was used for 30 lymph node biopsies under CT guidance with 100% technical success with 3/30 (10%) minor complications, one case of hematoma and two cases of pneumothoraces in mediastinal biopsies [9]. More recently, a blunt-tip needle was used for 26 CT-guided biopsies and 9 abscess drainages in cases with less than 10 mm from a critical structure. In the biopsy group, there were 19% of minor complications (4 pneumothoraces and one hematoma) [11]. Though this limited available evidence points to the likely safety of the blunt-tip technique, all three studies include only a small number of patients and none of these three small series compare the accuracy and safety of the technique in the narrow window compared to wide window access procedures. In the current study, we report the safety and accuracy of 73 procedures performed with window less than 15 mm and we compare the results to the wide window access group.
There were no major complications in our study cohort, and the minor complication rate was 1.8%, which is slightly lower than the reported complication rates in the literature [20, 21]. Furthermore, the complication rates from CT-guided biopsies and fiducial placement through a narrow window approach were similar to the wide window approach (1.3% compared to 1.9%). Previous studies showed the utility of the hydrodissection technique to displace vital organs located along the trajectory to the target lesion [22, 23]. However, these studies did not specifically evaluate the approach to a target lesion with a narrow window access.
Alternative methods to approach narrow window access biopsies have been proposed. One of the techniques is hydrodissection, which is employed routinely for ablation procedures [13, 14, 16]. One known downside of this technique is poor control of the liquid instilled as it tends to collect in dependent spaces, which is not necessarily the site needed for the biopsy trajectory [15, 22]. Curved needles with specific pre-shaped angles have been used to approach difficult biopsies [24,25,26]. Using a curved needle does not allow modifications of the trajectory during the procedure and at times it may be difficult to predict the exact course the needle will take through the tissues. The utility of curved needles has not been confirmed in independent studies yet. As a steep learning curve, decreased ability to modify the needle trajectory and increased procedure time could represent significant obstacles to wide clinical applicability [24].
Our study has several limitations. First, patient selection is influenced by the available resources and the interventional radiologists’ preference to refer a patient to either a US-guided or CT-guided biopsy. This limitation is somehow mitigated by the fact that we have significant experience and availability in both US- and CT-guided procedures. Given the study’s retrospective nature, we could not determine with certainty if there were procedures where the blunt-tip technique was not used for accessing the narrow window. While there is no formal protocol to use the blunt-tip technique, this technique is almost universally utilized by our interventional radiologists while traversing a narrow window as per typical institution practice and consensus. The cutoff of 1.5 cm is arbitrary and depends on the clinical indication and type of critical structure along the trajectory of the needle. Nevertheless, 1.5 cm or greater is a reasonable window for performing CT-guided procedures with a standard sharp needle for our interventional radiologists. While an ideal study would present a randomized comparison between the “blunt” and “sharp” approaches, it is challenging to randomize this choice while simultaneously guaranteeing patient safety and maintaining the radiologist’s confidence throughout all procedures. Our institution has a fellowship training program that might impact the technical and success rate based on the experience of the fellow and the level of training. However, technical and clinical success in the current study was very high and comparable to the literature. This may also be related to the experience of the attending radiologists who supervise the fellow or trainee through all aspects of the procedure and can take over completely in difficult cases to ensure technical success and patient safety. While we accurately maintain immediate and 30-day complication rates for our patients undergoing CT-guided procedures, there is a possibility that some of these patients are referred to outside clinics for follow-up of any delayed complications.
Our study shows a high success rate and safety profile of CT-guided procedures with narrow window access. The use of blunt-tip needle technique and the experience of the interventional radiologists likely contribute to these results.
Abbreviations
- CNB:
-
Core needle biopsy
- ED:
-
Emergency department
- IQR:
-
Interquartile range
- SIR:
-
Society of Intervention Radiology
References
Gupta S, Madoff DC (2007) Image-guided percutaneous needle biopsy in cancer diagnosis and staging. Tech Vasc Interv Radiol. https://doi.org/10.1053/j.tvir.2007.09.005
Sheth RA, Baerlocher MO, Connolly BL et al (2020) Society of interventional radiology quality improvement standards on percutaneous needle biopsy in adult and pediatric patients. J Vasc Interv Radiol. https://doi.org/10.1016/j.jvir.2020.07.012
Appelbaum L, Kane RA, Kruskal JB, Romero J, Sosna J. (2009) Focal hepatic lesions: US-guided biopsy—lessons from review of cytologic and pathologic examination results. Radiology. https://doi.org/10.1148/radiol.2502080182
Frederick-Dyer K, Ahmad A, Arora SS, Wile G (2016) Difficult biopsy and drainage: just say yes. Abdom Radiol (NY). https://doi.org/10.1007/s00261-016-0666-2
vanSonnenberg E, Wittenberg J, Ferrucci JT, Mueller PR, Simeone JF (1981) Triangulation method for percutaneous needle guidance: the angled approach to upper abdominal masses. AJR Am J Roentgenol. https://doi.org/10.2214/ajr.137.4.757
Langen HJ, Klose KC, Keulers P, Adam G, Jochims M, Günther RW (1995) Artificial widening of the mediastinum to gain access for extrapleural biopsy: clinical results. Radiology. https://doi.org/10.1148/radiology.196.3.7644632
De Filippo M, Saba L, Rossi E et al (2015) Curved needles in CT-guided fine needle biopsies of abdominal and retroperitoneal small lesions. Cardiovasc Intervent Radiol. https://doi.org/10.1007/s00270-015-1107-2
Garnon J, Cazzato RL, Ramamurthy N et al (2016) Curved needles: beyond diagnostic procedures. Cardiovasc Intervent Radiol. https://doi.org/10.1007/s00270-016-1397-z
de Bazelaire C, Farges C, Mathieu O et al (2009) Blunt-tip coaxial introducer: a revisited tool for difficult CT-guided biopsy in the chest and abdomen. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.08.2125
Akins EW, Hawkins IF, Mladinich C, Tupler R, Siragusa RJ, Pry R (1989) The blunt needle: a new percutaneous access device. AJR Am J Roentgenol. https://doi.org/10.2214/ajr.152.1.181
Cazzato RL, Garnon J, Shaygi B et al (2017) Performance of a new blunt-tip coaxial needle for percutaneous biopsy and drainage of “hard-to-reach” targets. Cardiovasc Intervent Radiol. https://doi.org/10.1007/s00270-017-1663-8
de Oliveira Schiavon LH, Tyng CJ, Travesso DJ, Dias Rocha R, Schiavon ACSA, Bitencourt AGV (2018) Computed tomography-guided percutaneous biopsy of abdominal lesions: indications, techniques, results, and complications. Radiol Bras. https://doi.org/10.1590/0100-3984.2017.0045
Teng D, Dong C, Sun D, Liu Z, Wang H (2021) Comparison of ultrasound-guided core needle biopsy under the assistance of hydrodissection with fine needle aspiration in the diagnosis of high-risk cervical lymph nodes: a randomized controlled trial. Front Oncol. https://doi.org/10.3389/fonc.2021.799956
Ebrahiminik H, Chegeni H, Jalili J et al (2021) Hydrodissection: a novel approach for safe core needle biopsy of small high-risk subcapsular thyroid nodules. Cardiovasc Intervent Radiol. 44(10):1651–1656. https://doi.org/10.1007/s00270-021-02838-w
Dantas GC, Travesso DJ, Amoedo MK, Barbosa PNV, Tyng CJ (2020) Modified hydrodissection for percutaneuous biopsy of small lesions: the “marshmallow” technique. Diagn Interv Radiol. https://doi.org/10.5152/dir.2019.19270
Khan F, Ho AM, Jamal JE, Gershbaum MD, Katz AE, Hoffmann JC (2018) Long-term outcomes after percutaneous renal cryoablation performed with adjunctive techniques. Clin Imaging. https://doi.org/10.1016/j.clinimag.2017.12.003
Tyng CJ, Almeida MFA, Barbosa PNV et al (2015) Computed tomography-guided percutaneous core needle biopsy in pancreatic tumor diagnosis. World J Gastroenterol. https://doi.org/10.3748/wjg.v21.i12.3579
HawkinsTM Blunt Needle Access System. https://www.argonmedical.com/. Accessed November 25, 2022
Hawkins-Akins Blunt Needle | Cook Medical. . https://www.cookmedical.com/products/ir_dwoppn_webds/. Accessed November 25, 2022
Heerink WJ, de Bock GH, de Jonge GJ, Groen HJM, Vliegenthart R, Oudkerk M (2017) Complication rates of CT-guided transthoracic lung biopsy: meta-analysis. Eur Radiol. https://doi.org/10.1007/s00330-016-4357-8
Midia M, Odedra D, Shuster A, Midia R, Muir J (2019) Predictors of bleeding complications following percutaneous image-guided liver biopsy: a scoping review. Diagn Interv Radiol. https://doi.org/10.5152/dir.2018.17525
Asvadi NH, Arellano RS (2015) Hydrodissection-assisted image-guided percutaneous biopsy of abdominal and pelvic lesions: experience with seven patients. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.14.13040
Cheng Z, Liang P (2019) US-guided core needle biopsy under assistance of hydrodissection to diagnose small lymph node metastases adjacent to cervical large vessels. Diagn Intervent Radiol. https://doi.org/10.5152/dir.2019.18166
Schulze-Hagen MF, Pfeffer J, Zimmermann M et al (2017) Development and evaluation of a novel curved biopsy device for CT-guided biopsy of lesions unreachable using standard straight needle trajectories. Cardiovasc Intervent Radiol. https://doi.org/10.1007/s00270-017-1597-1
Singh AK, Leeman J, Shankar S, Ferrucci JT (2008) Core biopsy with curved needle technique. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.08.1165
Gupta S, Ahrar K, Morello FA, Wallace MJ, Madoff DC, Hicks ME (2002) Using a coaxial technique with a curved inner needle for CT-guided fine-needle aspiration biopsy. AJR Am J Roentgenol. https://doi.org/10.2214/ajr.179.1.1790109
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Olga R. Brook.
Conflict of interest
F. Rigiroli received funding as a research fellowship from Bracco Diagnostics (not related to the present article). The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors, Alexander Brook, has significant statistical expertise.
Informed Consent
Written informed consent was waived by the Institutional Review Board of Beth Israel Deaconess Medical Center.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
None
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rigiroli, F., Camacho, A., Chung, A. et al. Safety profile and technical success of narrow window CT-guided percutaneous biopsy with blunt needle approach in the abdomen and pelvis. Eur Radiol 34, 2364–2373 (2024). https://doi.org/10.1007/s00330-023-10231-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10231-z