Abstract
Objectives
We aim to investigate associations between different coil strategies and outcomes in the aneurysms treated by a pipeline embolization device (PED).
Methods
Patients with medium-to-giant-sized aneurysms treated by PED were included. The total cohort was divided into PED-alone and PED-coiling groups, and the PED-coiling group was further divided into loose and dense packing subgroups. Multivariate logistic analyses and stabilized inverse probability of treatment weighting (sIPTW) were performed to investigate the relationships between coiling strategies and outcomes. Restricted cubic spline (RCS) curves were used to describe the coiling degree and angiographic outcome relationship.
Results
A total of 398 patients with 410 aneurysms were included. Aneurysms treated with PED coiling had a lower incomplete occlusion rate (15.3% vs. 30.3%, p = 0.002), higher total perioperative complication rate (14.2% vs. 3.5%, p = 0.001), longer production time (142.14 min vs. 101.26 min, p < 0.001), and higher total cost ($45,158.63 vs. $34,680.91, p < 0.001) than those treated with PED alone. There were no differences in outcomes between the loose and dense packing subgroups. However, the total cost was higher in the dense packing group ($43,787.46 vs. $47,288.32, p = 0.001) than in the loose packing group. The result was still robust in the multivariate and sIPTW analyses. The RCS curves showed “L-shape” relationships between the coil degree and angiographic outcomes.
Conclusion
Compared with PED alone, PED coiling could improve aneurysm occlusion. However, it could also increase the total complication risk, prolong procedure time, and increase the total cost. Compared with loose packing, dense packing did not enhance the treatment effectiveness but increased the treatment cost.
Clinical relevance statement
The additional treatment effect from coiling embolization declines sharply after a certain point. Specifically, the aneurysm occlusion rate is roughly stable when the coil number is greater than 3 or the total coil length is longer than 150 cm.
Key Points
• Compared with pipeline embolization device (PED) alone, PED combined with coiling can improve aneurysm occlusion.
• Compared with PED alone, PED combined with coiling increases the total complication risk, cost, and prolongs procedure time.
• Compared with loose packing, dense packing did not increase the treatment effectiveness but increased the cost.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Flow diversion devices, such as the pipeline embolization device (PED; Covidien), have gained acceptance in the treatment of intracranial aneurysms (IAs) because of the higher occlusion rate without additional mortality and morbidity compared to traditional coiling embolization [1,2,3]. Although the PED was designed as a novel independent treatment modality for IA, many operators still use coils during PED placement. Compared with PED alone, an adjunction with coiling could provide immediate dome protection and may decrease the risk of device prolapse [4]. Recent studies have also reported a high occlusion rate and low need for retreatment in aneurysms treated with PED-assisted coiling [5,6,7,8,9,10]. Despite the benefits of coiling combined with PED, several studies have reported increasing morbidity from complications associated with this treatment. For example, the IntrePED and PLUS studies reported that PED with coiling could prolong the procedure time and result in higher neurological or ischemic stroke morbidity [5, 11]. Moreover, adjunctive coiling may not be cost-effective. Thus, the use of coils may still be a double-edged sword.
Considering the differences in PED and coil embolization mechanisms, the relationship between PED and coil embolization should be one of cooperation rather than competition. Coil embolization used in the PED treatment could be divided into loose and dense packing. Although several studies suggest the loose packing of coils during PED placement [6, 9, 12], few have evaluated the difference between loose and dense packing to support this hypothesis. In patients treated with PED assisted with coiling, an association between coiling degree and angiographic outcome, clinical outcome, complication, and cost remains unclear. Therefore, this study aimed to investigate the association between different coil embolization strategies and patient/aneurysm outcomes in medium-to-giant-sized aneurysms. We used stabilized inverse probability of treatment weighting (sIPTW) analysis by balancing differences in baseline characteristics, mimicking a randomized controlled trial. In addition, we used restricted cubic spline (RCS) curves to describe the nonlinear relationship between the coiling degree and angiographic outcome to research the effect of different coiling applications utilized in the clinical setting.
Materials and methods
Study population
The Beijing Tiantan Hospital institutional research ethics boards approved this study; however, informed consent was not required because of the study’s retrospective nature. This retrospective study was conducted at Beijing Tiantan Hospital. All aneurysms treated with PED between January 1, 2015, and December 31, 2020, were reviewed. The exclusion criteria were as follows: (1) aneurysms treated with multiple stents (including PED or other stents), (2) patients with arteriovenous malformations and fistulas, (3) aneurysms with evidence of parent artery occlusion at final follow-up, (4) ruptured aneurysms, and (5) aneurysm size (defined as the maximum diameter of any two points on the aneurysm) ≤ 7 mm.
We collected information on the patients’ characteristics, including the modified Rankin Scale (mRS; range, 0 to 6, where a score of 0 indicates no disability, 1 indicates no clinically significant disability, 2 indicates slight disability, 3 indicates moderate disability but with an ability to walk unassisted, 4 indicates moderately severe disability, 5 indicates severe disability, and 6 indicates death) in addition to age, sex, comorbidities, cigarette smoking history, and alcohol consumption. Two authors measured aneurysm characteristics, including location, size, neck (maximum diameter of any two points on the neck section), and parent artery diameter (mean diameter of the artery at the proximal and distal ends of the aneurysms). Two neurosurgeons with more than 15 years of experience supervised these measurements. Aneurysm size was categorized into three groups as follows: medium (> 7 mm and ≤ 15 mm), large (> 15 mm and ≤ 25 mm), and giant (> 25 mm). Treatment details were collected from the medical records, including the PED diameter, PED length, coil numbers, total coil length, and balloon application. Each case’s procedure time and total cost (converted to US dollars at the 2021 average exchange rate) were also collected. The total cost was calculated as the sum of all types of costs incurred during hospitalization, including surgery treatment, complication treatment (if needed), and other expenses incurred during hospitalization.
The supporting data of this study are available from the corresponding author upon reasonable request.
Procedural details
All procedures were performed under dual antiplatelet therapy (100 mg/d aspirin and 75 mg/d clopidogrel) at least 3–5 days before, and general anesthesia was administered to all patients during the procedure. During the procedure, patients received heparin as a bolus (3000 IU) followed by an infusion (1000 IU per h). After the procedure, clopidogrel (75 mg/d) and aspirin (100 mg/d) were continued for 8–12 weeks and at least 6 months, respectively. Standard light transmittance aggregometry was used to measure platelet aggregation and evaluate platelet function (AG800; Techlink Biomedical, Inc.). Patients identified as clopidogrel nonresponders were recommended aspirin (100 mg/d) and ticagrelor (90 mg twice daily). A suitable working projection was performed according to three-dimensional rotational angiography. Adjunct coiling was used for large aneurysms or those with a high risk of rupture (such as irregularly shaped aneurysms or those in patients with a history of sentinel headache). Generally, based on the size of the aneurysm, the first coil is as large as possible. Then, the latter coils are selected according to the previous coil’s packing effect; the subsequent coil size gradually decreases. A panel of neuro-interventionalists with more than 15 years of aneurysm treatment experience determined the number and size of coils. When encountering severe poor wall apposition, we usually corrected it using balloon angioplasty.
Study exposures and outcomes
The coiling use and coiling degree were set as the primary exposures. Raymond–Roy’s class score was used to assess the degree of coiling immediately following the procedure. We defined Raymond–Roy class III as loose packing and Raymond–Roy class I/II as dense packing [13]. The coil number and total coil length also represented the degree of coiling.
The study’s set outcomes were angiographic follow-up, clinical follow-up, perioperative complications, procedure time, and total cost. The occlusion rate was determined during the angiographic follow-up. For aneurysms treated with PED assisted with coiling, we defined Raymond–Roy class I as complete occlusion and Raymond–Roy class II/III as incomplete occlusion [13]. According to the Byrne grading scale, grade 4 was defined as complete occlusion for aneurysms treated with PED alone, and grades 0–3 were defined as incomplete occlusion [14]. The first angiographic assessments were performed 3–6 months after PED placement, and later angiographic follow-ups were performed at 6 or 12 months. Treatment failure was defined as incomplete occlusion following at least 24 months of observation. An independent panel of neurosurgeons and radiologists analyzed all angiographic imaging. The clinical follow-up was represented by the mRS score; scores of 0–2 were considered a good outcome and 3–5, a poor outcome.
We also collected information on intraoperative hemorrhagic complications, intraoperative thrombosis, postoperative subarachnoid hemorrhage (SAH), postoperative hemorrhage, major postoperative stroke (a change in the National Institutes of Health Stroke Scale score of > 4 lasting > 7 days), minor postoperative stroke (a change in score of ≤ 4 lasting < 7 days or a transient neurological deficit with or without corroborative imaging), transient ischemic attack (a transient neurological deficit without corroborative imaging), and mortality. Considering the relatively low rates of each complication, we defined the major complications as the overall rates of intraoperative hemorrhage, intraoperative thrombosis, postoperative SAH, postoperative hemorrhage, major postoperative stroke, and mortality. Likewise, we defined total complications as the overall rate of all complications. We did not double-count cases with multiple complications (i.e., we only recorded them once).
Statistical analysis
Continuous variables are expressed as means ± standard deviations and were tested using a t-test or Wilcoxon rank sum test. Categoric variables are expressed as the number of events and percentage and were analyzed using χ2 or Fisher’s exact test. Multivariate logistic regression analyses were performed to identify whether the exposures were independent predictors of study outcomes. All variables with a p value < 0.20 in the univariate analysis were enrolled in the multivariate logistic regression models as confounders. The associations between the extent of coiling and occlusion rate were evaluated on a continuous scale with RCS curves based on the same multivariate logistic regression model with three knots at the 10th, 50th, and 90th percentiles of coil numbers and total coil length. The sIPTW estimated the sensitivity analysis. Weights were calculated based on the propensity score, which considered patient age, sex, aneurysm location, size, neck, type, and parent artery diameter. p-values < 0.05 were considered statistically significant. R software (R Foundation for Statistical Computing) was used for all calculations.
Results
Baseline characteristics
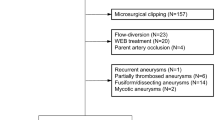
A total of 798 patients with 904 aneurysms were reviewed. We excluded 39 aneurysms treated with multiple stents, 15 aneurysms combining with arteriovenous malformations or fistulas, 19 aneurysms with parent artery occlusion at the follow-up, 27 ruptured aneurysms, and 394 aneurysms with a size of ≤ 7 mm. Thus, our final analysis included 398 patients with 410 aneurysms (Supplement Fig. 1). In the total cohort, 170 (41.5%) aneurysms were treated with PED alone, and 240 (58.5%) aneurysms were treated with PED coiling. Most of the patients were women (68.5%), and the mean age of patients was 54.63 ± 11.21 years, while 125.33 ± 55.83 min was the mean procedure time. The mean total cost was $40,814.21 ± $8802.77. The total treatment cost was higher in patients with complications than in those without complications ($45,396.24 ± $10,665.73 vs. $40,332.54 ± $8457.40, p = 0.001). Aneurysms treated with PED coiling were more likely to be located at the internal carotid artery (ICA; 88.3% vs. 52.9%, p < 0.001), be saccular type (95.0% vs. 69.4%, p < 0.001), and be larger (16.61 ± 7.13 mm vs. 11.79 ± 5.34 mm, p < 0.001) than the aneurysms treated with PED alone. In the PED-coiling group, most aneurysms (60.8%) were loosely packed. The location and type of aneurysm were similar between the loose and dense packing groups. However, the size of aneurysms in the loose packing group was larger than those in the dense packing group (17.92 ± 7.25 mm vs. 14.58 ± 6.47 mm, p < 0.001). Details of the differences among groups with different degrees of coiling are given in Table 1.
Association between coiling and study outcomes
The mean coiling number in the total PED-coiling group was 4.86 ± 3.15, and the mean total coil length was 162.28 ± 129.33 cm. There was no statistical significance between the PED-coiling and PED-alone groups for the poor clinical outcome in either univariate (5.3% vs. 3.1%, p = 0.414; Table 1) or multivariate analysis (odds ratio [OR]: 1.96, 95% confidence interval [CI]: 0.42–10.1, p = 0.401; Table 2). Aneurysms treated with PED coiling had a significantly lower incomplete occlusion rate (15.3% vs. 30.3%, p = 0.002) and significantly higher total perioperative complications (14.2% vs. 3.5%, p = 0.001) than the aneurysms treated with PED alone. After adjusting for confounders, these trends were still significant, with an OR of 0.28 (95% CI: 0.14–0.56, p < 0.001) for incomplete occlusion and an OR of 4.54 (95% CI: 1.67–15.00, p = 0.006) for total perioperative complications. In the analysis of major perioperative complications, although the rate was slightly higher in the PED-coiling group, the difference was not statistically significant in either univariate (5.0% vs. 1.8%, p = 0.146) or multivariate analysis (OR: 2.72, 95% CI: 0.61–19.7, p = 0.307). After sIPTW, the results remained robust (Table 3). Details of baseline information on the PED-alone and PED-coiling groups after sIPTW are shown in Supplementary Table 1. In addition, the procedure time (137.55 ± 55.06 min vs. 107.93 ± 40.66 min, p < 0.001) and total cost ($43,614.16 ± $8141.77 vs. $35,118.07 ± $5006.45, p < 0.001) were significantly higher in aneurysms treated with PED coiling (Fig. 1).
Association between coiling degree and study outcomes
The mean coiling number (4.01 ± 2.29 vs. 6.22 ± 3.80, p < 0.001) and total coil length (143.23 ± 102.66 cm vs. 192.97 ± 159.32 cm, p = 0.004) were smaller in the loose packing group than in the dense packing group (Table 1). However, there were no differences identified in the incomplete occlusion rate (18.3% vs. 10.7%, p = 0.224), poor clinical outcome (5.1% vs. 5.7%, p > 0.999), and total (12.3% vs. 17.0%, p = 0.408) or major (4.8% vs. 5.3%, p > 0.999) perioperative complications between the loose and dense packing groups (Table 1). Similar results were also found in the multivariate (Table 2) and sIPTW (Table 3) analyses. After sIPTW, although no difference was found in procedure time (136.76 ± 53.93 min vs. 152.09 ± 67.17 min, p = 0.111); however, the loose packing group had a significantly lower total cost ($43,454.28 ± $6827.66 vs. $48,535.47 ± $9404.29, p < 0.001; than the dense packing group Fig. 1). In the total cohort, we constructed two RCS curves (Fig. 2) to investigate the association between the degree of coiling (coiling number and total coiling length) and aneurysm occlusion rate. After adjusting for hypertension, diabetes, ischemic stroke history, mRS score at admission, aneurysm type, size groups, neck, balloon, PED diameter, PED length, and angiographic follow-up time, the incomplete occlusion risk decreased as the coiling number or the total coiling length increased. When the coiling number was greater than 3 or the total coiling length was larger than 150 cm, the incomplete occlusion risk reached a trough, remaining stable as the coiling number or total coiling length increased (Fig. 2).
Images of a 42-year-old woman with a left internal carotid artery aneurysm treated by a pipeline embolization device combined with loose packing of coils. The size of the aneurysm is 17.3 mm. Four coils, totaling 161 cm, were placed into the aneurysm. Images A and B show the immediate postoperative results and C and D show the last-time follow-up results
Discussion
The primary purpose of this study was to investigate the association between different coil embolization application strategies, complications, and angiographic as well as clinical outcomes. We found that the aneurysm occlusion rates improved when PED insertion was combined with coiling (Fig. 3); however, it also increased total perioperative complication risk, prolonged the procedure time (Fig. 4), and increased the total cost. Compared with loose packing, although the dense packing did not further increase complication risk, poor clinical outcome, and procedure time, it did not enhance the treatment effectiveness but increased the cost of treatment. Additionally, the RCS curves (Fig. 5) showed “L-shaped” relationships between the coil number or total coil length and angiographic outcomes. The occlusion rate began to remain roughly stable when the coil number was greater than 3 or the total coil length was longer than 150 cm; this was used to illustrate that the additional treatment effect from coiling embolization declines sharply after reaching a certain degree of coiling. These results were highly consistent in univariate, multivariate, and sensitivity analyses (sIPTW analysis), enhancing our study’s reliability.
Images of a 66-year-old woman with a left internal carotid artery aneurysm treated by pipeline embolization device combined with dense packing of coils. The size of the aneurysm is 15.8 mm. Six coils, totaling 191 cm, were placed into the aneurysm. Images A and B show the immediate postoperative results and C and D show the last-time follow-up results
Comparison of the total cost (A) and procedure time (B) between different groups. The difference in total cost (dollars) (A) and procedure time (min) (B) between the pipeline embolization device (PED)-alone and PED-coiling groups and between loose and dense packing groups after stabilized inverse probability of treatment weighting
Restricted cubic spline (RCS) curves of coiling number (A) or total coiling length (B) and study outcomes. Solid black lines represent multivariate-adjusted odds ratios (ORs), with gray scales showing 95% confidence intervals derived from RCS regressions with three knots. The dashed lines indicate the reference lines for no association at an OR of 1.0. After adjusting for hypertension, diabetes, ischemic stroke history, modified Rankin Scale score at admission, aneurysm type, size groups, neck, balloon, pipeline embolization device (PED) diameter, PED length, and angiographic follow-up time, the risk of incomplete occlusion decreased as the coiling number (A), or total coiling length (cm) (B) increased; when the coiling number was greater than 3 or total coiling length was larger than 150 cm, the risk of incomplete occlusion reached the lowest and remained stable as the coiling number or total coiling length increased
Compared with PED alone, adjunctive coiling has a series of benefits. First, PED coiling may increase the complete occlusion rate compared with PED alone [5,6,7,8,9]. These findings were in line with our results. Previous hemodynamic studies have reported that adjunctive coiling with flow diversion device placement may significantly reduce intra-aneurysmal flow velocity and wall shear stress on the top of flow diversion placement. Therefore, it promotes thrombosis formation and aneurysm occlusion [15, 16]. Second, assisted coiling usage may decrease the need for multiple PED placements. Previous studies have found that multiple PEDs may further increase the risk of branch occlusion, prolong antiplatelet drug use, and increase thrombotic events [9, 17]. Third, adjunct coiling may reduce the need for aneurysm retreatment, which has limited options such as placement of another PED. Finally, coiling embolization could provide immediate protection from aneurysm rupture. The rate of aneurysm rupture or re-rupture after PED treatment is about 4% [18, 19]. The mechanism of this phenomenon remains unclear. Previous studies have shown that a postoperative aneurysm rupture after PED placement may be associated with acute thrombosis within the aneurysm [20]. Although PED reduces aneurysm inflow, static intra-aneurysmal pressure is unaffected [21, 22]. Coil placement does not affect mean aneurysm pressures but dampens the pressure amplitude during locally induced hypertension [23]. Despite no difference in postoperative SAH rates between the PED-alone and PED-coiling groups in this study, an adjunct coil could theoretically provide immediate dome protection, decreasing the risk of postoperative aneurysm rupture [4, 24].
There are also potential risks with adjunctive coiling in association with PED treatment. First, this study found that total perioperative complications were higher in aneurysms treated with PED coiling. The rate was still slightly higher in the PED-coiling group, though the major perioperative complications were not significantly different. This study is not the first to report this phenomenon. According to an IntrePED Registry study, higher neurological morbidity was associated with PED coiling [11]. Siddiqui et al described a patient with a giant middle cerebral artery aneurysm treated using PED with coiling and identified acute thrombosis after placement of the PED [12]. Second, the procedure time for PED-coiling-treated aneurysms was longer, and this result was also in line with the published literature [11]. Finally, Tan et al found that longer procedure times for PED treatment were associated with higher thromboembolic event risks [17].
Meanwhile, a longer procedure could also confer prolonged surgical anesthesia time and more radiation exposure, leading to anesthesia and radiation complications. Third, adjunctive coiling could increase a hospital’s total cost by 30%. Previous studies found that PED treatment was a cost-effective strategy for small or larger and giant aneurysms than traditional stent-assisted or single coiling [25, 26]. However, whether the use of coiling is cost-effective compared to PED alone remains unclear.
In this study, we grouped complications into major and total complications. Regarding major complications, no significant difference was found between the PED-coiling and PED-alone groups in the original and sIPTW cohorts. However, the total complication rate was significantly higher in the PED-coiling group compared with the PED-alone group in both the original and sIPTW cohorts; this may be owing to a higher rate of minor complications in the PED-coiling group.
Perioperative complications include intraoperative and postoperative complications. Owing to the study’s retrospective design, we could only determine whether an intraoperative complication was directly caused by additional coiling. However, we did not find intraoperative complications resulting from additional coiling. Among the postoperative complications, the major difference between the PED-coiling and PED-alone groups was the minor ischemic stroke complications. Most patients had only transient ischemic symptoms without any angiographic evidence of pathology; therefore, we could not prove whether coiling is directly related to this type of complication. In the sIPTW cohort, complications differed significantly even after adjusting for confounding factors such as aneurysm size, which indicates that coiling may be related to postoperative complications. Therefore, further randomized controlled trials are needed to address this issue.
In the aneurysms treated with PED coiling, we found that the complications and angiographic and clinical outcomes were similar to those undergoing loose and dense packing. Dense packing, however, resulted in a 7% total cost increase. Similar results were also observed in the sIPTW analysis. These results demonstrated that loose packing is sufficient when coiling is used for PED treatment. However, dense packing should also be avoided to reduce the possibility of thrombosis and mass effects in the treatment of large IAs [12].
Furthermore, Nossek et al reported that loose packing achieved early complete occlusion of aneurysms compared with dense packing, without inducing any mass effect [9]. From a hemodynamic viewpoint, intra-aneurysmal hemodynamics tend to stabilize beyond a packing density of 7.06% or the use of two coils [15]. In our study, we first investigated the association between the coiling number and angiographic outcome and presented it in the RSC curve from a larger clinical setting. We found an “L-shaped” relationship between them across the entire cohort. When the coiling number is larger than approximately 3, the risk of incomplete occlusion is lowest and stable, indicating that excessive packing of the aneurysm sac is futile and could increase the total hospital cost. This population analysis result is highly consistent with previous hemodynamic results. Our results from a population analysis viewpoint could help surgeons treating IAs with PED to determine how many coils can achieve the best treatment effect.
Limitations
Our study has some limitations. Although we introduced our experience of coiling utilization in PED treatment in a large cohort, the single-center and retrospective design may still affect the generalizability of the results. Additionally, different centers may differ in the specific details of PED treatment. Prospective research is needed to further investigate the use of coiling embolization in aneurysms with PED treatment. A calculation error could be introduced since we only used coil numbers and total coil length to represent the degree of coiling. Although we performed multivariate analyses (Tables 4 and 5) to adjust for possible confounding factors and applied sIPTW to ensure the stability of the results among different aneurysms, factors including aneurysm size, location, and morphology can influence the choice regarding the degree of coiling pursued.
Conclusion
Assisted coiling may improve the aneurysm occlusion. However, it could also increase the total perioperative complication risk, prolong the procedure time, and increase the total treatment cost. Compared with loose packing, dense packing did not enhance the treatment effectiveness but increased the treatment cost. Our RCS curves showed “L-shape” relationships between the coil number or total coil length and angiographic outcomes. When the coil number was greater than 3 or the total coil length was longer than 150 cm, the incomplete occlusion risk reached a trough and began to remain stable.
Abbreviations
- CI:
-
Confidence interval
- IA:
-
Intracranial aneurysm
- OR:
-
Odds ratio
- PED:
-
Pipeline embolization device
- RCS:
-
Restricted cubic spline
- SAH:
-
Subarachnoid hemorrhage
- sIPTW:
-
Stabilize inverse probability of treatment weighting
References
Petr O, Brinjikji W, Cloft H, Kallmes DF, Lanzino G (2016) Current trends and results of endovascular treatment of unruptured intracranial aneurysms at a single institution in the flow-diverter era. AJNR Am J Neuroradiol 37:1106–1113
Zhang Y, Liang F, Zhang Y et al (2019) Exploring the feasibility of pipeline embolization device compared with stent-assisted coiling to treat non-saccular, unruptured, intradural vertebral artery aneurysms. Front Neurol 10:275
Chalouhi N, Tjoumakaris S, Starke RM et al (2013) Comparison of flow diversion and coiling in large unruptured intracranial saccular aneurysms. Stroke 44:2150–2154
Turowski B, Macht S, Kulcsár Z, Hänggi D, Stummer W (2011) Early fatal hemorrhage after endovascular cerebral aneurysm treatment with a flow diverter (SILK-Stent): do we need to rethink our concepts? Neuroradiology 53:37–41
Kang H, Luo B, Liu J et al (2022) Postoperative occlusion degree after flow-diverter placement with adjunctive coiling: analysis of complications. J Neurointervent Surg 14:371–375
Lin N, Brouillard AM, Krishna C et al (2015) Use of coils in conjunction with the pipeline embolization device for treatment of intracranial aneurysms. Neurosurgery 76:142–149
Zhang Q, Shao Q, Chang K et al (2021) Safety and efficacy of coils in conjunction with the pipeline flex embolization device for the treatment of cerebral aneurysms. Front Neurol 12:651465
Peschillo S, Caporlingua A, Resta MC et al (2017) Endovascular treatment of large and giant carotid aneurysms with flow-diverter stents alone or in combination with coils: a multicenter experience and long-term follow-up. Oper Neurosurg (Hagerstown) 13:492–502
Nossek E, Chalif DJ, Chakraborty S, Lombardo K, Black KS, Setton A (2015) Concurrent use of the pipeline embolization device and coils for intracranial aneurysms: technique, safety, and efficacy. J Neurosurg 122:904–911
Bender MT, Jiang B, Campos JK et al (2018) Single-stage flow diversion with adjunctive coiling for cerebral aneurysm: outcomes and technical considerations in 72 cases. J Neurointervent Surg 10:843–850
Park MS, Kilburg C, Taussky P et al (2016) Pipeline embolization device with or without adjunctive coil embolization: analysis of complications from the IntrePED registry. AJNR Am J Neuroradiol 37:1127–1131
Siddiqui AH, Kan P, Abla AA, Hopkins LN, Levy EI (2012) Complications after treatment with pipeline embolization for giant distal intracranial aneurysms with or without coil embolization. Neurosurgery 71:E509–E513
Raymond J, Guilbert F, Weill A et al (2003) Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke 34:1398–1403
Kamran M, Yarnold J, Grunwald IQ, Byrne JV (2011) Assessment of angiographic outcomes after flow diversion treatment of intracranial aneurysms: a new grading schema. Neuroradiology 53:501–508
Zhang M, Tian Z, Zhang Y et al (2022) How to perform intra-aneurysmal coil embolization after pipeline deployment: a study from a hemodynamic viewpoint. J Neurointervent Surg 15:157–162
Jing L, Zhong J, Liu J et al (2016) Hemodynamic effect of flow diverter and coils in treatment of large and giant intracranial aneurysms. World Neurosurg 89:199–207
Tan LA, Keigher KM, Munich SA, Moftakhar R, Lopes DK (2015) Thromboembolic complications with pipeline embolization device placement: impact of procedure time, number of stents and pre-procedure P2Y12 reaction unit (PRU) value. J Neurointerv Surg 7:217–221
Cagnazzo F, di Carlo DT, Cappucci M, Lefevre P-H, Costalat V, Perrini P (2018) Acutely ruptured intracranial aneurysms treated with flow-diverter stents: a systematic review and meta-analysis. AJNR Am J Neuroradiol 39:1669–1675
Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF (2013) Endovascular treatment of intracranial aneurysms with flow diverters: a meta-analysis. Stroke 44:442–447
Ikeda H, Ishii A, Kikuchi T et al (2015) Delayed aneurysm rupture due to residual blood flow at the inflow zone of the intracranial paraclinoid internal carotid aneurysm treated with the pipeline embolization device: histopathological investigation. Interv Neuroradiol 21:674–683
Tateshima S, Jones JG, Mayor Basto F, Vinuela F, Duckwiler GR (2016) Aneurysm pressure measurement before and after placement of a pipeline stent: feasibility study using a 0.014 inch pressure wire for coronary intervention. J Neurointervent Surg 8:603–607
Kerl HU, Boll H, Fiebig T et al (2014) Implantation of pipeline flow-diverting stents reduces aneurysm inflow without relevantly affecting static intra-aneurysmal pressure. Neurosurgery 74:321–334
Sorteberg A, Sorteberg W, Turk AS, Rappe A, Nakstad PH, Strother CM (2001) Effect of Guglielmi detachable coil placement on intraaneurysmal pressure: experimental study in canines. AJNR Am J Neuroradiol 22:1750–1756
Kan P, Siddiqui AH, Veznedaroglu E et al (2012) Early postmarket results after treatment of intracranial aneurysms with the pipeline embolization device: a U.S. multicenter experience. Neurosurgery 71:1080–1087
Malhotra A, Wu X, Brinjikji W et al (2019) Pipeline endovascular device vs stent-assisted coiling in small unruptured aneurysms: a cost-effectiveness analysis. Neurosurgery 85:E1010–E1019
Wali AR, Park CC, Santiago-Dieppa DR, Vaida F, Murphy JD, Khalessi AA (2017) Pipeline embolization device versus coiling for the treatment of large and giant unruptured intracranial aneurysms: a cost-effectiveness analysis. Neurosurg Focus 42:E6
Acknowledgements
We thanked Yuesong Pan for the statistics methodology and Zhongxue Wu for being the guarantor.
Funding
This study has received funding from the Natural Science Foundation of China (81771233,82171290); Research and Promotion Program of Appropriate Techniques for Intervention of Chinese High-risk Stroke People (GN-2020R0007); BTH Coordinated Development-Beijing Science and Technology Planning Project (Z181100009618035); Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20190501) and Beijing Natural Science Foundation (19L2013, 22G10396).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Zhongxue Wu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Yuesong Pan kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained. The Beijing Tiantan Hospital institutional research ethics boards approved this study.
Methodology
• Retrospective
• case-control study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tong, X., Han, M., Xue, X. et al. Coiling embolization strategy for medium-to-giant-sized intracranial aneurysms treated with pipeline embolization device: a propensity score-weighted study. Eur Radiol 33, 7967–7977 (2023). https://doi.org/10.1007/s00330-023-09800-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09800-z