Abstract
Objectives
To describe injury patterns in children with multiple trauma (MT), evaluate the yield of dual-phase whole-body CT (WBCT), and quantify missed injuries detected on second reading.
Methods
Remotely analyzed WBCT performed between 2011 and 2020 in 63 emergency departments on children admitted for MT were included. Second reading occurred within 24 h. Collected data included age, sex, mechanism, Injury Severity Score (ISS), radiologists’ experience, time and duration of first reading, conclusion of both readings, and dosimetry. Melvin score assessed the clinical impact of missed injuries.
Results
Overall, 1114 patients were included, 1982 injuries were described in 662 patients (59.4%), 452/1114 (40.6%) WBCT were negative, and 314 (28.2%) patients had MT (≥ 2 body parts injured). The most frequent injuries were pulmonary contusions (8.3%), costal fractures (6.2%), and Magerl A1 vertebral fractures (4.9%). Overall, 151 injuries were missed in 92 (8.3%) patients. Independent predictors for missed injuries were age ≤ 4 years (p = 0.03), number of injured body parts ≥ 2 (p = 0.01), and number of injuries ≥ 3 (p < 0.001). Melvin score grade 3 lesions were found in 16/92 (17.4%) patients with missed injuries (1.4% of all WBCT), where only prolonged follow-up was necessary. Thirteen active bleeding or pseudoaneurysms were detected (0.7% of injuries).
Conclusion
Injuries were diagnosed in 59.4% of patients. Double-reading depicted additional injuries in 8.3% of patients, significantly more in children ≤ 4 years, with ≥ 3 injuries or ≥ 2 injured body parts. As 28 % of patients had MT and 1.1% had active extravasation or pseudoaneurysm, indication for WBCT should be carefully weighted.
Key Points
• When performed as a first-line imaging evaluation, approximately 41% of WBCT for MT children were considered normal.
• The three most common injuries were pulmonary contusions, costal fractures, and Magerl A1 vertebral fractures, but the patterns of traumatic injuries on WBCT depended on the children’s age and the trauma mechanism.
• The independent predictors of missed injuries were age ≤ 4 years, number of body parts involved ≥ 2, and total number of injuries ≥ 3.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Trauma is a major public health problem and the leading cause of pediatric morbidity and mortality. In the USA, traffic accidents are the leading cause (20%) of pediatric deaths [1]. Multisystem trauma (MT) is defined as associated injuries (i.e., ≥ 2 severe injuries in ≥ 2 body areas) or with multiple injuries (i.e., ≥ 2 severe injuries in one body area) [2].
While relationships among injury mechanisms, patterns, severity, and missed injuries have been described in adults with precise guidelines [3,4,5], pediatric literature remains scarce. However, children and adults display distinct injury patterns [6].
Previous studies demonstrated that half of children’s deaths are due to neurological or cardiovascular trauma [7,8,9]. The head is more impacted in younger children with increased craniofacial injuries [10]. Although mediastinal injuries are rare, high thoracic plasticity in children implies limited parietal injuries but frequent parenchymal injuries. The mobility of intra-abdominal organs combined with abdominal wall weakness may lead to more damaging renal, splenic, and liver trauma [6, 7].
The best emergency imaging strategy for children is currently debated [11,12,13,14]. To date, recommendations are to perform first-line assessment with standard X-rays and abdominal ultrasound [15], color Doppler and contrast-enhanced ultrasound being debated. The systematic use of whole-body CT scans (WBCT) is controversial because of higher ionizing radiation and missing evidence to better target children who would benefit from WBCT compared to standard imaging [14, 15]. Several studies suggested that pediatric WBCT are mainly normal [16,17,18,19]. As compared with adults, the use of WBCT was not found to improve survival as compared with selective imaging [3, 4].
Among other reasons [20], the expansion of emergency teleradiology, as a reasonable solution to the shortage in medical resources, might have led to a significant increase in the use of WBCT for MT children instead of standard imaging. Besides, emergency teleradiology can gather large multicentric series due to homogeneous information and technology tools. Such large series could help capture the specificity of pediatric injuries, their relationships to age or mechanism, and the risk factors for missed injuries. Ultimately, a better understanding of the links between the initial patients and trauma characteristics may help personalize the imaging strategy for MT children.
Additionally, systematic double-reading of WBCT in adults revealed a significant proportion of first-reading missed injuries despite the implementation of standardized workflows and WBCT protocols [21,22,23]. However, the clinical interest of systematic double-reading has not been thoroughly evaluated in MT children.
Therefore, our main objectives were to describe the pattern of injuries in children with MT, to evaluate the yield of a second reading and the frequency and predictive factors of missed injuries on WBCT and to assess the clinical impact of missed injuries.
Materials and methods
Study design
The National Radiological Ethics Review Board approved this multicenter observational retrospective study (IRB: CRM-2101–126).
We included all consecutive WBCT performed between February 2011 and February 2020 in the emergency departments of 63 partner hospitals of our teleradiology company during on-call hours (i.e., 6:00 p.m. to 8:00 a.m. on weekdays and 24 h on weekends). Inclusion criteria were age < 18 years old justifying WBCT with contrast media.
WBCT was performed on emergency physicians’ requests for children suspected of having trauma-associated injury or with multiple injuries, according to the French trauma triage guidelines [24].
WBCT technique
Once patients stabilized, examinations were performed using 16- or 64-slice multidetector CT scanners according to standardized protocols adapted to children’s habitus (Supplementary Material 1).
First, a noncontrast 1- to 1.25-mm slice thickness acquisition covering the brain and cervical spine in dorsal decubitus with arms besides the body was performed and reconstructed to reach 1 mm thickness in bone and brain kernels. When possible, arms were then raised above the head. Intravenous injection of nonionic contrast agent was performed. The contrast agents were Omnipaque 350 (GE Healthcare), Iomeron 400 (Bracco Diagnostics), and Ultravist 370 (Bayer Healthcare). An automatic injector was used at a rate of 1.5 cc/s (concentration: 300–350 mg/mL). The injected volume was 2 cc/kg for children < 5 kg and 1.5 cc/kg for those ≥ 5 kg. A thorax-abdomen-pelvic acquisition was achieved at the arterial phase (slice thickness: 1–1.25 mm, reconstructed to 1 mm) followed by an abdominopelvic acquisition at the portal phase (slice thickness: 2–2.5 mm, reconstructed to 2 mm). A 5–10-min late phase was added if urinary tract injury was clinically or radiologically suspected. Delayed phase was decided by the off-site radiologist in charge, the technologists always calling him/her before ending the CT procedure. A bone kernel of the thorax-abdomen-pelvic acquisition was reconstructed from the thickness of native sections.
Radiological interpretation
The interpretation protocol met the current French medical recommendations for teleradiology practice [25].
Radiologists worked in dedicated centers with specific high-standard ergonomic conditions. Standardized examination requests with clinical and laboratory information were received via ITIS software (ITIS; Deeplink Medical). Each request was medically validated by one of the on-call radiologists. Examinations were then performed on-site, and images were securely transferred via a private server to a local picture archiving and communication system (Carestream Health 11.0). WBCT were interpreted in one of the three interpretation centers (Bordeaux or Lyon, France). The main findings were immediately communicated by phone call to the emergency physician, followed by a written report to the referring institution through ITIS software.
The radiologist panel consisted of 57 senior radiologists (with ≥ 5 years of emergency imaging experience in a level 1 trauma center [average: 7 years]) and 37 juniors (residents with 3–5 years of emergency imaging experience in a level 1 center [average: 4 years]). All junior and senior radiologists validated a 6-month pediatric rotation certified by the French College of Radiology Teachers (CERF). Four seniors performed a 2-year pediatric imaging fellowship. In our dedicated centers, experienced radiologists are constantly available for advising juniors.
The number of radiologists per on-call duty period ranged from 2 to 8.
Second readings occurred 12 to 24 h after the first reading, and was performed by another radiologist who was not on call and had access to the initial report. All discrepancies were described in a new report sent to the requiring hospital, and the referring emergency physician was called if complementary management was required. Second reading took place even if initial reading was normal.
Data collection
Two radiologists (P.D. and N.B. with 5 and 8 years of experience in emergency imaging, respectively) extracted the following data from our database: age (further categorized as 0–4 years, 4–8 years, 8–14 years, and 14–18 years [8, 26]); sex; partner hospital; dosimetry; trauma mechanism (categorized as fall [for fall and horse-riding accident], motor vehicle accident [MVA, by car or two-wheels], non-motorized accident [bicycle or pedestrian], aggression [physical assault], and other/unknown); experience of the radiologist at first and second readings (categorized as senior if the radiologist achieved his or her MD diploma and had more than 2 years of experience in emergency imaging and junior otherwise); time period and duration of first reading (defined as the delay from the reception of the 1st image of the WBCT to the validation of the radiological report); conclusions of both readings.
All injuries described in both reports were classified according to the corresponding injured body parts (i.e., head and neck, face, thorax, abdomen, spine, bone, and soft tissue). The Abbreviated Injury Scale (AIS) was determined for each of the six following body parts, enabling the calculation of the Injury Severity Score (ISS) [27]: head and neck, face, thorax, abdomen, limbs, and external surface.
The clinical effect of missed injuries was retrospectively classified with the Melvin scoring system [28]. Grade 0 means no discrepancy. Grade 1 means minor discrepancy with minor effect on treatment or management. Grade 2 means significant discrepancy that significantly affects treatment or management, with no effect on outcome. Grade 3 is a major discrepancy that affects outcome.
Statistical analysis
Statistical analyses were performed with R (v3.5.3). All tests were two-tailed. A p value < 0.05 was considered significant. Comparison of continuous variables depending on categorical variables with more than two levels was achieved using the Kruskal-Wallis test and the corresponding chi-squared statistics (K) was given.
Regarding factors leading to missed injuries, continuous variables were compared between the patients with and without missed injuries using the Wilcoxon rank-sum test. The frequencies of categorical variables were compared between the two groups by using Fisher’s exact test or the chi-squared test as appropriate. Predictors with a p value less than 0.100 in the univariate analysis were selected for the multivariate modelling. Beforehand, continuous variables were transformed into binary variables using the coordinates of the closest top left point of the receiver operating characteristic (ROC) curves (“pROC” package). The final set of explanatory variables was entered into a stepwise binary logistic regression with backward and forward elimination to identify the independent predictors of the occurrence of a missed injury and to estimate their odds ratio (OR) with 95% confidence intervals (95% CI) based on the minimization of the Akaike Information criteria.
Results
Study population and examinations
Figure 1 shows the flow chart. Overall, 1114 patients were included. Table 1 shows the population characteristics. Overall, 756/1114 (67.9%) patients were boys, and 358/1114 (32.1%) were girls. The median age was 14 years (range: 0–17, including 43 children ≤ 2 years).
The average interpretation time was 32.4 ± 13 min (median: 30 min; range: 8–92 min, with 95% of the interpretation duration < 57 min). Junior radiologists interpreted 402/1114 (36.1%) WBCT, and seniors interpreted 712/1114 (63.9%) WBCT, mostly during the 9 p.m.–0 a.m. time period (338/1114 [30.3%] examinations). Second readings were performed by junior radiologists in 303/1114 cases (27.2%) and seniors in 811/1114 (72.8%).
Traumatic mechanisms were distributed as follows: 194/1114 (17.4%) falls and 47/1114 (4.2%) horse riding accidents (“falls” in Table 1: 241/1114 [21.6%]); 261/1114 (23.4%) MVA by car and 334/1114 (30%) MVA by two-wheels (total MVA: 595/1114 [53.4%]); 114/1114 (10.2%) trauma involving pedestrians and 91/1114 (8.2%) trauma involving cyclists (non-motorized accidents: 205/1114 [18.4%]); 25/1114 (2.2%) aggression; and 48/1114 (4.4%) others/unknown.
The average dosimetry was 1983.5 ± 1051.1 mGy.cm (details: 805 ± 297.7 mGy.cm for 0- to 4-year-old children, 988.2 ± 509 mGy.cm for 4- to 8-year-old children, 1712 ± 847 mGy.cm for 8- to 14-year-old children, and 2489.1 ± 965.3 mGy.cm for 14- to 18-year-old children).
The distribution of WBCT among partner hospitals is detailed in Supplementary material 2.
Distribution of traumatic injuries
Overall, 452/1114 (40.6%) examinations did not demonstrate any traumatic injury after two readings, and 1982 distinct traumatic injuries were described (median number of injuries per patient: 1, range: 0–21) in 662/1145 (59.4%) patients. There were 314 (28.2%) patients that had multisystemic trauma (≥ 2 body part injured). Of 662 patients with injuries, 319 (48.2%) had minor findings with an ISS < 5. Figure 2 shows the proportion of normal examinations depending on age and trauma mechanisms. There were 313/1982 (15.7%) moderate to severe injuries (AIS ≥ 3).
Distribution of the normal examinations depending on the trauma mechanism and the age group. A Motor vehicle accident (MVA), (B) fall, (C) non-motorized accident, (D) other, and (E) aggression. Abbreviation: y, years. For each bar, the numbers correspond to the number of normal examinations divided by the total number of examinations in the subgroup with percentages in parentheses
Supplementary material 3 shows 131 possible types of injuries described, and the distribution of these injuries. There were 13 cases (0.7%) with active bleeding or pseudoaneurysms. Regarding age, brain was the most frequently injured body part for patients 0–4 and 4–8 years old (63/184 [34.2%] and 43/192 [22.4%] injuries in these groups, respectively), and bone for patients 8–14 and 14–18 years old (172/597 [28.8%] and 214/1009 [21.2%] injuries in these groups, respectively) (Table 2). The average ISS was 4.9 ± 6.9 (range: 0–45) (Table 1). The highest average ISS was found in the 0–4 years group (average ISS = 5.9 ± 7.4) and for the fall mechanism (average ISS = 5.7 ± 7.2) (Supplementary data 4); however, comparisons of the average ISS depending on age groups or trauma mechanisms did not reach significance (K = 6.23, p = 0.1 and K = 5.55, p = 0.2, respectively). Table 2 and Fig. 3 show the distribution of injuries by body part and by mechanism or age group. The most frequently affected body areas were as follows: bones for falls and MVA traumas (117/497 [23.5%] and 232/1007 [23%] of injuries, respectively); brain for non-motorized traumas (97/373 [26%] of injuries); and face for aggressions (17/33 [51.5%] of injuries). No association was found between the number of lesions and the trauma mechanism (K = 4.73, p = 0.3), and the number of lesions and the age groups (K = 4.28, p = 0.2)
The three most frequent injuries in descending order were pulmonary contusions (165/1982 [8.3%]), costal fractures (123/1982 [6.2%]), and Magerl A1 vertebral fractures (97/1982 [4.9%]). The most frequent injuries for each age group and trauma mechanism are shown in Supplementary data 5.
Missed injuries
Overall, 1831 injuries were described at first reading, and 151 missed injuries were found on 92 WBCT. The incidence of missed injuries was calculated as 7.6% on a per-injury basis and 8.3% on a per-patient basis. The 5 most frequently missed injuries were transverse process fractures (11/151 [7.3%]), rib fractures (10/151 [6.6%]), pneumothoraces (10/151 [6.6%]), peritoneal effusion (9/151 [6%]), and Magerl A1 vertebral fractures (9/151 [6%]). In univariate analysis, the following four variables were significantly associated with missed injuries: age ≤ 4 years old (p = 0.02), number of injuries per patient (p <0.001), number of distinct injured body areas (p < 0.001), and ISS (p < 0.001) (Table 3). ROC curve analysis emphasized the following thresholds for the continuous potential predictors: ≥ 3 injuries, ISS ≥ 5 injuries, and ≥ 2 distinct injured body parts (Fig. 4). Table 4 shows the results of multivariate stepwise binary logistic regression. The following three variables were selected as independent predictors of missed injuries: age < 4 years old (OR = 2.04, 95% CI = 1.02–3.85, p = 0.03), ≥ 2 distinct injured body areas (OR = 2.5, 95% CI = 1.2–5, p < 0.001), and ≥ 3 injuries (OR = 3.7, 95% CI = 1.9–7.6, p < 0.001) (Fig. 5).
Cut-off analysis with ROC curves and thresholds for the following continuous variables significantly correlated with the occurrence of missed injuries in univariable analysis: (A) number of lesions, (B) number of distinct injured body parts reached, and (C) Injury Severity Score (ISS). The area under the ROC curve (AUROC) for the number of lesions was 0.82 (95% CI = 0.78–0.85) with the closest top left point for a cut-off of 3 lesions (sensitivity = 0.66; specificity = 0.79). The AUROC for the number of injured distinct body parts was 0.80 (95% CI = 0.77–0.84) with the closest top left point for a cut-off of 2 lesions (sensitivity = 0.68; specificity = 0.75). The AUROC for ISS was 0.78 (95% CI = 0.74–0.82) with the closest top left point for a cut-off of 5 (sensitivity = 0.67; specificity = 0.73)
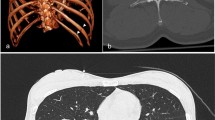
Missed lesions identified at the second reading. A 3-year-old boy crushed on the back with a 125-kg gate was unconscious for a few seconds, and he had no neurological symptoms. However, the physical examination was hampered by the child’s pain. A Right K8 to K10 rib fractures as well as coronal MPR bone reconstruction identified at the first reading (arrowheads). B Right pulmonary contusions and axial lung reconstruction diagnosed at the first reading (arrows). C L1 and L2 Magerl A1 fractures as well as sagittal bone reconstruction missed at the first reading but correctly identified at the second reading (arrowheads). There were no modifications in the medical care (ISS of 9 at the first reading and ISS of 13 after the second reading; Melvin score grade 1 of discrepancy with minor clinical significance)
There was no significant difference regarding missed injuries between junior and senior radiologists as 35/92 missed injuries (38%) were missed by juniors compared to 57/92 (62%) by seniors (p = 0.2).
Missed injuries with a grade 3 clinical effect according to the Melvin scoring system were found in 16 of 92 (17.4%) WBCT with missed injuries (16/1114 (1.4%) of all WBCT). For all 16 patients, the only change in medical care was prolonged follow-up and medical stay (i.e., same medical stay as if the missed injuries had been diagnosed during the 1st reading). There were 56 of 92 (60.8%) WBCT with missed injuries of grade 2 and 20/92 (21.7%) WBCT with missed injuries of grade 1, with no change or minor change in medical management.
Discussion
This multicentric study offers an extensive overview of the most frequent injuries in MT children based on the mechanism and identifies factors leading to missed injuries.
Epidemiological data from other pediatric series agree with our results concerning the accident mechanism rate (MVA was the most frequent), most frequent injuries (pulmonary contusion and rib fractures were the most frequent), and body part injuries (bone and thorax were the two most frequent) [13, 29].
In our study, bone and chest injuries were the most frequent in MVA (23 and 19.3%), while bone and spine injuries prevailed in falls (23.5 and 17.9%). Brain and bone injuries predominated in non-motorized accidents (26 and 21.2%), and facial injuries predominated in physical assault (51.5%). We also found the most frequently injured body part was different between 0- to 8-year-old and 8- to 17-year-old children (i.e., brain versus bone, respectively). Indeed, brain injuries were more common at a young age in MVA. The head-body ratio is negatively correlated with age, and there are preferential head impacts at a younger age [30]. Overall, pulmonary contusion was the most common injury (8% of all injuries), which can be explained by chest plasticity [30].
Herein, the incidence of missed injuries (7.6% on a per-injury basis and 8.2% on a per-patient basis) was comparable with the literature. For example, Banaste et al found 8.8% missed injuries in a mixed pediatric and adult population [21], and Giannakopoulos et al found 8.2% missed injuries in 1124 level-1 trauma patients of any age [31]. Interpretation of emergency WBCT during on-call periods contributes to a significant number of missed injuries and encourages a systematic double reading [21, 23].
However, our retrospective follow-up review of 92 patients with missed injuries revealed that the clinical impact in children was minor. Indeed, a grade 3 clinical effect via the Melvin scoring system was reported in 16/92 (17.4%) of these patients, and the sole medical adjustment was prolonged hospital follow-up. However, Banaste et al reported 19.4% of grade 3 missed injuries, and of these, 64.4% of them had a medical care change, which could be explained by the conservative management of pediatric MT, especially in solid organ injuries [32]. As described in adults, however, accurate measurement of lung contusion volume could identify patients at higher risk of delayed ARDS [33].
In the present study, age < 4 years was an independent predictor for missed injuries. Some of the higher proportion of missed injuries in younger children may be explained by the challenge of distinguishing normal age-related variations from injuries. Thus, second readings by pediatric radiologists could be helpful in children younger than 4 years old with multiple injuries involving multiple body parts. Additionally, providing emergency radiologists with educational content dedicated to trauma in children < 4 years may help reduce missed injuries.
Greater than or equal to 2 distinct injured body areas and ≥ 3 injuries were significantly associated with missed injuries. Similar results were found in adults [21]. Most of the time, a combination of factors leads to missed injuries, such as fatigue, experience, and cognitive biases. Our results may also be explained by the satisfaction of the search effect, i.e., when the radiologist’s attention is held or focused on a specific injury or area, it may cause the radiologist to overlook other body parts [34].
Our study had limitations. First, it focused on emergency WBCT for MT children, whereas such use is strongly debated [35]. Of note, our purpose was not to evaluate the interest of WBCT as first-line imaging for MT children. It was to take advantage of a series in which physicians did not have other alternatives, to better understand specific pediatric MT injury patterns and risk factors for missed injuries. The main disadvantage of WBCT in children is over-irradiation, whereas ALARA principle remains mandatory [36,37,38]. Our average dosimetry was 1983.5 ± 1051.1 mGy.cm, which was comparable to 1877.46 ± 562.57 mGy.cm in the study by Frellesen et al [13]. The need for WBCT must be justified by the individual benefit/risk ratio and the implementation of clinico-biological scores and prediction models. However, this has been mainly studied to avoid unnecessary abdominal CT [39]. In the present study, we observed a significant proportion of normal WBCT (40.6%), which was consistent with the literature [16,17,18,19]. Thus, the role of selective scanning remains debated for isolated high-velocity trauma, except if the patient is unstable and/or critical. As compared with adults, the use of WBCT was not found to improve survival as compared with selective imaging [3, 4]. Obviously, a stepwise approach with dedicated X rays and abdominal ultrasound, and in clinically stable patients a wait-and-see policy would have obviated most if not all of these normal WBCT [40]. The importance of the radiologists’ experience (i.e., junior or senior) may have been biased because junior radiologists could ask seniors for advice when facing complex examinations.
Second, our study was limited by its retrospective design and data collection focused on radiological reports. Initial and follow-up clinical data were not available to calculate in-hospital or delayed mortality, or subsequent therapeutic managements. We were not able to investigate the influence of the delay between the 1st and 2nd readings on the changes in therapeutic management. Besides, on the study period, multiphasic protocols were used, which are more irradiating. From then, practices are now moving to monophasic protocols.
Third, the number of cervical sprains may have been over-estimated by non-pediatric radiologists due to cervical collars and decubitus position, reducing physiological lordosis [41].
Besides, we involved junior radiologists. However, we demonstrated that they did not miss more injuries than seniors, and the types of readers’ combinations showed no difference from nonspecific pediatric CTs [21]. An explanation might be our organization in dedicated centers where experienced radiologists are constantly available for advising juniors.
Finally, approximately 200 patients are part of the population studied in Banaste et al [21]. Nevertheless, herein we analyzed more variables like trauma mechanisms and we made a complete description of pediatric injuries and identified specific pediatric factors that may lead to missed injuries by radiologists. Thus, our current study provides new knowledge about pediatric trauma and imaging.
To conclude, our study highlighted different patterns of injuries depending on age and trauma mechanism in MT children. Brain injuries were more common at a young age in MVA. Bone and spine injuries prevail in falls whereas bone and chest injuries were most frequent in MVA. We found that studies in children < 4 years, with ≥ 2 injured body areas, and ≥ 3 injuries had a high risk of missed injury and may benefit from a second reading.
We believe this may help (i) general and pediatric radiologists to improve the reading accuracy of pediatric WBCT, (ii) emergency physicians to prompt a second reading in selected cases, and (iii) establish decisional imaging algorithms to reduce the overuse of WBCT in pediatric patients managed in nondedicated trauma centers.
Abbreviations
- 95% CI:
-
95% confidence interval
- AIS:
-
Abbreviated Injury Scale
- ISS:
-
Injury Severity Score
- K:
-
Kruskal-Wallis chi-squared statistics
- MT:
-
Multisystem trauma
- MVA:
-
Motor vehicle accident
- OR:
-
Odds ratio
- WBCT:
-
Whole-body CT scans
References
Cunningham RM, Walton MA, Carter PM (2018) The major causes of death in children and adolescents in the United States. N Engl J Med 379:2468–2475. https://doi.org/10.1056/nejmsr1804754
Nice (2016) Major trauma : assessment and initial management. NICE Guidel
Philipp MO, Kubin K, Hörmann M, Metz VM (2003) Radiological emergency room management with emphasis on multidetector-row CT. Eur J Radiol. https://doi.org/10.1016/S0720-048X(03)00206-7
Geyer LL, Körner M, Linsenmaier U et al (2013) Incidence of delayed and missed diagnoses in whole-body multidetector CT in patients with multiple injuries after trauma. Acta Radiol. https://doi.org/10.1177/0284185113475443
Huber-Wagner S, Biberthaler P, Häberle S et al (2013) Whole-body CT in haemodynamically unstable severely injured patients - a retrospective, multicentre study. PLoS One. https://doi.org/10.1371/journal.pone.0068880
Chaumoître K, Merrot T, Petit P, Panuel M (2008) Particularités des traumatismes thoraciques et abdominaux chez l’enfant. J Radiol. https://doi.org/10.1016/s0221-0363(08)74492-5
Orliaguet GA, Meyer PG, Blanot S et al (1998) Predictive factors of outcome in severely traumatized children. Anesth Analg. https://doi.org/10.1213/00000539-199809000-00006
Javouhey E, Guérin AC, Amoros E et al (2006) Severe outcome of children following trauma resulting from road accidents. Eur J Pediatr. https://doi.org/10.1007/s00431-006-0118-z
Desforges JF, Trunkey D (1991) Initial treatment of patients with extensive trauma. N Engl J Med. https://doi.org/10.1056/nejm199105023241806
Ducrocq SC, Meyer PG, Orliaguet GA et al (2006) Epidemiology and early predictive factors of mortality and outcome in children with traumatic severe brain injury: experience of a French pediatric trauma center. Pediatr Crit Care Med. https://doi.org/10.1097/01.PCC.0000235245.49129.27
Hilbert-Carius P, Hofmann GO, Lefering R et al (2015) Whole-body-CT in severely injured children. Results of Retrospective, Multicenter Study with Patients from the TraumaRegsiter DGU®. Klin Pädiatrie. https://doi.org/10.1055/s-0035-1547311
Abe T, Aoki M, Deshpande G et al (2019) Is whole-body CT associated with reduced in-hospital mortality in children with trauma? A nationwide study*. Online Clin Investig. https://doi.org/10.1097/PCC.0000000000001898
Frellesen C, Klein D, Tischendorf P et al (2018) Indication of whole body computed tomography in pediatric polytrauma patients—diagnostic potential of the Glasgow Coma Scale, the mechanism of injury and clinical examination. Eur J Radiol. https://doi.org/10.1016/j.ejrad.2018.05.022
Strohm PC, Uhl M, Hauschild O et al (2008) What is the value of the whole body spiral CT in the primary radiological imaging of severely injured children? Z Orthop Unfall. https://doi.org/10.1055/s-2007-989438
Miele V, Di Giampietro I, Ianniello S et al (2014) Diagnostic imaging in pediatric polytrauma management. Radiol Med. https://doi.org/10.1007/s11547-014-0469-x
Da Dalt L, Marchi AG, Laudizi L et al (2006) Predictors of intracranial injuries in children after blunt head trauma. Eur J Pediatr. https://doi.org/10.1007/s00431-005-0019-6
Hulka F, Mullins RJ, Leonardo V et al (1998) Significance of periteneal fluid as an isolated finding on abdominal computed tomographic scans in pediatric trauma patients. J Trauma. https://doi.org/10.1097/00005373-199806000-00021
Neish AS, Taylor GA, Lund DP, Atkinson CC (1998) Effect of CT information on the diagnosis and management of acute abdominal injury in children. Radiology. https://doi.org/10.1148/radiology.206.2.9457182
Jindal A, Velmahos GC, Rofougaran R (2002) Computed tomography for evaluation of mild to moderate pediatric trauma: are we overusing it? World J Surg. https://doi.org/10.1007/s00268-001-0174-5
Pandit V, Michailidou M, Rhee P et al (2016) The use of whole body computed tomography scans in pediatric trauma patients: are there differences among adults and pediatric centers? J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2015.12.002
Banaste N, Caurier B, Bratan F et al (2018) Whole-body CT in patients with multiple traumas: factors leading to missed injury. Radiology. https://doi.org/10.1148/radiol.2018180492
Agostini C, Durieux M, Milot L et al (2008) Value of double reading of whole body CT in polytrauma patients. J Radiol. https://doi.org/10.1016/s0221-0363(08)93007-9
Agrawal A, Koundinya DB, Raju JS et al (2017) Utility of contemporaneous dual read in the setting of emergency teleradiology reporting. Emerg Radiol. https://doi.org/10.1007/s10140-016-1465-3
Riou B, Thicoïpé M, Atain-Kouadio P et al (2002) Comment évaluer la gravité? SAMU de France. In: SFEM éditions (ed) Actualités en réanimation préhospitalière: le traumatisé grave. Vittel, France, pp 115–12825
SNITEM, Conseil professionnel de la Radiologie (2011) Téléimagerie – Téléradiologie Recommandations du SNITEM et du Conseil professionnel de la radiologie. http://www.sfrnet.org/rc/org/sfrnet/htm/Article/2004/mie-20040517-000000-07794/src/htm_fullText/fr/SNITEM-G4Rx-recos-TeleRx.pdf. Accessed 18 Feb 2018
Muhm M, Danko T, Henzler T et al (2015) Pediatric trauma care with computed tomography—criteria for CT scanning. Emerg Radiol. https://doi.org/10.1007/s10140-015-1332-7
Association for the Advancement of Automotive Medicine - Committee on Injury Scaling The Abbreviated Injury Scale. Des Plains, IL
Melvin C, Bodley R, Booth A et al (2004) Managing errors in radiology: a working model. Clin Radiol 59:841–845. https://doi.org/10.1016/j.crad.2004.01.016
National Highway Traffic Safety Administration (2010) Children injured in motor vehicle traffic crashes. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/811325
Huelke DF (1998) An overview of anatomical considerations of infants and children in the adult world of automobile safety design. Annu Proc Assoc Adv Automot Med 42:93–113
Giannakopoulos GF, Saltzherr TP, Beenen LFM et al (2012) Missed injuries during the initial assessment in a cohort of 1124 level-1 trauma patients. Injury 43:1517–1521. https://doi.org/10.1016/j.injury.2011.07.012
Gates RL, Price M, Cameron DB et al (2019) Non-operative management of solid organ injuries in children: an American Pediatric Surgical Association Outcomes and Evidence Based Practice Committee systematic review. J Pediatr Surg 54:1519–1526. https://doi.org/10.1016/j.jpedsurg.2019.01.012
Miller PR, Croce MA, Bee TK et al (2001) ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma 51:223–230. https://doi.org/10.1097/00005373-200108000-00003
Berbaum KS, El-Khoury GY, Ohashi K et al (2007) Satisfaction of search in multitrauma patients: severity of detected fractures. Acad Radiol. https://doi.org/10.1016/j.acra.2007.02.016
Meltzer JA, Stone ME, Reddy SH, Silver EJ (2018) Association of whole-body computed tomography with mortality risk in children with blunt trauma. JAMA Pediatr. 172:542–549. https://doi.org/10.1001/jamapediatrics.2018.0109
Munk RD, Strohm PC, Saueressig U et al (2009) Effective dose estimation in whole-body multislice CT in paediatric trauma patients. Pediatr Radiol. https://doi.org/10.1007/s00247-008-1091-7
Miglioretti DL, Johnson E, Williams A et al (2013) The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. https://doi.org/10.1001/jamapediatrics.2013.311
Fenton SJ, Hansen KW, Meyers RL et al (2004) CT scan and the pediatric trauma patient - are we overdoing it? J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2004.08.007
Streck CJ Jr, Jewett BM, Wahlquist AH, Gutierrez PS, Russell WS (2012) Evaluation for intra-abdominal injury in children after blunt torso trauma: can we reduce unnecessary abdominal computed tomography by utilizing a clinical prediction model? J Trauma Acute Care Surg 73(2):371–376. https://doi.org/10.1097/TA.0b013e31825840ab
Van Schuppen J, Olthof D, Wilde J et al (2013) Diagnostic accuracy of a step-up imaging strategy in pediatric patients with blunt abdominal trauma. Eur J Radiol. https://doi.org/10.1016/j.ejrad.2013.09.024
Hassan N, Butler C, DeCou J et al (2020) Pediatric cervical spine injuries on CT: difference in accuracy of interpretations by pediatric versus non-pediatric radiologists. Emerg Radiol. https://doi.org/10.1007/s10140-019-01743-7
Acknowledgements
We would like to thank Julien May (DICOM referent, IMADIS Teleradiology) for his technical support and assistance, and all partner centers for their trust and effective collaboration.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr Guillaume Gorincour.
Conflict of interest
PD, AC, SH, NB, and MS disclosed no relevant relationships.
AD and GG have shares in Deeplink Medical.
Statistics and biometry
One of the authors has significant statistical expertise (AC).
Informed consent
Written informed consent was not required for this study because of the retrospective nature of this study, and patients were informed about the reuse of their anonymized data.
Ethical approval
Institutional Review Board approval was obtained (CRM-2101-126).
Study subjects or cohorts overlap:
Approximately 200 patients are part of the population studied in the article Banaste et al, Radiology 2018; 00:1-101, https://doi.org/10.1148/radiol.2018180492.
Methodology
• retrospective
• observational
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 59 kb)
Rights and permissions
About this article
Cite this article
Didion, P., Crombé, A., Dabadie, A. et al. Emergency whole-body CT scans in pediatric patients with trauma: patterns of injuries, yield of dual-phase scanning, and influence of second read on detection of injuries. Eur Radiol 32, 8473–8484 (2022). https://doi.org/10.1007/s00330-022-08878-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08878-1