Abstract
Objectives
To compare the visibility of intracranial aneurysm wall and thickness quantification between 7 and 3 T vessel wall imaging and evaluate the association between aneurysm size and wall thickness.
Methods
Twenty-nine patients with 29 unruptured intracranial aneurysms were prospectively recruited for 3D T1-weighted vessel wall MRI at both 3 T and 7 T with 0.53 mm (3 T) and 0.4 mm (7 T) isotropic resolution, respectively. Two neuroradiologists independently evaluated wall visibility (0–5 Likert scale), quantified the apparent wall thickness (AWT) using a semi-automated full-width-half-maximum method, calculated wall sharpness, and measured the wall-to-lumen contrast ratio (CRwall/lumen).
Results
Twenty-four patients with 24 aneurysms were included in this study. 7 T achieved significantly better aneurysm wall visibility than 3 T (3.6 ± 1.1 vs 2.7 ± 0.8, p = 0.003). AWT measured on 3 T and 7 T had a good correlation (averaged r = 0.63 ± 0.19). However, AWT on 3 T was 15% thicker than that on 7 T (0.52 ± 0.07 mm vs 0.45 ± 0.05 mm, p < 0.001). Wall sharpness on 7 T was 57% higher than that on 3 T (1.95 ± 0.32 mm−1 vs 1.24 ± 0.15 mm−1, p < 0.001). CRwall/lumen on 3 T and 7 T was comparable (p = 0.424). AWT on 7 T was positively correlated with aneurysm size (saccular: r = 0.58, q = 0.046; fusiform: r = 0.67, q = 0.049).
Conclusions
7 T provides better visualization of intracranial aneurysm wall with higher sharpness than 3 T. 3 T overestimates the wall thickness relative to 7 T. Aneurysm wall thickness is positively correlated with aneurysm size. 7 T MRI is a promising tool to evaluate aneurysm wall in vivo.
Key Points
• 7 T provides better visualization of intracranial aneurysm wall with higher sharpness than 3 T.
• 3 T overestimates the wall thickness comparing with 7 T.
• Aneurysm wall thickness is positively correlated with aneurysm size.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
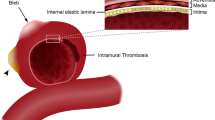
Intracranial aneurysms (IAs) are abnormal bulging of the intracranial artery wall. It occurs in approximately 3.2% [1] of the general population, and it is the most common cause of non-traumatic subarachnoid hemorrhage (SAH) [2]. The management of IAs is still controversial, and a considerable amount of small aneurysms, which are not treated endovascularly but rather monitored, rupture [3]. The development or rupture of intracranial aneurysms is characterized by pathological remodeling of the artery wall with inflammatory cell infiltration, internal elastic lamina disruption, and migration of smooth muscle cells [4]. Traditional imaging modalities such as digital subtraction angiography (DSA), computed tomography angiography (CTA), and magnetic resonance angiography (MRA) cannot provide key pathophysiological information about aneurysm vulnerability and the associated wall characteristics.
High-resolution vessel wall imaging (VWI) is playing an increasing role in the direct evaluation of the artery wall (10–12). The vast majority of studies on aneurysm VWI have used 3 T MR [5,6,7,8,9,10]. In comparison to 3 T, 7 T has higher signal-to-noise (SNR) and imaging resolution, which may provide an improved evaluation of the aneurysm wall [11,12,13,14,15]. However, direct comparison between 7 and 3 T field strengths for IA evaluation in the same patient cohort still lacks, except for a few case series (n ≤ 6) (Zhu et al [11] n = 6, Roa et al [15] n = 3). In addition, aneurysm wall thickness is a potential marker of aneurysm instability [16, 17]; however, the accuracy of 3 T and 7 T MRI for the IA wall thickness quantification has never been compared.
Our study aims to compare 3 T and 7 T for the visualization of IA wall and the quantification of wall thickness in the same cohort of patients and investigate the association between aneurysm size and wall thickness.
Materials and methods
Subjects
This study was approved by the local institutional review board (IRB). Twenty-nine consecutive patients with unruptured intracranial aneurysms were prospectively recruited from March 2016 through January 2020 to have both 3 T and 7 T vessel wall imaging on the same day. Patients with renal dysfunction, mental impairment, metal implants, and claustrophobia were excluded. If the patient only had an MRI scan in one field strength, the patient was excluded from the analysis. Written informed consent was obtained from all patients before enrollment.
Imaging protocol
All the MR examinations were performed using a 7 T magnetic resonance system (Siemens Healthineers) with Nova 32 channel head coil and a 3 T MAGNETOM Prisma MR scanner (Siemens Healthineers) equipped with a 64-channel neurovascular coil. The imaging resolution of 7 T and 3 T vessel wall MRI was 0.4 mm isotropic and 0.53 mm isotropic, respectively. Details of imaging protocols were provided in the supplemental file.
Image analysis
Image visualization and evaluation were performed on a 3D slicer (version 4.10.2, https://www.slicer.org). All images were anonymized before evaluation. MR images were independently reviewed by two experienced neuroradiologists (with 5 and 7 years of experience in neurovascular imaging, respectively) blind to patient information and magnetic field strength. The inter-reader agreement was evaluated. Aneurysms were divided into saccular and fusiform types based on morphological features. The size of the aneurysm was measured on 7 T TOF using Maximum Intensity Projection (MIP). Saccular aneurysm size was defined as maximum aneurysm height, which was measured from the midpoint of the aneurysm neck to the dome of the aneurysm. Fusiform aneurysm size was defined as the maximal luminal diameter.
The wall visibility of each aneurysm on SPACE images was graded on a qualitative scale of 0–5 as adopted from a previous publication [18]. Details of the scale and example figures were shown in the supplemental file. The ratings of image quality were based on raw data by the two neuroradiologists.
Vessel wall images of 3 T were co-registered to 7 T for each patient using the build-in rigid image registration function of the 3D slicer software. Manual adjustment was then performed when misalignment occurred. The images were interpolated to 0.1 mm for post-processing without any additional changes in image reconstruction or filtering, thus the signal intensities were unchanged. The quantitative measurements of wall thickness and sharpness were performed using in-house developed software based on Matlab (version 2017a).
Three consecutive slices through the region of the aneurysm with the largest cross-sectional area were selected (Fig. 1). The aneurysm outer wall boundary was manually drawn on vessel wall images by the two neuroradiologists. Radial lines were then automatically generated from the center of the aneurysm to the outer wall, and 16 circumferential segments were defined (Fig. 1). Profiles of signal intensity were determined across the aneurysm wall for each radial line. For each segment, apparent wall thickness (AWT) was defined as the half-width at half maximum (FWHM) of the aneurysmal wall on the signal profile (Fig. 1), which is a commonly used method for thickness measurement and can measure the sub-voxel thickness with acceptable accuracy [19, 20]. For the locations where aneurysm wall adhesive to the brain tissue, if the FWHM method couldn’t detect the outer wall edge, these locations were excluded from the analysis. The sharpness of the inner wall boundary was calculated using a previously defined method [21]. The distance, d20–80%, between 20 and 80% positions of the difference between the maximum and minimum intensity values across the profile was measured. The sharpness was defined as 1/d20–80% [21].
The calculation algorithm diagram for apparent wall thickness (AWT). Top, from left to right: Three consecutive slices through the region of the aneurysm with the largest cross-sectional area; 16 defined circumferential segments divided by 16 radial lines from the center; one representative line for the wall thickness calculation. Bottom: Signal intensity profile (the distance between two half peaks points d was defined as the thickness of this segment)
Aneurysm lumen boundary was also manually drawn to calculate the mean signal intensity of the aneurysm lumen. The wall-to-lumen contrast ratio (CRwall/lumen) was defined as [11]:
where SIwallis the average signal of the aneurysm wall, and the SIlumen is the average signal of the aneurysm lumen in the three slices.
Histological analysis was performed when the specimen was available and the protocol is shown in the supplemental file.
Statistical analysis
All data were analyzed using IBM SPSS Statistics 23. Normal-distributed data and non-normal-distributed data were expressed as mean ± standard deviation, and median [interquartile range], respectively. Categorical data were expressed as a percentile. T-test and Wilcoxon’s rank-sum test were used to compare continuous variables that were normally or not normally distributed. Pearson’s correlation was used for correlation analysis of AWT between 7 and 3 T and correlation analysis of aneurysm size and AWT. For multiple comparisons, a false discovery rate (Benjamini and Hochberg) was used to calculate the corrected p value, which was represented as the q value. The inter-observer agreement was evaluated with the intraclass correlation coefficient (ICC). q < 0.05 and p < 0.05 were considered statistically significant for multiple comparisons and non-multiple comparisons respectively.
Results
Patient and aneurysm characteristics
Twenty-nine individuals diagnosed with unruptured intracranial aneurysms (male = 13) were recruited. Five patients were excluded (2 for severe flow artifacts in the aneurysm lumen, 3 for signal loss due to susceptibility artifact from the sphenoid sinus). The final sample included 24 patients (12 male; age median, IQR 55 [46, 63]) with 24 aneurysms (15 saccular and 9 fusiform; size 7.5 ± 1.9 mm). Patient and aneurysm characteristics are presented in Table 1.
Qualitative and quantitative analysis
The comparison of 3 T and 7 T for the aneurysm wall visibility grade, sharpness, CRwall/lumen, and AWT is shown in Fig. 2.
The wall visibility grade of 7 T was greater than that of 3 T (3.6 ± 1.1 vs. 2.7 ± 0.8, p = 0.003) (Fig. 2a).The sharpness of 7 T was significantly higher than 3 T (1.95 ± 0.32 mm−1 vs 1.24 ± 0.15 mm−1, p < 0.001) (Fig. 2b), and the CRwall/lumen measurement was comparable between 7 and 3 T (2.37 [2.17, 3.31] vs. 2.74 [2.35, 3.56], p = 0.424) (Fig. 2c).
Mean AWT on 7 T was significantly smaller than that on 3 T on aneurysm-based analysis (0.45 ± 0.05 mm vs 0.52 ± 0.07 mm, p < 0.001) (Fig. 2d). When performing segment-based analysis in each aneurysm (Supplementary Fig. 2), the AWT on 7 T was significantly smaller than 3 T in 21 of 24 aneurysms. Min AWT on 7 T was also significantly smaller than that on 3 T on aneurysm-based analysis (0.30 ± 0.05 mm vs 0.34 ± 0.08 mm, p = 0.028).
The AWT range of each segment was 0.22 to 1.04 mm on 7 T and 0.18 to 1.14 mm on 3 T, respectively. AWT measurements showed good agreement between 7 and 3 T (averaged Pearson’s r in all the patients 0.63 ± 0.19) (Fig. 3).
Correlation analysis of AWT between 7 and 3 T in three cases. From top to bottom: a basilar tip aneurysm, (b) middle cerebral artery aneurysm, (c) anterior communicating artery aneurysm. From left to right: original 7 T images, original 3 T images, AWT measurement results on 7 T (numbers represent 16 defined circumferential segments), AWT measurement results on 3 T (numbers represent 16 defined circumferential segments), line plot of AWT of 16 segments from 7 T (dotted line) and 3 T (solid line), and AWT correlation plot between 7 and 3 T
Due to the higher quality and resolution of 7 T MRI, the AWT measurements on 7 T were used to evaluate the correlation of aneurysm size and wall thickness and the difference between saccular and fusiform aneurysms. Because in principle, a higher resolution helps more accurate quantification of wall thickness because of reduced partial volume effect [22]. Mean AWT of both saccular and fusiform aneurysms was positively correlated with aneurysm size (saccular r = 0.58, q = 0.046; fusiform r = 0.67, q = 0.049) (Supplementary Fig. 3). AWT of saccular aneurysms was similar to that of fusiform aneurysms (0.44 ± 0.05 mm vs 0.47 ± 0.06 mm p = 0.110). However, there was no correlation between the min AWT and the aneurysm size (r = 0.32, p = 0.127).
Histological analysis
One aneurysm specimen was harvested from an adult patient with a 7-mm anterior communicating artery aneurysm for histological analysis (Supplementary Fig. 4). The specimen was collected 1 week after the MRI scan. Immunohistochemistry demonstrated the proliferation of smooth muscle cells in the medial layer at the thickened site and infiltration of inflammatory cells. Electron microscopic analysis showed that an abundant vasa vasorum had developed at the tunica adventitia at the thickened site, some smooth muscle cells apoptosis at the thin site, and the absence of endothelial cells. MRI showed a variable AWT (0.32–0.71 mm for 7 T, 0.39–0.75 mm for 3 T). Histological analysis showed that the wall thickness was heterogeneous, and the thickness ranged from 0.27 to 0.63 mm, which was closer to the AWT measurement of 7 T than 3 T.
Measurement reproducibility
Two neuroradiologists had a good to excellent inter-observer agreement with ICCs from 0.80 to 0.93 (supplemental file).
Post hoc sample size analysis was provided in the supplemental file.
Discussion
In this study, we performed a comparison between 3 and 7 T vessel wall imaging for the evaluation of the intracranial aneurysm wall. We found 7 T images were sharper than 3 T and provided significantly better visualization of the wall. The higher resolution and better image quality at 7 T improved the wall thickness measurement, and traditional 3 T MRI would overestimate the wall thickness compared to 7 T. We also found the thicker wall was related to larger aneurysm size, which was the first study to demonstrate such correlation using in vivo quantitative imaging. To the best of our knowledge, this was the first study systematically comparing the ability of 3 T and 7 T for intracranial aneurysm wall evaluation using quantitative analysis, while previous comparison studies were only case series (n < 6) [11, 15]. Our results highlighted that 7 T MRI is a promising tool to evaluate the intracranial aneurysm wall in vivo.
Ultra-high-field 7 T MRI can be particularly beneficial for intracranial vessel wall imaging due to its high SNR and resolution [12]. The intracranial vessel wall is a very thin structure (healthy vessel wall thickness is around 0.5 mm and aneurysm wall thickness has been reported between 0.03 and 0.2 mm) [23] that required high isotropic resolution imaging for reliable visualization and quantification. However, only a few studies directly compared 3 T and 7 T for intracranial vessel wall imaging [11, 15, 24]. Harteveld et al [24] compared 3 T (1 mm isotropic) and 7 T (0.8 mm isotropic, CSF-suppressed) MRI for visualizing intracranial atherosclerotic plaques in 21 elderly asymptomatic volunteers [24]. They found 7 T detected more intracranial plaques than 3 T, but in some patients, there was disagreement, possibly due to the limited resolution in their study. For intracranial aneurysms, the comparison between 3 and 7 T was still sparse with a few case series (Zhu et al [11] n = 6, Roa et al [15] n = 3). Zhu et al [11] found 7 T provided sharper images and better image quality than 3 T in 6 aneurysms, and Roa et al [15] found 3 T and 7 T had comparable wall enhancement quantification. Neither study quantified the wall thickness. Our study agreed with Zhu et al [11] that 7 T achieved higher sharpness and better image quality.
We found 7 T had better visibility of the aneurysm wall than 3 T, and all aneurysm walls at least can be partially visualized at 7 T, and 88% (21/24) can visualize > 50% of the vessel wall. Kleinloog et al [25] evaluated 33 intracranial aneurysms using 7 T MRI with isotropic 0.8-mm resolution and found aneurysm wall was not visible in 5 aneurysms (15%). Another 1.5 T study found 29% of the aneurysms’ wall (4/14) could not be visualized using the 2D imaging method with 3 mm slice thickness [26]. The improved visibility in our 7 T MRI was possibly due to our higher resolution (0.4 mm3 vs 0.8 mm3, 1/8 of the voxel size of Kleinloog et al [25]). We did not observe significant differences between the CRwall/lumen of 3 T and 7 T, possibly because the wall-to-lumen contrast was mostly determined by the flow suppression, and we did not apply advanced blood suppression techniques [27, 28] in this study at both 3 T and 7 T.
Aneurysm wall thickness is an important pathological feature, and previous histological studies found the thick aneurysm wall was associated with atherosclerotic changes and the thin wall was associated with the reduction of smooth muscle cells, and the wall thickness was potentially related to aneurysm rupture and remolding [4, 29, 30]. Kadasi et al [16] and Jiang et al [17] further identified aneurysm wall thickness variation using intraoperative photographs. Quantification of the aneurysm wall thickness variation in vivo using MRI is promising because it is a non-invasive way for the evaluation of the pathology. Park et al [26] measured aneurysm wall thickness on 2D black-blood images with 3 mm slice thickness and reported the mean thickness at the dome and neck was 0.46 ± 0.05 mm and 0.60 ± 0.13 mm. However, 2D imaging was limited by the thick slices and partial volume effect. Blankena et al [13] measured intracranial aneurysm wall thickness on 7 T MR VWI with an isotropic resolution of 0.8 mm and corrected the partial volume effect by considering signal intensity variations and found AWT ranged from 0.07 to 0.53 mm. Compared with previous studies, the major advantage of our study was that we used the highest resolution as reported in the current literature of intracranial aneurysms (0.4-mm isotropic resolution), and thus the partial volume effect could be minimized [22]. In addition, we performed segment-based analysis and applied an objective FWHM method for the thickness quantification, which was accurate and reproducible [19]. We demonstrated that 3 T overestimated the wall thickness compared to 7 T due to the lower resolution (0.53 mm3) and highlighted the importance of high resolution in thickness quantification. However, such findings need to be confirmed in future histology validation studies.
Finally, we found AWT was positively correlated with aneurysm size, which agreed with previous histopathology studies [4, 31]. Histopathological analysis of the IAs showed that the wall of IA < 10 mm was more likely to be thin and hypocellular and lacked smooth muscle and inflammatory cells [4, 29]. On the contrary, a proliferation of smooth muscle cells and inflammatory cells often existed in larger IAs (> 10 mm) with thick walls [29]. This was the first time that this “thickness-size” relationship was demonstrated by a non-invasive imaging examination. There have been many studies linking wall thickness with aneurysm stability. Most studies showed thinning of the aneurysm wall may be an important factor for aneurysm rupture [5, 32,33,34]. One study reported that a thin portion of the aneurysm dome correlated with the point of rupture [32]. Hartman et al [33] showed that aneurysms with PHASES score > 3 were more likely to demonstrate wall thinning (9.2% vs 0%, p = 0.044). In contrast, Song et al [34] demonstrated that the translucent aneurysms were smaller in size, and the aneurysm height < 3 mm was related to wall thinning. A recent large-scale study (N = 333) [5] found thick wall enhancement was associated with IA rupture, symptoms, and growth. It needs to be noted that these results were not actually conflicting with each other, but reflecting the different concepts of wall thickness. The wall thickness within a single aneurysm is variable. A focal thinning may not reflect on the average thickness, and the aneurysm rupture normally happens on a focal point. We found minimal AWT was not correlated with aneurysm size but average AWT was. A larger study with 3D thickness mapping is required to confirm our findings.
Limitations
This study had several limitations. First, this was a single-center study, and the sample size was relatively small. Our findings need to be validated using a larger cohort. Second, in our cohort, only one patient underwent open surgery with histology analysis. Matching the location of in vivo wall thickness to histology specimen in 3D is extremely hard, and the wall thickness in vivo (under blood pressure) is different from ex vivo specimen (without pressure). Still, the evaluation of wall thickness in vivo will enrich our understanding of the pathology of intracranial aneurysms. Third, all the measurements were performed in 2D slices. A 3D thickness map of the entire aneurysm wall will provide more comprehensive information. Fourth, aneurysm wall pulsation through the cardiac cycle may lead to image blurring and signal loss, and slow flow artifacts can have a residual signal near the wall, and these factors may result in measurement error of wall thickness. Fifth, three para-clinoid aneurysms were excluded due to poor image quality from adjacent susceptibility. 7 T MR was more sensitive to tissue-air interface than 3 T, which could result in signal loss. Sixth, in this study, we did not compare the wall enhancement between 3 and 7 T, which was a surrogate marker of wall inflammation and related to aneurysm rupture, growth, and symptoms [5, 6, 35]. We are running a prospective study comparing wall enhancement between 3 and 7 T. All of the above limitations may generate study bias.
Conclusions
7 T vessel wall MRI provides better visualization of the intracranial aneurysm wall with higher sharpness compared to 3 T vessel wall MRI. 3 T also overestimates aneurysm wall thickness. Aneurysm wall thickness is positively correlated with aneurysm size. 7 T MRI is a promising tool to evaluate aneurysm wall in vivo.
Abbreviations
- AWT:
-
Apparent wall thickness
- CRwall/lumen :
-
Wall-to-lumen contrast ratio
- FWHM:
-
Half-width at half maximum
- IA:
-
Intracranial aneurysm
- MIP:
-
Maximum Intensity Projection
- VWI:
-
High-resolution vessel wall imaging
References
Vlak MHM, Algra A, Brandenburg R, Rinkel GJE (2011) Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol 10:626–636
Molyneux AJ, Kerr RS, Birks J et al (2009) Risk of recurrent subarachnoid haemorrhage, death, or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow-up. Lancet Neurol 8(5):427–33
Wang Y, Cheng M, Liu S et al (2021) Shape related features of intracranial aneurysm are associated with rupture status in a large Chinese cohort. J Neurointerv Surg. https://doi.org/10.1136/neurintsurg-2021-017452
Kataoka K, Taneda M, Asai T, Kinoshita A, Ito M, Kuroda R (1999) Structural fragility and inflammatory response of ruptured cerebral aneurysms. A comparative study between ruptured and unruptured cerebral aneurysms. Stroke 30:1396–1401
Edjlali M, Guédon A, Ben Hassen W et al (2018) Circumferential thick enhancement at vessel wall MRI has high specificity for intracranial aneurysm instability. Radiology 289:181–187
Fu Q, Wang Y, Zhang Y et al (2021) Qualitative and quantitative wall enhancement on magnetic resonance imaging is associated with symptoms of unruptured intracranial aneurysms. Stroke 52:213–222
Zhu C, Wang X, Eisenmenger L et al (2020) Wall enhancement on black-blood MRI is independently associated with symptomatic status of unruptured intracranial saccular aneurysm. Eur Radiol 30:6413–6420
Zhu C, Wang X, Eisenmenger L et al (2019) Surveillance of unruptured intracranial saccular aneurysms using noncontrast 3D-black-blood MRI: comparison of 3D-TOF and contrast-enhanced MRA with 3D-DSA. AJNR Am J Neuroradiol 40:960–966
Tian B, Toossi S, Eisenmenger L et al (2019) Visualizing wall enhancement over time in unruptured intracranial aneurysms using 3D vessel wall imaging. J Magn Reson Imaging 50:193–200
Wang X, Zhu C, Leng Y, Degnan AJ, Lu J (2019) Intracranial aneurysm wall enhancement associated with aneurysm rupture: a systematic review and meta-analysis. Acad Radiol 26:664–673
Zhu C, Haraldsson H, Tian B et al (2016) High resolution imaging of the intracranial vessel wall at 3 and 7 T using 3D fast spin echo MRI. MAGMA 29:559–570
Rutland JW, Delman BN, Gill CM, Zhu C, Shrivastava RK, Balchandani P (2020) Emerging use of ultra-high-field 7T MRI in the study of intracranial vascularity: state of the field and future directions. AJNR Am J Neuroradiol 41:2–9
Blankena R, Kleinloog R, Verweij BH et al (2016) Thinner regions of intracranial aneurysm wall correlate with regions of higher wall shear stress: a 7T MRI study. AJNR Am J Neuroradiol 37:1310–1317
Liu X, Zhang Z, Zhu C et al (2020) Wall enhancement of intracranial saccular and fusiform aneurysms may differ in intensity and extension: a pilot study using 7-T high-resolution black-blood MRI. Eur Radiol 30:301–307
Roa JA, Zanaty M, Osorno-Cruz C et al (2020) Objective quantification of contrast enhancement of unruptured intracranial aneurysms: a high-resolution vessel wall imaging validation study. J Neurosurg. https://doi.org/10.3171/2019.12.Jns192746:1-8
Kadasi LM, Dent WC, Malek AM (2013) Colocalization of thin-walled dome regions with low hemodynamic wall shear stress in unruptured cerebral aneurysms Clinical article. J Neurosurg 119:172–179
Jiang P, Liu Q, Wu J, Chen X, Wang S (2019) Hemodynamic characteristics associated with thinner regions of intracranial aneurysm wall. J Clin Neurosci 67:185–190
Tian B, Toossi S, Eisenmenger L et al (2018) Visualizing wall enhancement over time in unruptured intracranial aneurysms using 3D vessel wall imaging. J Magn Reson Imaging. https://doi.org/10.1002/jmri.26553
Mikami Y, Kolman L, Joncas SX et al (2014) Accuracy and reproducibility of semi-automated late gadolinium enhancement quantification techniques in patients with hypertrophic cardiomyopathy. J Cardiovasc Magn Reson 16:85
Song Y, Hamtaei E, Sethi SK, Yang G, Xie H, Mark Haacke E (2017) COnstrained Data Extrapolation (CODE): a new approach for high definition vascular imaging from low resolution data. Magn Reson Imaging 44:111–118
Larson AC, Kellman P, Arai A et al (2005) Preliminary investigation of respiratory self-gating for free-breathing segmented cine MRI. Magn Reson Med 53:159–168
Qiao Y, Steinman DA, Qin Q et al (2011) Intracranial arterial wall imaging using three-dimensional high isotropic resolution black blood MRI at 3.0 Tesla. J Magn Reson Imaging 34:22–30
Isaksen JG, Bazilevs Y, Kvamsdal T et al (2008) Determination of wall tension in cerebral artery aneurysms by numerical simulation. Stroke 39:3172–3178
Harteveld AA, van der Kolk AG, van der Worp HB et al (2017) High-resolution intracranial vessel wall MRI in an elderly asymptomatic population: comparison of 3T and 7T. Eur Radiol 27:1585–1595
Kleinloog R, Korkmaz E, Zwanenburg JJ et al (2014) Visualization of the aneurysm wall: a 7.0-Tesla magnetic resonance imaging study. Neurosurgery 75:614–622 (discussion 622)
Park JK, Lee CS, Sim KB, Huh JS, Park JC (2009) Imaging of the walls of saccular cerebral aneurysms with double inversion recovery black-blood sequence. J Magn Reson Imaging 30:1179–1183
Zhu C, Cao L, Wen Z et al (2019) Surveillance of abdominal aortic aneurysm using accelerated 3D non-contrast black-blood cardiovascular magnetic resonance with compressed sensing (CS-DANTE-SPACE). J Cardiovasc Magn Reson 21:66
Zhu C, Graves MJ, Yuan J, Sadat U, Gillard JH, Patterson AJ (2014) Optimization of improved motion-sensitized driven-equilibrium (iMSDE) blood suppression for carotid artery wall imaging. J Cardiovasc Magn Reson 16:61
Meng H, Tutino VM, Xiang J, Siddiqui A (2014) High WSS or low WSS? Complex interactions of hemodynamics with intracranial aneurysm initiation, growth, and rupture: toward a unifying hypothesis. AJNR Am J Neuroradiol 35:1254–1262
Kataoka K, Taneda M, Asai T, Yamada Y (2000) Difference in nature of ruptured and unruptured cerebral aneurysms. Lancet 355:203
Mizoi K, Yoshimoto T, Nagamine Y (1996) Types of unruptured cerebral aneurysms reviewed from operation video-recordings. Acta Neurochir (Wien) 138:965–969
Asari S, Ohmoto T (1994) Growth and rupture of unruptured cerebral aneurysms based on the intraoperative appearance. Acta Med Okayama 48:257–262
Hartman JB, Watase H, Sun J et al (2019) Intracranial aneurysms at higher clinical risk for rupture demonstrate increased wall enhancement and thinning on multicontrast 3D vessel wall MRI. Br J Radiol 92:20180950
Song J, Park JE, Kim HR, Shin YS (2015) Observation of cerebral aneurysm wall thickness using intraoperative microscopy: clinical and morphological analysis of translucent aneurysm. Neurol Sci 36:907–912
Zhu C, Wang X, Degnan AJ et al (2018) Wall enhancement of intracranial unruptured aneurysm is associated with increased rupture risk and traditional risk factors. Eur Radiol 28:5019–5026
Acknowledgements
We thank Dr. Jing An (Siemens Shenzhen Magnetic Resonance Ltd) for her effort on MRI technical support. We sincerely thank all the patients and health care workers who participated in this study.
Funding
This study has received funding by the National Natural Science Foundation of China (82001804, 81901197), the Natural Science Foundation of Beijing Municipality (7191003), the Ministry of Science and Technology of China (2019YFA0707103), and the Chinese Academy of Sciences (XDB32010300). Chengcheng Zhu is supported by the US National Institutes of Health (NIH) grant R00HL136883.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Youxiang Li.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in “Wall enhancement of intracranial saccular and fusiform aneurysms may differ in intensity and extension: a pilot study using 7-T high-resolution black-blood MRI. Eur Radiol 2020;30(1):301–307” and “Quantitative analysis of unruptured intracranial aneurysm wall thickness and enhancement using 7 T high-resolution, black-blood magnetic resonance imaging. J NeuroIntervent Surg 2021;0:1–7.”
Methodology
• Prospective
• Observational
• Performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Feng, J., Liu, X., Zhang, Z. et al. Comparison of 7 T and 3 T vessel wall MRI for the evaluation of intracranial aneurysm wall. Eur Radiol 32, 2384–2392 (2022). https://doi.org/10.1007/s00330-021-08331-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08331-9