Abstract
Objectives
Magnetic resonance enterography (MRE) and ultrasound (US) can be used to diagnose inflammatory bowel diseases (IBD) in children. This meta-analysis aimed to determine the diagnostic performance of MRE and US in pediatric patients with IBD.
Methods
PubMed, Embase, and the Cochrane Library were searched for eligible studies published up to June 1, 2020. The outcomes were the performances of MRE and US at the segment and patient levels. Pooled sensitivity, specificity, positive and negative likelihood ratios (PLR and NLR), diagnostic odds ratio (DOR), and the area under the summary receiver operating characteristic curves value (SROC) were analyzed.
Results
Eight studies (340 children) were included. Compared with the reference standard, MRE showed pooled sensitivity of 93.0% (95% confidence interval (CI): 90.0–95.4%), specificity of 94.6% (95% CI: 92.1–96.5%), PLR of 11.146 (95% CI: 5.027–24.713), NLR of 0.094 (95% CI: 0.057–0.155), and DOR of 134.21 (95% CI: 40.72–442.29), with a SROC of 0.9721. Similar results were observed at the patient and segment levels. Compared with the reference standard, US had pooled sensitivity of 84.1% (95% CI: 69.9–93.4%), specificity of 82.9% (95% CI: 66.4–93.4%), PLR of 4.924 (95% CI: 2.351–10.310), NLR of 0.207 (95% CI: 0.103–0.413), and DOR of 25.919 (95% CI: 7.63–88.07), but only two studies were included. US (reader 1) had a similar diagnostic value to US (reader 2).
Conclusions
The present meta-analysis shows that MRE has good performance in detecting IBD in pediatric patients. Only two studies used US, and additional studies are necessary to confirm the diagnostic performance of US for IBD in children.
Key Points
• MRE has good performance in the detection of IBD in pediatric patients.
• Similar results were observed at the patient and segment levels for MRE.
• Only two studies were included for US, without differentiating patient/segment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) is a chronic inflammatory, multisystem disorder, mainly affecting the gastrointestinal tract, more typically the small bowel (especially ileum) or colon [1,2,3]. Ulcerative colitis (UC) is a chronic colonic inflammatory disease with proximal extension from the rectum but without small bowel involvement [1,2,3,4]. About 20–30% of patients with CD are diagnosed during childhood [1, 3], but children can suffer from CD, with an incidence of 0.3–9.2 per 100,000 children worldwide [3]. The reported incidence of UC is 0.2–6.7 per 100,000 children in North America and Europe [3, 5]. Children with CD or UC are at risk of intestinal and abdominal complications, macronutrient and micronutrient deficiency, poor bone health, anemia, and impaired growth [1,2,3, 6, 7]. The management of pediatric CD involves drugs and sometimes surgeries [1,2,3, 7].
The diagnosis of inflammatory bowel disease (IBD) in children is based on symptoms, bloodwork, stool tests, endoscopy, and imaging [1,2,3, 7]. Ultrasound (US) is a screening tool in the preliminary diagnostic workup of suspected IBD in children, but more sensitive imaging modalities are required for the small bowel [2]. US allows the visualization of bowel thickness, strictures, fistulae, abscesses, and inflammation of the mesentery [3]. The benefits of US include excellent images of the bowel wall, no exposure to ionizing radiations, widely available, well-tolerated, and low cost [3]. US limitations include operator dependency, high interobserver variability, and difficulty distinguishing or visualizing the entire gastrointestinal tract, including the proximal ileum, jejunum, transverse colon, and rectum [2, 3, 7]. Magnetic resonance enterography (MRE) is an imaging technique using magnetic resonance imaging (MRI) with oral intraluminal contrast and intravenous gadolinium [8]. It is the imaging modality of choice in diagnosing pediatric inflammatory bowel disease [1,2,3]. MRE is preferred over computed tomography (CT) and fluoroscopy due to the lack of ionizing radiation exposure and high diagnostic accuracy [2, 9]. MRE can detect small intestinal involvements, inflammatory changes in the intestinal wall, and fibrosis/inflammation (but it is difficult for MRE to differentiate fibrosis and inflammation clearly) and help identify disease complications (fistula, abscess, stenosis) at diagnosis [2, 3]. MRE can determine the degree of intestinal inflammation and damage, but there is no validated scoring system in children [2]. The limitations of MRE include motion artifacts, difficulties in tolerating oral contrast, high cost, and limited availability compared to other imaging modalities [3].
Because children are more sensitive than adults to ionizing radiation, MRE and US are the methods of choice for the diagnosis and subsequent management of pediatric IBD [2]. A previous meta-analysis showed that MRE has high diagnostic performance in children, especially at the per-patient level [10]. Another meta-analysis showed that capsule endoscopy, MRE, and US all had similar diagnostic yields for small bowel CD [11]. On the other hand, a systematic review suggested that the diagnostic accuracy of US for pediatric IBD was inconclusive [12].
Even though these analyses are recent (2017–2019) [10,11,12], new evidence has been published that could provide new light on the diagnostic accuracy of MRE and US for IBD in children. In addition, Kopylov et al. [11] included only studies on CD, but it is known that CD and UC can be difficult to differentiate in children [1,2,3,4], which could lead to bias. Therefore, this meta-analysis aimed to determine the diagnostic performance of MRE and US in pediatric patients with IBD.
Materials and methods
Literature search
This meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines [13]. Since no original clinical raw data was collected or used, ethical approval was not requested for this meta-analysis.
The eligibility criteria were as follows: (1) pediatric (definition according to each included study but could vary among studies) patients with suspected or known IBD (only IBD, irrespective of fistula or stage); (2) use of MRE or US for diagnosis; (3) the reported data could be used to construct at least one 2 × 2 table for test performance; (4) prospective studies; (5) full text published in English.
PubMed, Embase, and the Cochrane Library were searched for studies published up to June 1, 2020, using the Medical Subject Headings (MeSH) terms “Inflammatory Bowel Diseases”, “Crohn Disease”, “Colitis, Ulcerative”, “Child”, “Ultrasonography”, and “Magnetic resonance enterography”, as well as relevant keywords.
Data extraction and quality assessment
The potentially relevant publications were screened and evaluated by two reviewers (Lili He and Qiong Yao) double-blindly, with a third reviewer (Yinghua Sun) being invited to resolve any disagreement. A structured data collection form was developed. Two researchers (Lili He and Qiong Yao) independently extracted the data, including authors, year of publication, country, sample size, age, percentage of males, included patients, study aim, the standard of reference, magnet strength or probe frequency, diagnostic criteria, and data for diagnostic performance. The studies were evaluated according to the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool [12].
Statistical analysis
All analyses were performed using MetaDiSc 1.4 (Unit of Clinical Biostatistics, Ramon y Cajal Hospital, Madrid, Spain). Pooled sensitivity, specificity, positive and negative likelihood ratios (PLR and NLR), diagnostic odds ratio (DOR), and the area under the summary receiver operating characteristic curves value (SROC) were combined for statistical analysis. Statistical heterogeneity was evaluated using the chi-square test and the I2 index. An I2 index > 50% and Q-test p < 0.10 indicated high heterogeneity, and the random-effects model was used; otherwise, the fixed-effects model was used [14]. p values < 0.05 were considered statistically significant. Potential publication bias analysis was not performed because < 10 studies were included in each meta-analysis [14].
Results
Selection of the studies
Figure 1 presents the study selection process. Initially, 155 articles were retrieved from the three databases and 121 articles were left after removing the duplicates. Twenty-three articles were excluded based on the report type, and 98 full-text papers were assessed for eligibility. Eighteen were excluded because of study aim/design, 34 because of the population, 13 because MRE or US was not used for diagnosis, 20 because the reported data could be used to construct at least one 2 × 2 table for test performance, and five for not being published in English. Therefore, eight studies were included in the present meta-analysis (Table 1).
This meta-analysis included 340 children. All patients had either suspected, diagnosed, known, or histologically proven IBD. All eight studies used MRE for diagnosis, and two used US. The studies were from Europe [15, 18,19,20, 22] and the USA [16, 17, 21]. The reference diagnostic standard was histology [16, 17, 19, 22] or a comprehensive diagnosis based on history, clinical parameters, imaging, and/or histology [15, 18, 20, 21].
The QUADAS-2 tool showed that all studies had low risks of biases, except for Gee et al. [16], Quencer et al. [17], and Tsai et al. [21], for an uncertain risk of patient selection bias, and Gee et al. [16], for an uncertain risk of flow timing bias (Table 2).
Overall performance of MRE
All eight studies [15,16,17,18,19,20,21,22] could be included for the analysis of MRE overall performance (irrespective of per-patient/per-segment level). Compared with the reference standard, MRE showed a pooled sensitivity of 93.0% (95% confidence interval (CI): 90.0–95.4%; I2 = 29.2%, pheterogeneity = 0.195), pooled specificity of 94.6% (95% CI: 92.1–96.5%; I2 = 66.0%, pheterogeneity = 0.004), pooled PLR of 11.146 (95% CI: 5.027–24.713; I2 = 71.9%, pheterogeneity = 0.001), pooled NLR of 0.094 (95% CI: 0.057–0.155; I2 = 35.9%, pheterogeneity = 0.142), and pooled DOR of 134.21 (95% CI: 40.72–442.29; I2 = 68.0%, pheterogeneity = 0.003), with a SROC of 0.9721 (Fig. 2).
Overall performance of magnetic resonance enterography (MRE). a Pooled sensitivity. b Pooled specificity. c Pooled positive likelihood ratio (PLR). d Pooled diagnostic likelihood ratio (DLR). e Overall diagnostic odds ratio (DOR). f The area under the summary receiver operating characteristic curves value (SROC).
Performance of MRE at the patient level
Five studies [15, 19,20,21,22] could be included for the analysis of MRE performance at the patient level. Compared with the reference standard, MRE had a pooled sensitivity of 93.2% (95% CI: 87.8–96.7%; I2 = 48.2%, pheterogeneity = 0.102), pooled specificity of 95.4% (95% CI: 89.5–98.5%; I2 = 13.9%, pheterogeneity = 0.325), pooled PLR of 13.187 (95% CI: 6.116–28.434; I2 = 0.0%, pheterogeneity = 0.471), pooled NLR of 0.087 (95% CI: 0.036–0.207; I2 = 45.5%, pheterogeneity = 0.119), and pooled DOR of 181.87 (95% CI: 39.81–380.85; I2 = 40.1%, pheterogeneity = 0.154), with a SROC of 0.9778 (Fig. 3).
Performance of magnetic resonance enterography (MRE) at the patient level. a Pooled sensitivity. b Pooled specificity. c Pooled positive likelihood ratio (PLR). d Pooled diagnostic likelihood ratio (DLR). e Overall diagnostic odds ratio (DOR). f The area under the summary receiver operating characteristic curves value (SROC).
Performance of MRE at the segment level
Three studies [16,17,18] could be included for the analysis of the MRE performance at the segment level (duodenum, jejunum, ileum, ascending colon, transverse colon, descending colon, and rectum). Compared with the reference standard, MRE had a pooled sensitivity of 93% (95% CI: 89–96%; I2 = 7.0%, pheterogeneity = 0.341), pooled specificity of 94% (95% CI: 91–97%; I2 = 87.3%, pheterogeneity < 0.001), pooled PLR of 8.72 (95% CI: 2.14–35.44; I2 = 90.5%, pheterogeneity < 0.001), pooled NLR of 0.09 (95% CI: 0.05–0.19; I2 = 50.6%, pheterogeneity = 0.132), and pooled DOR of 89.71 (95% CI: 11.41–705.63; I2 = 86.9%, pheterogeneity < 0.001), with a SROC of 0.9718 (Fig. 4).
Performance of magnetic resonance enterography (MRE) at the segment level. a Pooled sensitivity. b Pooled specificity. c Pooled positive likelihood ratio (PLR). d Pooled negative likelihood ratio (NLR). e Overall diagnostic odds ratio (DOR). f The area under the summary receiver operating characteristic curves value (SROC).
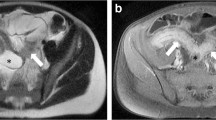
Performance of US
Two studies [20, 21] could be included for the analysis of US (reader 2) overall performance. Compared with the reference standard, US had a pooled sensitivity of 84.1% (95% CI: 69.9–93.4%; I2 = 0.0%, pheterogeneity = 0.319), pooled specificity of 82.9% (95% CI: 66.4–93.4%; I2 = 0.0%, pheterogeneity = 0.939), pooled PLR of 4.924 (95% CI: 2.351–10.310; I2 = 0.0%, pheterogeneity = 0.806), pooled NLR of 0.207 (95% CI: 0.103–0.413; I2 = 0.0%, pheterogeneity = 0.328), and pooled DOR of 25.919 (95% CI: 7.63–88.07; I2 = 0.0%, pheterogeneity = 0.463). US (reader 1) (Fig. 5) had a lower pooled diagnostic value of 15.26 (95% CI 2.32–100.33; I2 = 60.7%, pheterogeneity = 0.111) than US (reader 2) (Fig. 6).
Discussion
This meta-analysis aimed to determine the diagnostic performance of MRE and US in pediatric patients with IBD. The results suggest that both MRE (at the patient and segment levels) and US (irrespective of the reader) have good performance in detecting IBD in pediatric patients.
Yoon et al. [10] completed a meta-analysis of 18 studies (687 patients) to determine the diagnostic accuracy of MRE. They included any type of study that examined this issue, while the present study included only studies from which a 2 × 2 table could be built, explaining the smaller number of studies in the present meta-analysis, which only included prospective studies. Still, compared with Yoon et al. [10], the present meta-analysis captured one recent paper [22] and one older one [17]. Yoon et al. [10] reported a lower sensitivity (83%) than in the present meta-analysis (93%) but similar specificity (93% and 95%). They observed that the scanner manufacturer influenced the diagnostic value of MRE, but this could not be examined in the present study because of the small number of studies included and a too-large variety of scanners. Nevertheless, the sensitivity and specificity reported here are a little higher than what was reported before (80–88% sensitivity and 81–90% specificity) for MRE for the diagnosis of IBD in children [23, 24], which could be due to the technological improvements in scanners and software, increased experience and awareness of the radiologists, and the inclusion of prospective studies only.
Another factor that could improve sensitivity and specificity is the relatively recent popularization of the use of diffusion-weighted imaging (DWI) [25], in which a restricted diffusion indicates active inflammation [26, 27]. The meta-analysis by Yoon et al. [10] observed that DWI influenced their results, but this could not be observed here because DWI was not always used, or it was not always clear whether DWI was included among the MRE examinations or not. In addition, only one study performed a comparison of MRE with vs. without DWI for IBD. It warrants further studies.
In the present study, the pooled sensitivity and specificity of US were 84% and 83%, respectively, which are lower than in two previous meta-analyses in adults by Fraquelli et al. [28] (88% and 93%) and by Dong et al. [29] (88% and 97%). The variations in diagnostic value could be due to the gold standard being used.
A recent meta-analysis directly compared capsule endoscopy, MRE, and US to determine bowel inflammation and reported no significant differences in diagnostic yield among the three modalities [11]. It is supported by van Wassenaert et al. [12], who could not conclude that US was better than MRE for IBD diagnosis. Nevertheless, in the present study, the sensitivity and specificity of US were lower than that of MRE, but the small number of studies prevented any direct comparison. Future studies will have to examine this. Nevertheless, current guidelines support the use of all three modalities for IBD diagnosis [30]. The examinations in IBD aim to determine the characteristics of the disease, to monitor the mucosal response to treatments, and identify complications as early as possible [31,32,33,34,35], emphasizing the role of imaging in the detection of small bowel IBD, aiding the distinction between CD and UC, and defining disease extent. Nevertheless, MRE and US have different advantages and disadvantages, making the two modalities complementary. Indeed, the two modalities are ionizing radiation-free. US can display the bowel wall but cannot visualize the entire gastrointestinal tract [2, 3, 7]. On the other hand, MRE has difficulty distinguishing fibrosis from inflammation but can display the entire gastrointestinal tract [2, 3]. In addition, US is recommended as the first-line examination, followed by a complementary one, like MRE [2]. Therefore, those non-invasive, highly accurate, and radiation-free examinations can be used in children with IBD, which are important characteristics because they are likely to undergo re-examination several times in their lifetime.
Meta-analyses should always be considered in relation to their limitations. Heterogeneity is an issue in meta-analyses [14] and was observed for some of the measurements analyzed here, including overall MRE specificity, PLR, and DOR. There was no uniformity in the gold standard used in the different studies. The small number of included studies prevented the analysis of the publication bias and the analysis of the factors that could influence the diagnostic value of MRE for IBD in children. This meta-analysis excluded conference abstracts; including them might have increased the sample size and allowed the publication bias analysis, but the data extracted from conference abstracts are limited, and constructing 2 × 2 would probably have been impossible. Nevertheless, the PRISMA principle [13] and the meta-analysis principles [14] were rigorously applied. Three of the eight included studies presented an uncertain risk of bias for patient selection. The DOR for MRE was very large because of the small numbers of false-negative in Casciani et al. [15] and the small numbers of false-positive in Tsai et al. [21]. Therefore, for these two studies, statistics were necessary to calculate the DOR. Finally, only two studies of US could be included.
In conclusion, the present meta-analysis determined that MRE has good performance in detecting IBD in pediatric patients. Only two studies used US for the diagnosis of IBD in children, and additional studies are necessary.
Abbreviations
- CD:
-
Crohn disease
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- DOR:
-
Diagnostic odds ratio
- DWI:
-
Diffusion-weighted imaging
- IBD:
-
Inflammatory bowel diseases
- MRE:
-
Magnetic resonance enterography
- MRI:
-
Magnetic resonance imaging
- PLR and NLR:
-
Pooled sensitivity, specificity, positive and negative likelihood ratios
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QUADAS-2:
-
Quality Assessment of Diagnostic Accuracy Studies
- SROC:
-
Summary receiver operating characteristic curves value
- UC:
-
Ulcerative colitis
- US:
-
Ultrasound
References
Conrad MA, Rosh JR (2017) Pediatric inflammatory bowel disease. Pediatr Clin North Am 64:577–591
Levine A, Koletzko S, Turner D et al (2014) ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr 58:795–806
Oliveira SB, Monteiro IM (2017) Diagnosis and management of inflammatory bowel disease in children. BMJ 357:j2083
Stenke E, Hussey S (2014) Ulcerative colitis: management in adults, children and young people (NICE Clinical Guideline CG166). Arch Dis Child Educ Pract Ed 99:194–197
Turner D, Levine A, Escher JC et al (2012) Management of pediatric ulcerative colitis: joint ECCO and ESPGHAN evidence-based consensus guidelines. J Pediatr Gastroenterol Nutr 55:340–361
Gasparetto M, Guariso G (2014) Crohn ' s disease and growth deficiency in children and adolescents. World J Gastroenterol 20:13219–13233
Gomollon F, Dignass A, Annese V et al (2017) 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn ' s Disease 2016: Part 1: Diagnosis and Medical Management. J Crohns Colitis 11:3–25
Rabizadeh S, Dubinsky M (2013) Update in pediatric inflammatory bowel disease. Rheum Dis Clin North Am 39:789–799
Giles E, Barclay AR, Chippington S, Wilson DC (2013) Systematic review: MRI enterography for assessment of small bowel involvement in paediatric Crohn ' s disease. Aliment Pharmacol Ther 37:1121–1131
Yoon HM, Suh CH, Kim JR et al (2017) Diagnostic performance of magnetic resonance enterography for detection of active inflammation in children and adolescents with inflammatory bowel disease: a systematic review and diagnostic meta-analysis. JAMA Pediatr 171:1208–1216
Kopylov U, Yung DE, Engel T et al (2017) Diagnostic yield of capsule endoscopy versus magnetic resonance enterography and small bowel contrast ultrasound in the evaluation of small bowel Crohn ' s disease: systematic review and meta-analysis. Dig Liver Dis 49:854–863
van Wassenaer EA, de Voogd FAE, van Rijn RR et al (2019) Diagnostic accuracy of transabdominal ultrasound in detecting intestinal inflammation in paediatric IBD patients-a systematic review. J Crohns Colitis 13:1501–1509
Selcuk AA (2019) A guide for systematic reviews: PRISMA. Turk Arch Otorhinolaryngol 57:57–58
Higgins JPT, Thomas J, Chandler J et al (2019) Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane Collaboration, London
Casciani E, Masselli G, Di Nardo G et al (2011) MR enterography versus capsule endoscopy in paediatric patients with suspected Crohn ' s disease. Eur Radiol 21:823–831
Gee MS, Nimkin K, Hsu M et al (2011) Prospective evaluation of MR enterography as the primary imaging modality for pediatric Crohn disease assessment. AJR Am J Roentgenol 197:224–231
Quencer KB, Nimkin K, Mino-Kenudson M, Gee MS (2013) Detecting active inflammation and fibrosis in pediatric Crohn ' s disease: prospective evaluation of MR-E and CT-E. Abdom Imaging 38:705–713
Maccioni F, Al Ansari N, Mazzamurro F et al (2014) Detection of Crohn disease lesions of the small and large bowel in pediatric patients: diagnostic value of MR enterography versus reference examinations. AJR Am J Roentgenol 203:W533–W542
Dubron C, Avni F, Boutry N, Turck D, Duhamel A, Amzallag-Bellenger E (2016) Prospective evaluation of free-breathing diffusion-weighted imaging for the detection of inflammatory bowel disease with MR enterography in childhood population. Br J Radiol 89:20150840
Oliva S, Cucchiara S, Civitelli F et al (2016) Colon capsule endoscopy compared with other modalities in the evaluation of pediatric Crohn ' s disease of the small bowel and colon. Gastrointest Endosc 83:975–983
Tsai TL, Marine MB, Wanner MR et al (2017) Can ultrasound be used as the primary imaging in children with suspected Crohn disease? Pediatr Radiol 47:917–923
Masselli G, De Vincentiis C, Aloi M et al (2019) Detection of Crohn ' s disease with diffusion images versus contrast-enhanced images in pediatric using MR enterography with histopathological correlation. Radiol Med 124:1306–1314
Church PC, Turner D, Feldman BM et al (2015) Systematic review with meta-analysis: magnetic resonance enterography signs for the detection of inflammation and intestinal damage in Crohn ' s disease. Aliment Pharmacol Ther 41:153–166
Ahmed O, Rodrigues DM, Nguyen GC (2016) Magnetic resonance imaging of the small bowel in Crohn ' s disease: a systematic review and meta-analysis. Can J Gastroenterol Hepatol 2016:7857352
Park SH (2016) DWI at MR enterography for evaluating bowel inflammation in Crohn disease. AJR Am J Roentgenol 207:40–48
Mollard BJ, Smith EA, Dillman JR (2015) Pediatric MR enterography: technique and approach to interpretation-how we do it. Radiology 274:29–43
Ream JM, Dillman JR, Adler J et al (2013) MRI diffusion-weighted imaging (DWI) in pediatric small bowel Crohn disease: correlation with MRI findings of active bowel wall inflammation. Pediatr Radiol 43:1077–1085
Fraquelli M, Colli A, Casazza G et al (2005) Role of US in detection of Crohn disease: meta-analysis. Radiology 236:95–101
Dong J, Wang H, Zhao J et al (2014) Ultrasound as a diagnostic tool in detecting active Crohn ' s disease: a meta-analysis of prospective studies. Eur Radiol 24:26–33
Pennazio M, Spada C, Eliakim R et al (2015) Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 47:352–376
Greener T, Klang E, Yablecovitch D et al (2016) The impact of magnetic resonance enterography and capsule endoscopy on the re-classification of disease in patients with known Crohn ' s disease: a prospective Israeli IBD Research Nucleus (IIRN) Study. J Crohns Colitis 10:525–531
Kopylov U, Yablecovitch D, Lahat A et al (2015) Detection of small bowel mucosal healing and deep remission in patients with known small bowel Crohn ' s disease using biomarkers, capsule endoscopy, and imaging. Am J Gastroenterol 110:1316–1323
Kopylov U, Nemeth A, Koulaouzidis A et al (2015) Small bowel capsule endoscopy in the management of established Crohn ' s disease: clinical impact, safety, and correlation with inflammatory biomarkers. Inflamm Bowel Dis 21:93–100
Kopylov U, Ben-Horin S, Seidman EG, Eliakim R (2015) Video capsule endoscopy of the small bowel for monitoring of Crohn ' s disease. Inflamm Bowel Dis 21:2726–2735
Danese S, Fiorino G, Fernandes C, Peyrin-Biroulet L (2014) Catching the therapeutic window of opportunity in early Crohn ' s disease. Curr Drug Targets 15:1056–1063
Funding
This study has received funding by the General Program of Shanghai Municipal Commission of Health and Family Planning (201640070) to Xihong Hu.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Qiong Yao.
Conflict of interest
The authors declare no competing interests.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Not applicable in this study
Ethical approval
Institutional Review Board approval was not required because it’s meta-analysis.
Methodology
• This meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
He, L., Sun, Y., Hu, X. et al. Diagnostic performance of magnetic resonance enterography and ultrasound in children with inflammatory bowel diseases: a diagnostic test accuracy meta-analysis. Eur Radiol 32, 1330–1341 (2022). https://doi.org/10.1007/s00330-021-08172-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08172-6