Abstract
Objectives
To explore differences in the clinical management of men and women in the 5 years after detecting a solitary pulmonary nodule (SPN) by chest radiograph or CT in routine clinical practice.
Methods
We followed up 545 men and 347 women with an SPN detected by chest radiograph or CT in a retrospective cohort of 25,422 individuals undergoing routine thoracic imaging in 2010–2011. We compared the frequency of each management strategy (no further test, immediate intervention or follow up) according to sex by means of chi-squared. We estimated the relative risk of women versus men of having been followed up instead of an immediate intervention using multivariate logistic regression. We compared by sex the time between detection of the nodule and lung cancer diagnosis, the time between diagnosis and death by means of Mann-Whitney U test and the cumulative effective dose of radiation in each management strategy by means of t test.
Results
Women were more likely than men to have follow-up rather than immediate intervention (aRR = 1.8, CI 1.3–2.7, p = 0.002), particularly in those who underwent CT (aRR = 4.2, CI 1.9–9.3, p < 0.001). The median time between SPN detection and lung cancer diagnosis was higher in women (4.2 months, interquartile range (IQR) 5.1) than in men (1.5 months, IQR 16.2). The mean cumulative effective dose was 21.3 mSv, 19.4 mSv in men and 23.9mv in women (p = 0.023).
Conclusions
Our results could reflect decisions based on a greater suspicion of lung cancer in men. The incidental detection of SPNs is increasing, and it is necessary to establish clear strategies aimed to reduce variability in their management according to patient’s sex.
Key Points
• After incidental finding of SPN, women were less likely to receive an immediate intervention.
• Accumulative radiation was higher in women than in men.
• Our results could reflect decisions based on a greater suspicion of lung cancer in men.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Solitary pulmonary nodules (SPNs), frequently detected during clinical practice by chest radiograph and CT [1], are clinically important as they may potentially represent malignancy. Several SPN and patient characteristics have been identified as lung cancer risk factors. Regarding patient characteristics, studies have shown that risk is higher for increasing age, female sex, a current or prior history of smoking, a family history of lung cancer and previous malignancy [2]. The majority of SPN are benign, but they can also represent an important opportunity for early detection of lung cancer. How to manage SPN remains controversial [3], and decisions can sometimes be based on clinician’s preferences rather than based on evidence. It is also possible that management differs between male and female patients.
Lung cancer has traditionally been considered as a male disease due to the higher smoking habit among men. Over the past 40 years, lung cancer incidence and mortality among males have declined, while a decrease among women has only recently been observed [4]. Nevertheless, most of the current evidence in lung cancer has been derived from the period where men reached the majority of the lung cancer cases, and we cannot translate the pattern of lung cancer in men to women [5]. Some studies have shown a better lung cancer prognosis among women, mainly in those with adenocarcinoma histology [5, 6], suggesting that the natural history of lung cancer may differ in women and men due to the different histologic types or hormonal factors [7]. In fact, previous studies have shown a more pronounced association between particular genotypes and lung cancer risk in women [8]. It is worth noting that non-smoking women appear to be two to three timed more at risk for developing lung cancer than non- smoking men [9, 10].
Even though female sex has been identified as risk factor, only the British Thoracic Society (BTS) [11] guidelines and the Brock University Model [12] have considered it. In addition, the studies about management of SPNs have not explored the potential differences in clinical decision-making if the patient is male or female. Recently, we showed that women whose SPNs were detected by a chest radiograph in routine clinical practice were less likely to have an immediate intervention than men, but the limited follow-up prevented and in-depth analysis [13]. Evidence also points out differences in treatment between men and women with lung cancer; these studies showed that women were less likely than men to receive timely surgical resection and that radiation therapy is more frequently administered to men than women [14]. A different management in men and women could have important consequences for health, such as different delays in diagnosis, overuse or underuse of clinical interventions and survival, among others.
Therefore, the aim of this study was to explore if there were differences in the clinical management of men and women in the 5 years following detection of an SPN by a thoracic imaging test carried out in routine clinical practice.
Materials and methods
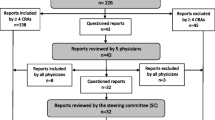
In order to explore differences in the clinical management strategy after SPN detection in clinical practice while undergoing CT or chest radiograph for any reason, 545 men and 347 women with an SPN were included in the analysis. This population formed part of a study that recruited 25,422 consecutive patients undergoing thoracic imaging in two National Health hospitals in the Valencian Community (Spain) in 2010 and 2011, which has been described elsewhere [1, 15]. In brief, the two hospitals recruited all patients referred to the radiology department from other hospital services and those referrals from primary health care centres. Patients previously diagnosed with lung cancer were excluded. SPNs were detected in 893 out of the originally included 25,422 patients and they were followed for 5 years. For the purpose of this study, we excluded one patient who died before characterisation of the SPN was completed.
We obtained Institutional Review Board approval (University Miguel Hernandez Committee Ref DSP-BLL-001-10). The institutional board exempted the study to ask for informed consent.
Data collection
Eight expert radiologists (all of whom had more than 10 years of experience) working in the radiology department of each hospital determined the presence and characteristics of the SPNs. Details of the procedure have been previously described [1].
Using a predesign form, the radiologists described nodule characteristics: (a) size: in mms and categorised according to Fleischner guidelines; (b) nodule shape (smooth, lobular, spiculated or other irregular type); (c) location (upper, middle or lower lobe); and (d) for those patients who underwent a CT, nodule consistency (solid, partly solid, ground glass, calcification or not specified). Inter- and intra-observer agreement was evaluated [1].
Selected variables were collected from the electronic medical record for men and women: age, type of imaging test by which the SPN was detected, reason for requesting imaging test, smoking status, previous cancer, chronic obstructive pulmonary disease (COPD).
All imaging tests carried out to characterise the nodule were collected from digital medical registers for 60 months after the detection of the nodule. As previously described [16], we classified patients according to management strategy into the following:
-
a)
Immediate intervention: any study performed within a 3-month window following SPN identification.
-
b)
Follow-up: any imaging study performed from 3 to 12 months after SPN detection.
-
c)
No further testing (no follow-up in the 12 months following SPN detection). Imaging tests performed the same day of SPN identification were considered tests for the characterisation of SPN.
We estimated the cumulative effective dose of diagnostics procedures in the study population according to previous evidence [17, 18]: chest radiograph (0.1 mSv), CT (7 mSv), PET/CT (25 mSv), lung perfusion (2 mSv) and lung ventilation (0.5 mSv).
Statistical analysis
We computerised and checked all data to discard errors. All analyses were carried out with Stata/SE 15 (StataCorp. LLC).
We performed a descriptive analysis of patients and SPN characteristics in order to describe the frequency of relevant clinical characteristics in men and women. Disaggregating data by type of imaging test, we compared the frequency of each management strategy according to sex. We used t test and chi-squared test to compare data between women and men. The p value level chosen to determine significance was established to be 0.05. We estimated the relative risk of women versus men of having been followed up instead of having an immediate intervention using multivariable logistic regression (the model included only predictors that reached statistical significance p < 0.05).
In patients diagnosed with lung cancer, we compared the time between detection of the nodule and lung cancer diagnosis by sex, and for those who died during the study, we estimated time from lung cancer diagnosis to death. Results were presented as median and interquartile range and compared by sex using Mann-Whitney U test.
We compared the mean cumulative effective dose of radiation by sex in each management strategy, disaggregating data by type of imaging test used when the SPN was detected, by means of t test.
Results
The population included more men (n = 545, 61.1%) than women (n = 347, 38.9%). Men were older than women (41% of men and 32.9% of women were older than 70 years, p value = 0.022), they had more frequently been previously diagnosed of COPD (33.7% of men and 16.4% of women, p value ≤ 0.001) and presented a tobacco habit (former or current) more often than women (62.9% versus 52.7%, p value = 0.003). Similarly, a higher proportion of SPN found in men were larger (65.6% larger than 8 mm vs 53%, p value = 0.006), had spiculated borders (17.2% vs 6.1%, p value ≤ 0.001) and were located in the upper lobe (54.1% vs 48.1%, p value = 0.093), than those found in women. The most frequent reason for requesting imaging test was for non-respiratory reasons (27.7%) in women and for extrapulmonary neoplasm in men (24%), although there was no statistical significance between men and women regarding the reasons for requesting imaging test (p value = 0.130). 34.7% of men and 29.7% of women presented previous malignancy (no statistical significance, p value = 0.140).
There were differences between the imaging test carried out when the SPN was detected: for 479 patients (52.4% of the men and 56.1% of the women with an SPN) as the first imaging test where the SPN was observed had been a chest radiograph, while for 413 of the patients (47.6% of the men and 46.9% of the women with an SPN), the initial imaging test was a CT (p value = 0.261) (Table 1).
Diagnostic pathways in men and women (Table 2)
After detection of an SPN, 235 (26.3%) patients had immediate interventions, 343 (38.5%) patients were followed up and 314 (35.2%) patients did not have further tests.
Men had immediate interventions more frequently than women (29% versus 22.2%, p = 0.028). Women were more likely to be followed up than men (43.2% vs 35.4%, p = 0.025). Conservative clinical decision (no further testing) was similar for both men and women (35.6% and 34.6%, p = 0.757).
According to the initial test by which SPN was detected, there were differences in the management strategy between men and women. In those patients with SPN detected on by CT, men were more likely to have immediate testing than women (n = 60, 23% versus n = 11, 7.2% p < 0.001), while women were followed up more frequently than men (n = 89, 58.6% versus n = 100, 38.3%, p < 0.001). There were no differences between men (32.8% followed up and 35.5% immediate testing) and women (31.3% followed up and 33.8% immediate testing) in the clinical management strategy of patients with an SPN detected by chest radiograph (p value = 0.884).
In multivariate analysis adjusted by patients’ sociodemographic (age, smoking status and COPD diagnosis) and clinical characteristics (SPN diameter, localisation and border), women were more likely than men to have follow-up than immediate intervention (RR = 1.8, CI 1.3–2.7, p = 0.002). In patients with an SPN detected by chest radiograph, there was no statistically significant difference between men and women (RR = 1.2, CI 0.7–1.9, p = 0.482). In patients with an SPN detected by CT, women were also more likely than men to be followed up (RR = 4.2; CI 1.9–9.3, p < 0.001) than to undergo immediate intervention.
Time between SPN detection, lung cancer diagnosis and death
Thirty-five women and 97 men were diagnosed of lung cancer. The median time between SPN detection and lung cancer diagnosis was higher in women (4.2 months, IQR 5.1) than in men (1.5 months, IQR 16.2), although this difference was not statistically significant.
In patients with an SPN detected by chest radiograph, the time from detection to diagnosis was 2.2 (IQR 8) months in men and 2.7 (IQR 13.4) months in women, while in patients with an SPN detected by CT, it was 1.1 (IQR 3.6) months for men and 5.8 (IQR 19.1) months for women.
In patients with lung cancer diagnosis who died, the time between diagnosis and death was 21.1 (IQR 35.6) months for men and 17.3 (IQR14.5) months for women, among patients with an SPN detected by chest radiograph, and 5.4 (IQR 11.6) months for men and 7.5 (IQR 17.4) months for women, among patients with an SPN detected by CT.
Exposure to radiation (Table 3)
The total mean effective dose during the study period was 21.3 mSv (95% CI 19.1 to 23.4), 19.4 mSv (95% CI 16.9 to 22) in men and 23.9 (95% CI 20.2 to 27.7) in women (p = 0.023). In patients with SPNs detected by CT, the mean effective dose was 27.3 mSV (95% CI 24 to 30.5), which was higher for women (31.4 mSV, 95% CI 25.9 to 36.9) than for men (24.5 mSv, 95% CI 20.5 to 28.4; p = 0.044). In those patients with SPN detected by chest radiograph, the mean effective dose was 16.5 mSV (18.1 mSv (95% CI 13.2 to 23) for women and 15.5 mSv (12.2 to 18.7) for men, p = 0.378). No differences were detected when comparing effective dose between men and women according to the SPN management strategy: mean effective dose in patients who had been followed up was 26.8 mSv (95% CI 22.9 to 30.6) in men and 31.1 mSv (95% CI 26.1 to 36.1) in women (p value = 0.174); 8.4 mSv (95% CI 7.1 to 9.7) in men and 7.4 mSv (95% CI 6.1 to 10.7) in women immediate testing (p value = 0.516).
Discussion
To our knowledge, this is the first study to evaluate different clinical management strategies in women and men after detecting an SPN in a routine clinical setting. In our cohort, regardless of clinical and SPN characteristics, women were less likely than men to receive an immediate intervention. As a result of the different clinical management strategies for men and women, accumulative radiation was higher in women than in men. Additionally, the time between SPN detection and lung cancer diagnosis was longer in women than in men, and the time between lung cancer diagnosis and death was shorter in women.
Women, particularly those whose SPNs were detected by CT, were more likely than men to be followed up rather than having an immediate intervention. Our results could reflect decisions based on differing suspicion of lung cancer associated with the higher frequency of lung cancer in men, rather than decisions based on evidence and clinical guidelines. Even though previous studies have not explored the potential influence of patients’ sex in SPN management, there is great deal of evidence regarding differential diagnostic procedures in women and men. A diagnostic delay among women has been observed in as many as seven hundred different diseases [19] and sadly, it is no surprise that an SPN detected in a women could be subjected to a different management strategy than an SPN in a man, even if it reflects a subconscious bias by the managing clinician.
Although clinical and radiographic risk factors for SPN malignancy are well described, little is known about factors that influence the clinical management strategy undertaken. In the last years, several guidelines for the management of SPN have been developed [11, 12, 16, 20, 21]. These guidelines base their recommendations mainly on the risk or probability of lung cancer considering age, smoking habit, COPD and SPN characteristics (size, border, consistency), but only the guidelines of the BTS recognise female sex as a risk factor. Remarkably, although BTS guidelines state that an SPN is a predictor of malignancy in women, the diagnostic strategy in our population was more aggressive in men. It is worth noting that previous studies found that a significant number of clinicians were unaware of SPN management guidelines, resulting in an excess of invasive procedures in patients with a benign nodule [22].
Previous studies have raised concerns regarding the application of guidelines and how clinicians use clinical factors to choose the most appropriate management strategy for individual patients [23]. In this sense, they have described cases of prolonged surveillance and exposure to unneeded radiation [24,25,26]. In our study, the management strategies in men and women resulted in a greater number of imaging tests and a higher radiation exposure in women (cumulative risk of cancer). Although we were not able to evaluate it, a long period of follow-up could also lead to more emotional harms in women.
The longer time between SPN detection and lung cancer diagnosis in women could be a consequence of the different management strategies applied to women, although the limited sample size impeded further exploration into these differences. In a previous analysis of our cohort, we showed that although the adjusted risk of lung cancer was higher among men compared with that among women overall, in patients with SPN detected by imaging test, the difference between men and women was not statistically significant in lung cancer diagnosis, nor mortality [27]. There is concern that delays in lung cancer diagnosis may contribute to a high frequency of advanced disease at the definitive presentation [28]. A longer diagnostic time could have led to worse outcomes, but in our study, we were not able to register the cancer stage at diagnosis [29].
The study has some limitations. It uses existing data obtained from routine clinical records, and consequently we were forced to limit the analysis to available data, meaning that potentially relevant information could not be included, like pathological findings.
Given that it was impossible to get individual machine parameters for all imaging tests, we estimated the associated radiation effective dose per test accordingly using previously published evidence [18]. This quantification method has been proposed for instance by the Dose-Data Med project [30]. Although this type of estimation has inherent limitations, it does not take into account the test date, the scanner model or the patient’s characteristics; it does not affect the overall result. Another limitation could be observer variability in the determination of the presence of an SPN and its characteristics. However, we minimised this potential limitation by the use of similar criteria for detection and description of SPNs and by the assessment of the observer agreement [1]. Our results are based on a limited number of SPNs and diagnosis of lung cancer and should therefore be interpreted with caution. Nevertheless, our study is the first to analyse differences in SPN management strategies in women and men, which can result in a diagnostic delay in women and a greater exposure to further diagnostic tests and their associated radiation.
Even though we were not able to evaluate the inappropriateness of immediate testing in men or follow-up strategy in women, our results led us to deduce that decisions could be influenced by clinician unconscious bias. The results observed in our cohort are in line with the evidence that suggests knowledge regarding signs and symptoms, diagnosis, treatment and prognosis in women is inferior for several diseases. This is especially relevant for diseases considered typically masculine—including lung cancer. The belief that there is a lower probability of lung cancer in women appears to result in different clinical management strategies in women and men after SPN detection, even if the SPN characteristics are the same. More immediate strategies in men are adopted while women undergo long follow-up periods and a higher number of subsequent imaging tests. In conclusion, the main contribution of this study is the analysis of SPN management strategies by patient sex in a clinical setting, and the fact that the differences observed between sexes cannot be explained by clinical or SPN characteristics. As the growing use of imaging tests increases the incidental detection of SPNs, it becomes more necessary to establish clear strategies to avoid unnecessary testing, and reduce variability in the management of SPNs according to sex.
Abbreviations
- BTS:
-
British Thoracic Society
- COPD:
-
Chronic obstructive pulmonary disease
- CT:
-
Computed tomography
- IQR:
-
Interquartile range
- mSV:
-
Millisievert
- PET/TC:
-
Positron emission tomography–computed tomography
- RR:
-
Relative risk
- SPN:
-
Solitary pulmonary nodule
References
Gomez-Saez N, Gonzalez-Alvarez I, Vilar J et al (2014) Prevalence and variables associated with solitary pulmonary nodules in a routine clinic-based population: a cross-sectional study. Eur Radiol 24:2174–2182
Naidich DP, Bankier AA, MacMahon H et al (2013) Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 266(1):304–317
Cruickshank A, Stieler G, Ameer F (2019) Evaluation of the solitary pulmonary nodule. Intern Med J 49(3):306–315
SEER Cancer Statistics (2019) Factsheets lung and bronchus cancer. National Cancer Institute, Bethesda. Available via http://seer.cancer.gov/statfacts/html/lungb.html. Accessed 5 June 2019
Morgan LC, Grayson D, Peters HE, Clarke CW, Peters MJ (2000) Lung cancer in New South Wales: current trends and the influence of age and sex. Med J Aust 172(12):578–582
Micheli A, Ciampichini R, Oberaigner W et al (2009) The advantage of women in cancer survival: an analysis of EUROCARE-4 data. Eur J Cancer 45(6):1017–1027
Skuladottir H, Olsen JH (2006) Can reproductive pattern explain better survival of women with lung cancer? Acta Oncol 45(1):47–53
Shi Q, Zhang Z, Li G et al (2005) Sex differences in risk of lung cancer associated with methylene-tetrahydrofolate reductase polymorphisms. Cancer Epidemiol Biomarkers Prev 14(6):1477–1484
Kovalchik SA, De Matteis S, Landi MT et al (2013) A regression model for risk difference estimation in population-based case-control studies clarifies gender differences in lung cancer risk of smokers and never smokers. BMC Med Res Methodol 13:143. https://doi.org/10.1186/1471-2288-13-143
Stiles BM, Rahouma M, Hussein MK et al (2018) Never smokers with resected lung cancer: different demographics, similar survival. Eur J Cardiothorac Surg 53(4):842–848
Baldwin DR, Callister ME (2015) The British Thoracic Society guidelines on the investigation and management of pulmonary nodules. Thorax 70(8):794–798
Chung K, Mets OM, Gerke PK et al (2018) Brock malignancy risk calculator for pulmonary nodules: validation outside a lung cancer screening population. Thorax 73(9):857–863
Lumbreras B, Vilar J, Gonzalez-Alvarez I et al (2016) The fate of patients with solitary pulmonary nodules: clinical management and radiation exposure associated. PLoS One 11(7):e0158458. https://doi.org/10.1371/journal.pone.0158458
Yorio JT, Yan J, Xie Y, Gerber DE (2012) Socioeconomic disparities in lung cancer treatment and outcomes persist within a single academic medical center. Clin Lung Cancer 13(6):448–457
Gomez-Saez N, Hernandez-Aguado I, Vilar J et al (2015) Lung cancer risk and cancer-specific mortality in subjects undergoing routine imaging test when stratified with and without identified lung nodule on imaging study. Eur Radiol 25(12):3518–3527
Nair A, Devaraj A, Callister MEJ, Baldwin DR (2018) The Fleischner Society 2017 and British Thoracic Society 2015 guidelines for managing pulmonary nodules: keep calm and carry on. Thorax 73:806–812
Mettler FA Jr, Huda W, Yoshizumi TT, Mahesh M (2008) Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology 248(1):254–263
Vilar-Palop J, Vilar J, Hernandez-Aguado I, Gonzalez-Alvarez I, Lumbreras B (2016) Updated effective doses in radiology. J Radiol Prot 36(4):975–990
Westergaard D, Moseley P, Sorup FKH, Baldi P, Brunak S (2019) Population-wide analysis of differences in disease progression patterns in men and women. Nat Commun 10(1):666
Gould MK, Donington J, Lynch WR et al (2013) Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143(5 Suppl):e93S–e120S
Wood DE (2015) National Comprehensive Cancer Network (NCCN) clinical practice guidelines for lung cancer screening. Thorac Surg Clin 25(2):185–197
Wiener RS, Gould MK, Slatore CG, Fincke BG, Schwartz LM, Woloshin S (2014) Resource use and guideline concordance in evaluation of pulmonary nodules for cancer: too much and too little care. JAMA Intern Med 174(6):871–880
Vachani A, Tanner NT, Aggarwal J et al (2014) Factors that influence physician decision making for indeterminate pulmonary nodules. Ann Am Thorac Soc 11(10):1586–1591
Slatore CG, Press N, Au DH, Curtis JR, Wiener RS, Ganzini L (2013) What the heck is a “nodule”? A qualitative study of veterans with pulmonary nodules. Ann Am Thorac Soc 10(4):330–335
Wiener RS, Gould MK, Woloshin S, Schwartz LM, Clark JA (2015) ‘The thing is not knowing’: patients’ perspectives on surveillance of an indeterminate pulmonary nodule. Health Expect 18(3):355–365
Wiener RS, Gould MK, Woloshin S, Schwartz LM, Clark JA (2013) What do you mean, a spot?: a qualitative analysis of patients' reactions to discussions with their physicians about pulmonary nodules. Chest 143(3):672–677
Chilet-Rosell E, Parker LA, Hernández-Aguado I et al (2019) The determinants of lung cancer after detecting a solitary pulmonary nodule are different in men and women, for both chest radiograph and CT. PLoS One 14:e0221134–e0221134
Salomaa E-R, Sällinen S, Hiekkanen H, Liippo K (2005) Delays in the diagnosis and treatment of lung cancer. Chest 128(4):2282–2288
Risberg T, Sorbye SW, Norum J, Wist EA (1996) Diagnostic delay causes more psychological distress in female than in male cancer patients. Anticancer Res 16(2):995–999
European Commission (EC) (2014) Medical radiation exposure of the European population. Radiation protection Report 180
Acknowledgements
We acknowledge the assistance of Jessica Gorlin for language editing in the preparation of this manuscript.
Funding
This study has received funding from the Centro de investigación en red en Epidemiología y Salud Pública, (CIBERESP) (grant number CB06/02/0008 (Grupo 26 CIBERESP)).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Blanca Lumbreras.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was not required for this study because given that the study uses only routine data and no additional interventions, informed consent was not sought from the patients. Patient’s identification code numbers were de-identified by replacing the original code number with a new random code number.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in:
Lumbreras B, Vilar J, González-Álvarez I, Gómez-Sáez N, Domingo ML, et al (2016). The fate of patients with solitary pulmonary nodules: clinical management and radiation exposure associated. PLOS ONE 11(7): e0158458. doi: https://doi.org/10.1371/journal.pone.0158458
2.Gómez-Sáez N, Hernández-Aguado I, Vilar J. et al Lung cancer risk and cancer-specific mortality in subjects undergoing routine imaging test when stratified with and without identified lung nodule on imaging study. Eur Radiol 2015; 25: 3518. doi.org/10.1007/s00330-015-3775-3
Gómez-Sáez N, González-Álvarez I, Vilar J et al Prevalence and variables associated with solitary pulmonary nodules in a routine clinic-based population: a cross sectional study. Eur Radiol. 2014; 4: 2174–82. doi: https://doi.org/10.1007/s00330-014-3249-z.
Chilet-Rosell E, Parker LA, Hernández-Aguado I, Pastor-Valero M, Vilar J, González-Álvarez I, Salinas-Serrano JM, Lorente-Fernández F, Domingo ML, Lumbreras B. The determinants of lung cancer after detecting a solitary pulmonary nodule are different in men and women, for both chest radiograph and CT. PLoS One. 2019 Sep 11;14(9):e0221134. doi: https://doi.org/10.1371/journal.pone.0221134.
Methodology
• Retrospective
• Observational
• Multicentre study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 49 kb)
Rights and permissions
About this article
Cite this article
Chilet-Rosell, E., Parker, L.A., Hernández-Aguado, I. et al. Differences in the clinical management of women and men after detection of a solitary pulmonary nodule in clinical practice. Eur Radiol 30, 4390–4397 (2020). https://doi.org/10.1007/s00330-020-06791-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06791-z