Abstract
Objectives
In the ascending aorta, calcification density was independently and inversely associated with cardiovascular disease (CVD) risk prediction. Until now, the density of thoracic aorta calcium (TAC) was estimated as the Agatston score divided by the calcium area (DAG). We thought to analyze TAC density in a full Hounsfield unit (HU) range and to study its association with TAC volume, traditional risk factors, and CVD events.
Methods
Non-enhanced CT images of 1426 patients at intermediate risk were retrospectively reviewed. A calcium density score was estimated as the average of the maximum HU attenuation in all calcified plaques of the entire thoracic aorta (DAV).
Results
During a mean 4.0 years follow-up, there were 26 events for a total of 674 patients with TAC > 0. TAC volume and DAV were positively correlated (R = 0.72). The median DAV value was 457 HU (IQ 323–603 HU) and was exponentially related to DAG (R = 0.86). DAV was inversely associated with systolic pressure (p < 0.05), pulse pressure (p < 0.01), hypertension (p < 0.05), and 10-year FRS (p < 0.001) after adjusting for TAC volume. When TAC volume and DAV were included in a logistic model, a significant improvement was shown in CVD risk estimation beyond coronary artery calcium (CAC) (AUC = 0.768 vs 0.814, p < 0.05). In multivariable Cox models, TAC volume and DAV showed an independent association with CVD.
Conclusions
In intermediate risk patients, TAC density was inversely associated with several risk factors after adjustment for TAC volume. A significant improvement was observed over CAC when TAC volume and density were added into the risk prediction model.
Key Points
• Calcifications in the aorta can be non-invasively assessed using CT images
• A higher calcium score is associated with a higher cardiovascular risk
• Measuring the calcifications size and the density separately can improve the risk prediction
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery calcium (CAC) is accepted as a strong predictor of cardiovascular disease (CVD) events [1, 2]. Although less studied, thoracic aorta calcification (TAC) detected in the visible parts of the thoracic aorta during CAC examination was also associated with CVD events and death [3,4,5]. The quantification of CAC and TAC using the Agatston score (AS) is based on the size of lesions positively weighted by a categorical factor of the calcium density [6]. Recently, the separation of calcium volume and density from the AS showed that the CAC volume was positively associated with occurrence of CVD when CAC density was inversely related to such occurrence [7]. This result was assumed to be related to the lower vulnerability of very dense calcified plaques of coronary artery lesions [8, 9]. The negative relation between CAC density and CVD risk was further extended recently to the thoracic aorta [10, 11]. Although calcifications in the ascending thoracic aorta are infrequent, when present, the risk of CVD events is elevated when the calcium volume increases and when the density drops [11]. Nevertheless, the incorporation of the TAC volume and density of calcifications of the ascending aorta to the model did not provide a significant improvement in CVD risk prediction over CAC. Two limitations were mentioned to explain this lack of improvement. First, the proposed calculation of density was approximated because it is based on the estimation of the simple ratio AS over the calcium area, giving a value within a limited range from 1 to 4 [8]. Second, the very frequent calcifications of the aortic arch were not taken into account due to insufficient aorta coverage in these studies, which were mainly focused on CAC [12, 13].
In the present work, the main objective was to calculate a calcium density score in a continuous HU scale and to study its association with the full calcium volume of the whole thoracic aorta, with traditional risk factors and with CVD events after taking the CAC score into account.
Methods
Study subjects
All study subjects were recruited in the same unit of the Hôpital Européen Georges Pompidou (Paris, France) over 3 years between 2009 and 2012. In this Cardiovascular Preventive Medicine unit, all consecutive primary prevention patients at intermediate risk for cardiovascular disease undergone an extended non-enhanced multislice computed tomography (MSCT) scan for CAC assessment in view of cardiovascular risk stratification program according to the current guidelines [14]. Thus, only subjects with at least one traditional risk factor and free of clinical overt CVD were likely to be included in the present study. All subjects accepting a voluntary monitoring follow-up program of their cardiovascular status every 6 months were included in the present study (n = 1426). Participants without TAC at baseline (n = 495) as well as patients that did not come to their first follow-up consultation at 6 months (n = 193) or because of the absence of full follow-up until the end of 2015 (n = 64) were excluded from this follow-up analysis. A diagram with the final patient group is shown in Fig. 1. In January 2016, the clinical history of all the remaining included patients (n = 674) was revised by an expert (AS) using the hospital database to look for documented presence or absence of occurrence of CV event.
Blood pressure, hypertension, cholesterol, and blood glucose were determined as described elsewhere [12, 14]. The Framingham risk score (FRS) was calculated in all subjects after recalibration for the French population. Patients during their hospitalization were informed of the use of their medical data for research purposes and all the institution received authorization from the National Commission for Informatics and Freedom after checking that the researches carried out was in accordance with the Helsinki Declaration.
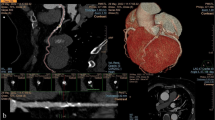
Image acquisition
All prospective ECG-gated non-enhanced images of the heart and of the thoracic aorta were obtained in the same breath hold with a 64-MSCT (Light-speed VCT; GE Health care) from the top of the aortic arch to the level of the diaphragm [12]. Acquisitions were performed at 120 kVp, with tube current adapted to the patient weight. All images were reconstructed with a thickness of 2.5 mm and a field of view of 250 mm before being analyzed using a custom software designed in our laboratory and previously used to detect and calculate the size and position of calcifications in the thoracic aorta (TA) [12, 14, 15]. As previously assessed, the effective radiation dose of our acquisition protocol was 1.23 ± 0.14 mSv (range 0.92–2.1 mSv) [14]. All measurements were made by the same expert, blinded to clinical parameters.
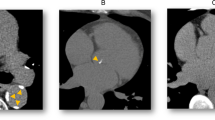
TA calcification assessment
A single automated algorithm developed by biomedical engineers in the Favaloro University was employed to segment the TA and to calculate the calcium scores. Details about the segmentation process can be found in previous reports [12, 14, 16]. Briefly, the algorithm extracted a list of ≈ 150 centerline points of the TA with the corresponding diameters, detected and quantified the aortic calcifications. The area in mm2 and the maximum attenuation values in HU (maxHU) were assessed for each lesion to calculate the calcium scores:
The Agatston score of a lesion was calculated using a categorical weighted value from 1-to-4 depending on the maxHU obtained in each calcification (1 = 130–199 HU, 2 = 200–299 HU, 3 = 300–399 HU, and 4 ≥ 400 HU) multiplied by the lesion area. For each participant, the TAC Agatston score was calculated as the sum of the detected lesions scores.
The TAC volume score was calculated as the lesion area multiplied by the slice thickness (2.5 mm). For each participant, the TAC volume score was calculated as the sum of all the detected lesions scores
The raw TAC density score (DAV) was calculated as the average of the maxHU values of all the detected lesions: DAV = mean (maxHU). For comparison purposes, a categorical density score (DAG) employed in the MESA study reports [8] was calculated as the TAC Agatston score divided by the sum of calcifications area. Whereas DAV values result in a continuous HU range, DAG values are restricted from 1-to-4.
Statistical analysis
Histograms of the TAC volume and density scores were constructed and box-plots indicating the median, interquartile range (IQ), and 10th-to-90th percentiles were calculated. Calcium scores were log-transformed (lnVolume and lnDensity) to reduce skewness and linear associations between them were evaluated with a Pearson correlation. The association of the TAC density scores (DAV and DAG) was evaluated using an exponential regression model.
Patients with and without CVD events were compared using a t test (p threshold < 0.05). Two multivariable linear regressions models were performed to evaluate the associations of several exposure variables with TAC volume and density scores as the outcome variables after adjustment for age, BSA, and male gender. For regression analyses, β-coefficients for continuous variables were expressed per SD change in the exposure variables. In a third multivariable linear regression, the TAC density model was further adjusted for TAC volume score.
Four logistic models were calculated to evaluate the association of incident CVD events with calcium scores, accounting for 10-year FRS. Model 1 only included lnCAC score as a cofactor. In models 2 and 3, lnTAC Agatston or lnTACVolume scores were incorporated. Model 4 included lnCAC, lnTAC volume, and lnDensity scores. Odds ratio were expressed per 1-SD change in the exposure variables. The area under the receiver operating characteristic curve (AUC) and the 95th confidence intervals (CI) were calculated for each model. The incremental value of each variable across the models for the prediction of CVD events was evaluated by the increase in the AUC [17].
Finally, Cox proportional hazard regression was used to estimate hazard ratios (HRs) for time to CVD events for both lnTACVolume and lnTACdensity scores adjusted for 10-year FRS and lnCAC score. HRs were expressed per 1-SD change in the covariates. All statistical calculations were performed with JMP 10 software (SAS institute) or MedCalc (version 14).
Results
Patients with and without CVD events
Demographics, clinical characteristics, and aortic measurements of the study participants are shown in Table 1. The mean follow-up was 4.0 ± 0.8 years (range 2.3–6.2 years). The 26 identified patients with CVD events were as follows: 11 with occurrence of CAD treated with stents and optimal medical treatment, 12 with arterial diseases that have benefited from surgery and/or interventional procedure aortic disease, 1 heart failure, 2 patients with occurrence of symptomatic brain vascular disease (1 ischemic attack and 1 vertebro-basilar insufficiency). FRS, CAC score, TAC Agatston score, and TAC volume score at baseline were higher in patients with CVD events than those without (all p < 0.001 except p < 0.01 for FRS). The TAC density score DAV was not different between groups (p = 0.36).
Histograms of TAC volume and density
The distribution of TAC volume and density scores is shown in Fig. 2. The median volume score value was 159 mm3 (IQ 48–500 mm3). The median DAV value was 457 HU (IQ 323–603 HU). Sixty-one percent of the patients had a density score above 400 HU. Patients with higher volume of TA calcium showed also higher density values (R = 0.72, Fig. 3). Most of patients with CV events relied below the TAC volume vs DAV regression line (n = 19 of 26, 73%). The relationship between the continuous (DAV) and categorical (DAG) density estimations showed an exponential association (R = 0.86, p < 0.001, Fig. 1 in supplementary material).
Association of TAC volume and density with risk factors
Both TAC volume and density scores were positively associated with age (β = 0.1100/years, p < 0.001, R = 0.48 and β = 0.0185/years, p < 0.001, R = 0.33 for lnTACVolume and lnTACDensity, respectively). TAC density score was inversely associated with male gender (6.08 ± 0.41 vs 6.18 ± 0.44, p < 0.001) and BSA (β = − 0.2404/m2, p < 0.01, R = 0.14). Associations between TAC volume and density scores with several exposure variables are shown in Table 2. Thus, TAC volume score was positively associated with pulse pressure (p < 0.01), hypertension (p < 0.01), hypertensive therapy (p < 0.001), lipid-lowering therapy (p < 0.001), current smoking (p < 0.001), highly correlated to CAC score (R = 0.56, p < 0.001), and negatively associated with LDL cholesterol (p < 0.05). In contrast, TAC density score was only positively associated with lipid-lowering therapy (p < 0.001), current smoking (p < 0.05), and CAC score (p < 0.001). However, after adjustment for TAC volume (Table 3), such TAC density DAV was inversely associated with systolic pressure (p < 0.05), pulse pressure (p < 0.01), hypertension (p < 0.05), and 10-year FRS (p < 0.001). Furthermore, TAC density score was positively associated with total and HDL cholesterol (p < 0.05).
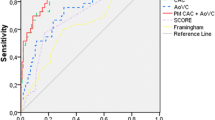
Association of TAC volume and density with CVD events
Logistic regression models combining CAC and TAC scores to predict CVD events are shown in Table 4. The base model 1 using CAC Agatston score resulted in an AUC of 0.768 (0.734–0.800). When either the TAC volume or TAC density scores were separately added to the initial model 1, AUCs increased to 0.786 (0.754–0.817) and 0.769 (0.735–0.801), respectively, but these increments did not reach significance. Only when TAC volume and density scores were both included into the basic model, the AUC increased significantly to 0.814 (0.782–0.842) (p < 0.05). As shown in Table 5, in the Cox regression model adjusted for 10-year FRS and lnCAC score, the lnTACVolume was a high significant predictor of CVD event with HR of 2.42 (95% CI 1.31 to 4.36; p < 0.01), whereas each SD increase in lnTACdensity was significantly associated with a 51% reduction (HR 0.49; 95% CI 0.27 to 0.93; p < 0.05).
Discussion
In our study, we found that when both the volume and density of TAC were incorporated with the CAC score in a logistic model, the prediction of the CV risk improved with respect to using CAC alone. In multivariable Cox models, both TAC volume and density scores showed an independent association with time to CVD events beyond CAC. Our results reinforce the idea that quantifying calcium throughout the entire thoracic aorta can add information complementary to CAC [13].
Our work shows that the relationships between systolic blood pressure, pulse pressure, presence of hypertension, and 10-year FRS were positively related to the TAC volume and negatively related to the TAC density after adjusting for calcification volume. Thus, this latter finding suggests that in presence of calcification along the thoracic aorta, beyond the volume, the density of such calcification is negatively related to some conventional cardiovascular risk factors (Table 3). This is in line with a recent study that estimated TAC density in the ascending aorta and showed that, even if the ascending TAC was uncommon, the density of the ascending aorta calcifications was negatively and independently associated with CHD and CVD after adjustment for CAC volume [11]. Other prospective studies comparing volume and density on CAC showed that CAC density was inversely related to CHD and CVD risk at any level of CAC volume and that many CVD risk factors, including male gender, diabetes, BMI, and non-Hispanic white race, were also inversely associated with CAC density score after adjustment for CAC volume [7]. More importantly, a risk model including the CAC volume score and the CAC density score as separate cofactors was more predictive than the use of the Agatston CAC score as a single factor, providing the highest correct reclassification [8, 9].
At the coronary artery site, the influence of the density of calcifications on CV risk prediction may be explained by the fact that a low density in atheromatous plaques within the arterial wall may reflect a greater vulnerability of such plaques [18]. At the aortic level, the hypothesis that can be proposed might not the same. Since arterial stiffening is directly related to blood pressure and age [19], it was not surprising to see that TAC volume was directly related to hypertension. The inverse relationship between density and both systolic and pulse pressure levels suggests that TAC volume and TAC density exert a differential effect on arterial hemodynamics.
In our study, the lipid-lowering therapy and the current smoking status were positively associated with both TAC volume and density, but this association was not statistically significant when DAV was adjusted for TAC volume. The positive association between lipid-lowering therapy and TAC density in the univariate model (Table 2) might be driven by the strong volume-density relation (Fig. 3). Some studies have shown that statins may increase calcified coronary plaques [20, 21] but the effect on aortic calcification was not reported. Since our population consists of intermediate-risk patients, statins are intensively prescribed to patients at higher risk and it might be a major confounding factor. Since the HCT treatment is a better marker of lipid disease than LDL in our patients, it is not surprising that this treatment was positively related to the TAC volume. Recent reports have shown that CAC and TAC incidence and progression shared similar determinants and both CAC and TAC increase under statin intake, supporting the hypothesis of a plaque-stabilizing effect [22, 23]. Our adjusted regression model has shown that TAC density was not associated with lipid-lowering therapy after accounting for TAC volume [10]. The same effect was observed in smoking patients. Smokers might have more density and volume of calcium because of the pro-atherosclerotic effect of tobacco on the arterial wall, but further studies including TAC volume and density progression in smokers and patients on statins are needed to confirm these results.
Strength and limitations of the study
To our knowledge, our study is the first to report a raw TAC density score where the calcifications volume and density scores were independently quantified. Calcium density score DAG was typically estimated as the quotient between the Agatston score and the calcium area, where a residual linear dependence with calcium area could not be completely disregarded. Until now, no other density estimations have been informed, probably because the size and the attenuation intensities were not registered for each calcification. Even if the 4-point scale categories adopted in the Agatston method would be insufficient to characterize the intensity of the TA calcified lesions, a linear correlation with the categorical estimation was still observed in our results (R = 0.77, p < 0.001). This association might partially justify the use of the DAG as a surrogate of DAV. Measurement of calcifications done along the whole thoracic aorta pathway with inclusion of the aortic arc is another strength of our study, together with the possibility of accounting for precise geometric descriptors of the aorta [15].
The first limitation to mention is the observational and retrospective nature of the study, together with the lack of measurement of the density of coronary calcification. Since our study was based on previous automated measurements of thoracic aorta geometry and calcium, automated detection and calcium quantification of coronary lesions were not included in our software and CAC score could not be separated into calcium volume and density. Due to the spatial resolution of non-enhanced CT images, we were not able to distinguish intimal or medial seat from calcifications of the thoracic aorta. Finally, the participants in this study were not retrieved from a general population and the extrapolation of our findings should be made with caution.
Conclusion
In a cohort of patients at intermediate risk of CVD, our study showed that some CVD risk factors were inversely associated with TAC density score after adjustment for TAC volume score, including 10-year FRS, systolic pressure, pulse pressure, and hypertension. The use of both TAC volume and TAC density as separate variables improved the risk prediction of CVD events beyond the CAC score.
Abbreviations
- AS:
-
Agatston score
- CAC:
-
Coronary artery calcium
- CHD:
-
Coronary heart disease
- CI:
-
Confidence intervals
- CVD:
-
Cardiovascular disease
- DAG:
-
Calcium density score based on Agatston
- DAV:
-
Calcium density score based on average attenuation
- FRS:
-
Framingham risk score
- HU:
-
Hounsfield units
- IQ:
-
Interquartile range
- maxHU:
-
Maximum HU attenuation value
- MSCT:
-
Multislice computed tomography
- TA:
-
Thoracic aorta
- TAC:
-
Thoracic aorta calcium
References
Detrano R, Guerci AD, Carr JJ et al (2008) Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 358:1336–1345
Gibson AO, Blaha MJ, Arnan MK et al (2014) Coronary artery calcium and incident cerebrovascular events in an asymptomatic cohort. The MESA Study. JACC Cardiovasc Imaging 7:1108–1115
Budoff MJ, Nasir K, Katz R et al (2011) Thoracic aortic calcification and coronary heart disease events: the multi-ethnic study of atherosclerosis (MESA). Atherosclerosis 215:196–202
Santos RD, Rumberger JA, Budoff MJ et al (2010) Thoracic aorta calcification detected by electron beam tomography predicts all-cause mortality. Atherosclerosis 209:131–135
Wong ND, Gransar H, Shaw L et al (2009) Thoracic aortic calcium versus coronary artery calcium for the prediction of coronary heart disease and cardiovascular disease events. JACC Cardiovasc Imaging 2:319–326
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832
Thomas IC, Shiau B, Denenberg JO et al (2018) Association of cardiovascular disease risk factors with coronary artery calcium volume versus density. Heart 104:135–143
Criqui MH, Denenberg JO, Ix JH et al (2014) Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA 311:271–278
Criqui MH, Knox JB, Denenberg JO et al (2017) Coronary artery calcium volume and density: potential interactions and overall predictive value: the multi-ethnic study of atherosclerosis. JACC Cardiovasc Imaging 10:845–854
Thomas IC, McClelland RL, Allison MA et al (2018) Progression of calcium density in the ascending thoracic aorta is inversely associated with incident cardiovascular disease events. Eur Heart J Cardiovasc Imaging:1343–1350
Thomas IC, McClelland RL, Michos ED et al (2017) Density of calcium in the ascending thoracic aorta and risk of incident cardiovascular disease events. Atherosclerosis 265:190–196
Craiem D, Chironi G, Casciaro ME, Graf S, Simon A (2014) Calcifications of the thoracic aorta on extended non-contrast-enhanced cardiac CT. PLoS One 9:e109584
Desai MY, Cremer PC, Schoenhagen P (2018) Thoracic aortic calcification: diagnostic, prognostic, and management considerations. JACC Cardiovasc Imaging 11:1012–1026
Craiem D, Chironi DG, Casciaro ME, Sirieix ME, Mousseaux E, Simon A (2016) Association of thoracic aorta calcium and non cardiac vascular events in cardiac disease-free individuals. Atherosclerosis 245:22–27
Craiem D, Alsac JM, Casciaro ME et al (2016) Association between thoracic aorta calcium and thoracic aorta geometry in a cohort of asymptomatic participants at increased cardiovascular risk. Rev Esp Cardiol (Engl Ed) 69:827–835
Craiem D, El Batti S, Casciaro ME et al (2017) Age-related changes of thoracic aorta geometry used to predict the risk for acute type B dissection. Int J Cardiol 228:654–660
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Hou ZH, Lu B, Gao Y et al (2012) Prognostic value of coronary CT angiography and calcium score for major adverse cardiac events in outpatients. JACC Cardiovasc Imaging 5:990–999
McEniery CM, Yasmin, Maki-Petaja KM et al (2010) The impact of cardiovascular risk factors on aortic stiffness and wave reflections depends on age: the Anglo-Cardiff Collaborative Trial (ACCT III). Hypertension 56:591–597
Houslay ES, Cowell SJ, Prescott RJ et al (2006) Progressive coronary calcification despite intensive lipid-lowering treatment: a randomised controlled trial. Heart 92:1207–1212
Saremi A, Bahn G, Reaven PD (2012) Progression of vascular calcification is increased with statin use in the Veterans Affairs Diabetes Trial (VADT). Diabetes Care 35:2390–2392
Dykun I, Lehmann N, Kalsch H et al (2016) Statin medication enhances progression of coronary artery calcification: the Heinz Nixdorf recall study. J Am Coll Cardiol 68:2123–2125
Kalsch H, Lehmann N, Moebus S et al (2017) Aortic calcification onset and progression: association with the development of coronary atherosclerosis. J Am Heart Assoc 6:e005093
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Damian Craiem.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects have been previously reported in previous articles of the research team, included in References 12, 14, 15, and 16.
Methodology
• Retrospective
• Cross-sectional study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 63 kb)
Rights and permissions
About this article
Cite this article
Craiem, D., Casciaro, M., Pascaner, A. et al. Association of calcium density in the thoracic aorta with risk factors and clinical events. Eur Radiol 30, 3960–3967 (2020). https://doi.org/10.1007/s00330-020-06708-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06708-w