Abstract
Objective
Evaluation of MRI-derived cerebral 23Na concentrations in patients with migraine in comparison with healthy controls.
Materials and methods
In this case-control study, 24 female migraine patients (mean age, 34 ± 11 years) were enrolled after evaluation of standardized questionnaires. Half (n = 12) of the cohort suffered from migraine, the other half was impaired by both migraine and tension-type headaches (TTH). The combined patient cohort was matched to 12 healthy female controls (mean age, 34 ± 11 years). All participants underwent a cerebral 23Na-magnetic resonance imaging examination at 3.0 T, which included a T1w MP-RAGE sequence and a 3D density-adapted, radial gradient echo sequence for 23Na imaging. Circular regions of interests were placed in predetermined anatomic regions: cerebrospinal fluid (CSF), gray and white matter, brain stem, and cerebellum. External 23Na reference phantoms were used to calculate the total 23Na tissue concentrations. Pearson’s correlation, Kendall Tau, and Wilcoxon rank sum test were used for statistical analysis.
Results
23Na concentrations of all patients in the CSF were significantly higher than in healthy controls (p < 0.001). The CSF of both the migraine and mixed migraine/TTH group showed significantly increased sodium concentrations compared to the control group (p = 0.007 and p < 0.001). Within the patient cohort, a positive correlation between pain level and TSC in the CSF (r = 0.62) could be observed.
Conclusion
MRI-derived cerebral 23Na concentrations in the CSF of migraine patients were found to be statistically significantly higher than in healthy controls.
Key Points
• Cerebral sodium MRI supports the theory of ionic imbalances and may aid in the challenging pathophysiologic understanding of migraine.
• Case-control study shows significantly higher sodium concentrations in cerebrospinal fluid of migraineurs.
• Cerebral sodium MRI may become a non-invasive imaging tool for drugs to modulate sodium, and hence migraine, on a molecular level, and influence patient management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Migraine is one of the most common headache disorders with a prevalence of about 18% in women and 6% in men. The highest incidence is found between 35 and 45 years, with a prevalence of 3:1, women versus men. Different theories have been proposed to explain the pathophysiology of migraine including cortical spreading depression [1, 2], meningeal neuroinflammation [3], cortical neuromodulation [3, 4], and disturbed ionic imbalances [5]. Despite these different mechanisms, a true understanding, e.g., whether the different theories are intertwined or migraine is more than one disease, remains incomplete. Hence, many migraine patients go undiagnosed or are falsely or under-treated. Recent focus has shifted towards studying the disturbed ionic imbalances. A study by Harrington et al of a rat migraine model supports the role of sodium in migraine, with rising sodium levels that increase neuronal excitability [5]. Another study by the same group revealed higher sodium concentrations in lumbar cerebrospinal fluid (CSF) of migraine patients, which was drawn during migraine [6]. However, lumbar punctures are invasive, time-consuming, and require a high patient tolerance.
Tension-type headaches (TTH) are the most common form of primary headaches with different studies suggesting a prevalence ranging between 20 and 78%. Up to now, the underlying pathophysiological concept of TTH is unclear, and the pathogenetic differentiation between migraine and TTH remains controversial. Possible theories for the development of TTH include increased tension of the neck musculature [7] leading to a secondary sensitization via increased nociceptive influence on trigeminal neurons and further NO (nitrogen oxide)-dependent central sensitization [8], as well as mechanical and mental stress factors [8, 9].
For the treatment of headaches in general, it is important to distinguish between migraine and TTH, since both forms are treated with totally different medications. Many patients, especially those with frequent headaches, show symptoms of both migraine and TTH. Thus, a non-invasive imaging tool, which could be clinically implemented on a larger scale, would be desirable.
The feasibility of cerebral 23Na magnetic resonance imaging (MRI) for in vivo imaging has been demonstrated in several studies, including stroke [10], brain tumors, and multiple sclerosis [11,12,13]. So far, no in vivo imaging study in migraineurs or patients suffering from TTH measuring sodium concentrations has been reported. Thus, the purpose of our study was to evaluate MRI-derived cerebral 23Na concentrations in patients with migraine in comparison with healthy controls. We hypothesized that 23Na MRI imaging can detect higher cerebral sodium concentrations in migraineurs in comparison with healthy controls. In addition, we evaluated the impact of accompanying TTH on cerebral sodium concentration, as well as potential influencing factors such as an accompanying aura, time between last attack and MRI measurement, disease duration, average duration and frequency of migraine attacks, pain intensity, and patients’ age.
Methods
This study was performed without any financial or non-financial support from the industry. The authors had complete control of the data submitted for publication. The local institutional review board and ethics committee approved this study which was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from all study participants.
Migraine cohort
Migraine patients were recruited within our university hospital. Eligible patients were asked to complete the Kieler headache survey [14], which serves as an aid for the clinical implementation of the International Headache Society classification guidelines (3rd edition). It was developed to especially support the diagnosis of migraine and TTH, which represent the most frequent headache disorders (92% of all headaches). The survey includes a standardized checklist with 26 questions aiming at typical migraine characteristics as well as TTH characteristics. We retrieved the questionnaire from 62 patients, of which 42 were invited for an in-depth interview by a pain physician. The case history was taken regarding the onset of disease, length, typical intensity (scale 0–10) and frequency of migraine attacks (per month and in the last 3 months), and the possible presence of accompanying aura. Migraine without TTH could be verified in 19 patients according to the case history taken and survey guidelines, and 20 patients showed characteristics for both migraine and TTH. Three patients had to be excluded as two patients did not show distinct migraine features and one patient was not suffering from migraine any longer. Therefore, 26 otherwise healthy female subjects (mean age, 34 ± 11 years; Table 1) were randomly selected and finally included in our patient cohort. Of these, 12 were classified with migraine, whereas the other 12 were suffering from both migraine and accompanying TTH. Overall, two patients had to be excluded because of image artifacts in one and prior contrast media administration in the other patient. Figure 1 portrays a flowchart of the patient recruitment.
Healthy volunteers
The final patient cohort of 24 migraineurs was age-matched to a cohort of 12 healthy female subjects (mean age, 34 ± 11 years; Table 1). The volunteers were recruited through the hospital’s email distributor. Volunteers were considered eligible with the following parameters: (i) no headaches in the past 12 months and (ii) age between 18 and 80 years. Exclusion criteria included any history of neurologic disease including — but not limited to — migraine or TTH, pregnancy, and general contraindications against MRI examinations (e.g., claustrophobia, pacemaker).
Cerebral MRI
Between May 2015 and April 2016, both volunteers and migraineurs underwent an identical cerebral 23Na magnetic resonance imaging examination at 3.0 T (MAGNETOM Tim Trio, Siemens Healthineers). Patients were positioned supine, head first. No contrast media was administered. For each scan, a non-contrast-enhanced T1w MP-RAGE sequence for anatomical referencing and a 3D density-adapted, radial gradient echo sequence [15] for 23Na imaging were acquired using a dual-tuned (23Na/1H), dedicated head-coil (Rapid Biomedical GmbH, Rimpar). The following scan parameters were used: TR 120 ms; TE 0.2 ms; 17,000 projections; flip angle 87°; spatial resolution 4 × 4 × 4 mm3 for 23Na imaging and TR 1630 ms; TE 3.4 ms; bandwidth 179; inversion time 900 ms; flip angle 9°; spatial resolution 1 × 1 × 1 mm3 for the MP-RAGE. Data were regridded performing a convolution with a Kaiser–Bessel kernel (2× oversampling and window width of 4) followed by a complex fast Fourier transformation and deconvolution. 23Na sequences were reconstructed according to the MP-RAGE, allowing direct cross-referencing of regions of interest (ROI).
Quantification of sodium concentration
Offline co-registration of 23Na MRI images to the corresponding T1-weighted MP-RAGE image was done using the statistical parametric mapping toolbox (SPM8, The Wellcome Trust Centre for Neuroimaging) in MATLAB (R2010a, The MathWorks Inc.). Data sets of every patient were analyzed on an OsiriX DICOM viewer 3.8.1 (OsiriX Foundation).
Circular ROIs were placed by two radiologists (M. M., 5 years of experience; A. S., in-training) in consensus in predetermined anatomic regions (similar location in all patients): CSF in the anterior horn of the right lateral ventricle, in subregions of the gray and white matter (postcentral gyri of the GM/ centrum semiovale of the WM), brain stem (pons), and cerebellum (middle cerebellar peduncle), with identical-sized ROIs in all individuals for each anatomic region (exemplary ROI placement can be viewed in Fig. 2). To minimize recall bias, all technical and personal data were removed from the images and datasets were randomized prior to reading. Readers were blinded to the diagnosis of the patient. External sodium reference phantoms placed within the field of view including 2% and 5% agarose doped with 50 mmol and 154 mmol of sodium concentration were used to calculate the tissue total sodium concentration (TSC). Values for 23Na concentration in millimoles per kilogram wet weight were calculated as in [16].
Statistical analysis
Statistical analysis was performed using SAS (SAS Institute Inc.). p values less than 0.05 were considered statistically significant. Descriptive statistics (median, mean, 95% confidence interval, and standard deviation (SD)) were used for all data. The Shapiro–Wilk test was used to check for normal distribution. Two-sided t tests were used for age distribution. Overall, TSCs in the different anatomic regions were evaluated. TSCs of healthy controls and migraineurs overall, as well as compared to patients with migraine alone versus mixed migraine/TTH, were tested for differences using the Wilcoxon rank sum test. Significance level in multiple testing was corrected by the Bonferroni–Holm method.
Within the migraine cohort (migraine and mixed migraine/TTH), correlations between TSC in the different anatomic regions and migraine characteristics including onset of disease, length, historical typical intensity (scale 1–10) and frequency of attacks, and accompanying aura were tested using Pearson’s correlation for continuous variables and the Kendall Tau test for ordinal variables. The following r cutoff values were utilized: 0, no correlation; 0.3, 0.5, and 0.7, weak, moderate, and strong positive correlation, respectively; − 1, negative perfect correlation; − 0.3, − 0.5, and − 0.7, weak, moderate, and strong negative correlation, respectively.
For all measurements, a power analysis was performed, indicating a power > 0.85.
Results
No statistically significant age difference was observed between migraineurs and healthy volunteers (p = 0.76) and migraineurs, mixed migraineurs/TTH patients, and volunteers (p = 0.9).
Quantitative analysis
The overall mean TSCs (in millimoles per kilogram wet weight) for all study participants were 34 mmol/L in the white matter, 40 mmol/L in the gray matter, 92 mmol/L for CSF in the anterior horn of the lateral ventricles, 31 mmol/L in the brainstem, and 32 mmol/L in the cerebellum, respectively.
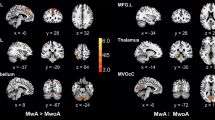
Healthy controls vs. migraine patients
TSC in CSF of the lateral ventricles showed higher concentrations of sodium in migraine patients (n = 24) versus controls (n = 12) with values of 96.1 ± 9.4 mmol/L vs. 84.6 ± 6.2 mmol/L (p < 0.001) (see Figs. 3 and 4 and Table 2). TSCs in the cerebellum and brain stem, as well as white and gray matter, were not statistically different (see Table 2 for details).
Migraine vs. mixed (migraine/TTH) patients
CSF of the lateral ventricles in both the migraine and mixed migraine/TTH group showed a significantly increased TSC compared with that in the control group (p = 0.007 and p < 0.001, respectively) (Fig. 5). Both migraine and mixed migraine/TTH groups did not differ significantly (p = 0.38). No statistically significant difference was found in the other anatomical areas (p > 0.05 for WM, GM, brainstem, and cerebellum).
Qualitative analysis
Evaluation between pain level and TSC of migraine patients
A positive weak correlation between historical typical pain level and TSC of migraine patients in the CSF of the lateral ventricles was observed (r = 0.38), see Fig. 6. Furthermore, a weak positive correlation between pain level and TSC in the brain stem was found (r = 0.31). No substantial correlation was found between pain level and TSC in white (r = 0.08) and gray (r = 0.26) matter, or cerebellum (r = 0.06).
Evaluation of further migraine characteristics
No significant differences between TSC of migraine patients with (n = 10) and without (n = 14) an accompanying aura were found (p > 0.05 for all anatomic regions). No significant correlations were observed between the onsets of disease, length of migraine attacks, number of migraine attacks in the past 3 months, and age (p > 0.05 for all anatomic regions). Although no significant correlation was found between the frequency of migraine attacks and TSC, it is interesting to note that the highest CSF values (120.4 mmol/L) were found in the patient suffering from chronic migraine, including more than 15 attacks per month (the highest frequency of all patients). Qualitative migraine characteristics of migraine and migraine/TTH patients are displayed in Tables 3 and 4.
Analysis of age correlation with the different anatomic regions revealed no statistically significant results.
Discussion
In this first human in vivo sodium imaging study in migraine, our data suggest significantly higher sodium concentrations in CSF of migraine patients compared with healthy controls, results that concur with the aforementioned results of increased lumbar CSF in migraine patients. This is also in accordance with previous animal and human studies, which have emphasized the importance of sodium in the pathophysiology of migraine. Previous studies have demonstrated the potential key role of sodium in migraine development: Cranial sodium shows an increase after nitroglycerin-triggered sensitization in a rat migraine model [5]; sodium in lumbar CSF (but not in blood plasma) shows an increase during a migraine attack [6]; migraine history is inversely correlated with dietary sodium intake [17]; and cerebrospinal fluid sodium rhythms demonstrate peaks in the early morning and late afternoon, matching the two most frequent times of migraine onset [18]. The influence of sodium on action potential frequency dates back to 1949 [19]. More recently, Arakaki et al demonstrated faster transmissions with higher amplitudes of action potentials in hippocampal neurons when extracellular sodium was elevated [20], which may explain the increased excitability of pyramidal cells in migraineurs. In addition, Zakharov et al attempted to understand the direct influence of sodium channels on pain transmission by studying the meninges of rats and the nerve fibers of the trigeminal nerve embedded in them. They were able to show that the transmission of pain signals could be interrupted by tetrodotoxin (TTX), a sodium channel blocker, which might indicate that TTX-sensitive sodium channels have an influence in migraine development [21].
Breaking down the cohort into migraine and mixed migraine/TTH patients, the significantly increased values for TSC in CSF holds true for both groups compared with those of healthy controls. Unfortunately, recruitment of patients only suffering from TTH could not be realized due to an insufficient number of participants.
Although no correlations were found between TSC and the onset of disease, length, and frequency of migraine attacks or accompanying aura overall, we found the highest CSF values for the only patient suffering from chronic headaches (> 15 headaches per month). One could argue that the high frequency of headaches may induce higher sodium concentrations. However, this was only a case-based observation and therefore no conclusion can be drawn. Future studies including more patients suffering from chronic headaches will be of interest to explore the consistency of this CSF sodium change in migraine.
Although our WM and GM values were found to match those found in the literature [22], our CSF values were lower (85 ± 6 mmol/L vs. 140–150 mmol/L). This could be due to the long T1-relaxation time of CSF [23]. Another explanation for this could be partial volume effects which may have resulted in lower calculated sodium concentrations in the CSF. However, as this would be a systematic error, the observed differences between migraineurs and volunteers still hold. In future studies, higher field strength would be desirable because the higher signal-to-noise ratio allows more accurate quantification of TSC by minimizing partial volume effects [24]. Reduction of scanning duration at higher field strengths might also help, especially when examining patients ictally (reduced scan duration may increase patient comfort).
Overall, the advantages of sodium imaging compared with other diagnostic measurements include its non-invasiveness and the possibility of a feasible bio-monitoring tool during therapies.
Limitations
Some study limitations must be acknowledged, especially as this is the first report of this potential migraine biomarker. First, migraine patients were not scanned during migraine. Although preferable, this might have resulted in severe discomfort for the patients and possible premature termination of scans. Nonetheless, future studies should aim on scanning migraineurs ictally, thus merging our scan methods with the study setup from Harrington et al, as presented in the “Introduction” section. This could be pursued with the appropriate preparations, e.g., noise-canceling headphones, and different stimulating methods. Second, we did not investigate males, and it will be important to determine the importance of sex on the TSC changes in migraine. Third, medication status showed a high variation in terms of medication type and intake. Thus, sample size for analysis was insufficient and could have influenced TSC in our cohort. Future studies should aim for detailed medication status and, ideally, homogenous adequately sized cohorts for further analysis. Fourth, post-processing of sodium images was dependent on a physicist, but this could be overcome through different quantification tools or plug-ins, if the clinical benefit of the imaging exam can be justified by further studies. Fifth, although manual ROI placement was done in a similar fashion and the same anatomic region for all volunteers and patients, a (semi-) automatic quantification tool would be preferable, as sodium concentrations may fluctuate according to a study by Abad et al [25]. In addition, future studies should consider scanning volunteers and patients at the same time of day to exclude circadian rhythm changes [18].
Conclusion
We have tested the hypothesis that migraineurs might suffer from increased concentrations of brain sodium and found significantly higher values in the CSF of migraine patients compared with healthy controls. Furthermore, we found a moderate positive correlation between pain level and TSC in CSF of the lateral ventricles. These observations provide further support for a role of brain sodium in the pathophysiology of migraine. If further in-depth studies can confirm our findings, cerebral 23Na MRI may aid in the pathophysiological understanding of migraine and may become a non-invasive imaging tool for drugs to modulate sodium, and hence migraine, on a molecular level. This will hopefully help to reduce the burden of migraine in the future.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- DWI:
-
Diffusion-weighted imaging
- FLAIR:
-
Fluid-attenuated inversion recovery
- GM:
-
Gray matter
- MP-RAGE:
-
Magnetization-prepared rapid acquisition gradient echo
- MRI:
-
Magnetic resonance imaging
- SD:
-
Standard deviation
- TSC:
-
Total sodium concentration
- TTH:
-
Tension-type headaches
- WM:
-
White matter
References
Charles A (2010) Does cortical spreading depression initiate a migraine attack? Maybe not. Headache 50(4):731–733
Zhang X, Levy D, Noseda R, Kainz V, Jakubowski M, Burstein R (2010) Activation of meningeal nociceptors by cortical spreading depression: implications for migraine with aura. J Neurosci 30(26):8807–8814
Buzzi MG, Moskowitz MA (1992) The trigemino-vascular system and migraine. Pathol Biol (Paris) 40(4):313–317
Sun YG, Pita-Almenar JD, Wu CS et al (2013) Biphasic cholinergic synaptic transmission controls action potential activity in thalamic reticular nucleus neurons. J Neurosci 33(5):2048–2059
Harrington MG, Chekmenev EY, Schepkin V, Fonteh AN, Arakaki X (2011) Sodium MRI in a rat migraine model and a NEURON simulation study support a role for sodium in migraine. Cephalalgia 31(12):1254–1265
Harrington MG, Fonteh AN, Cowan RP et al (2006) Cerebrospinal fluid sodium increases in migraine. Headache 46(7):1128–1135
Fernández-de-las-Peñas C, Madeleine P, Caminero AB, Cuadrado ML, Arendt-Nielsen L, Pareja JA (2010) Generalized neck-shoulder hyperalgesia in chronic tension-type headache and unilateral migraine assessed by pressure pain sensitivity topographical maps of the trapezius muscle. Cephalalgia 30(1):77–86
Bendtsen L (2000) Central sensitization in tension-type headache--possible pathophysiological mechanisms. Cephalalgia 20(5):486–508
Jensen R (1999) Pathophysiological mechanisms of tension-type headache: a review of epidemiological and experimental studies. Cephalalgia 19(6):602–621
Wetterling F, Chatzikonstantinou E, Tritschler L (2016) Investigating potentially salvageable penumbra tissue in an in vivo model of transient ischemic stroke using sodium, diffusion, and perfusion magnetic resonance imaging. BMC Neurosci 17(1):82
Zaaraoui W, Konstandin S, Audoin B (2012) Distribution of brain sodium accumulation correlates with disability in multiple sclerosis: a cross-sectional 23Na MR imaging study. Radiology 264(3):859–867
Petracca M, Fleysher L, Oesingmann N, Inglese M (2016) Sodium MRI of multiple sclerosis. NMR Biomed 29(2):153–161
Ouwerkerk R, Bleich KB, Gillen JS, Pomper MG, Bottomley PA (2003) Tissue sodium concentration in human brain tumors as measured with 23Na MR imaging. Radiology 227(2):529–537
Göbel H (2001) Classification of headaches. Cephalalgia 21(7):770–773
Konstandin S, Nagel AM (2014) Measurement techniques for magnetic resonance imaging of fast relaxing nuclei. MAGMA 27(1):5–19
Haneder S, Konstandin S, Morelli JN (2011) Quantitative and qualitative (23)Na MR imaging of the human kidneys at 3 T: before and after a water load. Radiology 260(3):857–865
Pogoda JM, Gross NB, Arakaki X (2016) Severe headache or migraine history is inversely correlated with dietary sodium intake: NHANES 1999-2004. Headache 56(4):688–698
Harrington MG, Salomon RM, Pogoda JM (2010) Cerebrospinal fluid sodium rhythms. Cerebrospinal Fluid Res 7:3
Hodgkin AL, Katz B (1949) The effect of sodium ions on the electrical activity of giant axon of the squid. J Physiol 108(1):37–77
Arakaki X, Foster H, Su L (2011) Extracellular sodium modulates the excitability of cultured hippocampal pyramidal cells. Brain Res 1401:85–94
Zakharov A, Vitale C, Kilinc E (2015) Hunting for origins of migraine pain: cluster analysis of spontaneous and capsaicin-induced firing in meningeal trigeminal nerve fibers. Front Cell Neurosci 9:287
Madelin G, Regatte RR (2013) Biomedical applications of sodium MRI in vivo. J Magn Reson Imaging 38(3):511–529
Thulborn K, Lui E, Guntin J (2016) Quantitative sodium MRI of the human brain at 9.4 T provides assessment of tissue sodium concentration and cell volume fraction during normal aging. NMR Biomed 29(2):137–143
Mirkes CC, Hoffmann J, Shajan G, Pohmann R, Scheffler K (2015) High-resolution quantitative sodium imaging at 9.4 Tesla. Magn Reson Med 73(1):342–351
Abad N, Rosenberg JT, Hike DC, Harrington MG, Grant SC (2018) Dynamic sodium imaging at ultra-high field reveals progression in a preclinical migraine model. Pain 159(10):2058–2065
Acknowledgments
IRB approval: Medical Ethics Committee II Mannheim, Germany; reference number: 2013 566N – MA.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Melissa Meyer, MD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Lothar R. Pilz, co-author.
Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• case-control study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Meyer, M.M., Schmidt, A., Benrath, J. et al. Cerebral sodium (23Na) magnetic resonance imaging in patients with migraine — a case-control study. Eur Radiol 29, 7055–7062 (2019). https://doi.org/10.1007/s00330-019-06299-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06299-1