Abstract
Purpose
To determine the utility of cervical spine MRI in blunt trauma evaluation for instability after a negative non-contrast cervical spine CT.
Methods
A review of medical records identified all adult patients with blunt trauma who underwent CT cervical spine followed by MRI within 48 h over a 33-month period. Utility of subsequent MRI was assessed in terms of findings and impact on outcome.
Results
A total of 1,271 patients with blunt cervical spine trauma underwent both cervical spine CT and MRI within 48 h; 1,080 patients were included in the study analysis. Sixty-six percent of patients with a CT cervical spine study had a negative study. Of these, the subsequent cervical spine MRI had positive findings in 20.9%; 92.6% had stable ligamentous or osseous injuries, 6.0% had unstable injuries and 1.3% had potentially unstable injuries. For unstable injury, the NPV for CT was 98.5%. In all 712 patients undergoing both CT and MRI, only 1.5% had unstable injuries, and only 0.42% had significant change in management.
Conclusions
MRI for blunt trauma evaluation remains not infrequent at our institution. MRI may have utility only in certain patients with persistent abnormal neurological examination.
Key Points
• MRI has limited utility after negative cervical CT in blunt trauma.
• MRI is frequently positive for non-specific soft-tissue injury.
• Unstable injury missed on CT is infrequent.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute cervical spine injury (CSI) is not uncommon after blunt trauma and has been reported in 2–6% of cases [1, 2]. Early detection is critical because delayed or un-diagnosed unstable injury can lead to severe morbidity and mortality[3,4,5]. Five to ten percent of CSI patients have been shown to have deterioration of neurological function in the emergency department (ED) admission because of delay in diagnosis or inadequate immobilization [6]. The National Emergency X-Radiography Utilization Study (NEXUS) cervical spine criteria and Canadian C-spine rules are clinical decision rules that have been widely studied and used in the clearance of the cervical spine after blunt trauma in awake, alert evaluable patients with no distracting injuries, neurologically intact status and no midline cervical spine (CS) tenderness [7, 8]. For patients who fail to meet this standard, multi-slice helical CT is the imaging modality of choice for screening of CSI as it is fast, safe, accurate and cost-effective [9, 10]. CT of the cervical spine has a high negative predictive value for excluding unstable injury in blunt trauma patients [11]. The use of MRI after a negative CT has been an issue of active debate. MRI, due to its superior contrast resolution, has been advocated to assess for ligamentous injury and to potentially evaluate unstable injury. This is especially relevant in obtunded patients since a reliable neurological examination may be precluded [12]. However, the studies investigating the utility of MRI in detecting CSI have shown conflicting results. Some suggest that MRI provides no additional clinically significant findings after normal CT [13,14,15,16,17,18]. Others conclude that MRI does detect clinically significant CSI missed by plain radiography and CT [12, 19,20,21]. The heterogeneity in the literature is partly due to varying definitions of ‘clinically significant’ injury used to assess the utility of MRI [2, 11]. The Trauma Society guidelines were revised to recommend cervical collar removal after a negative CT result alone even in obtunded adult blunt trauma patients [22]. The guidelines were based on studies published until 2013. The purpose of our study was to assess the utility and frequency of MRI use after a negative CT since 2013, examine findings on MRI and assess their impact on patient treatment and outcome.
Methods
This study was a Health Insurance Portability and Accountability Act-compliant retrospective cohort study. The radiology database of our academic, tertiary health system and Level I trauma centre was queried to identify all adult patients with blunt trauma who underwent CT followed by MRI within 48 h. The Human Investigational Committee and Institutional Review Board at our institution approved this review, with a waiver of consent.
Patient selection
Our initial search criteria involved identifying patients who underwent a CT of the cervical spine during a 33-month period (February 2013–November 2015) followed by an MRI of the cervical spine within 48 h. Only patients with suspected blunt cervical spine injury were selected based on history and assessment by emergency room providers. Patients transferred from an outside institution who had a prior cervical spine CT followed by MRI performed at our facilities were included, as well as patients experiencing inpatient falls. Patients were excluded if the CT study was non-diagnostic due to patient motion or if their medical record was incomplete.
Image acquisition
CT cervical spine images were acquired with 64-detector scanners (Discovery CT750 HD and Revolution CT; GE Healthcare, Little Chalfont, UK) with 1.25-mm slice helical acquisition without intravenous contrast and reformatted in coronal and sagittal planes. Siemens 1.5T and 3T magnets were used for MRI scanning without intravenous contrast utilizing trauma protocol sequences that included sagittal T1 FSE, axial and sagittal T2 FSE, sagittal STIR and sagittal GRE sequences.
Image interpretation
CT studies were reviewed by a neuroradiology fellow to classify interpretations as ‘negative’ or ‘positive’ for acute traumatic injury based on the final report given by the emergency department radiology faculty at the time of the scan, since this was used by clinical providers in their decision to pursue subsequent MRI. Studies interpreted unequivocally as negative for CSI were classified ‘Negative CT’. Studies were classified ‘Positive CT’ if impressions included any of the following features: fractures of occipital condyles or C1-C7 vertebral bodies, disc space widening, vertebral subluxation, prevertebral or paravertebral oedema and haematoma, epidural heamatoma, cord haematoma or new disc herniation.
The cervical spine MRI reports were then reviewed in patients with ‘Negative CT’ classification. Studies were classified as ‘Positive MRI’ if they contained any of the following features: fractures of occipital condyles or C1-C7 vertebral bodies, osseous oedema or contusion, ligamentous injury or paravertebral muscle strain, spinal cord oedema or haemorrhage, epidural/subdural haematoma, new or acute disc herniation, and prevertebral oedema or haematoma. MRI studies interpreted unequivocally as negative for any of the above findings were classified ‘Negative MRI’. MRI examination findings were confirmed on a PACS workstation (Synapse, Fuji, Stamford, CT, USA) by neuroradiology faculty with 8 years’ experience, blinded to patient characteristics, outcome, management and report contents other than the impression. CSI was categorized into the following based on the Denis’ 3-column model of instability: None, stable, unstable and potentially unstable [23, 24]. Potentially unstable injuries included patients with discontinuous same-level multicolumn injuries, or cord injury and minimum 1-column injury but not definite 2- or 3-column injury. CT scans on these patients with unstable injuries were also reviewed retrospectively.
Data collection and analysis
We queried the electronic medical record (Epic Systems, Verona, WI, USA) to record patient gender, age, mechanism of injury, Glasgow Coma Scale (GCS), neurological examination deficits and additional polytrauma injuries. If varying GCS assessments were recorded during workup, only the lowest encountered score was documented. Mechanisms of injury were recorded in the following categories: motor vehicle accident (MVA)-automobile or boat, MVA-motorcycle, MVA-pedestrian, battery, sports related injury, struck by falling object, fall from height and fall from standing.
The hospital course of each patient was then retrospectively reviewed to determine cervical collar use, management of spinal injury-surgical or nonsurgical, and post-discharge follow-up. The following five management categories were utilized: surgery during admission, surgery within 2 months of discharge, collar clearance during admission, discharged from hospital with precautionary collar and no surgery, and patient expiration before discharge.
The following statistical analyses were performed using JMP software (JMP Pro, Version 11, SAS, Cary, NC, USA): Chi-square was used to analyse categorical variables and logistic regression was used to analyse continuous variables. A p-value of 0.05 was selected for establishing statistical significance.
Results
During the 33-month study period, a total of 1,271 patients with blunt cervical spine trauma underwent both a CT and an MRI of the cervical spine within 48 h. 191 patients were excluded based on incomplete Epic information, limited CT studies or absent CT reports (usually transferred patients). Thus, a total of 1,080 patients were included in the study analysis.
Sixty-six percent (712/1080) of patients with a CT cervical spine study had a negative study, and 34% were considered positive for cervical spine injury on CT (368/1080). Of the 712 with a negative CT, the subsequent cervical spine MRI had positive findings in 20.9% (149/712). Alternatively, 79.1% of CT studies reported as negative had a subsequent MRI demonstrating no evidence of cervical spine injury (563/712). The mean age of included patients was 57 years (range, 18–93 years). Fifty-five percent (82/149) of the patients were men.
Subanalysis of patients with negative CT and positive MRI
In the 149 patients with initial CT reported negative but with subsequent MRI reported positive for injuries, 92.6% (138/149) had stable ligamentous or osseous injuries, 6.0% (9/149) had unstable injuries and 1.3% (2/149) had potentially-unstable injuries. Due to the paucity of potentially-unstable injuries, these were included for statistical analysis with the unstable group (total – 11/149 or 7.4%).
The majority of findings identified on MRI that were not visible or misinterpreted on CT included the following types of soft tissue injury: ligamentous and cervical fascia injury (n = 97), prevertebral oedema (n = 22), cord injury (n = 16), sub-occipital ligament oedema/injury (n = 14), subchondral oedema, osseous contusions, epidural haemorrhage (n = 8) and acute disc herniation (n = 5) (Table 1).
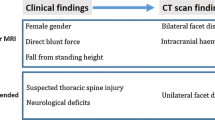
Table 2 describes the 11 unstable or potentially unstable injuries identified on subsequent MRI that were not prospectively identified on CT. A representative case is presented in Fig. 1.
Midsagittal CT (a) was read as negative. Sagittal STIR images (b and c). Increased T2 signal is identified in the midline posterior to the spinous processes from the levels of C3-C6, likely representing strain of the supraspinous ligaments. Suspected disruption of ALL at C5-C6 as well as prevertebral fluid. Increased T2 signal involving the C5-C6 intervertebral disc; suspicious for acute traumatic disc injury and adjacent bone marrow oedema
The most common mechanism of injury included fall from standing (65/149), MVC-auto (either passenger or pedestrian victim, 31/149), and fall from height (29/149). Table 3 describes the frequency of each mechanism of injury and incidence of unstable injuries. Mechanism of injury had no effect on predicting likelihood of unstable injury.
Our patient population characteristics show that men had significantly more unstable injuries than women (p = 0.0144), and increasing age had no association with unstable injury (p = 0.99).
Glasgow Coma Scale scores ranged from 4 to 15 with a mean of 13.4. Obtunded patients with a GCS lower than 13 were significantly more likely to have unstable injury (p = 0.035). Five of 11 patients with unstable injuries had a GCS <13 while the remaining six had a GCS ≥ 13 (see Online Supplemental Table 1).
Fewer than half of all patients had neurological examination deficits (46.3%), and 7/11 patients with unstable injuries had no motor or sensory deficits. The presence of neurological deficits was not found to be a significant predictor of unstable injury (p = 0.84). (see Online Supplemental Table 2).
Midline tenderness to palpation and reported neck pain could only be assessed in non-obtunded patients. In those able to respond, it was not a significant predictor of unstable injury (p = 0.25).
In patients with both stable and unstable injuries, 30.9% had their collar discontinued before discharge (46/149), 30.2% were discharged with collar but were lost to follow-up (45/149), 20.8% were discharged with collar and re-evaluated at follow-up appointment but no surgery planned (31/149), 7.3% underwent surgery (11/149), 5.4% were discharged with collar but the patient discontinued the collar before appointment (8/149) and 5.4% expired before discharge (8/149). Out of 11 patients managed with surgery, 72.7% surgeries occurred during initial admission (8/11) and 27.3% had surgery within 2 months of discharge (3/11).
Of the 11 patients with unstable injury on MRI, 54.5% were discharged with collar and appointment for spine reassessment (6/11), 27.3% had inpatient surgery (3/11), 9% expired (1/11) and 9% had their collar removed during admission (1/11). Of those discharged with collar and plan for appointment (6/11), half were lost to follow-up, and half attended the appointment with no further plan for surgical intervention.
The majority (72.7%) of patients who underwent inpatient or outpatient surgery had stable injuries on MRI, most of whom had pre-existing spinal canal stenosis (8/11) (Table 4). Only 2% of patients with missed findings on CT had a significant change in management (surgery in 3/149). In all 712 patients undergoing both CT and MRI, only 1.5% had unstable injuries (11/712), and only 0.42% had significant change in management (3/712).
Using a negative MRI examination as the gold standard in clinically suspicious or unevaluable blunt trauma patients for excluding any ligamentous and osseous injuries, CT demonstrated a negative predictive value of 79.1% (563/712) (Table 5). For unstable injury, the NPV for CT was 98.5%.
Discussion
Early detection and immobilization of unstable cervical spine injury are a critical goal in evaluation of blunt trauma patients. Imaging has been deemed unnecessary in awake, alert patients who are neurologically intact and without distracting injury.[7] However, the use of NEXUS criteria is inconsistent, especially in patients with persistent neck tenderness [25, 26]. In patients who fail the NEXUS low-risk criteria, CT is accepted as the imaging modality of choice for blunt trauma evaluation. Although the clinical indication for subsequent MRI examination is questionable, its use is not infrequent. The Western Trauma Association Trial results published recently showed that nearly 10% of alert patients at 18 Level I and II trauma centres in North America between September 2013 and March 2015 received an MRI for blunt trauma after a CT [27]. MRI is more frequently advocated for further evaluation in obtunded or clinically unevaluable patients (due to traumatic brain injury, distracting injury or intoxication). Even in this subset of patients, the guidelines by the Eastern Association for the Surgery of Trauma (EAST) were recently revised (2013) to recommend the removal of the collar in obtunded patients after a negative high-quality CT result alone, although this is based on Level III evidence [22].
Multiple studies have been published assessing the utility of MRI in the setting of blunt trauma, with opposing conclusions even in recent literature. Muchow et al. (2008), Schoenfeld et al. (2010), Russin et al. (2013) and James et al. (2014) recommended the use of MRI based on meta-analyses of 5, 13, 11 and 11 studies, respectively [12, 28,29,30]. On the other hand, Panczykowski et al. (2011, 17 studies), Raza et al. (2013, ten studies) and Badhiwala et al. (2015, seven studies) deemed CT alone as sufficient [2, 31, 32]. The heterogeneity in the literature is partly due to varying definitions of ‘clinically significant’ injury used to assess the utility of MRI [11]. The decision to have prolonged external immobilization or operative stabilization seems arbitrary and has not been clearly outlined, but has been used by previous studies to determine the role of MRI [2].
We retrospectively reviewed the institutional utilization of MRI after a negative CT, its utility and impact on outcome. We found the use of MRI in cervical clearance not infrequent. Among evaluable patients, focal neurological deficits and persistent cervical tenderness were the most frequent reasons for ordering the MRI, although this was mostly at the discretion of the treating clinician. This trend is very similar to the multi-institutional trial results published recently where midline tenderness was the reason in half the patients [27]. We found the MRI to be positive in 20.9% (149/712), most of them being ligamentous signal changes that would be classified as stable (92.6% or 138/149). Further analysis of the 11 patients with unstable/potentially unstable injuries showed that they were more frequent in obtunded patients, but showed no association with age, mechanism of trauma or neurological deficits. Subgroup analysis of patients with unstable injuries revealed that 7/11 injuries were difficult to detect on CT even in retrospect. In two patients, osseous fragments on CT were misinterpreted as chronic injuries, which on MRI were shown to be acute extension tear-drop fractures. Evaluation for prevertebral swelling was complicated in two patients by the presence of an endotracheal tube, which can artificially widen the prevertebral space and potentially mask the finding on CT.
The majority (72.7%) of patients who underwent inpatient or outpatient surgery had stable injuries on MRI, most of whom had pre-existing spinal canal stenosis (8/11). Three of 149 patients who had a negative CT but positive MRI underwent surgery, and all had neurological deficits on examination.
In summary, only 1.5% (11/712) patients had evidence of unstable injury on MRI after a negative CT, and only 0.42% had a significant change in management (3/712). These results are similar to the prospective, multi-institutional Western Trauma Association trial that found a sensitivity of CT of 98.5% and a negative predictive value of 99.97% [27]. Twenty percent (2063/10,276) of patients in that study were discharged with a collar. We also found a significant percentage (30%) of patients who were discharged with a cervical collar after ‘positive’ MRI findings but no finding of instability on imaging. In the patients in whom follow- up was available, surgery was not planned in any case. The significance of these MRI findings and their evolution could not be evaluated, and that is a limitation of this study.
The current institutional study results are consistent with our previous meta-analysis of the literature that found the utility of MRI for detecting unstable injury in both alert and obtunded patients to be rather low [33]. Although there is a 15% abnormal finding rate overall on subsequent MRI, the overall risk of detecting an unstable injury on follow-up is as low as 0.3% when weighted by size of patient population, and 0.0029% when weighted by inverse of variance to reduce the disproportionate contribution to smaller studies. The fear of missed unstable injury and potential legal implications are often used to justify performing an MRI following a negative CT [34]. However, there is no evidence supporting MRI as a cost-effective strategy to-date [35]. Cervical collar use or surgery done as follow-up often does not correlate with evidence of unstable injury on imaging [36, 37]. We found similar results in our study. Recent propensity-matched analysis has also found the incorporation of MRI in routine evaluation of blunt trauma patients to be unsubstantiated [38].
This study is limited by its retrospective single-institution model with challenges in obtaining all data points. Specifically, we were not able to determine the clinical justification for MRI in every patient included in the study. In addition, a significant number of patients discharged with cervical collars were lost to follow-up.
In conclusion, this study shows that the use of MRI for blunt trauma evaluation is not infrequent despite its relatively high cost, limited availability, prolonged scan time and inability to be used in haemodynamically unstable patients. Nonspecific findings on MRI do not positively impact outcome. It supports the results of previous prospective studies that have shown the sensitivity of CT for those with cervical tenderness or neurological deficits to be 100% for clinically significant injuries [27, 39]. MRI may be warranted in certain patients with persistent abnormal neurological examination.
Abbreviations
- ALL:
-
Anterior Longitudinal Ligament
- CSI:
-
Cervical spine injury
- CT:
-
Computed tomography
- ED:
-
Emergency department
- GCS:
-
Glasgow Coma Scale
- IRB:
-
Institutional Review Board
- MRI:
-
Magnetic resonance imaging
- MVA:
-
Motor vehicle accident
- NEXUS:
-
National Emergency XRadiography Utilization Study
- NPV:
-
Negative predictive value
- PLC:
-
Posterior ligamentous complex
- PLL:
-
Posterior longitudnal ligament
References
Young AJ, Wolfe L, Tinkoff G, Duane TM (2015) Assessing incidence and risk factors of cervical spine injury in blunt trauma patients using the National Trauma Data Bank. Am Surg 81:879–883
Badhiwala JH, Lai CK, Alhazzani W et al (2015) Cervical spine clearance in obtunded patients after blunt traumatic injury: a systematic review. Ann Intern Med 162:429–437
Harris MB, Kronlage SC, Carboni PA et al (2000) Evaluation of the cervical spine in the polytrauma patient. Spine (Phila Pa 1976) 25:2884–2891 discussion 2892
Levi AD, Hurlbert RJ, Anderson P et al (2006) Neurologic deterioration secondary to unrecognized spinal instability following trauma--a multicenter study. Spine (Phila Pa 1976) 31:451–458
Reid DC, Henderson R, Saboe L, Miller JD (1987) Etiology and clinical course of missed spine fractures. J Trauma 27:980–986
Poonnoose PM, Ravichandran G, McClelland MR (2002) Missed and mismanaged injuries of the spinal cord. J Trauma 53:314–320
Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI (2000) Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med 343:94–99
Stiell IG, Wells GA, Vandemheen KL et al (2001) The Canadian C-spine rule for radiography in alert and stable trauma patients. Jama 286:1841–1848
Holmes JF, Akkinepalli R (2005) Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma 58:902–905
Hennessy D, Widder S, Zygun D, Hurlbert RJ, Burrowes P, Kortbeek JB (2010) Cervical spine clearance in obtunded blunt trauma patients: a prospective study. J Trauma 68:576–582
Malhotra A, Wu X, Kalra VB et al (2017) Utility of MRI for cervical spine clearance after blunt traumatic injury: a meta-analysis. Eur Radiol 27:1148–1160
Muchow RD, Resnick DK, Abdel MP, Munoz A, Anderson PA (2008) Magnetic resonance imaging (MRI) in the clearance of the cervical spine in blunt trauma: a meta-analysis. J Trauma 64:179–189
Stelfox HT, Velmahos GC, Gettings E, Bigatello LM, Schmidt U (2007) Computed tomography for early and safe discontinuation of cervical spine immobilization in obtunded multiply injured patients. J Trauma 63:630–636
Tomycz ND, Chew BG, Chang YF et al (2008) MRI is unnecessary to clear the cervical spine in obtunded/comatose trauma patients: the four-year experience of a level I trauma center. J Trauma 64:1258–1263
Sanchez B, Waxman K, Jones T, Conner S, Chung R, Becerra S (2005) Cervical spine clearance in blunt trauma: evaluation of a computed tomography-based protocol. J Trauma 59:179–183
Harris TJ, Blackmore CC, Mirza SK, Jurkovich GJ (2008) Clearing the cervical spine in obtunded patients. Spine (Phila Pa 1976) 33:1547–1553
Gargas J, Yaszay B, Kruk P, Bastrom T, Shellington D, Khanna S (2013) An analysis of cervical spine magnetic resonance imaging findings after normal computed tomographic imaging findings in pediatric trauma patients: ten-year experience of a level I pediatric trauma center. J Trauma Acute Care Surg 74:1102–1107
Vanguri P, Young AJ, Weber WF et al (2014) Computed tomographic scan: it's not just about the fracture. J Trauma Acute Care Surg 77:604–607
Diaz JJ Jr, Aulino JM, Collier B et al (2005) The early work-up for isolated ligamentous injury of the cervical spine: does computed tomography scan have a role? J Trauma 59:897–903 discussion 903-894
Kaiser ML, Whealon MD, Barrios C, Kong AP, Lekawa ME, Dolich MO (2012) The current role of magnetic resonance imaging for diagnosing cervical spine injury in blunt trauma patients with negative computed tomography scan. Am Surg 78:1156–1160
Benzel EC, Hart BL, Ball PA, Baldwin NG, Orrison WW, Espinosa MC (1996) Magnetic resonance imaging for the evaluation of patients with occult cervical spine injury. J Neurosurg 85:824–829
Patel MB, Humble SS, Cullinane DC et al (2015) Cervical spine collar clearance in the obtunded adult blunt trauma patient: a systematic review and practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 78:430–441
Denis F (1983) The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 8:817–831
Cybulski GR, Douglas RA, Meyer PR Jr, Rovin RA (1992) Complications in three-column cervical spine injuries requiring anterior-posterior stabilization. Spine (Phila Pa 1976) 17:253–256
Morrison J, Jeanmonod R (2014) Imaging in the NEXUS-negative patient: when we break the rule. Am J Emerg Med 32:67–70
Ackland HM, Cameron PA, Varma DK et al (2011) Cervical spine magnetic resonance imaging in alert, neurologically intact trauma patients with persistent midline tenderness and negative computed tomography results. Ann Emerg Med 58:521–530
Inaba K, Byerly S, Bush LD et al (2016) Cervical spinal clearance: a prospective Western Trauma Association Multi-institutional Trial. J Trauma Acute Care Surg 81:1122–1130
James IAO, Moukalled A, Yu E et al (2014) A systematic review of the need for MRI for the clearance of cervical spine injury in obtunded blunt trauma patients after normal cervical spine CT. J Emerg Trauma Shock 7:251–255
Russin JJ, Attenello FJ, Amar AP, Liu CY, Apuzzo ML, Hsieh PC (2013) Computed tomography for clearance of cervical spine injury in the unevaluable patient. World Neurosurg 80:405–413
Schoenfeld AJ, Bono CM, McGuire KJ, Warholic N, Harris MB (2010) Computed tomography alone versus computed tomography and magnetic resonance imaging in the identification of occult injuries to the cervical spine: a meta-analysis. J Trauma 68:109–113 discussion 113-104
Panczykowski DM, Tomycz ND, Okonkwo DO (2011) Comparative effectiveness of using computed tomography alone to exclude cervical spine injuries in obtunded or intubated patients: meta-analysis of 14,327 patients with blunt trauma. J Neurosurg 115:541–549
Raza M, Elkhodair S, Zaheer A, Yousaf S (2013) Safe cervical spine clearance in adult obtunded blunt trauma patients on the basis of a normal multidetector CT scan--a meta-analysis and cohort study. Injury 44:1589–1595
Malhotra A, Wu X, Kalra VB, Schindler J, Matouk CC, Forman HP (2016) Evaluation for blunt cerebrovascular injury: review of the literature and a cost-effectiveness analysis. AJNR Am J Neuroradiol 37:330–335
Hogan GJ, Mirvis SE, Shanmuganathan K, Scalea TM (2005) Exclusion of unstable cervical spine injury in obtunded patients with blunt trauma: is MR imaging needed when multi-detector row CT findings are normal? Radiology 237:106–113
Wu X, Malhotra A, Geng B et al (2017) Cost-effectiveness of magnetic resonance imaging in cervical spine clearance of neurologically intact patients with blunt trauma. Ann Emerg Med. https://doi.org/10.1016/j.annemergmed.2017.07.006
Fisher BM, Cowles S, Matulich JR, Evanson BG, Vega D, Dissanaike S (2013) Is magnetic resonance imaging in addition to a computed tomographic scan necessary to identify clinically significant cervical spine injuries in obtunded blunt trauma patients? Am J Surg 206:987–993 discussion 993-984
Sarani B, Waring S, Sonnad S, Schwab CW (2007) Magnetic resonance imaging is a useful adjunct in the evaluation of the cervical spine of injured patients. J Trauma 63:637–640
Schoenfeld AJ, Tobert DG, Le HV et al (2017) The utility of adding magnetic resonance imaging to computed tomography alone in the evaluation of cervical spine injury: a propensity matched analysis. Spine (Phila Pa 1976). https://doi.org/10.1097/brs.0000000000002285
Resnick S, Inaba K, Karamanos E et al (2014) Clinical relevance of magnetic resonance imaging in cervical spine clearance: a prospective study. JAMA Surg 149:934–939
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ajay Malhotra.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Ethical approval
Institutional Review Board of Yale University approval was obtained for this study.
Informed consent
Written informed consent was waived by Institutional Review Board.
Methodology
• retrospective
• case-control study
• performed at one institution
Electronic supplementary material
ESM 1
(DOCX 40 kb)
Rights and permissions
About this article
Cite this article
Malhotra, A., Durand, D., Wu, X. et al. Utility of MRI for cervical spine clearance in blunt trauma patients after a negative CT . Eur Radiol 28, 2823–2829 (2018). https://doi.org/10.1007/s00330-017-5285-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5285-y