Abstract
Objectives
To compare the diagnostic performance of gradient-recalled echo-based magnetic resonance elastography (GRE-MRE) and spin-echo echo-planar imaging-based MRE (SE-EPI-MRE) in liver fibrosis staging.
Methods
A systematic literature search was performed to identify studies involving the performance of MRE for the diagnosis of liver fibrosis. Pooled sensitivity, specificity, positive and negative likelihood ratios, the diagnostic odds ratio, and a summary receiver operating characteristic (ROC) curve were estimated by using a bivariate random effects model. Subgroup analyses were performed between different study characteristics.
Results
Twenty-six studies with a total of 3,200 patients were included in the meta-analysis. Pooled sensitivity and specificity of GRE-MRE and SE-EPI-MRE did not differ significantly. The area under the summary ROC curve for stage diagnosis of any (F ≥ 1), significant (F ≥ 2), advanced (F ≥ 3), and cirrhosis (F = 4) on GRE-MRE and SE-EPI-MRE were 0.93 versus 0.94, 0.95 versus 0.94, 0.94 versus 0.95, and 0.92 versus 0.93, respectively. Substantial heterogeneity was detected for both sequences.
Conclusion
Both GRE and SE-EPI-MRE show high sensitivity and specificity for detection of each stage of liver fibrosis, without significant differences. Magnetic resonance elastography (MRE) may be useful for noninvasive evaluation of liver fibrosis in chronic liver disease.
Key points
• Pooled sensitivity and specificity of GRE-MRE and SE-EPI-MRE did not differ significantly.
• GRE-MRE and SE-EPI-MRE were highly accurate for detecting all stages of fibrosis.
• Due to better agreement and repeatability, GRE-MRE should be used first.
• In case of failure on GRE-MRE, SE-EPI-MRE should be used.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Liver fibrosis is characterised by excessive deposition of the extracellular matrix, leading to consequent liver architectural distortion. As progressive liver fibrosis leads to cirrhosis, patients are at increased risk for hepatic decompensation and hepatocellular carcinoma [1, 2]. Consequently, identifying fibrosis across the spectrum from early fibrosis to cirrhosis is of great clinical importance for the management of patients with chronic liver disease (CLD) [3]. Although liver biopsy is considered to be the gold standard for liver fibrosis measurements, it has several limitations such as invasiveness, risks of complications, sampling errors, and interobserver variations in interpretation [4]. Therefore, several noninvasive imaging-based methods for the assessment of liver fibrosis have been developed [5].
Recent advances in magnetic resonance (MR) imaging have led to a growing interest in multiparametric MR imaging to assess liver fibrosis, including MR spectroscopy, diffusion-weighted imaging (DWI), perfusion-weighted imaging, and MR elastography (MRE) [6, 7]. Of these, MRE is gaining acceptance as the most accurate noninvasive tool for the assessment of liver fibrosis [8,9,10,11,12]. Gradient recalled echo-based MRE (GRE-MRE) has been well studied and is available in many specialised centres. Although MRE is not limited by obesity, most failures of GRE-MRE are caused by the short T2* transverse relaxation time of iron-overloaded liver [4, 11, 13]. Because spin-echo echo-planar imaging-based MRE (SE-EPI-MRE) is less sensitive to transverse relaxation signal decay than GRE-MRE, SE-EPI-MRE has been described to better estimate stiffness maps for increased spatial coverage within similar acquisition time, as well as having larger areas of stiffness measurement, and lower overall failure rate [13,14,15,16]. However, a direct comparison of GRE and SE-EPI-MRE for the assessment of liver fibrosis with histopathology as a reference standard has rarely been examined [17, 18].
Several recent meta-analyses have characterised the diagnostic performance of GRE-MRE in various CLDs [19,20,21]. However, since many studies on MRE were published after 2016, the data need to be updated. In addition, there are no meta-analyses comparing GRE and SE-EPI-MRE. Therefore, the purpose of this study is to compare the overall diagnostic value of GRE and SE-EPI-MRE for the detection and staging of liver fibrosis by performing a meta-analysis, using histopathology as the reference standard.
Materials and methods
The overall process of this meta-analysis was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [22,23,24].
Literature search
We searched MEDLINE, EMBASE, and Cochrane library databases for relevant studies by using the following keywords and medical subject heading (MeSH) terms: “liver fibrosis” OR “hepatic fibrosis” AND “magnetic resonance elastography” OR “MR elastography” OR “MRE”. The last search date was 31 January 2017. The search included all articles, without time limits or language restrictions. References cited within potentially eligible articles and related citations suggested by PubMed were assessed to find other relevant studies. Details of the literature search are given in Table E1 (online).
Study selection
All search results were screened for eligibility on the basis of the title and abstract by two independent reviewers. Animal studies, review articles, and case reports were excluded. Subsequently, the same two reviewers evaluated the full text of articles for final inclusion. Studies were selected if they included all of the following criteria: (1) the study appraised the performance of MRE for the diagnosis of liver fibrosis; (2) histopathology was used as the reference standard; (3) the study used a comparable liver fibrosis staging system; (4) available data could be used to compute the true-positive, false-positive, true-negative, and false-negative results of MRE for the diagnosis of the fibrosis stage. Studies were excluded if any of the following exclusion criteria were present: (1) the study reported a conference abstract; (2) the study was not written in English; (3) the study involved fewer than 20 patients; (4) the study evaluated only children or transplant recipients. Studies with greater sample sizes were brought in when overlapping samples were recruited in more than one study. All discrepancies in study selection between the two reviewers were resolved by consensus following discussion.
Data extraction
Data were extracted by two independent reviewers using a predefined form. For each study, we retrieved the following study design information: the names of the first and corresponding authors; hospital or medical school; the country where the study was conducted; year of publication; study design; time range of study; number of patients; reference test; scoring system for histopathologic staging of liver fibrosis; time period between reference standard and index test; mean or median patient age; gender ratio; patient spectrum. The following technical characteristics of MRE were recorded: magnetic field strength; MR scanner; MRE dimension; wave frequency of MRE; cut-off value used for each stage of liver fibrosis. To compare fibrosis staging acquired with various scoring systems, we transformed each reported fibrosis stage into the simplified five-stage fibrosis scoring system shown in Table E2 (online).
Study quality assessment
The quality of studies included in the meta-analysis was assessed using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool by two independent reviewers. This tool enables reviewers to evaluate the risk of bias in patient selection, index test, reference standard, patient flow and timing, and a study’s applicability to clinical practice in terms of patient selection, index tests, and reference standards [25]. We considered an acceptable interval of time between MRE and biopsy to be less than or equal to 1 year, given the relatively slow progression of liver fibrosis.
Statistical analysis
For each study, two-by-two contingency tables were extracted or reconstructed for the classification of F0 versus F ≥ 1, F0 and F1 versus F ≥ 2, F0–F2 versus F ≥ 3, and F0–F3 versus F4, respectively. The primary analysis was the diagnostic performance of GRE and SE-EPI-MRE for detection of significant fibrosis (F ≥ 2). The secondary analysis was the performance of each MRE sequence for detection of any fibrosis (F ≥ 1), advanced fibrosis (F ≥ 3), and cirrhosis (F = 4), respectively. The pooled estimates of sensitivity, specificity, positive and negative likelihood ratios, and the diagnostic odds ratio, along with the 95% confidence interval (CI), were calculated by using the bivariate random effects model of Reitsma et al. [26]. A summary receiver operating characteristic (ROC) curve was generated using the bivariate model of Reitsma et al. [26], which is equivalent to a hierarchical summary ROC. Heterogeneity among the included studies was assessed with I 2 and χ2 statistics for each of the pooled estimates [23]. Heterogeneity was judged to be substantial if I 2 was more than 50% and if the P value for χ2 statistics was less than 0.10 [27]. To investigate the cause of heterogeneity, threshold effects, influence and sensitivity analysis, and subgroup analysis were performed. Threshold effects were explored by assessing a linear correlation between the sensitivity and false-positive rates and were regarded as substantial if a Spearman’s correlation coefficient was 0.6 or higher [28]. In the influence analysis, the presence of outlier and influential research was assessed by using Cook’s distance, with 4/n as a cut-off, where n is the number of studies [29]. Sensitivity analysis was performed to quantify the effects of each study on the pooled estimates. Subgroup analysis for sensitivity was performed by using a random effects model with several covariates that could have accounted for heterogeneity. Publication bias was assessed by using the funnel plot asymmetry test, with a P value of less than 0.10 considered to indicate significant small-study bias [30]. Statistical analysis was performed by using R software (R Foundation for Statistical Computing, Vienna, Austria; version 3.3.2; http://www.R-project.org ) with the “metafor” and “mada” packages.
Results
Study selection and characteristics of the included studies
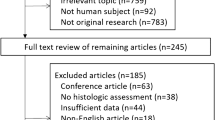
A total of 360 relevant studies were identified in the initial search after the removal of duplicates, and 233 articles were excluded on the basis of the screening of titles or abstracts. Among 127 potentially relevant studies, 26 studies with a total of 3,200 cases were finally included in the meta-analysis [9,10,11,12, 17, 31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50] (Fig. 1).
Important characteristics of the 26 included studies are summarised in Tables 1, 2, and E3 (online). The number of patients ranged from 20 to 416. In five studies the disease spectrum was restricted to non-alcoholic fatty liver disease (NAFLD) [36, 41, 45, 49, 50], in four studies to chronic hepatitis B (CHB) [37, 38, 40, 43], in three studies to chronic hepatitis B or C [17, 39, 48], and in one study to primary sclerosing cholangitis [42]. In the study by Chang et al. [40], the CHB group and the non-CHB group were evaluated independently. Accordingly, we separately considered each group as a unit of analysis. The reference standard was liver resection for all patients in 1 study [44], a combination of resection, biopsy, and/or explant in 7 studies [9, 12, 17, 35, 38,39,40], and biopsy for all patients in the remaining 18 studies.
Quality assessment
Figure 2 demonstrates the results of study quality assessment with the QUADAS-2 tool. The included studies satisfied most of the QUADAS-2 questions. In 15 studies, however, the risk of bias in patient selection was high because of a restricted disease spectrum or non-consecutive patient enrolment. The details of quality assessment for each study are provided in Table E4 (online).
Diagnostic accuracy of MRE
Primary analysis
Nineteen and six units of data were included for detection of significant fibrosis (F ≥ 2) on GRE and SE-EPI sequences, respectively. The pooled sensitivity, specificity, positive and negative likelihood ratios, and diagnostic odds ratios for detection of significant fibrosis with GRE-MRE were 0.92 (95% CI: 0.89, 0.94), 0.92 (95% CI: 0.90, 0.95), 9.44 (95% CI: 5.99, 14.87), 0.12 (95% CI: 0.08, 0.17), and 93.28 (95% CI: 49.21, 176.81), respectively (Fig. 3, A, Table 3). The pooled sensitivity, specificity, positive and negative likelihood ratios, and diagnostic odds ratios for detection of significant fibrosis with SE-EPI-MRE were 0.87 (95% CI: 0.77, 0.96), 0.93 (95% CI: 0.89, 0.97), 9.09 (95% CI: 6.22, 13.28), 0.14 (95% CI: 0.07, 0.30), and 90.32 (95% CI: 39.38, 207.19), respectively (Fig. 3, B, Table 3). There was no difference in the pooled sensitivity of the GRE and SE-EPI sequence (0.92 vs. 0.87, P = 0.336). The area under the summary ROC curve was 0.95 and 0.94 for the GRE and SE-EPI sequences, respectively, which suggested high diagnostic accuracy (Fig. 4).
Summary ROC curve of the accuracy of detection of significant fibrosis (F ≥ 2) with A GRE sequence and B SE-EPI sequence. Each circle (GRE) and square (SE-EPI) indicates the data of each included study, while the black circles (GRE) and squares (SE-EPI) indicate summary estimates of each sequence. Continuous lines represent a 95% confidence region and dotted lines represent a 95% prediction region
Secondary analysis
The areas under the summary ROC curve for stage diagnosis of any fibrosis, advanced fibrosis, and cirrhosis on GRE and SE-EPI sequences were 0.93 versus 0.94, 0.94 versus 0.95, and 0.92 versus 0.93, respectively, suggesting high diagnostic accuracy (Table 3). The summary ROC plot is shown in Figure E1-4 (online).
Assessment of heterogeneity
In the primary analysis, GRE-MRE exhibited substantial heterogeneity (P < 0.001 for χ2 and I2 > 60%) for both sensitivity and specificity. However, SE-EPI-MRE exhibited substantial heterogeneity for sensitivity (P < 0.001 for χ2 and I2 = 92.1%), but not for specificity (P = 0.15 for χ2 and I2 = 40.2%).
Diagnostic threshold effects
In the primary analysis, the Spearman’s correlation coefficient between sensitivity and the false-positive rate for GRE and SE-EPI-MRE was calculated to be -0.391 (P = 0.098) and 0.543 (P = 0.266), respectively. Therefore, a weak positive correlation between sensitivity and the false-positive rate was demonstrated only for SE-EPI-MRE. No substantial threshold effect (correlation coefficient of 0.6 or higher) was observed in the secondary analysis. Heterogeneity statistics and threshold effects are summarised in Table E5 (online).
Influence and sensitivity analysis
In the influence analysis for GRE-MRE, studies by Godfrey et al. [33] and Cui et al. [41] showed relatively larger values for Cook’s distance (0.48 and 0.58) than other studies and accordingly may be considered to have suggested greater influence. In the sensitivity analysis, the amount of heterogeneity (I 2) was reduced from 60.4% to 52.0% and 53.3% when studies by Godfrey et al. and Cui et al., respectively, were excluded. However, pooled sensitivities were almost unchanged. In the influence analysis for SE-EPI-MRE, a study by Bohte et al. [48] was judged to show greater influence (Cook’s distance, 0.65). In the sensitivity analysis, however, the amount of heterogeneity was minimally altered after removal of the study by Bohte et al.
Subgroup analysis
For GRE-MRE, sensitivity was significantly higher in studies originating from Asian countries compared to studies originating from Western countries (94% vs. 82%, P = 0.003), in studies with an aetiology of CLD that was specified to be viral in comparison to studies in which aetiologies were not specified (95% vs. 88%, P = 0.004) and in studies in which the METAVIR system was used in all patients in comparison to studies where the METAVIR system was not used in all patients (94% vs. 85%, P = 0.007). Other subgroup factors did not show statistically significant differences (P > 0.166). For SE-EPI-MRE, significantly higher sensitivity was reported in studies that used 3D MRE than in studies that used 2D MRE (98% vs. 81%, P = 0.039). There was no significant difference in sensitivity for the remaining subgroups (P > 0.078) (Table 4).
Assessment of publication bias
In the primary analysis, low likelihoods of publication bias for GRE and SE-EPI sequences (P = 0.136 and P = 0.119) were observed with funnel plot asymmetry tests. However, high likelihoods of publication bias were observed for GRE-MRE for the staging of advanced fibrosis and cirrhosis (P = 0.041 and P = 0.002) and for SE-EPI-MRE for the staging of advanced fibrosis (P < 0.001).
Discussion
Early and accurate detection of liver fibrosis is important because liver fibrosis is now considered a dynamic process, with significant potential for reversal [51]. Significant fibrosis (≥ F2) is typically considered a hallmark of the progressive form of liver disease, and the ultimate aim of treatment for this fibrosis stage is to cure the patient by resolving the underlying cause of liver disease [51]. Furthermore, discernment of advanced fibrosis (F3) or cirrhosis (F4) is essential because advanced fibrosis and cirrhosis patients should be screened for portal hypertension and hepatocellular carcinoma [5]. On the basis of our study results, both GRE and SE-EPI-MRE were highly accurate for detecting all stages of liver fibrosis, could be acquired by various MR systems and sequences, and had the advantage of being associated with MR, which was a better method of detection for hepatocellular carcinoma than other modalities.
Primary and secondary analysis of our meta-analysis on GRE-MRE and SE-EPI-MRE demonstrated an excellent diagnostic performance with area under the summary ROC curve values of 0.92-0.95. Previous studies comparing GRE and SE-EPI-MRE were without histopathologic data [13,14,15, 52] or were limited to specific diseases [17, 50]. The current meta-analysis included only studies with pathologic fibrosis staging as the reference standard, directly compared two MRE sequences, included various aetiologies of CLD, and showed that SE-EPI-MRE is highly accurate for detecting each stage of fibrosis without significant differences in pooled sensitivity, specificity, and area under the summary ROC curve values in comparison to GRE-MRE.
According to the findings of a recent study on the agreement and repeatability of MRE in 24 adult volunteers, GRE-MRE showed better agreement and repeatability than SE-EPI-MRE [52]. However, the results of SE-EPI-MRE require a shorter acquisition time in comparison to GRE-MRE, and this may be beneficial in CLD patients or in children and young adults who lack the ability to breath-hold appropriately [14]. In addition, due to a higher wave signal-to-noise ratio in comparison to GRE-MRE, SE-EPI-MRE enabled wave tracking through larger and deeper regions of the liver, which resulted in larger measurable regions of interest in an obese patient. Obtaining as much of the liver volume as possible is important for both the accuracy and reproducibility of liver stiffness measurement as well as to overcome limitations related to sampling errors with biopsy or US elastography. Because GRE-MRE has better agreement and repeatability, GRE sequences should be used in the first place. However, in patients with conditions of iron overload in the liver (e.g., cirrhosis, thalassemia, and hemochromatosis), or in obese patients who are likely to fail on GRE sequences, SE-EPI sequences should be used.
In a subgroup analysis of GRE-MRE on fibrosis staging systems, significant differences in sensitivity between METAVIR versus other systems were present (94% vs. 85%, P = 0.007). This may be in line with the findings of studies from Western countries and in studies in which the CLD aetiology was not specified (which included NAFLD), which also demonstrated significantly lower sensitivity in subgroup analysis. NAFLD is the most common liver disease in the USA, and a recent meta-analysis of MRE on NAFLD demonstrated a pooled sensitivity and specificity of 75-88% and 77-87%, respectively [19]. We assume that the different histopathologic findings of viral hepatitis and NAFLD together with the different fibrosis staging systems used may have affected the results.
Three-dimensional (3D) SE-EPI is advantageous in that all three-directional motion encoding gradients are applied and enable true 3D volumetric acquisition of MRE, making the measurement of liver stiffness more accurate and generalisable. In a subgroup analysis, significantly higher sensitivity was reported in 3D SE-EPI than in 2D SE-EPI. However, all of the studies with 3D SE-EPI included large numbers of normal patients, which may have caused the diagnostic performance to be overestimated because of spectrum bias. Future studies comparing 2D and 3D SE-EPI-MRE with histopathology as a reference standard are necessary.
This study has both strengths and limitations. One major strength is that this is the first meta-analysis to compare GRE and SE-EPI-MRE with histopathology as the reference standard. Another strength of this study is inclusion of some of the most recently published studies, with 12 out of 26 included studies having been published after January 2016, as well as subgroup and sensitivity analyses to evaluate the stability of findings and to identify potential factors responsible for heterogeneity. The main limitation of this study is that it was a study-level diagnostic accuracy meta-analysis, as opposed to being based on individual participant data. Second, we could not compare the failure rate of each MRE sequence because most of the included studies lacked sufficient data to calculate the failure rate. However, several recent studies have shown that SE-EPI-MREs have lower failure rates, particularly in patients with iron overload in the liver [13, 15]. Third, considerable heterogeneity was observed for both GRE and SE-EPI sequences. Fourth, we considered an acceptable interval of time between MRE and biopsy to be less than or equal to 1 year. This could have resulted in some bias if the disease progressed during that time interval.
In conclusion, through a systematic review and meta-analysis, MRE with both GRE and SE-EPI was shown to be a highly accurate and noninvasive technique for staging liver fibrosis in CLD. Since GRE-MRE has better agreement and repeatability, GRE-MRE should be used in the first place. However, in patients who are likely to fail on GRE-MRE, SE-EPI-MRE should be used. Future research comparing SE-EPI-MRE and other noninvasive methods is warranted.
Abbreviations
- CLD:
-
Chronic liver disease
- MRE:
-
Magnetic resonance elastography
- GRE:
-
Gradient recalled echo
- SE-EPI:
-
Spin-echo echo-planar imaging
References
Tsochatzis EA, Bosch J, Burroughs AK (2014) Liver cirrhosis. Lancet 383:1749–1761
D'Amico G, Garcia-Tsao G, Pagliaro L (2006) Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol 44:217–231
Martínez SM, Crespo G, Navasa M, Forns X (2011) Noninvasive assessment of liver fibrosis. Hepatology 53:325–335
Venkatesh SK, Yin M, Ehman RL (2013) Magnetic resonance elastography of liver: technique, analysis, and clinical applications. J Magn Reson Imaging 37:544–555
Castera L (2012) Noninvasive methods to assess liver disease in patients with hepatitis B or C. Gastroenterology 142:1293-1302.e1294
Hagiwara M, Rusinek H, Lee VS, Losada M, Bannan MA, Krinsky GA et al (2008) Advanced liver fibrosis: diagnosis with 3D whole-liver perfusion MR imaging--initial experience. Radiology 246:926–934
Friedrich-Rust M, Muller C, Winckler A, Kriener S, Herrmann E, Holtmeier J et al (2010) Assessment of liver fibrosis and steatosis in PBC with FibroScan, MRI, MR-spectroscopy, and serum markers. J Clin Gastroenterol 44:58–65
Loomba R, Wolfson T, Ang B, Hooker J, Behling C, Peterson M et al (2014) Magnetic resonance elastography predicts advanced fibrosis in patients with nonalcoholic fatty liver disease: a prospective study. Hepatology 60:1920–1928
Yoon JH, Lee JM, Joo I, Lee ES, Sohn JY, Jang SK et al (2014) Hepatic fibrosis: prospective comparison of MR elastography and US shear-wave elastography for evaluation. Radiology 273:772–782
Batheja M, Vargas H, Silva AM, Walker F, Chang YH, De Petris G et al (2015) Magnetic resonance elastography (MRE) in assessing hepatic fibrosis: performance in a cohort of patients with histological data. Abdom Imaging 40:760-765
Chen J, Yin M, Talwalkar JA, Oudry J, Glaser KJ, Smyrk TC et al (2016) Diagnostic performance of MR elastography and vibration-controlled transient elastography in the detection of hepatic fibrosis in patients with severe to morbid obesity. Radiology. https://doi.org/10.1148/radiol.2016160685:160685
Yoshimitsu K, Mitsufuji T, Shinagawa Y, Fujimitsu R, Morita A, Urakawa H et al (2016) MR elastography of the liver at 3.0 T in diagnosing liver fibrosis grades; preliminary clinical experience. Eur Radiol 26:656–663
Wagner M, Besa C, Bou Ayache J, Yasar TK, Bane O, Fung M et al (2016) Magnetic resonance elastography of the liver: qualitative and quantitative comparison of gradient echo and spin echo echoplanar imaging sequences. Invest Radiol 51:575–581
Serai SD, Dillman JR, Trout AT (2017) Spin-echo echo-planar imaging MR elastography versus gradient-echo MR elastography for assessment of liver stiffness in children and young adults suspected of having liver disease. Radiology 282:761–770
Mariappan YK, Dzyubak B, Glaser KJ, Venkatesh SK, Sirlin CB, Hooker J et al (2017) Application of modified spin-echo-based sequences for hepatic MR elastography: evaluation, comparison with the conventional gradient-echo sequence, and preliminary clinical experience. Radiology 282:390–398
Kim YS, Song JS, Kannengiesser S, Seo SY (2017) Comparison of spin-echo echoplanar imaging and gradient recalled echo-based MR elastography at 3 Tesla with and without gadoxetic acid administration. Eur Radiol 27:4120–4128
Ichikawa S, Motosugi U, Enomoto N, Matsuda M, Onishi H (2016) Noninvasive hepatic fibrosis staging using mr elastography: The usefulness of the bayesian prediction method. J Magn Reson Imaging. https://doi.org/10.1002/jmri.25551
Loomba R, Cui J, Wolfson T, Haufe W, Hooker J, Szeverenyi N et al (2016) Novel 3D magnetic resonance elastography for the noninvasive diagnosis of advanced fibrosis in NAFLD: A Prospective Study. Am J Gastroenterol 111:986–994
Singh S, Venkatesh SK, Loomba R, Wang Z, Sirlin C, Chen J et al (2016) Magnetic resonance elastography for staging liver fibrosis in non-alcoholic fatty liver disease: a diagnostic accuracy systematic review and individual participant data pooled analysis. Eur Radiol 26:1431–1440
Singh S, Venkatesh SK, Wang Z, Miller FH, Motosugi U, Low RN et al (2015) Diagnostic performance of magnetic resonance elastography in staging liver fibrosis: a systematic review and meta-analysis of individual participant data. Clin Gastroenterol Hepatol 13:440–451 e446
Su LN, Guo SL, Li BX, Yang P (2014) Diagnostic value of magnetic resonance elastography for detecting and staging of hepatic fibrosis: a meta-analysis. Clin Radiol 69:e545–e552
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Kim KW, Lee J, Choi SH, Huh J, Park SH (2015) Systematic review and meta-analysis of studies evaluating diagnostic test accuracy: a practical review for clinical researchers-part I. General guidance and tips. Korean J Radiol 16:1175–1187
Lee J, Kim KW, Choi SH, Huh J, Park SH (2015) Systematic review and meta-analysis of studies evaluating diagnostic test accuracy: a practical review for clinical researchers-part II. Statistical methods of meta-analysis. Korean J Radiol 16:1188–1196
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH (2005) Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 58:982–990
Higgins JP, Green S (2011) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons
Deville WL, Buntinx F, Bouter LM, Montori VM, de Vet HC, van der Windt DA et al (2002) Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol 2:9
Cook RD (2000) Detection of influential observation in linear regression. Technometrics 42:65–68
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 58:882–893
Yin M, Talwalkar JA, Glaser KJ, Manduca A, Grimm RC, Rossman PJ et al (2007) Assessment of hepatic fibrosis with magnetic resonance elastography. Clin Gastroenterol Hepatol 5:1207–1213.e1202
Wang Y, Ganger DR, Levitsky J, Sternick LA, McCarthy RJ, Chen ZE et al (2011) Assessment of chronic hepatitis and fibrosis: comparison of MR elastography and diffusion-weighted imaging. AJR Am J Roentgenol 196:553–561
Godfrey EM, Patterson AJ, Priest AN, Davies SE, Joubert I, Krishnan AS et al (2012) A comparison of MR elastography and 31P MR spectroscopy with histological staging of liver fibrosis. Eur Radiol 22:2790–2797
Rustogi R, Horowitz J, Harmath C, Wang Y, Chalian H, Ganger DR et al (2012) Accuracy of MR elastography and anatomic MR imaging features in the diagnosis of severe hepatic fibrosis and cirrhosis. J Magn Reson Imaging 35:1356–1364
Choi YR, Lee JM, Yoon JH, Han JK, Choi BI (2013) Comparison of magnetic resonance elastography and gadoxetate disodium-enhanced magnetic resonance imaging for the evaluation of hepatic fibrosis. Invest Radiol 48:607–613
Kim D, Kim WR, Talwalkar JA, Kim HJ, Ehman RL (2013) Advanced fibrosis in nonalcoholic fatty liver disease: noninvasive assessment with MR elastography. Radiology 268:411–419
Shi Y, Guo Q, Xia F, Dzyubak B, Glaser KJ, Li Q et al (2014) MR elastography for the assessment of hepatic fibrosis in patients with chronic hepatitis B infection: does histologic necroinflammation influence the measurement of hepatic stiffness? Radiology 273:88–98
Venkatesh SK, Wang G, Lim SG, Wee A (2014) Magnetic resonance elastography for the detection and staging of liver fibrosis in chronic hepatitis B. Eur Radiol 24:70–78
Wu WP, Chou CT, Chen RC, Lee CW, Lee KW, Wu HK (2015) Non-invasive evaluation of hepatic fibrosis: the diagnostic performance of magnetic resonance elastography in patients with viral hepatitis B or C. PLoS One 10:e0140068
Chang W, Lee JM, Yoon JH, Han JK, Choi BI, Yoon JH et al (2016) Liver fibrosis staging with MR elastography: comparison of diagnostic performance between patients with chronic hepatitis B and those with other etiologic causes. Radiology 280:88–97
Cui J, Heba E, Hernandez C, Haufe W, Hooker J, Andre MP et al (2016) Magnetic resonance elastography is superior to acoustic radiation force impulse for the diagnosis of fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease: A prospective study. Hepatology 63:453–461
Eaton JE, Dzyubak B, Venkatesh SK, Smyrk TC, Gores GJ, Ehman RL et al (2016) Performance of magnetic resonance elastography in primary sclerosing cholangitis. J Gastroenterol Hepatol 31:1184–1190
Hennedige TP, Wang G, Leung FP, Alsaif HS, Teo LL, Lim SG et al (2016) Magnetic resonance elastography and diffusion weighted imaging in the evaluation of hepatic fibrosis in chronic hepatitis B. Gut Liver. https://doi.org/10.5009/gnl16079
Jang S, Lee JM, Lee DH, Joo I, Yoon JH, Chang W et al (2016) Value of MR elastography for the preoperative estimation of liver regeneration capacity in patients with hepatocellular carcinoma. J Magn Reson Imaging. https://doi.org/10.1002/jmri.25517
Park CC, Nguyen P, Hernandez C, Bettencourt R, Ramirez K, Fortney L et al (2017) Magnetic resonance elastography vs transient elastography in detection of fibrosis and noninvasive measurement of steatosis in patients with biopsy-proven nonalcoholic fatty liver disease. Gastroenterology 152:598–607 e592
Huwart L, Sempoux C, Vicaut E, Salameh N, Annet L, Danse E et al (2008) Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology 135:32–40
Asbach P, Klatt D, Schlosser B, Biermer M, Muche M, Rieger A et al (2010) Viscoelasticity-based staging of hepatic fibrosis with multifrequency MR elastography. Radiology 257:80–86
Bohte AE, de Niet A, Jansen L, Bipat S, Nederveen AJ, Verheij J et al (2014) Non-invasive evaluation of liver fibrosis: a comparison of ultrasound-based transient elastography and MR elastography in patients with viral hepatitis B and C. Eur Radiol 24:638-648
Imajo K, Kessoku T, Honda Y, Tomeno W, Ogawa Y, Mawatari H et al (2016) Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology 150:626–637.e627
Loomba R, Cui J, Wolfson T, Haufe W, Hooker J, Szeverenyi N et al (2016) Novel 3D magnetic resonance elastography for the noninvasive diagnosis of advanced fibrosis in NAFLD: A prospective study. American Journal of Gastroenterology 111:986–994
Sohrabpour AA, Mohamadnejad M, Malekzadeh R (2012) Review article: the reversibility of cirrhosis. Aliment Pharmacol Ther 36:824–832
Trout AT, Serai S, Mahley AD, Wang H, Zhang Y, Zhang B et al (2016) Liver stiffness measurements with mr elastography: agreement and repeatability across imaging systems, field strengths, and pulse sequences. Radiology 281:793–804
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ji Soo Song.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Funding
The authors state that this work has not received any funding.
Statistics and biometry
Professor HyeMi Choi from Department of Statistics, Chonbuk National University, kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
-
• retrospective
• observational
• performed at one institution
Electronic supplementary material
ESM 1
(DOCX 17331 kb)
Rights and permissions
About this article
Cite this article
Kim, Y.S., Jang, Y.N. & Song, J.S. Comparison of gradient-recalled echo and spin-echo echo-planar imaging MR elastography in staging liver fibrosis: a meta-analysis. Eur Radiol 28, 1709–1718 (2018). https://doi.org/10.1007/s00330-017-5149-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5149-5