Abstract
Objectives
To evaluate changes in liver function after right portal vein embolization (PVE) and extended right hemihepatectomy using gadolinium ethoxybenzyl-DTPA-enhanced (Gd-EOB-DTPA) MRI.
Methods
In this prospective trial, 37 patients undergoing PVE were examined before and 14 and 28 days after PVE and 10 days after extended hemihepatectomy using Gd-EOB-DTPA-enhanced MRI. Lobar volume, kinetic growth rate (KGR), relative enhancement (RE) as well as hepatocellular uptake index (HUI) and fat signal fraction (FSF) were calculated for each lobe.
Results
RE of the left liver lobe (LLL) was steadily increasing after PVE and decreased to 0.48 ± 0.19 10 days after surgery, which is significantly lower than 14 days and 28 days post PVE (P < 0.05). KGR was 14.06 ± 9.82%/week for the period from PVE to 14 days after PVE. HUI of the LLL increased steadily after PVE and was significantly higher at both 14 and 28 days after PVE compared to pre PVE (P < 0.05). HUI of the residual liver after surgery was lower than before.
Conclusions
Gd-EOB-DTPA-enhanced MRI may be used to monitor the functional increase in the FLR after PVE and to depict the intraoperative liver injury leading to a decrease in liver remnant function.
Key Points
• The most significant FLR volume increase happens within the first 14 days.
• No MRI parameter was able to predict the success of FLR growth.
• Our data suggest an early resection about 14 days after PVE.
• Routine Gd-EOB-DTPA-enhanced MRI might be suitable to replace ICG-test.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Portal vein embolization (PVE) is a well-established technique for redirecting portal blood flow to the future liver remnant (FLR) and thus initiating hypertrophy of the non-embolized segments [1–3]. This pretreatment decreases the risk of postoperative liver insufficiency in patients with extensive primary and secondary liver malignancies and too small an anticipated FLR [4, 5]. FLR hypertrophy is currently being measured using volumetry based on computed tomography (CT) or magnetic resonance imaging (MRI) to estimate the FLR volume and normalize this volume to the patient’s size [1, 4, 6–8]. While the expected increase in FLR function is assumed to linearly correlate with the increase in FLR volume, this gain is challenging to measure [9, 10]. One approach to predicting postoperative liver function and thereby reducing the risk of postoperative liver failure is to combine volumetric results with a global liver function test such as the indocyanine green (ICG) clearance or the LiMAx test. Global function tests are based on the assumption that liver function is the same throughout the liver [11, 12]. Therefore, the combination of volumetric and global liver function tests might be unsuitable for predicting FLR function after PVE because function is distributed unequally between left and right liver lobe [13–15]. Contrast-enhanced MRI using Gd-EOB-DTPA may have the potential to evaluate regional liver function and could therefore be an ideal diagnostic test for performing volumetric and functional measurement after PVE in one examination [10, 16–19].
The purpose of this study was to prospectively evaluate the change in volume and Gd-EOB-DTPA uptake in the hepatobiliary phase in the embolized and non-embolized liver lobes after portal vein embolization both before and after hemihepatectomy.
Materials and methods
All patients were presented to and discussed by an interdisciplinary tumour board, where the indication for extended right hemihepatectomy with prior portal vein embolization was approved. The study complied with the principles of the Declaration of Helsinki. The study protocol was approved by the institutional review board, patients received printed information about the study purpose and examinations, and written informed consent was obtained.
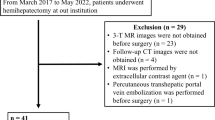
Inclusion and exclusion criteria
In this prospective trial we included patients who were scheduled for interventional PVE before extended hemihepatectomy. Patients with prior systemic chemotherapy or other therapies affecting the liver (surgical resection, transarterial chemoembolization, radiofrequency ablation, brachytherapy, radioembolization therapy) were excluded from the study.
MRI
Patients underwent MRI in a 1.5 Tesla Siemens Magnetom Avanto MRI scanner (Siemens Healthcare, Erlangen, Germany) 1 day prior to PVE, 14 and 28 days after PVE, and 10 days after surgery using an eight-channel body phased-array coil. Images were acquired with a sequence before and 20 min after manual bolus injection of 0.1 ml/kg body weight of Gd-EOB-DTPA (Primovist, Bayer Schering Pharma, Berlin, Germany). Images were obtained with a transverse breath-hold T1-weighted dual gradient-recalled echo (in-phase (IP)/out-of-phase (OP)) sequence (repetition time (TR)/echo time (TE)) typically, 290/4.84 ms and 2.16 ms. In addition, a volume-interpolated breath-hold examination sequence (VIBE) in an axial plane with a TR of 4.26 ms, a TE of 1.93 ms, a flip angle of 10°, a slice thickness of 3 mm and a matrix size of 256 × 127 was acquired covering the entire liver with 60–72 slices and an adjusted field of view (FOV) of 255–300 × 340–400 mm. A dose of 0.1 ml of Gd-EOB-DTPA (0.25 mmol/ml) per kg body weight was then manually injected into an anterior cubital vein, followed by a saline flush of 20 ml. After 20 min, in the hepatocyte phase, the same sequence was repeated.
PVE
PVE was performed via a CT- or ultrasound-guided ipsilateral percutaneous transhepatic access of the right portal vein (PV). After visualization of PV anatomy using direct portography, embolization of the postolateral and anteromedial branches was achieved using PVA particles (Contour, Boston Scientific). In addition, the main branch of the right PV was sealed using either a type I Amplatzer plug (St. Jude Medical, St. Paul, MN, USA) and/or large coils to seal the entry of the right branches. This was followed by portography to document the final result of the intervention. During retraction of the sheath, the puncture channel was sealed with 2 ml of fibrinogen (Tissucol Duo; Baxter, Deerfield, IL, USA) to prevent bleeding or bile leakage.
Image analysis
All measurements were performed by a clinical radiologist with 6 years of MRI experience in consensus with a hepatic surgeon involved in the patient’s surgery.
Signal intensity (SI) was measured using Visage 7.1.4 (Visage Imaging, Richmond, NSW, Australia). Avoiding large vessels, bile ducts or tumour masses, three regions of interest (ROIs) were placed in the left liver lobe (LLL), the right liver lobe (RLL) and the spleen in both the precontrast and the hepatobiliary phases using the 14-days-post-PVE images (Fig. 1). ROIs for LLL, RLL and spleen were then placed in the corresponding positions in the images taken before and 28 days after PVE as well as ROIs for the LLL and spleen 10 days after surgery. Relative enhancement (RE) was calculated according to the following formula:
A 66-year-old male with hilar cholangiocarcinoma. Image shows MRI with hepatobiliary phase after intravenous administration of Gd-EOB-DTPA 14 days after PVE. Three regions of interest were placed in the right and the left liver lobe as well as the spleen avoiding tumour, large vessels and bile ducts
The liver volume was determined by excluding tumour, large vessels and bile ducts, the liver as a whole and the LLL were delineated manually in the images acquired 14 or 28 days after PVE using the difference in enhancement as demarcation line. Transferring this line to the before-PVE images, TLV (total liver volume) and the volume of the LLL could be determined. From the 10-days-after-surgery images, the volume of the remaining liver tissue was measured and still labelled as LLL since parts of segment IV might have been preserved. The kinetic growth rate (KGR) was calculated using the following formula: KGR = degree of hypertrophy at post-PVE volume assessment (%) ÷ time elapsed since PVE (weeks) at post-PVE volume assessment according to Shindoh et al [20].
The hepatocellular uptake index (HUI) was calculated according to the following formula:
For calculation of VL (volume of liver) and SIL, the corresponding values of either the RLL or LLL were used.
Fat signal fraction (FSF(%)), of the RLL and LLL was calculated as described by Yoshimitsu et al. [21]:
where SI R/LLLIP is the signal intensity of the right or left liver lobe on in-phase (IP) images and SI R/LLLOP is signal intensity on the corresponding opposed-phase (OP) images of the T1-weighted dual gradient-recalled echo sequence. Negative values of SI FLRIP − SI FLROP were set to zero. Global FSF was calculated as the average FSF of RLL and LLL.
Statistical analysis
Statistical analysis was performed using SPSS Statistics 23 (IBM, Armonk, NY, USA). The Wilcoxon signed-rank test and repeated-measures ANOVA were used to evaluate differences in signal intensity, HUI, volumes and growth rate. Correlation analysis was performed using Pearson’s test. A P value of <0.05 was considered statistically significant. All quantitative data are expressed as mean ± standard deviation, unless otherwise indicated.
Results
Between January 2012 and December 2014, 37 patients (22 male, 15 female) with a mean age of 62.3 years (SD: 10.8) met the inclusion criteria. Twenty-four patients had cholangiocarcinoma, 11 had liver metastasis from colorectal cancer and one each had hepatocellular carcinoma (HCC) and large focal nodular hyperplasia (FNH). Total serum bilirubin at the time of PVE was 1.18 ± 1.41 mg/dl (range 0.3–7.4; normal value <1.2 mg/dl). Eight patients had elevated serum bilirubin (between 2.9 and 7.4 mg/dl) because of obstructive jaundice. All patients with cholangiocarcinoma and significant cholestasis in the left liver lobe (n = 13) received endoscopic stent placement to the left main duct before PVE. No patient had clinical or radiological signs of cirrhosis or renal impairment defined by a creatinine clearance lower than 50 ml/min Fig. 2 (Table 1).
A total of 131 MRI examinations were analysed. One patient did not undergo 14-days-post-PVE but 28-days-post-PVE MRI, six patients did not undergo 28-days-post-PVE MRI, and ten patients did not undergo 10-days-post-surgery MRI. Overall, 22 patients were examined at all four time points. Of the 37 patients, six patients did not receive extended hemihepatectomy because of extrahepatic disease which was revealed during laparoscopy. Four patients were not able to undergo post-surgery MRI because they were still in the intensive care unit.
Average time from PVE to surgery was 28.6 ± 6.6 days; average time from MRI 28 days after PVE to surgery was 4.0 ± 5.2 days.
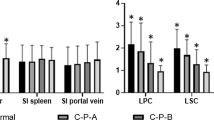
Relative enhancement
RE of the LLL was steadily increasing after PVE, although not statistically significantly, and decreased to 0.48 ± 0.19 10 days after surgery, which was significantly lower than 14 days and 28 days post PVE (P < 0.05) (Fig. 3). RE of the RLL was significantly lower at both 14 days and 28 days after PVE compared to baseline before PVE (P < 0.05) (Fig. 3). Serum bilirubin correlated negatively with RE of LLL and RLL (r 2 = −0.665 and −0.676; P < 0.05). Patient age correlated negatively with RE of the RLL 14 days post PVE (r 2 = −0.343; P < 0.05) and RE 10 days post surgery (r 2 = −0.557; P < 0.05) (Table 2).
Volume and kinetic growth rate
Average volume before PVE was 1,039.8 ± 343.6 cm3 (range 555–2,116) for RLL and 642.2 ± 168.9 cm3 (303–967) for LLL; residual liver volume after surgery was 1,061.6 ± 197.9 cm3 (Fig. 4).
Volume increase in the LLL 14 days and 28 days after PVE as well as 10 days after surgery compared with the volume before PVE was statistically significant (P < 0.05). The RLL decreased in size statistically significantly 14 days and 28 days after PVE (P < 0.05).
Kinetic growth rate was 14.06 ± 9.82%/week for the period from PVE to the 14-days-after-PVE measurement and 8.85 ± 4.95%/week for the period from PVE to the 28-days-after-PVE measurement. KGR from 14 days to 28 days after PVE was just 3.65 ± 3.56%/week (Fig. 5).
There was no significant correlation of SI or HUI with the KGR for the LLL (P = 0.32), but LLL volume before PVE showed a significantly negative correlation with KGR after 14 days and KGR after 28 days (r 2 = −0.47 and −0.62; P < 0.05). Serum bilirubin before PVE also did not correlate with KGR.
Hepatocellular uptake index
Average SI of the spleen in the HBP was 197 ± 36.4 before PVE, 201 ± 30.8 14 days after PVE and 205 ± 29.8 28 days after PVE. HUI of the LLL increased steadily after PVE and was significantly higher at both 14 and 28 days after PVE compared to pre PVE (P < 0.05). HUI of the residual liver after surgery was lower than after PVE but this was not statistically significant. HUI of the RLL was significantly lower both 14 days and 28 days after PVE compared to baseline before PVE (P < 0.05), but did not decrease significantly from 14 days to 28 days after PVE (Fig. 6). Serum bilirubin correlated negatively with HUI of LLL (r 2 = −0.535; P < 0.05) but not for RLL (r 2 = −0.306; P = 0.065). Patient age correlated negatively with HUI of the RLL before PVE (r 2 = −0.530; P < 0.05), HUI of the RLL 14 days after PVE (r 2 = −0.624; P < 0.05), HUI of the LLL 14 days after PVE (r 2 = −0.455; P < 0.05) and HUI 10 days post surgery (r 2 = −0.500; P < 0.05).
Fat signal fraction
Average FSF before PVE was 3.15 ± 7.74% for RLL and 2.72 ± 6.31% for LLL, global FSF was 2.93 ± 6.70%. There was no significant correlation of FSF (either RLL, LLL or global) with the KGR from PVE to 14 days after PVE (r 2 = −0.030; P = 0.861) or from PVE to 28 days after PVE (r 2 = −0.239; P = 0.195). Also, there was no significant correlation of FSF with RE or HUI at the corresponding time points.
Discussion
In this prospective study we evaluated the course of liver function after PVE using Gd-EOB-DTPA-enhanced MRI as a possible imaging-based liver function test in patients undergoing extended right hemihepatectomy. Our study shows that RE and HUI of the FLR increased steadily after PVE, while for HUI this increase was statistically significant; this is in line with preliminary results obtained 14 days after PVE [15]. Additionally, our results show that RE and HUI decrease after extended right hemihepatectomy compared with the results immediately before surgery.
Besides its possible application in multiple fields of hepatology, an imaging-based liver function test may allow better prediction of future liver remnant function (FLR-F) after hemihepatectomy and thus contribute to a reduction of posthepatecomy liver failure, which is still significant with around 14% [22]. Global liver function tests such as the LiMAx or ICG test may not provide an accurate picture in patients with regional dysfunction because of biliary atrophy following central cholangiocarcinoma or with heterogeneous distribution of functional and non-functional liver volume such as after PVE. Several methods of determining FLR-F have been proposed. De Graaf et al. used 99mTc-labelled mebrofenin scintigraphy combined with SPECT to show that the increase in FLR-F after PVE is higher than the increase in FLR volume [13, 14]. Further studies in humans and rats found an increase in uptake function or biliary excretion of ICG in the FLR after PVE [23–25]. An emerging technique for an imaging-based liver function is Gd-EOB-DTPA-enhanced MRI [19, 26]. The metabolization of Gd-EOB-DTPA in the body is similar to that of ICG and mebrofenin and its distribution in the liver can be measured with high temporal and spatial resolution [17, 27]. Additionally, MRI-based determination of liver function can be integrated into the routine preoperative workflow [28]. Several studies have proved the applicability of Gd-EOB-DTPA-enhanced MRI for the determination of liver function using several different parameters derived from pre- and post-contrast T1 sequences [17, 18, 26, 29–31].
Portal vein embolization introduces an artificial heterogeneity in the distribution of a patient’s liver function, and the inclusion of an MRI examination before PVE, as in our study, allows intraindividual assessment of the impact of PVE. Additionally, to our knowledge, this is the first study to include an MRI time point after hemihepatectomy [10, 16].
Our findings indicate that both RE and HUI of the FLR increase steadily after PVE. The most significant increase happens within the first 14 days, while the additional increase from 14 days to 28 days after PVE is no longer statistically significant. These results are in line with other published studies [15, 16] and provide an additional argument in favour of early resection after PVE, which is also desirable to minimize tumour progression. In fact, tumour progression can even be aggravated by growth stimulation after portal vein occlusion – ultimately leading to inoperability [4].
The MRI examination 10 days after surgery was conducted in 27 of the 37 patients; six patients did not undergo resection because of tumour progression and four patients were still in the ICU. It showed a significantly lower RE and HUI than the MRI before surgery, which took place an average of 4.0 ± 5.2 days before surgery. This decrease may be attributable to intraoperative hepatic pedicle clamping, resulting in liver ischaemia and parenchymal damage [32, 33]. Using HUI as a possible indicator, the resulting functional loss is about 11%; therefore we suggest taking an appropriate safety range into account when calculating FLR-F.
Another interesting finding concerns the prediction of growth rate using MRI findings before PVE. Barth et al. reported that liver fat content, but not function, derived from Gd-EOB-DTPA-enhanced MRI can serve as a predictor of FLR-growth after PVE. This conclusion is not corroborated by our findings. Neither FSF (either for RLL, LLL or global) nor RE or HUI show a correlation with the KGR, making it impossible to predict the success of PVE using individual MRI parameters. The only predictor we identified in our population was the LLL volume before PVE, which showed a significantly negative correlation with KGR.
We could partially reproduce the findings of Matoori et al., who reported an age dependence of hepatic signal enhancement with Gd-EOB-DTPA normalized to the enhancement in the spleen and skeletal muscle [34]. Negative correlation with age was however not only found for HUI (representing a normalization to the enhancement in the spleen) but also for RE alone, although the sample size is much smaller than in the referenced study. Further studies have to show if the cause of this effect is not solely the decrease in functional hepatic tissue in the elderly.
Our study has several limitations: first, we only used static measurement of signal intensity and neither dynamic measurement – which allows calculation of hepatic extraction fraction – nor T1 mapping – which yields more reproducible and transferable values. Second, we were unable to account for effects of renal function on the hepatic supply of Gd-EOB-DTPA. Gd-EOB-DTPA is eliminated both renally and hepatically, and reduced renal capacity can slightly increase hepatic enhancement [35, 36]. In our population, however, no patient had renal impairment defined by a creatinine clearance lower than 50 ml/min. Third, hyperbilirubinemia due to cholestasis could influence the results because of a competition of Gd-EOB-DTPA with bilirubin in the hepatocellular uptake transporters OATP1B1 and OATP1B3 [37, 38]. A subgroup analysis of patients without elevated bilirubin did, however, not show different overall results.
In conclusion, we postulate that Gd-EOB-DTPA-enhanced MRI may be used to monitor the functional increase in the FLR after PVE and to depict the intraoperative liver injury leading to a decrease in FLR function. The shift in hepatic Gd-EOB-DTPA uptake from the right to the left liver lobe takes place in the first 14 days after PVE with no further significant increase in the following 14 days, favouring early resection after PVE. Contrary to other studies, we identified no MRI parameter able to predict the success of FLR growth in our population. In summary, the Gd-EOB-DTPA-based liver function test opens the possibility of integrating functional information on a regional level in routine liver workup, but the optimal output parameter has yet to be identified.
Abbreviations
- FSF:
-
Fat signal fraction
- FLR:
-
Future liver remnant
- Gd-EOB-DTPA:
-
Gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid
- HUI:
-
Hepatic uptake index
- ICG:
-
Indocyanine green
- KGR:
-
Kinetic growth rate
- LiMAx:
-
Maximum liver function capacity
- LLL:
-
Left liver lobe
- PVE:
-
Portal vein embolisation
- RE:
-
Relative enhancement
- RLL:
-
Right liver lobe
- ROI:
-
Region of interest
- SI:
-
Signal intensity
- VIBE:
-
Volume interpolated breath-hold examination
References
Abdalla EK, Hicks ME, Vauthey JN (2001) Portal vein embolization: rationale, technique and future prospects. Br J Surg 88:165–175
Farges O, Belghiti J, Kianmanesh R et al (2003) Portal vein embolization before right hepatectomy: prospective clinical trial. Ann Surg 237:208
Nagino M, Kamiya J, Nishio H et al (2006) Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg 243:364–372
Madoff DC, Gaba RC, Weber CN et al (2016) Portal venous interventions: state of the art. Radiology 278:333–353
Ribero D, Abdalla EK, Madoff DC et al (2007) Portal vein embolization before major hepatectomy and its effects on regeneration, resectability and outcome. Br J Surg 94:1386–1394
Vauthey J-N, Abdalla EK, Doherty DA et al (2002) Body surface area and body weight predict total liver volume in Western adults. Liver Transpl 8:233–240
van Lienden KP, van den Esschert JW, de Graaf W et al (2012) Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol 36:25–34
Vauthey JN, Chaoui A, Do KA et al (2000) Standardized measurement of the future liver remnant prior to extended liver resection: methodology and clinical associations. Surgery 127:512–519
Hemming AW, Reed AI, Howard RJ et al (2003) Preoperative portal vein embolization for extended hepatectomy. Ann Surg 237:686–91– discussion 691–3
Sato Y, Matsushima S, Inaba Y et al (2015) Preoperative estimation of future remnant liver function following portal vein embolization using relative enhancement on gadoxetic acid disodium-enhanced magnetic resonance imaging. Korean J Radiol 16:523–530
Fazakas J, Mándli T, Ther G et al (2006) Evaluation of liver function for hepatic resection. Transplant Proc 38:798–800
Stockmann M, Lock JF, Riecke B et al (2009) Prediction of postoperative outcome after hepatectomy with a new bedside test for maximal liver function capacity. Ann Surg 250:119–125
de Graaf W, van Lienden KP, Dinant S et al (2010) Assessment of future remnant liver function using hepatobiliary scintigraphy in patients undergoing major liver resection. J Gastrointest Surg 14:369–378
de Graaf W, van Lienden KP, van den Esschert JW et al (2011) Increase in future remnant liver function after preoperative portal vein embolization. Br J Surg 98:825–834
Geisel D, Lüdemann L, Keuchel T et al (2013) Increase in left liver lobe function after preoperative right portal vein embolisation assessed with gadolinium-EOB-DTPA MRI. Eur Radiol 23:2555–2560. doi:10.1007/s00330-013-2859-1
Akiba A, Murata S, Mine T et al (2014) Volume change and liver parenchymal signal intensity in Gd-EOB-DTPA-enhanced magnetic resonance imaging after portal vein embolization prior to hepatectomy. Biomed Res Int 2014:684754–684757
Saito K, Ledsam J, Sourbron S et al (2013) Assessing liver function using dynamic Gd-EOB-DTPA-enhanced MRI with a standard 5-phase imaging protocol. J Magn Reson Imaging 37:1109–1114
Verloh N, Haimerl M, Zeman F et al (2014) Assessing liver function by liver enhancement during the hepatobiliary phase with Gd-EOB-DTPA-enhanced MRI at 3 Tesla. Eur Radiol 24:1013–1019
Geisel D, Lüdemann L, Hamm B, Denecke T (2015) Imaging-based liver function tests - past, present and future. Rofo. doi:10.1055/s-0035-1553306
Shindoh J, Truty MJ, Aloia TA et al (2013) Kinetic growth rate after portal vein embolization predicts posthepatectomy outcomes: toward zero liver-related mortality in patients with colorectal liver metastases and small future liver remnant. J Am Coll Surg 216:201–209
Yoshimitsu K, Kuroda Y, Nakamuta M et al (2008) Noninvasive estimation of hepatic steatosis using plain CT vs. chemical-shift MR imaging: significance for living donors. J Magn Reson Imaging 28:678–684
Robles R, Marín C, Lopez-Conesa A et al (2012) Comparative study of right portal vein ligation versus embolisation for induction of hypertrophy in two-stage hepatectomy for multiple bilateral colorectal liver metastases. Eur J Surg Oncol 38:586–593
Wakabayashi H, Ishimura K, Okano K et al (2002) Application of preoperative portal vein embolization before major hepatic resection in patients with normal or abnormal liver parenchyma. Surgery 131:26–33
de Graaf W, Bennink RJ, Heger M et al (2011) Quantitative assessment of hepatic function during liver regeneration in a standardized rat model. J Nucl Med 52:294–302
Uesaka K, Nimura Y, Nagino M (1996) Changes in hepatic lobar function after right portal vein embolization. An appraisal by biliary indocyanine green excretion. Ann Surg 223:77–83
Haimerl M, Verloh N, Fellner C et al (2014) MRI-based estimation of liver function: Gd-EOB-DTPA-enhanced T1 relaxometry of 3T vs. the MELD score. Sci Rep 4:5621. doi:10.1038/srep05621
Michaely HJ, Morelli JN, Budjan J et al (2013) CAIPIRINHA-Dixon-TWIST (CDT)-volume-interpolated breath-hold examination (VIBE): a new technique for fast time-resolved dynamic 3-dimensional imaging of the abdomen with high spatial resolution. Invest Radiol 48:590–597
Neri E, Bali MA, Ba-Ssalamah A et al (2016) ESGAR consensus statement on liver MR imaging and clinical use of liver-specific contrast agents. Eur Radiol 26:921–931
Haimerl M, Schlabeck M, Verloh N et al (2015) Volume-assisted estimation of liver function based on Gd-EOB-DTPA-enhanced MR relaxometry. Eur Radiol :1–9. doi:10.1007/s00330-015-3919-5
Nilsson H, Blomqvist L, Douglas L et al (2010) Assessment of liver function in primary biliary cirrhosis using Gd-EOB-DTPA-enhanced liver MRI. HPB (Oxford) 12:567–576
Nilsson H, Blomqvist L, Douglas L, et al (2013) Gd-EOB-DTPA-enhanced MRI for the assessment of liver function and volume in liver cirrhosis. Br J Radiol 86:20120653. doi:10.1259/bjr.20120653
Nuzzo G, Giuliante F, Giovannini I et al (2001) Liver resections with or without pedicle clamping. Am J Surg 181:238–246
Malinowski M, Lock JF, Seehofer D, et al (2015) Preliminary study on liver function changes after trisectionectomy with versus without prior portal vein embolization. Surg Today :1–9. doi:10.1007/s00595-015-1293-1
Matoori S, Froehlich JM, Breitenstein S et al (2016) Age dependence of spleen- and muscle-corrected hepatic signal enhancement on hepatobiliary phase gadoxetate MRI. Eur Radiol 26:1889–1894
Gschwend S, Ebert W, Schultze-Mosgau M, Breuer J (2011) Pharmacokinetics and imaging properties of Gd-EOB-DTPA in patients with hepatic and renal impairment. Invest Radiol 46:556–566
Talakic E, Steiner J, Kalmar P et al (2014) Gd-EOB-DTPA enhanced MRI of the liver: correlation of relative hepatic enhancement, relative renal enhancement, and liver to kidneys enhancement ratio with serum hepatic enzyme levels and eGFR. Eur J Radiol 83:607–611
Leonhardt M, Keiser M, Oswald S et al (2010) Hepatic uptake of the magnetic resonance imaging contrast agent Gd-EOB-DTPA: role of human organic anion transporters. Drug Metab Dispos 38:1024–1028
Pascolo L, Cupelli F, Anelli PL et al (1999) Molecular mechanisms for the hepatic uptake of magnetic resonance imaging contrast agents. Biochem Biophys Res Commun 257:746–752
Acknowledgements
The scientific guarantor of this publication is Dominik Geisel. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Some study subjects or cohorts have been previously reported in European Radiology. Methodology: prospective, observational/experimental, performed at one institution
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Geisel, D., Raabe, P., Lüdemann, L. et al. Gd-EOB-DTPA-enhanced MRI for monitoring future liver remnant function after portal vein embolization and extended hemihepatectomy: A prospective trial. Eur Radiol 27, 3080–3087 (2017). https://doi.org/10.1007/s00330-016-4674-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4674-y