Abstract
Objectives
To identify imaging algorithms and indications, CT protocols, and radiation doses in polytrauma patients in Swiss trauma centres.
Methods
An online survey with multiple choice questions and free-text responses was sent to authorized level-I trauma centres in Switzerland.
Results
All centres responded and indicated that they have internal standardized imaging algorithms for polytrauma patients. Nine of 12 centres (75 %) perform whole-body CT (WBCT) after focused assessment with sonography for trauma (FAST) and conventional radiography; 3/12 (25 %) use WBCT for initial imaging. Indications for WBCT were similar across centres being based on trauma mechanisms, vital signs, and presence of multiple injuries. Seven of 12 centres (58 %) perform an arterial and venous phase of the abdomen in split-bolus technique. Six of 12 centres (50 %) use multiphase protocols of the head (n = 3) and abdomen (n = 4), whereas 6/12 (50 %) use single-phase protocols for WBCT. Arm position was on the patient`s body during scanning (3/12, 25 %), alongside the body (2/12, 17 %), above the head (2/12, 17 %), or was changed during scanning (5/12, 42 %). Radiation doses showed large variations across centres ranging from 1268-3988 mGy*cm (DLP) per WBCT.
Conclusions
Imaging algorithms in polytrauma patients are standardized within, but vary across Swiss trauma centres, similar to the individual WBCT protocols, resulting in large variations in associated radiation doses.
Key Points
• Swiss trauma centres have internal standardized imaging algorithms for trauma patients
• Whole-body CT is most commonly used for imaging of trauma patients
• CT protocols and radiation doses vary greatly across Swiss trauma centres
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The initial diagnostic evaluation, including a rapid and precise physical examination of severely injured patients, represents an important element of structured trauma management. Traditionally, the imaging work-up of trauma patients consists of a focused assessment with sonography for trauma (FAST) and conventional radiography, eventually complemented by computed tomography (CT) of specific body regions [1, 2]. In the past decade, the concept of whole-body CT (WBCT) has gained increasing importance in the early phase of trauma care, gradually replacing ultrasound and conventional radiography [3–5].
Interestingly, there is still conflicting evidence regarding the proper use and indication of WBCT in the literature [6]. For example, in a recent systematic review, Surendran et al. [7] questioned the usefulness of WBCT in early trauma care regarding a reduction of mortality. Another issue that must be considered in regard to WBCT is the associated radiation dose. Most previous studies did not determine radiation doses of WBCT, but rather provided estimates or extrapolations [8]. However, it is mandatory to weigh the clinical usefulness of the technique against the radiation exposure and the small theoretical risk of cancer induction from ionizing radiation. We assume that many clinicians and radiologists alike may still be unfamiliar with the magnitude of radiation exposure that is received during a WBCT examination and with the factors that contribute to this radiation dose. This information, however, is critical for the development of strategies allowing for a reduction of patient exposure to be adherent to the as-low-as-reasonably-achievable (ALARA) principle.
Still there exist a number of different imaging algorithms and used modalities in the assessment of severely injured patients in different hospitals and countries. Smith et al. [9] showed for the UK that less than a quarter (22 %) of trauma centres implemented a WBCT-based algorithm and that hospitals having a higher volume of trauma patients were more likely to have algorithms including WBCT. Wiklund et al. [10] showed for several Nordic countries that 84 % of the hospitals had official guidelines for the indication of WBCT, but that there exist major differences in how WBCT was performed.
So far, it is not known which imaging algorithms for the initial radiologic evaluation are applied in trauma centres in Switzerland, including the knowledge about the use of different imaging modalities, including CT. In addition, none of the surveys mentioned above [9, 10] included a thorough assessment of associated radiation doses from WBCT in the various centres. Thus, the aim of this study was to identify the diversity of imaging algorithms in trauma patients, including indications for WBCT, specific protocols for WBCT, and the radiation doses in trauma centres in Switzerland.
Materials and Methods
We created an online survey about imaging algorithms in polytrauma patients in October 2015. It was reviewed and tested by a radiologist of our emergency radiology unit and a revised version was sent to the selected hospitals. Designated hospitals were the 12 level-I trauma centres in Switzerland being authorized to treat seriously injured patients with acute life-threatening injuries (according to the highly specialized medicine (HSM) directive, 2011 [11]). Participating radiologist being the section heads of emergency radiology in the respective hospitals were invited by email to undertake the web-based questionnaire devised using dedicated online software (www.surveymonkey.com). Hospitals that did not reply until December 2015 were reminded through email or phone call to ensure maximized answering frequency.
The survey comprised 25 multiple choice and free text response questions focusing on usage of imaging algorithms, imaging modalities, radiation dose exposures, CT and contrast media protocols, and patient’s alignment of the arms (see supplementary material, available online only). Additionally, information about the type of scanner and use of iterative image reconstruction were obtained.
At the beginning of the survey, the definition of polytrauma was provided to the radiologists as follows: Severely injured patient with two or more severe injuries in at least two areas of the body or two or more severe injuries in one body region [12].
To assess the radiation dose to trauma patients from CT we asked for the dose-length product (DLP, in mGy*cm). Hospitals were demanded to provide the average DLP of their WBCT protocol (head CT and body CT separately, the latter including the c-spine) of their last 10 polytrauma patients. Hospitals performing CT scans of selected body regions for initial radiologic evaluation were asked to provide the average DLP of the examined body area of their last 10 polytrauma patients.
To reach a conclusion, responders were asked about their opinion regarding the need for national or international guidelines concerning the imaging algorithms for polytrauma patients. In addition, they were asked if their department would be interested in adopting such new guidelines in the future.
Statistical methods
Summation of data for comparison was made using basic spreadsheet functions (Microsoft Excel 2010, Microsoft Corp, Redmond, WA, USA). Data from 16 of the 25 questions (64 %) were categorized as tick box answers (n = 5) or as yes/no answers (n = 11). In addition, quantitative variables were expressed as means ± standard deviation for normally distributed and as medians ± interquartile range for non-normally distributed values. Percentages were used for categorical parameters; free-text responses were captured (n = 9, 36 %).
The Mann-Whitney U test was used to test for differences regarding radiation dose exposure with different alignment of the patients’ arms. This test was also used for comparing the radiation dose with the split-bolus technique vs. no split-bolus technique. Multiphase CT acquisitions were compared with single-phase CT protocols regarding radiation dose exposure. Multiphase acquisition was defined as repetition of a CT scan of a certain body region at different contrast phases. A two-tailed p-value below 0.05 was considered statistically significant. Data were analyzed using commercially available software (IBM SPSS Statistics for Windows, Version 22.0, IBM Corp, Armonk, NY, USA).
Results
Response rate
Of the 12 participating trauma centres, all (100 %) completed the questionnaire. Initial response rate within our deadline was 75 %. The remaining centres answered the online survey until the end of January 2016.
Number of trauma patients and initial radiologic work-up
Centres were asked to indicate the average number of acute polytrauma patients, according to the definition mentioned above, treated per week in the past month who underwent imaging as part of their initial work-up. Six of the 12 centres (50 %) responded that they had more than 10 polytrauma patients per week, two centres (17 %) indicated 5-10 polytrauma patients per week, and four centres (33 %) less than 5 polytrauma patients per week.
An internal standardized imaging algorithm for polytrauma patients exists in each of the 12 centres. Eight of the 12 centres (67 %) use WBCT after FAST and conventional radiography for the initial radiologic work-up. One centre (8 %) uses WBCT after FAST and whole-body radiography (Lodox Xmplar-dr, Lodox Systems (Pty) Ltd, Johannesburg, South Africa). Of the eight centres using FAST for the initial radiologic imaging work-up, three (38 %) perform extended FAST for the additional rapid detection of pneumo- or hemothorax and pleural effusion. Three centres (25 %) perform initial WBCT without foregoing FAST and/or conventional radiography.
Criteria for performing WBCT
The criteria used for deciding whether WBCT should be performed are similar across centres and are based on the following criteria: mechanism of injury, abnormal vital signs, presence of multiple injuries, and use of the Abbreviated Injury Severity Score (AIS).
Three of the centres (25 %) used the criteria mentioned above except for the AIS score.
Protocols for WBCT
All centres routinely use intravenous contrast media. A fixed volume of contrast media is used in 10/12 centres (83 %), whereas two centres (17 %) adapt contrast media doses to the individual patient based on age, body weight, and renal function.
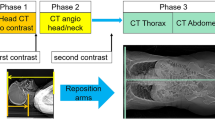
The CT protocols of all 12 centres are presented in Table 1. Six of the 12 centres (50 %) acquire WBCT in a single phase, and six centres (50 %) use multiple phases for their WBCT protocols. WBCT protocols with multiple phases are used for images of the head and abdomen (head: non-enhanced and arterial phase, n = 3, abdomen: arterial and venous phase, n = 4). Seven of the 12 trauma centres (42 %) avoid multiple phase acquisitions by using the split bolus technique for combining the arterial and the venous phase of enhancement into one spiral acquisition of the neck (n = 1), chest (n = 7), and abdomen (n = 7).
Renal excretory phase acquisitions are not implemented routinely in any centre, but are added to the protocol on an individual basis depending on the CT imaging findings.
Alignment of the arms
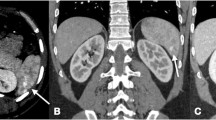
Five of the 12 centres (42 %) change the position of the arms during WBCT: Arms are placed on the patient’s body or parallel to the body while scanning the head and were repositioned above the head while scanning the torso.
Two centres (17 %) align the arms above the head during the entire WBCT scan, two centres (17 %) position the arms alongside the torso during the entire scan, and three centres (25 %) place the arms on the patient’s body ventral to the chest and upper abdomen during the entire scan (Fig. 1).
Radiation doses
The radiation doses of WBCT show a large variation among centres and range between 1268 and 3988 mGy*cm (DLP) per examination (Fig. 2). Doses of those WBCT protocols with arms positioned within the scan field-of-view (FoV) were higher than those with arms outside the scan FoV, however, the difference did not reach statistical significance (p = 0.58). Use of the split-bolus technique was associated with lower DLP values for the chest and abdomen compared to protocols without the split-bolus technique (p < 0.05). The radiation dose of WBCT protocols employing multiple phases was higher than those with a single phase only; however, the sample size was too small to reach statistical significance (p = 0.20) (Fig. 3).
CT scanners and use of iterative reconstructions
All centres used 64-slice or higher CT scanners for their polytrauma patients. Three centres (25 %) use a 64-slice CT system, eight (67 %) trauma centres use a 128-slice CT system, and one centre (8 %) use a 256-slice CT system. Nine centres (75 %) use a single-source CT machine and three (25 %) use a dual-source CT machine (operated in the single-source mode).
Iterative image reconstruction is a standard tool in nine centres (75 %), one centre (8 %) uses iterative image reconstruction in patients younger than 40 years only, and two centres (17 %) use filtered back projection reconstructions.
Need for national/international guidelines
Ten centres (83 %) indicated the need for developing national/international guidelines for imaging of polytrauma patients. Nine centres (75 %) are interested in adopting such national or international guidelines for imaging of their polytrauma patients (Fig. 4).
Discussion
Previous surveys performed in the United Kingdom and in Nordic European countries mainly focused on the number of hospitals with a WBCT-based trauma work-up and on WBCT reporting attitudes including the presence of the radiologist and the use of teleradiologic services [9, 10]. Other main issues were the location of the emergency radiology CT scanner [10], criteria for performing WBCT [9, 10], and radiation doses of WBCT averaged over all included hospitals [10].
Our study focused on imaging algorithms for the initial radiologic work-up in all authorized level-I trauma centres in Switzerland. We investigated into the usage of conventional radiography, FAST (including extended FAST), and CT in the resuscitation room, with a main interest in the order of using these modalities. Since WBCT was used in all trauma centres, we additionally evaluated the types of protocols and along with this, the variations in associated radiation doses from WBCT and the factors that contribute to these differences.
Despite conflicting data regarding the usefulness of WBCT [6, 7], the conventional imaging algorithm in trauma patients including FAST and conventional radiography is continuously challenged by WBCT, which is reflected by its increased use for the initial imaging evaluation [13]. Several studies have shown that WBCT as initial imaging modality is clinically feasible, allows for a reduction of time in the resuscitation room by avoiding other imaging techniques such as conventional radiography and that images obtained are of high quality [14, 15]. The more frequent use of WBCT requires the attention on the associated radiation exposure. Here, an individual risk/benefit analysis of using CT needs to be done, as, for example, severe injuries of the extremities may justify an extended scan length and hence a higher radiation dose.
The reported high utilization rate of WBCT was also reflected in our survey, where all centres did use WBCT as part of their imaging algorithm: 25 % of the centres use WBCT as the initial diagnostic tool, whereas 75 % use WBCT after foregoing FAST and radiography. Extended FAST was performed in 38 % of the centres, which represents an extension of traditional FAST for detecting pneumo- or hemothorax and pleural effusion in addition to intraperitoneal traumatic lesions. Ianniello et al. [16] showed that extended FAST has an excellent accuracy of 97.2 % for the detection of pneumothorax in trauma patients.
We found that the criteria for deciding whether or not to perform WBCT were similar across trauma centres and were comparable to the situation in the UK [9] and in Nordic countries [10]. Most of the centres use the mechanism of injury (100 %) and abnormal vital signs (100 %) as major criteria for deciding whether or not to perform WBCT, followed by the presence of multiple injuries (92 %) and by using a trauma score (67 %).
As reflected by the results of our survey, there still exists no consensus about the specific CT protocol for trauma patients. Two recent studies indicated that a biphasic acquisition including an arterial and venous phase of enhancement is necessary for detecting traumatic contained vascular injuries of the spleen [17, 18]. In line with this, 92 % of the trauma centres in Switzerland perform a biphasic acquisition of the abdomen. Interestingly, 58 % of the centres use the split-bolus technique for obtaining both contrast phases in one acquisition. Although this technique combines the benefit of faster image acquisition and radiation dose reduction, Stedman et al. [19] recently raised concerns regarding this technique because of splenic heterogeneity potentially affecting image interpretation.
Alignment of the arms during CT scanning represents a major issue in trauma imaging affecting image quality, speed of data acquisition, and radiation dose [20, 21]. While several studies showed that positioning of the arms alongside the patient’s body increases radiation dose exposure and decreases image quality [20–23], there is still no agreement about the most appropriate position of the arms, which is also reflected by the results of our survey. Karlo et al. [24] showed a significantly better image quality of the liver and spleen when positioning the arms on a pillow ventrally to the chest compared to aligning the arms alongside the patient’s body. The downside of including the arms in the scan FoV is the significant increase in radiation dose, being approximately 20 %, according to Karlo et al. [24], and 18 %, according to Brink et al. [20]. That is explained by the higher tube current through the use of automatic attenuation-based tube current modulation.
Radiation dose of WBCT showed major differences across all investigated trauma centres, with doses almost doubling when comparing the centre with lowest to that with highest dose. As expected, DLP values were higher for those protocols including the arms in the scan FoV and for those who use multiple phases and were lower in protocols employing the split-bolus technique. Another reason for the observed variations in radiation dose is the different use of iterative image reconstructions, which were not used by two centres and were used only in patients below 40 years of age in one centre.
Based on these differences in doses being paralleled by variations in protocols and arm alignment, the development of guidelines for WBCT imaging in trauma patients should be encouraged. Such guidelines – to our knowledge existing only for head CT in trauma patients [25], but not for WBCT – would guarantee updated protocols in all centres with optimized radiation exposure. Based on our survey, 75 % of centres would be interested in adopting such new guidelines.
The following study limitations must be acknowledged. First, to determine more detailed radiation dose exposures for trauma patients, DLP values of each single body region would have been required. However, because many centres scan two or more body regions in the same spiral acquisition, such values cannot be obtained. Second, our study points-out the present usage of imaging algorithms in trauma patients and provides neither solutions regarding the appropriate use of WBCT nor answers about the effect of WBCT on patient outcome. The questionnaire did not include questions about the delivery of care to trauma patients nor about the location of the CT scanner [26]. Also, the survey did not contain questions about the use of WBCT in hemodynamically instable patients. All these factors affect the decision whether or not to perform WBCT and may also influence the CT protocols.
Finally, our study was performed in trauma centres of a relatively small European country with currently 8.4 million inhabitants and a relatively well developed infrastructure (indicated by the fact that all centres used 64-slice and higher CT scanners) and health care system. Thus, our results may not be generalizable to other countries.
In conclusion, imaging algorithms in polytrauma patients are standardized within, but vary across trauma centres in Switzerland. The same holds true for individual WBCT protocols, which results in considerable variations in associated radiation exposure to trauma patients. The development of guidelines regarding WBCT protocols, based on scientific evidence, is strongly encouraged.
Abbreviations
- WBCT:
-
Whole-body computed tomography
- FAST:
-
Focused assessment with sonography for trauma
- DLP:
-
Dose-length product
References
Bernhard M, Becker TK, Nowe T et al (2007) Introduction of a treatment algorithm can improve the early management of emergency patients in the resuscitation room. Resuscitation 73:362–373
Wintermark M, Poletti P-A, Becker CD, Schnyder P (2002) Traumatic injuries: organization and ergonomics of imaging in the emergency environment. Eur Radiol 12:959–968
Huber-Wagner S, Lefering R, Qvick L-M et al (2009) Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet 373:1455–1461
Poletti P-A, Wintermark M, Schnyder P, Becker CD (2002) Traumatic injuries: role of imaging in the management of the polytrauma victim (conservative expectation). Eur Radiol 12:969–978
Linsenmaier U, Krotz M, Hauser H et al (2002) Whole-body computed tomography in polytrauma: techniques and management. Eur Radiol 12:1728–1740
Wurmb TE, Frühwald P, Hopfner W, Roewer N, Brederlau J (2007) Whole-body multislice computed tomography as the primary and sole diagnostic tool in patients with blunt trauma: searching for its appropriate indication. Am J Emerg Med 25:1057–1062
Surendran A, Mori A, Varma DK, Gruen RL (2014) Systematic review of the benefits and harms of whole-body computed tomography in the early management of multitrauma patients: are we getting the whole picture? J Trauma Acute Care Surg 76:1122–1130
Gordic S, Alkadhi H, Hodel S et al (2015) Whole-body CT-based imaging algorithm for multiple trauma patients: radiation dose and time to diagnosis. Br J Radiol 88:20140616
Smith CM, Mason S (2012) The use of whole-body CT for trauma patients: survey of UK emergency departments. Emerg Med J 29:630–634
Wiklund E, Koskinen SK, Linder F, Aslund PE, Eklof H (2016) Whole body computed tomography for trauma patients in the Nordic countries 2014: survey shows significant differences and a need for common guidelines. Acta Radiol 57:750–757
Heller MT, Kanal E, Almusa O et al (2014) Utility of additional CT examinations driven by completion of a standard trauma imaging protocol in patients transferred for minor trauma. Emerg Radiol 21:341–347
Tscherne H, Oestern HJ, Sturm JA (1984) Stress tolerance of patients with multiple injuries and its significance for operative care. Langenbecks Arch Chir 364:71–77
Larson DB, Johnson LW, Schnell BM, Salisbury SR, Forman HP (2011) National trends in CT use in the emergency department: 1995-2007. Radiology 258:164–173
Ptak T, Rhea J, Novelline R (2001) Experience with a continuous, single-pass whole-body multidetector CT protocol for trauma: the three-minute multiple trauma CT scan. Emerg Radiol 8:250–256
Fanucci E, Fiaschetti V, Rotili A, Floris R, Simonetti G (2007) Whole body 16-row multislice CT in emergency room: effects of different protocols on scanning time, image quality and radiation exposure. Emerg Radiol 13:251–257
Ianniello S, Di Giacomo V, Sessa B, Miele V (2014) First-line sonographic diagnosis of pneumothorax in major trauma: accuracy of e-FAST and comparison with multidetector computed tomography. La Radiologia Medica 119:674–680
Boscak AR, Shanmuganathan K, Mirvis SE et al (2013) Optimizing trauma multidetector CT protocol for blunt splenic injury: need for arterial and portal venous phase scans. Radiology 268:79–88
Uyeda JW, LeBedis CA, Penn DR, Soto JA, Anderson SW (2014) Active hemorrhage and vascular injuries in splenic trauma: utility of the arterial phase in multidetector CT. Radiology 270:99–106
Stedman JM, Franklin JM, Nicholl H, Anderson EM, Moore NR (2014) Splenic parenchymal heterogeneity at dual-bolus single-acquisition CT in polytrauma patients-6-months experience from Oxford, UK. Emerg Radiol 21:257–260
Brink M, de Lange F, Oostveen LJ et al (2008) Arm raising at exposure-controlled multidetector trauma CT of thoracoabdominal region: higher image quality, lower radiation dose. Radiology 249:661–670
Bayer J, Pache G, Strohm PC et al (2011) Influence of arm positioning on radiation dose for whole body computed tomography in trauma patients. J Trauma 70:900–905
Leidner B, Adiels M, Aspelin P, Gullstrand P, Wallen S (1998) Standardized CT examination of the multitraumatized patient. Eur Radiol 8:1630–1638
Nguyen D, Platon A, Shanmuganathan K, Mirvis SE, Becker CD, Poletti PA (2009) Evaluation of a single-pass continuous whole-body 16-MDCT protocol for patients with polytrauma. AJR Am J Roentgenol 192:3–10
Karlo C, Gnannt R, Frauenfelder T et al (2011) Whole-body CT in polytrauma patients: effect of arm positioning on thoracic and abdominal image quality. Emerg Radiol 18:285–293
Castillo M (2006) Neuroradiology companion: methods, guidelines, and imaging fundamentals, 3rd edn., Lippincott Williams & Wilkins Philadelphia
Saltzherr T, Bakker F, Beenen L, Dijkgraaf M, Reitsma J, Goslings JC (2012) Randomized clinical trial comparing the effect of computed tomography in the trauma room versus the radiology department on injury outcomes. Br J Surg 99:105–113
Acknowledgements
The scientific guarantor of this publication is Hatem Alkadhi. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Informed consent was not required because the study represents a national survey, and no patient data were handled for this manuscript. None of the subjects have been previously reported.
Methodology: retrospective, observational, multicenter study.
We would like to thank Dr. Christopher M Smith, author of a survey in the UK, and Dr. Hampus Eklöf, author of a survey in Nordic countries, for providing us their questionnaires. We thank also Dr. Alexandra Platon, Geneva, and Dr. Daniel Ott, Bern, for supporting our project.
Author information
Authors and Affiliations
Corresponding author
Additional information
P.-A. Poletti and H. Alkadhi on behalf of the Swiss Society of Emergency Radiology.
Rights and permissions
About this article
Cite this article
Hinzpeter, R., Boehm, T., Boll, D. et al. Imaging algorithms and CT protocols in trauma patients: survey of Swiss emergency centers. Eur Radiol 27, 1922–1928 (2017). https://doi.org/10.1007/s00330-016-4574-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4574-1