Abstract
Objectives
To compare interobserver agreements among multiple readers and accuracy for the assessment of solid components in subsolid nodules between the lung and mediastinal window settings.
Methods
Seventy-seven surgically resected nodules with solid components smaller than 8 mm were included in this study. In both lung and mediastinal windows, five readers independently assessed the presence and size of solid component. Bootstrapping was used to compare the interobserver agreement between the two window settings. Imaging-pathology correlation was performed to evaluate the accuracy.
Results
There were no significant differences in the interobserver agreements between the two windows for both identification (lung windows, k = 0.51; mediastinal windows, k = 0.57) and measurements (lung windows, ICC = 0.70; mediastinal windows, ICC = 0.69) of solid components. The incidence of false negative results for the presence of invasive components and the median absolute difference between the solid component size and the invasive component size were significantly higher on mediastinal windows than on lung windows (P < 0.001 and P < 0.001, respectively).
Conclusions
The lung window setting had a comparable reproducibility but a higher accuracy than the mediastinal window setting for nodule classifications and solid component measurements in subsolid nodules.
Key Points
• Reproducibility was similar between the two windows in nodule classifications.
• Reproducibility was similar between the two windows in solid component measurements.
• Accuracy for solid component assessment was higher on lung windows.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Peripheral adenocarcinomas are the most common type of lung cancer being diagnosed with an increasing frequency, which account for 30 − 35 % of all primary lung tumours [1]. The increasing frequency of adenocarcinomas may be in part attributed to the growing use of chest computed tomography (CT) and a corresponding increase in the detection rate of early adenocarcinomas manifesting as persistent subsolid nodules.
Subsolid nodules represent a wide spectrum of pathology, ranging from pre-invasive lesions such as atypical adenomatous hyperplasia (AAH) and adenocarcinoma in situ (AIS) to invasive lesions including minimally invasive adenocarcinoma (MIA) [2]. The pre-invasive lesions usually appear as pure ground-glass nodules (GGNs), especially when the lesion size is small, while the invasive lesions typically contain solid components of various sizes, which reflect invasive components on pathology [2–9].
In a recent study, the maximal diameter of the solid component only has been shown to be a better prognostic indicator than the maximal diameter of the whole lesion in part-solid nodules [10]. Therefore, accurate evaluation of solid components is considered as key to establishing optimal management plan for subsolid nodules. In particular, accumulating evidence of the indolent nature of pure GGNs and part-solid nodules with solid components less than 5 mm in size has suggested that conservative management may be indicated for the nodules [2].
However, assessing the presence or absence and the size of solid components in subsolid nodules may be challenging due to their small sizes and is inevitably subject to interobserver variability [11, 12]. Lack of a standardised approach may complicate the assessment of solid components. At present, the Fleischner Society recommends using the mediastinal window setting for this assessment [13], while Lung RADS recommends using the lung window setting for measuring nodules [14]. Based on the previous finding that disagreements on the presence and size of a solid component were the main sources of discrepancies in nodule categorisation [15], it would be essential to recommend using the same window setting for assessing subsolid nodules, because the interobserver variability would further increase if observers use different window settings. In this context, it has been reported that both the accuracy and interobserver agreement among the two readers for solid component measurements did not significantly differ between lung and mediastinal windows [16]. To our knowledge, however, in-depth investigation of the difference in interobserver agreements for the nodule classifications and solid component measurements between the two window settings has not yet been conducted.
The purpose of this study was to compare interobserver agreements among multiple readers and accuracy for the assessment of solid components in subsolid nodules between the lung and mediastinal window settings.
Materials and methods
This retrospective study was approved by our institutional review board, and informed consent was waived.
Patient selection
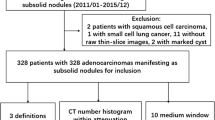
One hundred and two subsolid consecutive nodules, which were surgically resected between April 2013 and April 2015, were selected from our radiology report database. Prior to the surgery, sizes of the entire nodules and their solid components on preoperative chest CT scans were measured by one experienced radiologist (J.M.G. with 25 years of experience). Of the 102 nodules, 25 nodules with solid components larger than 8 mm were excluded. For the inclusion criteria, a cut-off value for the solid component was chosen as 8 mm, given that 8 mm is the threshold discriminating the 4A and 4B categories (i.e. suspicious category with findings for which additional diagnostic testing and/or tissue sampling is recommended) in Lung-RADS (Version 1.0) [14] and that the effect of interobserver variability is less apparent if the solid components are relatively large.
Finally, 77 nodules from 76 patients (32 men [mean age, 63 years; age range, 45–75 years] and 44 women [mean age, 55 years; age range, 33–72 years]) were included in this study. Part of the patient population in this study (n = 19) overlap with those in the previous study [16].
Image acquisition
Four CT scanners were used to obtain preoperative chest CT scans: Sensation 16 (Siemens Medical Solutions, Forchheim, Germany), Somatom Definition (Siemens Medical Solutions, Forchheim, Germany), LightSpeed Ultra (GE Healthcare, Milwaukee, WI, USA), and Brilliance 64 (Philips Medical Systems, Best, The Netherlands). Given the retrospective design of this study, various CT protocols were used including low-dose (n = 53) and standard-dose (n = 24) CT protocols with (n = 41) or without (n = 36) contrast administration, with the tube current ranging from 20 to 40 mAs for the low-dose and from 200 to 400 mAs for the standard-dose techniques at a fixed tube voltage of 120 kV. All CT images were reconstructed using the high-frequency algorithm with a section thickness of 0.625 − 1.25 mm. The field of view was optimised for the patient’s size and ranged from 300 to 350 mm. CT images were obtained in the supine position at full inspiration for all patients.
Image analysis
All CT scans were reviewed by five independent readers (R.E.Y., E.J.H, S.H.Y., C.M.P. and C.H.L. with 5, 4, 10, 14 and 20 years of experience, respectively), who were blinded to pathologic diagnosis, on a picture archiving and communication system workstation (Infinitt Healthcare, Seoul, Korea).
With regard to the nodule classifications (i.e. pure GGN or part-solid nodule), the presence or absence of solid component was first visually determined on a representative axial section of each nodule in both lung (window width, 1,500 HU; level, -700 HU) and mediastinal (window width, 400 HU; level, 30 HU) window settings. Because the nodules were assessed on both windows, the presence of ground-glass components in the nodules could be appreciated on lung windows. A nodule was classified as a GGN on mediastinal windows if there was a ground-glass component on lung windows but no demonstrable solid component on mediastinal windows. The representative axial section for each nodule was chosen by one experienced radiologist (J.M.G. with 25 years of experience) such that the section would contain the longest diameter of the solid component.
Cases in which there was discordance in nodule classifications between the lung and mediastinal windows were reviewed and the potential reasons for the discordance were categorised by one experienced radiologist (J.M.G.): (1) small-sized solid component, (2) intermediate attenuation (between completely ground-glass and completely solid) of solid components and (3) prominent vessels within the subsolid nodules.
Subsequently, one-dimensional measurements of the nodule sizes were performed by the five readers. The longest diameters of the solid components, if present, were measured on the representative sections in both window settings. In addition, overall sizes of the nodules (the longest diameters of the whole nodules including the ground-glass components) were measured on the representative sections in the lung window setting. Although contiguous axial CT sections containing the entire nodules were provided to the readers to help differentiate solid components from vessels, the readers were instructed to perform both the nodule classifications and solid component measurements on preselected representative sections to minimise other sources of variability.
Pathology measurement
The longest diameter of tumour was measured on gross specimen by using a ruler in most cases. However, when the entire tumour was small enough to be mounted on pathological slides, it was measured on a representative slide containing the largest cross-section of the tumour under light microscopy. An invasive component was measured with a ruler under light microscopy. In cases with invasive components larger than 10 mm, exact sizes were not provided on pathology reports and the sizes of the invasive components were simply reported to be larger than 10 mm.
Statistical analysis
All statistical analyses were performed with R software (version 3.2.0; http://www.r-project.org/). Results with P values less than 0.05 were considered statistically significant.
Comparison of interobserver agreements in the lung and mediastinal window settings
Fleiss kappa and intraclass correlation coefficients were calculated to determine interobserver agreements for the nodule classifications and solid component measurements, respectively, in both lung and mediastinal window settings. A k value or ICC of 0.00–0.20 was considered to indicate slight agreement, 0.21–0.40 fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 substantial agreement and 0.81–1.00 almost perfect agreement [17].
Interobserver agreements in the two window settings were compared using 95 % confidence intervals (CI) derived from 1,000 boot strapping replications. The results were considered to be significant if the 95 % CI for the difference between the two kappa values or ICCs did not include 0 [18].
Imaging-pathology correlation
The incidence of cases in which the presence or size of the invasive component was either underestimated or overestimated on CT with respect to the pathology was compared between the lung and mediastinal window settings by using the McNemar’s test.
In addition to Friedman test and Wilcoxon signed rank test, linear mixed model analysis was performed to compare the difference between the solid component size and the invasive component size according to window settings.
Results
Pathological findings of nodules
All nodules were surgically resected by lobectomy (n = 14), segmentectomy (n = 22), wedge resection (n = 40), and combined segmentectomy and wedge resection (n = 1). Pathological diagnoses of the nodules were as follows: AAH (n = 3), AIS (n = 8), MIA (n = 27), invasive adenocarcinoma (n = 35), focal fibrosis (n = 1), meningothelial hyperplasia (n = 1), anthracofibrotic lesion (n = 1), and inflammatory myofibroblastic tumour (n = 1). On the pathology, the median overall size of the 73 premalignant, pre-invasive, and invasive lesions for lung adenocarcinoma was 12 mm (interquartile range, 9-14).
Comparison of the lung and mediastinal window settings
Results of the nodule classifications and CT measurements are summarised in Table 1. With regard to the nodule classifications, the results for the potential reasons for discordance between the lung and mediastinal window settings are provided in Table 1. In 19 nodules, there was at least one discordant result between the lung and mediastinal window settings among the five readers. The discordant nodule classifications between lung and mediastinal windows are shown in Table 2.
Interobserver agreements were moderate for the nodule classifications and substantial for the solid component measurements in both lung (k = 0.51 and ICC = 0.70) and mediastinal (k = 0.57 and ICC = 0.69) window settings (Figs. 1, 2, and 3). There were no significant differences in the interobserver agreements between the two window settings with respect to both the nodule classifications (95 % CI, -0.22, 0.12) and solid component measurements (95 % CI, -0.14, 0.16).
Case with a high interobserver agreement on both lung (a) and mediastinal (b) windows. The subsolid nodule was interpreted as a part-solid nodule by all five readers in both window settings. The size of the solid component (arrow) was measured to be 5 mm by three readers, 4 mm by one reader and 6 mm by one reader on lung windows, while it was measured to be 3 mm by three readers and 4 mm by two readers on mediastinal windows
Case with a low interobserver agreement on both lung (a) and mediastinal (b) windows. In both window settings, the subsolid nodule was interpreted as a part-solid nodule by two readers and as a GGN by three readers. On the retrospective review by a single experienced radiologist, difficulty in differentiating a solid component from a vessel has been suggested as a potential reason for the discrepant readings
Case with a lower interobserver agreement on lung windows (a) compared with mediastinal windows (b). a On lung windows, a small area of equivocally increased attenuation (arrow) was interpreted as a solid component by three of the five readers. b On mediastinal windows, the nodule was classified as a pure GGN by all five readers
Imaging-pathology correlation
CT prediction of the presence of invasive components
Thirteen nodules (benign or premalignant lesions [n = 7]; nodules for which the presence or absence of invasive components were not reported on pathology [n = 6]) were excluded from the analysis. Pathological diagnoses of the remaining 64 nodules were AIS (n = 8), MIA (n = 27), and invasive adenocarcinoma (n = 29).
Given that an invasive component of adenocarcinoma is generally solid on CT, a false negative result corresponds to the case in which an invasive component was present on pathology although there was no discernible solid component on CT. In contrast, a false-positive result corresponds to the case in which an invasive component was absent on pathology despite the presence of definite solid component on CT. False negative results for the presence of invasive component were significantly more common in the mediastinal window setting than in the lung window setting (P < 0.001) (Fig. 4). There was no significant difference in the incidence of false positive results between the two window settings (Table 3).
CT prediction of the size of invasive components
Thirty-two nodules (benign or premalignant lesions [n = 7]; nodules for which the presence or absence of invasive components was not reported on pathology [n = 6]; nodules for which only the ranges, and not the specific sizes, were given on pathology [n = 11]) were excluded from the analysis. Pathological diagnoses of the 53 nodules were AIS (n = 8), MIA (n = 27), and invasive adenocarcinoma (n = 18). On the pathology, the median sizes of the tumour and invasive components were 11.0 mm (interquartile range, 9.0-14.0) and 4.0 mm (interquartile range, 2.0-6.0), respectively.
There were significant differences between the solid component size and the invasive component size in both window settings (2.2 mm [interquartile range, 0.2- 4.4] for lung windows versus 4.0 mm [interquartile range, 2.0-6.0] for pathology, P = 0.001; 0.8 mm [interquartile range, 0.0-2.5] for mediastinal windows versus 4.0 mm [interquartile range, 2.0- 6.0] for pathology, P < 0.001). However, the median absolute difference between the solid component size and the invasive component size was significantly larger in the mediastinal window setting than in the lung window setting (2.0 mm [interquartile range, 1.2-3.7] and 1.8 mm [interquartile range, 0.6-2.8], respectively; P < 0.001). In addition, the median solid component size on lung windows differed significantly from that on mediastinal windows (P < 0.001) (Table 3).
Discussion
With regard to the evaluation of lung adenocarcinomas manifesting as subsolid nodules, the initial step is to determine the presence or absence of solid components within the nodules, which reflect invasive components on pathology. Accumulating evidence suggests that subsolid nodules may be managed differently according to the presence or absence of solid components. Part-solid nodules warrant an aggressive diagnostic approach owing to its sufficiently greater likelihood of being malignant, except those with solid components measuring 5 mm or less, which frequently correspond to either AIS or MIA [19, 20]. As for pure GGNs, based on the results from a large prospective cohort [International Early Lung Cancer Action Program (I-ELCAP)], Yankelevitz et al. [21] have recently recommended that the nodules of any size can be safely followed with annual repeat scans to monitor transition to part-solid nodules and pathological diagnosis may be delayed until the development of solid components as the earlier treatment provides no additional benefit. In cases with part-solid nodules, the exact sizes of solid components are also of interest, given their close relationship to the prognosis of the patients. Several previous studies have proven that the solid component size may have a higher prognostic value than the total size of subsolid nodules [4, 10, 22–25].
In parallel to increasing emphasis placed on solid components as the key determinant of the prognosis and optimal management of patients with the subsolid nodules, there has been a growing interest in establishing a standardised approach for assessing the solid components [26–33]. In particular, although the mediastinal window setting is the one recommended to be used by the Fleischner Society at the present time, lack of evidence for the inferiority of the lung window setting, compared with the mediastinal window setting, has prompted a further investigation in this study.
First, for evaluation of the reproducibility, we compared interobserver agreements among multiple readers with respect to the nodule classifications and the solid component measurements between lung and mediastinal windows. Both window settings showed moderate agreements for the nodule classifications and substantial agreements for the solid component measurements. Low interobserver agreement was noted for cases in which there was a difficulty in distinguishing a solid component from a vessel, regardless of the window setting (Fig. 2). In addition, interobserver agreement for the nodule classifications was found to be slightly lower on lung windows than on mediastinal windows, partly because the area of equivocally increased attenuation on lung windows, which may have posed a diagnostic dilemma to some readers, appeared completely ground-glass on mediastinal windows (Fig. 3). However, there were no significant differences in the interobserver agreements between the two window settings. The results are in keeping with those of the previous study, which demonstrated no significant difference in the interobserver agreement among two observers for solid component measurements between the two window settings [16]. Our results confirm the previous findings with stronger evidence provided by larger numbers of nodules and readers.
As for the accuracy, the mediastinal window setting tended to underestimate the presence and size of invasive components, compared with the lung window setting. Higher false negative rate on mediastinal windows can be attributed to the fact that invasive components do not always manifest as dense solid components on CT. Invasive components may have various CT morphology, ranging from ground-glass to solid. In a previous study pertaining to annual follow-up screening CT of non-solid nodules, pathological evidence of stromal invasion was found to be present in 52 of 62 (84 %) nodules which remained non-solid prior to resection. Since it is impossible to discriminate ground-glass invasive components from the lepidic growth, the invasive components appearing ground-glass are inevitably underestimated in both lung and mediastinal windows. However, invasive components with intermediate attenuation between completely ground-glass and completely solid are likely to be underestimated in mediastinal windows but not in lung windows.
Meanwhile, the incidence of overestimation of the invasive components turned out to be significantly higher on lung windows than on mediastinal windows, although false-positive rates for the presence of invasive components did not significantly differ between the two windows. It has been speculated that inadequately inflated status of the lung tissue after resection and tissue processing may have an influence on pathology measurements and may cause tumour sizes to be measured smaller, compared with CT measurements [34]. Given that solid components were measured significantly larger on lung windows than on mediastinal windows in both the previous and present studies [16], it might not be surprising that the incidence of overestimation of the invasive components was significantly higher in the lung window setting.
In addition, we found the median difference between the solid component size and the invasive component size to be significantly larger on mediastinal windows than on lung windows, despite the presence of significant differences between the solid component size and the invasive component size in both window settings. Based on the findings, it is inferred that the accuracy of the nodule classification and solid component measurement may be higher on lung windows than on mediastinal windows. In the previous study by Lee et al. [16], however, the accuracy for solid component measurements in lung windows was not shown to significantly differ that in mediastinal windows. Our results may differ from those of the previous study, because we have investigated a larger number of subsolid nodules with a wider spectrum of pathology ranging from AIS to invasive adenocarcinoma to obtain results that can be generalised to other settings.
Apart from the intrinsic limits of any retrospective study, there were a few other limitations that should be mentioned. First, pathology assessments themselves, which served as the reference standard in this study, may not be accurate and subject to variability depending on several confounding factors. Specifically, it has been reported that interobserver agreement for the presence of invasive components among pathologists may vary widely depending on histological patterns [35]. Furthermore, inadequately inflated status of the lung tissue after resection and tissue processing may have caused tumour sizes to be measured smaller than the actual sizes. Discordance in measurement planes between CT and pathology and interobserver variability between pathologists may have also contributed to the variability. Second, some cases were excluded from the subgroup analysis for imaging-pathology correlation because of unavailability of the exact sizes of invasive components on pathology reports. Nonetheless, the reproducibility and accuracy are of concerns when evaluating small solid components, and therefore the exclusion of the cases does not undermine the clinical importance of our findings. Third, although the representative axial section for each nodule was used for analysis to minimise other sources of variability, the use of the preselected axial section only could have been a potential cause for the selection bias and lowered agreement with pathology. Moreover, given that readers may choose different sections for nodule measurements in routine practice, the use of preselected axial section may be a potential limitation for extrapolating the interobserver variability seen in this study to routine practice. In addition, coronal or sagittal sections (if available) could have been helpful in distinguishing solid components from vessels in some cases. Fourth, the potential reasons for discordance in nodule classifications between the two window settings should be interpreted with caution because they were based on the opinion of a single experienced radiologist.
In conclusion, the lung window setting had a comparable reproducibility but a higher accuracy than the mediastinal window setting for nodule classifications and solid component measurements in subsolid nodules. These findings imply that the lung window setting may be better than the mediastinal window setting for the evaluation of solid components in subsolid nodules.
Abbreviations
- AAH:
-
atypical adenomatous hyperplasia
- AIS:
-
adenocarcinoma in situ
- GGN:
-
ground-glass nodules
- MIA:
-
minimally invasive adenocarcinoma
References
Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60:277–300
Austin JH, Garg K, Aberle D et al (2013) Radiologic implications of the 2011 classification of adenocarcinoma of the lung. Radiology 266:62–71
Asamura H, Suzuki K, Watanabe S, Matsuno Y, Maeshima A, Tsuchiya R (2003) A clinicopathological study of resected subcentimeter lung cancers: a favorable prognosis for ground glass opacity lesions. Ann Thorac Surg 76:1016–1022
Borczuk AC, Qian F, Kazeros A et al (2009) Invasive size is an independent predictor of survival in pulmonary adenocarcinoma. Am J Surg Pathol 33:462–469
Ikeda K, Awai K, Mori T, Kawanaka K, Yamashita Y, Nomori H (2007) Differential diagnosis of ground-glass opacity nodules: CT number analysis by three-dimensional computerized quantification. Chest 132:984–990
Ishikawa H, Koizumi N, Morita T et al (2005) Ultrasmall pulmonary opacities on multidetector-row high-resolution computed tomography: a prospective radiologic-pathologic examination. J Comput Assist Tomogr 29:621–625
Kim HY, Shim YM, Lee KS, Han J, Yi CA, Kim YK (2007) Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology 245:267–275
Suzuki K, Kusumoto M, Watanabe S, Tsuchiya R, Asamura H (2006) Radiologic classification of small adenocarcinoma of the lung: radiologic-pathologic correlation and its prognostic impact. Ann Thorac Surg 81:413–419
Travis WD, Garg K, Franklin WA et al (2005) Evolving concepts in the pathology and computed tomography imaging of lung adenocarcinoma and bronchioloalveolar carcinoma. J Clin Oncol 23:3279–3287
Hwang EJ, Park CM, Ryu Y et al (2015) Pulmonary adenocarcinomas appearing as part-solid ground-glass nodules: is measuring solid component size a better prognostic indicator? Eur Radiol 25:558–567
Park CM, Goo JM, Lee HJ, Kim KG, Kang MJ, Shin YH (2010) Persistent pure ground-glass nodules in the lung: interscan variability of semiautomated volume and attenuation measurements. AJR Am J Roentgenol 195:W408–W414
Singh S, Pinsky P, Fineberg NS et al (2011) Evaluation of reader variability in the interpretation of follow-up CT scans at lung cancer screening. Radiology 259:263–270
Naidich DP, Bankier AA, MacMahon H et al (2013) Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 266:304–317
Lung CT Screening Reporting and Data System (Lung-RADS). American College of Radiology. Available via http://www.acr.org/Quality-Safety/Resources/LungRADS. Accessed 17 Aug 2015
van Riel SJ, Sanchez CI, Bankier AA et al (2015) Observer variability for classification of pulmonary nodules on low-dose ct images and its effect on nodule management. Radiology 277:863–871
Lee SM, Goo JM, Lee KH, Chung DH, Koh J, Park CM (2015) CT findings of minimally invasive adenocarcinoma (MIA) of the lung and comparison of solid portion measurement methods at CT in 52 patients. Eur Radiol 25:2318–2325
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Kim SY, Kim MJ, Yoon CS, Lee MS, Han KH, Lee MJ (2013) Comparison of the reliability of two hydronephrosis grading systems: the Society for Foetal Urology grading system vs. the Onen grading system. Clin Radiol 68:e484–e490
Henschke CI, Yankelevitz DF, Mirtcheva R et al (2002) CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol 178:1053–1057
Lee HJ, Goo JM, Lee CH, Yoo CG, Kim YT, Im JG (2007) Nodular ground-glass opacities on thin-section CT: size change during follow-up and pathological results. Korean J Radiol 8:22–31
Yankelevitz DF, Yip R, Smith JP et al (2015) CT screening for lung cancer: nonsolid nodules in baseline and annual repeat rounds. Radiology 277:555–564
Pelosi G, Rosai J (2007) Invited commentary. Ann Thorac Surg 83:214–215
Sakao Y, Miyamoto H, Sakuraba M et al (2007) Prognostic significance of a histologic subtype in small adenocarcinoma of the lung: the impact of nonbronchioloalveolar carcinoma components. Ann Thorac Surg 83:209–214
Sakao Y, Nakazono T, Tomimitsu S et al (2004) Lung adenocarcinoma can be subtyped according to tumor dimension by computed tomography mediastinal-window setting. Additional size criteria for clinical T1 adenocarcinoma. Eur J Cardiothorac Surg 26:1211–1215
Travis WD, Brambilla E, Noguchi M et al (2011) International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society International Multidisciplinary Classification of Lung Adenocarcinoma. J Thorac Oncol 6:244–285
Godoy MC, Naidich DP (2009) Subsolid pulmonary nodules and the spectrum of peripheral adenocarcinomas of the lung: recommended interim guidelines for assessment and management. Radiology 253:606–622
Goo JM, Park CM, Lee HJ (2011) Ground-glass nodules on chest CT as imaging biomarkers in the management of lung adenocarcinoma. AJR Am J Roentgenol 196:533–543
Jeudy J, White CS, Munden RF, Boiselle PM (2008) Management of small (3-5-mm) pulmonary nodules at chest CT: global survey of thoracic radiologists. Radiology 247:847–853
Kim HK, Choi YS, Kim J, Shim YM, Lee KS, Kim K (2010) Management of multiple pure ground-glass opacity lesions in patients with bronchioloalveolar carcinoma. J Thorac Oncol 5:206–210
Kim HK, Choi YS, Kim K et al (2009) Management of ground-glass opacity lesions detected in patients with otherwise operable non-small cell lung cancer. J Thorac Oncol 4:1242–1246
Prosch H, Strasser G, Oschatz E, Schober E, Schneider B, Mostbeck GH (2006) Management of patients with small pulmonary nodules: a survey of radiologists, pulmonologists, and thoracic surgeons. AJR Am J Roentgenol 187:143–148
Schultz EM, Silvestri GA, Gould MK (2008) Variation in experts’ beliefs about lung cancer growth, progression, and prognosis. J Thorac Oncol 3:422–426
van Klaveren RJ, Oudkerk M, Prokop M et al (2009) Management of lung nodules detected by volume CT scanning. N Engl J Med 361:2221–2229
Lee KH, Goo JM, Park SJ et al (2014) Correlation between the size of the solid component on thin-section CT and the invasive component on pathology in small lung adenocarcinomas manifesting as ground-glass nodules. J Thorac Oncol 9:74–82
Thunnissen E, Beasley MB, Borczuk AC et al (2012) Reproducibility of histopathological subtypes and invasion in pulmonary adenocarcinoma. An international interobserver study. Mod Pathol 25:1574–1583
Acknowledgements
The scientific guarantor of this publication is Jin Mo Goo. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study was supported by a grant from the National R&D Program for Cancer Control, Ministry for Health and Welfare, Republic of Korea (1520230).
One of the authors (Soyeon Ahn) has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Nineteen study subjects have been previously reported on by Lee et al. [16]. Methodology: retrospective, cross sectional study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoo, RE., Goo, J.M., Hwang, E.J. et al. Retrospective assessment of interobserver agreement and accuracy in classifications and measurements in subsolid nodules with solid components less than 8mm: which window setting is better?. Eur Radiol 27, 1369–1376 (2017). https://doi.org/10.1007/s00330-016-4495-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4495-z