Abstract
Objectives
To evaluate the clinical implications of lymph node (LN) density on 18F-FDG PET/CT for mediastinal LN characterization in non-small cell lung cancer (NSCLC).
Methods
One hundred and fifty-two patients with 271 mediastinal LNs who underwent PET/CT and endobronchial ultrasound-guided transbronchial needle aspiration for staging were enrolled. Maximum standardized uptake value (SUVmax), short axis diameter, LN-to-primary cancer ratio of SUVmax, and median Hounsfield unit (HU) based on CT histogram were correlated to histopathology.
Results
Of 271 nodes, 162 (59.8 %) were malignant. SUVmax, short axis diameter, and LPR of malignant LNs were higher than those of benign nodes. Among malignant LNs, 71.0 % had median HU between 25 and 45, while 78.9 % of benign LNs had values <25 HU or >45 HU. Using a cutoff value of 4.0, SUVmax showed the highest diagnostic ability for detecting malignant LNs with a specificity of 94.5 %, but showing a sensitivity of 70.4 %. Using additional density criteria (median HU 25-45) in LNs with 2.0< SUVmax ≤4.0, the sensitivity increased to 88.3 % with the specificity of 82.6 %.
Conclusions
LN density is useful for the characterization of LNs with mild 18F-FDG uptake. The risk of mediastinal LN metastasis in NSCLC patients could be further stratified using both 18F-FDG uptake and LN density.
Key Points
• SUVmax showed the highest diagnostic ability for detecting malignant LNs.
• LN density was useful in characterization of LNs with mild FDG uptake.
• SUVmax and LN density together could stratify the risk of LN metastasis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients with non-small cell lung cancer (NSCLC), mediastinal lymph node (LN) metastasis is a significant prognostic factor for clinical outcome and crucial for operability [1,2]. Hence, an accurate diagnosis of mediastinal LN involvement is essential for NSCLC staging. Currently, in addition to conventional contrast-enhanced chest computed tomography (CT), 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET)/CT is widely used for mediastinal LN staging. Previous studies reported a sensitivity of 50–79 % and specificity of 72–94 % for 18F-FDG PET/CT in mediastinal LN metastasis diagnosis [3–7]. Because inflammatory changes in LNs can induce increased 18F-FDG uptake, underlying lung disease can cause false-positive findings, resulting in a low diagnostic accuracy for 18F-FDG PET/CT [3,8,9]. To reduce false-positive findings, a high standardized uptake value (SUV) threshold was proposed; however, a high SUV threshold is associated with a greater number of false-negative findings [10–12]. In addition, various methods of interpreting 18F-FDG PET/CT, including the use of the ratio of the SUV of the LN to that of the primary cancer and consideration of Hounsfield unit (HU) values, have been used to enhance diagnostic accuracy for mediastinal LN metastasis [3,11,13]. Recently, CT histogram analysis was introduced for the improvement of detecting mediastinal LN metastasis on 18F-FDG PET/CT, but few studies have been performed to validate the use of CT histogram analysis in lung cancer patients [14].
In the present study, we investigated whether the combination of 18F-FDG uptake and LN density based on CT histogram analysis can be used to further enhance the ability of 18F-FDG PET/CT to characterize mediastinal LNs in NSCLC patients. We only enrolled mediastinal LNs that were clearly allocated to one specific LN on 18F-FDG PET/CT and endobronchial ultrasound guided-transbronchial needle aspiration (EBUS-TBNA) for an accurate comparison of the histopathological diagnosis and 18F-FDG PET/CT findings.
Materials and methods
Patients
The institutional review board of our medical centre approved this retrospective study, and the need for written informed consent was waived. We retrospectively reviewed the electronic medical records of 473 consecutive patients with lung cancer who underwent both staging 18F-FDG PET/CT and EBUS-TBNA before any treatment at our medical centre between 2010 and 2013. From those records, we enrolled 152 patients who 1) were diagnosed with NSCLC, 2) had undergone EBUS-TBNA of at least one mediastinal LN, and 3) had either a positive EBUS-TBNA result for mediastinal LN metastasis or a negative EBUS-TBNA result with histopathologic confirmation by subsequent LN dissection without neoadjuvant treatment. We excluded patients from the study if they 1) were diagnosed with small cell lung cancer, 2) had a prior history of another malignancy or synchronous malignancy, 3) had received any kind of treatment before 18F-FDG PET/CT or EBUS-TBNA, 4) had a negative EBUS-TBNA result without confirmation by surgical resection, or 5) only showed atypical cells or poor cellularity on EBUS-TBNA. From 152 patients, we recruited 298 mediastinal LNs for which locations were based on staging chest CT or 18F-FDG PET/CT according to the EBUS reports of internal medicine physicians; hence, all of the 298 LNs were clearly allocated on both 18F-FDG PET/CT and EBUS-TBNA. Among these nodes, the LNs that showed 1) metastasis on EBUS-TBNA or 2) negative EBUS-TBNA findings, but, metastasis on subsequent mediastinal LN dissection were enrolled in the study as metastatic LNs. Further, the LNs that revealed no evidence of metastasis on EBUS-TBNA and were confirmed on subsequent mediastinal LN dissection were enrolled as benign LNs. Given the consideration of false-negative result of EBUS-TBNA, negative LN stations on EBUS-TBNA without further surgical confirmation were excluded from the study. According to the inclusion criteria of metastatic and benign LNs, a total of 271 mediastinal LNs in 152 patients were finally enrolled in the present study. The mean interval between 18F-FDG PET/CT and EBUS-TBNA was 3.0 ± 4.0 days. All patients also underwent pretreatment contrast-enhanced chest CT for staging work-up along with 18F-FDG PET/CT.
18F-FDG PET/CT
All 18F-FDG PET/CT scans were performed on a dedicated PET/CT scanner (Discovery STe, GE Healthcare or Biograph 40 TruePoint, Siemens Medical Systems). All patients fasted for at least 6 hours prior to the PET/CT scan and a blood glucose level of less than 150 mg/dL was confirmed before the examination. The 18F-FDG PET/CT scan was performed 60 min after the intravenous administration of 5.5 MBq/kg of 18F-FDG. First, CT scanning was performed at 30 mA and 130 kVp on the Discovery STe scanner, or at 36 mA and 120 kVp on the Biograph TruePoint scanner without contrast enhancement. Afterwards, a PET scan was performed from the skull base to the proximal thighs with an acquisition time of 3 min per bed position in three-dimensional mode. PET images were reconstructed using an ordered-subset expectation maximization algorithm with attenuation correction.
EBUS-TBNA
Mediastinal staging with EBUS-TBNA was performed for patients who fulfilled one or more of the following criteria: (1) central tumours, (2) enlarged (≥0.5 cm) mediastinal LNs on CT, or (3) PET-positive LNs. EBUS-TBNA examinations were performed with a linear-array ultrasound bronchoscope (BF-UC260F; Olympus Ltd, Tokyo, Japan) and a 22-gauge needle (NA-200H-8022; Olympus Ltd, Tokyo, Japan) under conscious sedation using intravenous midazolam. Two to six punctures were performed for each LN, beginning with the highest node staging level in cases with multiple suspicious LN stations. The core tissues were obtained from the LNs by EBUS-TBNA, fixed with 10 % formalin, prepared on slides, and reviewed by pathologists. The remainder of the aspirated materials were smeared on glass slides and fixed with 95 % alcohol for cytology examinations.
PET image evaluation and CT histogram analysis
All 18F-FDG PET/CT images were reviewed by two nuclear medicine physicians without knowledge of the histopathological results of enrolled mediastinal LNs. All enrolled mediastinal LNs were classified into nine stations according to the International Association for the Study of Lung Cancer (IASLC) LN map [15]: station 1, low cervical, supraclavicular and sternal notch; station 2, upper paratracheal; station 3, prevascular and retrotracheal; station 4, lower paratracheal; station 5, subaortic; station 6, paraaortic; station 7, subcarinal; station 8, paraesophageal; and station 9, pulmonary ligament. With the use of CT images, a region of interest (ROI) was drawn for the primary cancer lesion and mediastinal LNs for each patient and the maximum standardized uptake value (SUVmax) was measured. The SUVmax was calculated as (decay-corrected activity/tissue volume)/(injected dose/body weight). Furthermore, the length of the short axis of the mediastinal LNs was measured using CT images on the axial plane with the largest short axis.
CT histogram analysis was performed on the basis of non-contrast enhanced CT images from a PET/CT scan. CT images were reconstructed at a slice thickness of 5.0 mm and a reconstruction increment of 2.5 mm with a standard soft-tissue reconstruction kernel (B30). All CT images were transferred using the Digital Imaging and Communications in Medicine protocol to Computational Environment for Radiotherapy Research (CERR) software [16–18]. ROIs were than manually drawn on transaxial CT images for each mediastinal LN with side-by-side correlations with preoperative contrast-enhanced CT images. Using the ROIs of the mediastinal LNs, cumulative CT histogram was calculated for each LN and the HU value of the 50th percentile of the LN voxels (median HU value) was measured.
Statistical analysis
Four parameters from 18F-FDG PET/CT were used for the evaluation of mediastinal LNs: SUVmax, short axis diameter, median HU value of the LN, and the LN-to-primary cancer ratio of SUVmax (LPR). Comparisons of these four parameters according to the histopathological results were performed using generalized estimating equations for clustered data to adjust for potential correlation between LNs assessed within the same individual. The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of the parameters were also determined. The diagnostic accuracies of parameters were evaluated on the basis of the area under the receiver operating characteristic (ROC) curve (AUC). To compare AUCs, the bootstrap method was used with resampling done 1000 times. p values were computed on the basis of 1,000 bootstrap samples, and afterwards, Bonferroni correction was performed to adjust for multiple comparisons.
All statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC, USA) and p values less than 0.05 were considered statistically significant.
Results
Characteristics and histopathological findings of the LNs
The characteristics of the enrolled 152 patients are shown in Table 1 and Fig. 1. Of the 152 patients, 97 showed metastatic mediastinal LNs on EBUS-TBNA. Among these 97 patients, 96 underwent neoadjuvant chemotherapy with subsequent surgical resection, concurrent chemoradiotherapy, chemotherapy, or targeted therapy; one patient underwent surgical resection with mediastinal LN dissection. The remaining 55 patients showed negative results on EBUS-TBNA, and all of these patients underwent surgical resection of lung cancer, including mediastinal LN dissection. Of the 55 patients, 49 were confirmed to have no mediastinal LN metastasis; however, six patients showed mediastinal LN metastasis on surgical resection. Of those six patients, three patients with three lymph nodes had false-negative EBUS-TBNA findings and included in the analysis. The remaining three patients with four lymph nodes had LN metastases at station 5 or 6, which could not be examined with EBUS-TBNA, and excluded from the study. The mean interval between 18F-FDG PET/CT and surgical resection was 11.0 ± 6.3 days.
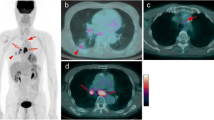
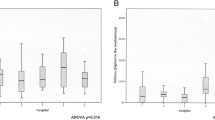
The characteristics of the enrolled 271 mediastinal LN stations are Table 2. Metastatic LNs were found at 162 stations (59.8 %), and the remaining 109 stations (40.2 %) showed no evidence of metastasis on EBUS-TBNA and were confirmed by mediastinal LN dissection. Of the 162 metastatic LN stations, 129 (79.6 %) were adenocarcinoma, 30 (18.5 %) were squamous cell carcinoma, two (1.2 %) were adenosquamous carcinoma, and the remaining one (0.6 %) was sarcomatoid carcinoma. The mean values of SUVmax, short axis diameter, and LPR of the metastatic LNs were higher than those of the benign ones (Fig. 2A–C), whereas the mean HU value of the metastatic LNs was similar to that of the negative LNs (Fig. 2D). However, the median HU values of metastatic LNs were mainly distributed around 25–45 HU, and 71.0 % of metastatic LNs (115/162) had a median density between 25 and 45 HU; meanwhile, 78.9 % of the median HU values of benign nodes (86/109) were lower or higher than 25–45 HU.
Diagnostic value of 18F-FDG PET/CT
SUVmax [0.890; 95 % confidence interval (CI), 0.852–0.925] had a significantly higher AUC value than short axis diameter (0.764; 95 % CI, 0.706–0.820; p < 0.001) or LPR (0.812; 95 % CI, 0.747–0.869; p = 0.03; Fig. 3). Further, there was no significant difference of AUC value between short axis diameter and LPR (p = 0.4). Using the optimal SUVmax cutoff value of 4.0, the sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were 70.4 % (114/162), 94.5 % (103/109), 95.0 % (114/120), 68.2 % (103/151), and 80.1 % (217/271), respectively. In contrast, the short axis diameter (cutoff value, 0.75 cm) and LPR (cutoff value, 0.40) showed sensitivities of 63.0 % (102/162) and 81.5 % (132/162), specificities of 79.8 % (87/109) and 79.2 % (80/101), positive predictive values of 82.3 % (102/124) and 86.3 % (132/153), negative predictive values of 59.2 % (87/147) and 72.7 % (80/110), and accuracies of 69.7 % (189/271) and 78.2 % (212/271), respectively.
Subgroup analysis with CT histogram
Although SUVmax showed the highest AUC among the 18F-FDG PET/CT parameters, the sensitivity and negative predictive value of SUVmax were moderate, and 48 metastatic mediastinal LNs (29.6 % of the metastatic nodes) showed an SUVmax ≤ 4.0. Because the distributions of median HU values were different between metastatic and benign nodes, a further analysis was performed using the median HU value to enhance the detection ability in subgroup LNs with low 18F-FDG uptake. Of the 271 examined LNs, 120 LNs (metastasis, 114; no metastasis, six) were > 4.0; meanwhile, the remaining 151 LNs (metastasis, 48; no metastasis, 103) were ≤ 4.0 (Fig. 4). Of 48 metastatic LNs with ≤ 4.0, only four nodes were ≤ 2.0 and the remaining 44 nodes were >2.0. With reference to the distribution of median HU values according to the SUVmax cutoff value (Fig. 5A), we found a possible cutoff value of 25–45 HU for 151 mediastinal LNs with 18F-FDG uptake ≤ 4.0. Of the 55 LNs with a median HU value between 25 and 45 HU, 58.2 % (32/55 LNs) were metastatic LNs. In contrast, 83.3 % (80/96 LNs) of 96 LNs with a median HU value of < 25 HU or > 45 HU were benign. Of note, all LNs with median HU values < 10 HU or > 60 HU were confirmed as benign LNs among the subgroup LNs with an SUVmax ≤ 4.0. In addition, even in the subgroup of 120 LNs with an SUVmax > 4.0, all the LNs with a density of 25–45 HU were malignant (Fig. 5B).
Evaluation of mediastinal LN metastasis by 18F-FDG uptake and a volumetric CT histogram. (A) A 59-year-old male patient with adenocarcinoma. An LN at the 4R station shows increased 18F-FDG uptake with SUVmax of 5.2 and median density of 37.9 HU, and was confirmed as a metastatic lesion. (B) A 59-year-old male patient with adenocarcinoma. An LN at station 7 shows mild 18F-FDG uptake with SUVmax of 2.3 and median density of 39.0 HU, and was confirmed as a metastatic lesion. (C) A 76-year-old male patient with pleomorphic carcinoma. An LN at the 4R station shows increased 18F-FDG uptake with SUVmax of 5.9 and median density of 78.9 HU, and was confirmed as a benign LN. (D) A 57-year old male patient with adenocarcinoma. An LN at the 4R station shows minimal 18F-FDG uptake with SUVmax of 1.3 and median density of 0.1 HU, and was confirmed as a benign LN
By using both SUVmax and median HU information, we set a new diagnostic criteria for detecting mediastinal LN metastasis; 1) LNs with SUVmax > 4.0 or 2) LNs with a median HU value between 25 and 45 HU in case with 2.0 < SUVmax ≤ 4.0. Using new diagnostic criteria, the sensitivity and accuracy for detecting metastatic LNs increased to 88.3 % (143/162) and 86.0 % (233/271) with specificity of 82.6 % (90/109). The AUC value of the new diagnostic criteria was 0.852 (95 % CI, 0.809–0.893), showing no significant difference of AUC values between SUVmax and the new diagnostic criteria (p = 0.2).
Discussion
In the present study, SUVmax on 18F-FDG PET/CT showed high specificity but moderate sensitivity for detecting mediastinal LN metastasis, and 29.6 % of metastatic LNs revealed low 18F-FDG uptake of less than the cutoff value of 4.0. The median HU value on CT histogram improved the characterization of LNs with mild 18F-FDG uptake; 58.2 % of LNs between 25 and 45 HU were malignant; meanwhile, only 16.7 % of LNs < 25 HU or > 45 HU were metastases. By using the LN density in LNs with low 18F-FDG uptake, the sensitivity and accuracy for detecting mediastinal LN metastases can further increase.
Mediastinal LN evaluation is crucial for treatment selection in NSCLC. Although 18F-FDG PET/CT is considered a non-invasive and effective imaging modality for detecting mediastinal LN metastasis, false-positive findings due to inflammatory and granulomatous conditions and false-negative findings due to small node size and microscopic metastasis are still significant problems. In the present study, SUVmax showed better diagnostic ability than the short axis diameter of the nodes or LPR, and by using a cutoff SUVmax value of 4.0, the sensitivity and specificity for detecting malignant LNs were 70.4 % and 94.5 %, respectively, which are similar to the results of previous studies, showing high specificity but moderate sensitivity using a high SUV threshold [3,6].
To improve the diagnostic ability of 18F-FDG PET/CT for detecting mediastinal LN metastasis, several previous studies have made an attempt to use information on non-contrast enhanced CT images on PET/CT. Previous studies asserted that mediastinal LNs with high attenuation (>70 HU) should be considered as benign LNs, even though the nodes showed increased 18F-FDG uptake, especially in endemic areas of chronic granulomatous disease [3,4,13,19]. These nodes show follicular hyperplasia in the cortex, anthracotic pigmentation, and macrophage infiltration with or without fibrotic micronodule formation in the medulla, and these inflammatory changes could induce an increase in 18F-FDG uptake in the nodes [13]. By considering highly attenuated LNs as benign, previous studies demonstrated an improvement in the specificity of 18F-FDG PET/CT [3,13]. In contrast to the results of these studies, a previous study by Flechsig et al. showed that the median CT density of metastatic LNs was significantly higher than that of benign LNs [14]. They also showed that 77 % of LNs with a density of > 20 HU were malignant; meanwhile, 82 % of LNs with a density of < 20 HU were benign. A higher density is expected in metastatic LNs because of the loss of the fatty hilar architecture that is generally used as an indicator of benignancy of a LN [14,20].
The results of our study could suggest a solution to the contradictory results of the previous studies. In the present study, benign LNs showed not only low density, but also high density, and 71.0 % of the metastatic nodes had a median density between 25 and 45 HU irrespective of 18F-FDG uptake, suggesting that the contradictory results of both previous studies held true findings. A previous study by Nambu et al. also used both nodular calcification and intranodal fat tissue as benign criteria for the visual analysis of a mediastinal LN [20]. Hence, the average HU of metastatic LNs showed a similar value to benign LNs, as shown in the present study and the previous study [7]. The use of information regarding LN density improved the risk stratification of metastasis, especially in LNs with an SUVmax ≤ 4.0, so-called mildly-positive nodes. Among the LNs with an SUVmax ≤ 4.0, 58.2 % of LNs with a density between 25 and 45 HU were malignant, and the sensitivity increased to 88.3 % by using information of LN density in LNs with 2.0 < SUVmax ≤ 4.0. Mediastinal LNs with a density between 25 and 45 HU should be further confirmed by an invasive procedure such as EBUS-TBNA or mediastinoscopy, even if the LNs show only mild 18F-FDG uptake. In contrast, only 16.7 % of LNs with a density of < 25 HU or > 45 HU were malignant. Furthermore, although the number of cases was small, benign LNs with an SUVmax > 4.0 also showed a tendency for a low or high density, suggesting that the density of LNs could be helpful for differentiating not only false-negative nodes, but also false-positive nodes.
In the present study, we enrolled patients who underwent 18F-FDG PET/CT and EBUS-TBNA for mediastinal LN staging. Many of the previous studies enrolled patients who underwent preoperative 18F-FDG PET and subsequent surgical resection [3,4,12,13,19–21]. However, in patients with multiple LNs in the same mediastinal station, an accurate correlation between the histopathological results and 18F-FDG PET/CT findings could not be achieved in the retrospective study because the exact location of the malignant LN is not always clearly identified in the reports [14]. In addition, because of the low prevalence of metastatic mediastinal nodes in patients with resectable NSCLC, the evaluation of the characteristics of malignant nodes could also be limited. In contrast, we enrolled mediastinal LNs that were clearly allocated to one specific LN on both 18F-FDG PET/CT and EBUS-TBNA in the study, and could more accurately correlate the histopathological diagnosis and 18F-FDG PET/CT findings. EBUS-TBNA allows access to bilateral paratracheal, subcarinal, and pulmonary hilar LNs, and has shown high diagnostic value for mediastinal LN staging [22–24]. Furthermore, because patients with advanced stages of N2 or N3 were also enrolled in the study, resulting in a high incidence rate of positive nodes, an evaluation and comparison of the characteristics between metastatic and benign LNs could be performed.
There are several limitations in the present study. First, our study was a retrospective single centre study, and a further prospective study is needed to evaluate whether LN density information from PET/CT can change the diagnostic work-up. Furthermore, only diagnostic ability was evaluated in the present study, and the effect of PET/CT LN density on treatment changes should be further evaluated. Second, 27 LNs, which revealed negative result on EBUS-TBNA but were not confirmed on surgical resection, were excluded from the study, which could lead to verification bias and affect the sensitivity and specificity. Third, because of the retrospective assessment, there might be limitation in exact correlation between PET/CT findings and EBUS-TBNA results. Fourth, patients enrolled in the study underwent EBUS-TBNA for positive findings on 18F-FDG PET/CT or CT images, resulting in a comparatively high incidence of positive LNs and a lack of false-negative LNs. Lastly, only mediastinal LNs accessible by EBUS-TBNA were enrolled, and LNs at stations 5 and 6 were excluded from the analysis.
In conclusion, LN density based on CT histogram analysis provides useful information for the diagnosis of mediastinal LN metastasis in patients with NSCLC, especially in patients with mild 18F-FDG uptake, and complements the moderate sensitivity of SUVmax. By using both 18F-FDG uptake and LN density, we could stratify the risk of malignant involvement of the mediastinal LN to determine further diagnostic work-ups and perform treatment planning. Further prospective study with more patients is needed to validate the results of the present study and assess the effect of the diagnostic criteria using 18F-FDG uptake and LN density on therapeutic strategies.
Abbreviations
- ROC:
-
Receiver operating characteristics
- AUC:
-
Area under the curve
- CCRT:
-
Concurrent chemoradiotherapy
- CERR:
-
Computational Environment for Radiotherapy Research
- EBUS-TBNA:
-
Endobronchial ultrasound-guided transbronchial needle aspiration
- LN:
-
Lymph node
- LPR:
-
Lymph node-to-primary cancer ratio of SUVmax
References
Alberts WM (2007) Diagnosis and management of lung cancer executive summary: ACCP evidence-based clinical practice guidelines (2nd Edition). Chest 132:1s–19s
Detterbeck FC, Postmus PE, Tanoue LT (2013) The stage classification of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143:e191S–e210S
Lee JW, Kim BS, Lee DS et al (2009) 18F-FDG PET/CT in mediastinal lymph node staging of non-small-cell lung cancer in a tuberculosis-endemic country: consideration of lymph node calcification and distribution pattern to improve specificity. Eur J Nucl Med Mol Imaging 36:1794–1802
Lu P, Sun Y, Sun Y, Yu L (2014) The role of (18)F-FDG PET/CT for evaluation of metastatic mediastinal lymph nodes in patients with lung squamous-cell carcinoma or adenocarcinoma. Lung Cancer 85:53–58
Li X, Zhang H, Xing L et al (2012) Mediastinal lymph nodes staging by 18F-FDG PET/CT for early stage non-small cell lung cancer: a multicenter study. Radiother Oncol 102:246–250
Darling GE, Maziak DE, Inculet RI et al (2011) Positron emission tomography-computed tomography compared with invasive mediastinal staging in non-small cell lung cancer: results of mediastinal staging in the early lung positron emission tomography trial. J Thorac Oncol 6:1367–1372
Lee AY, Choi SJ, Jung KP, Park JS, Lee SM, Bae SK (2014) Characteristics of Metastatic Mediastinal Lymph Nodes of Non-Small Cell Lung Cancer on Preoperative F-18 FDG PET/CT. Nucl Med Mol Imaging 48:41–46
Kwon SY, Min JJ, Song HC, Choi C, Na KJ, Bom HS (2011) Impact of Lymphoid Follicles and Histiocytes on the False-Positive FDG Uptake of Lymph Nodes in Non-Small Cell Lung Cancer. Nucl Med Mol Imaging 45:185–191
Lee SH, Min JW, Lee CH et al (2011) Impact of parenchymal tuberculosis sequelae on mediastinal lymph node staging in patients with lung cancer. J Korean Med Sci 26:67–70
Bryant AS, Cerfolio RJ, Klemm KM, Ojha B (2006) Maximum standard uptake value of mediastinal lymph nodes on integrated FDG-PET-CT predicts pathology in patients with non-small cell lung cancer. Ann Thorac Surg 82:417–422
Moloney F, Ryan D, McCarthy L et al (2014) Increasing the accuracy of 18F-FDG PET/CT interpretation of "mildly positive" mediastinal nodes in the staging of non-small cell lung cancer. Eur J Radiol 83:843–847
Vansteenkiste JF, Stroobants SG, De Leyn PR et al (1998) Lymph node staging in non-small-cell lung cancer with FDG-PET scan: a prospective study on 690 lymph node stations from 68 patients. J Clin Oncol 16:2142–2149
Kim BT, Lee KS, Shim SS et al (2006) Stage T1 non-small cell lung cancer: preoperative mediastinal nodal staging with integrated FDG PET/CT--a prospective study. Radiology 241:501–509
Flechsig P, Kratochwil C, Schwartz LH et al (2014) Quantitative volumetric CT-histogram analysis in N-staging of 18F-FDG-equivocal patients with lung cancer. J Nucl Med 55:559–564
Rusch VW, Asamura H, Watanabe H, Giroux DJ, Rami-Porta R, Goldstraw P (2009) The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 4:568–577
Deasy JO, Blanco AI, Clark VH (2003) CERR: a computational environment for radiotherapy research. Med Phys 30:979–985
El Naqa I, Grigsby P, Apte A et al (2009) Exploring feature-based approaches in PET images for predicting cancer treatment outcomes. Pattern Recognit 42:1162–1171
Lee JW, Yun M, Cho A et al (2015) The predictive value of metabolic tumor volume on FDG PET/CT for transarterial chemoembolization and transarterial chemotherapy infusion in hepatocellular carcinoma patients without extrahepatic metastasis. Ann Nucl Med 29:400–408
Shim SS, Lee KS, Kim BT et al (2005) Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology 236:1011–1019
Nambu A, Kato S, Motosugi U et al (2010) Thin-section CT of the mediastinum in preoperative N-staging of non-small cell lung cancer: comparison with FDG PET. Eur J Radiol 73:510–517
Al-Sarraf N, Gately K, Lucey J, Wilson L, McGovern E, Young V (2008) Mediastinal lymph node staging by means of positron emission tomography is less sensitive in elderly patients with non-small-cell lung cancer. Clin Lung Cancer 9:39–43
Lee JE, Kim HY, Lim KY et al (2010) Endobronchial ultrasound-guided transbronchial needle aspiration in the diagnosis of lung cancer. Lung Cancer 70:51–56
Rintoul RC, Tournoy KG, El Daly H et al (2009) EBUS-TBNA for the clarification of PET positive intra-thoracic lymph nodes-an international multi-centre experience. J Thorac Oncol 4:44–48
Hwangbo B, Kim SK, Lee HS et al (2009) Application of endobronchial ultrasound-guided transbronchial needle aspiration following integrated PET/CT in mediastinal staging of potentially operable non-small cell lung cancer. Chest 135:1280–1287
Acknowledgments
The authors are grateful to Jung Hwa Hong (Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, Korea) for her statistical comments and analysis. The scientific guarantor of this publication is Jae-Hoon Lee, MD. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Methodology: Retrospective diagnostic study performed at one institution
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, J.W., Kim, E.Y., Kim, D.J. et al. The diagnostic ability of 18F-FDG PET/CT for mediastinal lymph node staging using 18F-FDG uptake and volumetric CT histogram analysis in non-small cell lung cancer. Eur Radiol 26, 4515–4523 (2016). https://doi.org/10.1007/s00330-016-4292-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4292-8