Abstract
Objectives
To evaluate the prognostic value of CT to predict recurrence-free and overall survival in patients with pancreatic neuroendocrine neoplasms (PanNENs).
Methods
Between January 2004 and December 2012, 161 consecutive patients who underwent preoperative triphasic CT and surgical resection with curative intent for PanNENs were identified. The tumour consistency, margin, presence of calcification, pancreatic duct dilatation, bile duct dilatation, vascular invasion, and hepatic metastases were evaluated. The tumour size, arterial enhancement ratio, and portal enhancement ratio were measured. The Cox proportional hazard model was used to determine the association between CT features and recurrence-free survival and overall survival.
Results
By multivariate analysis, tumour size (>3 cm) (hazard ratio, 3.314; p = 0.006), portal enhancement ratio (≤1.1) (hazard ratio, 2.718; p = 0.006), and hepatic metastases (hazard ratio, 4.374; p = 0.003) were independent significant variables for worse recurrence-free survival. Portal enhancement ratio (≤1.1) (hazard ratio, 5.951; p = 0.001) and hepatic metastases (hazard ratio, 4.122; p = 0.021) were independent significant variables for worse overall survival.
Conclusions
Portal enhancement ratio (≤1.1) and hepatic metastases assessed on CT were common independent prognostic factors for worse recurrence-free survival and overall survival in patients with PanNENs.
Key points
• CT is useful to predict survival outcomes in patients with PanNENs.
• Survival outcomes are associated with portal enhancement ratio and hepatic metastases.
• Portal enhancement ratio is prognostic CT biomarker in patients with PanNENs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic neuroendocrine neoplasms (PanNENs) are a group of heterogeneous tumours, including well-differentiated neuroendocrine tumours (NETs) and poorly differentiated neuroendocrine carcinomas (NECs) [1]. Pancreatic NETs are assumed to have malignant potential [1] and NECs are known to have highly aggressive behaviour [2]. Surgery is the treatment of choice in patients with PanNENs [3, 4]. The survival benefit of surgery was demonstrated for patients with localized, regional, and metastatic disease [5].
A variety of prognostic factors can be used to stratify PanNENs into different risk groups, but the stage and grade of the tumour have been regarded as the potent predictive factors of prognosis [1]. The stage of the tumour represents the extent of tumour involvement, and the grade of the tumour represents the proliferative rate of tumour cells. The stage of PanNENs is determined by the primary tumour size and local extension, lymph node metastases, and distant metastases. Computed tomography (CT) plays an important role in the diagnosis of PanNENs [6], and three determinants of the tumour stage can be assessed with CT. The grade of the tumour might also be assessed with CT. Previous reports [7–10] showed that tumour enhancement on CT was associated with the grade of the PanNENs. We thus assumed that CT findings may provide a hybrid stage-based and grade-based classification system to stratify PanNENs with different clinical outcomes, including recurrence-free survival (RFS) or overall survival (OS). There are several reports of CT findings associated with disease recurrence or patient survival [7, 11]. However, previous studies had a relatively small study population and did not consider confounding variables [7, 11]. The purpose of this study was to evaluate the prognostic value of CT to predict RFS and OS in patients with PanNENs.
Materials and methods
Study population and clinical data
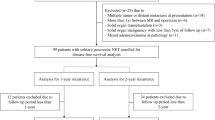
Our institutional review board approved this study, and the requirement for informed consent was waived. A computerized search of the pathology database between January 2004 and December 2012 revealed 198 consecutive patients with surgically confirmed PanNENs. The inclusion criteria were as follows: (a) preoperative triphasic CT; (b) surgery at our institution within one month after CT; (c) without local treatment or chemotherapy before surgery, and (d) visible tumour on CT. We excluded 33 patients without preoperative triphasic CT within 1 month prior to surgery, two patients who received ethanol injection or chemotherapy before surgery, and two patients with an invisible PanNEN on CT. Finally, 161 patients with PanNENs were included in our study. Data collected included the patient’s age, gender, tumour location, tumour type, initial presentation, tumour stage, tumour grade, and residual tumour. Multiple PanNENs were present in three patients, so the largest tumour was selected as the patient’s representative tumour. The stage of the tumour was recorded according to the European Neuroendocrine Tumour Society (ENETS) staging classification [12]. Tumour grade was categorized as grade 1 (G1), grade 2 (G2), or grade 3 (G3), based on 2010 World Health Organization (WHO) classification [1]. Baseline demographic and pathologic tumour characteristics are summarized in Table 1.
Image analysis
All CT examinations were performed using one of the following CT scanners: Sensation 16 (Siemens Medical Systems, Erlangen, Germany), Somatom Definition scanner (Siemens Medical Systems, Erlangen, Germany), LightSpeed 16 (GE Healthcare, Milwaukee, WI, USA), or LightSpeed VCT scanner (GE Healthcare, Milwaukee, WI, USA). Non-enhanced, arterial, and portal venous phase images were obtained in all patients. For contrast-enhanced CT, 100–120 mL iopromide (Ultravist 370 or Ultravist 300; Bayer Schering Pharma, Berlin, Germany) was administered intravenously at a rate of 3 mL/sec. Scan parameters, reconstruction thickness, and the delay time for the arterial phase of each CT scanner are summarized in Table 2. Portal venous phase images were obtained by using a fixed 75-second delay.
The qualitative CT findings were reviewed by a consensus between two radiologists (HJK and KWK, with 14 and 7 years of experience in abdominal radiology, respectively). They were aware that the study population had PanNEN, but they were blinded to the tumour grade, stage, and survival outcome. They evaluated the tumour consistency, tumour margin, calcification, vascular invasion, pancreatic duct dilatation, bile duct dilatation, lymph node enlargements, and hepatic metastases. Disagreements during image analysis occurred for CT findings such as tumour shape, vascular invasion, and lymph node enlargements, but were uncommon and resolved by consensus. Tumour consistency was categorized as predominantly solid (enhancing tissue more than 50 % of the tumour) or predominantly cystic (enhancing tissue less than 50 % of the tumour) [13]. The tumour margin was categorized as well defined (without spiculation or infiltration in > 80 % of the perimeter of the tumour) or poorly defined (spiculation or infiltration in ≥ 20 % of the perimeter of the tumour). The presence of calcification was evaluated on non-enhanced CT. Pancreatic duct dilatation was defined as a diameter of the main duct ≥ 4 mm. Bile duct dilatation was defined as dilatation of both the extrahepatic bile duct (>8 mm) and the intrahepatic bile duct (>2 mm). The criteria for vascular invasion were venous thrombus, vessel occlusion, focal narrowing, or contour deformity, and more than half of the perimeter in contact with the tumour [14, 15]. Lymph node enlargements were defined as short axis > 1 cm, abnormal round morphology, or central necrosis [14]. Criteria of vascular invasion and lymph node enlargements were adopted from the pancreas cancer evaluation [14, 15]. Hepatic metastasis was defined as a hepatic nodule with hypervascularity or peripheral enhancement without classic features of hemangioma or focal nodular hyperplasia. The criteria of hepatic metastases were adopted from the imaging features of hepatic metastases from PanNENs on dynamic MR study [16].
The quantitative CT findings were measured by radiologist KWK. Tumour size was determined as the longest tumour diameter on axial images. The arterial enhancement ratio was defined as the Hounsfield unit (HU) of the tumour / HU of the pancreas parenchyma measured on arterial phase images. The portal enhancement ratio was also defined in the same manner on portal venous phase images.
Statistical analysis
There is no standardized definition of the end points for RFS of PanNENs; hence, we modified the definition of end points used in breast cancer trials [17] and the definition of relapse-free survival in patients with surgically resected PanNENs [18]. RFS was calculated from the date of surgery (R0 or R1) to the earliest among the following: the date of PanNEN recurrence, the date of the last follow-up without evidence of disease, or the date of death attributable to any cause. Events of RFS were defined as local recurrence, distant recurrence, and death attributable to any cause. Recurrence was defined as local (limited to the operation site and the regional lymph node basin), distant (metastases to the liver, lung, peritoneum, or paraaortic lymph node), or both local and distant. A second primary invasive cancer was not considered as an event in the RFS [17]. OS was calculated from the date of PanNEN surgery to the date of death, the date the patient was last known to be alive, or the date of the most recent follow-up. The date of last known to be alive was assessed with medical record. The last date of data collection was 1 March 2014.
Univariate Cox proportional hazards analysis was used to analyze the effect on RFS and OS by clinical-pathologic variables (age, sex, tumour location, tumour type, initial presentation, tumour stage, tumour grade, and residual tumour) and CT variables (qualitative variables: tumour consistency, tumour margin, calcification, vascular invasion, pancreatic duct dilatation, bile duct dilatation, lymph node enlargements, and hepatic metastases; quantitative variables: tumour size, arterial enhancement ratio, and portal enhancement ratio). The quantitative CT variables were dichotomized for the statistical analysis. To set cutoff values for such dichotomization, we performed receiver operating characteristic (ROC) analysis. For tumour size, we tested 2 cm, 3 cm, and 4 cm as the cutoff values, because the ENETS staging classification used 2 cm and 4 cm as T-stage criteria [12]. For the enhancement ratio, we tested 0.9 and 1.1 as the cutoff values, because the attenuation difference between iso-attenuating pancreatic cancer and the pancreas parenchyma was approximately 10 %, according to a previous report [19]. The cutoff value with the largest sum of sensitivity and specificity on the ROC analysis was chosen as the optimal cutoff value.
Qualitative variables with p values of less than 0.10 in the univariate Cox proportional hazards analysis and quantitative variables determined by ROC analysis were entered as input variables for a multivariate Cox proportional hazards analysis. Variable selection was generated by a multivariate Cox proportional hazards model with a backward elimination method. A test of proportionality was performed to validate a Cox proportional hazard model for RFS and OS. Kaplan-Meier survival analysis with a log-rank test was performed for significant variables in multivariate analysis. We used the survival ROC package of R 2.15.3 (R Foundation for Statistical Computing, Vienna, Austria) for the ROC analysis and SPSS 21 (SPSS Inc., Chicago, IL, USA) for the other statistical analyses.
Results
Triphasic CT features
Most PanNENs showed predominantly solid consistency (93.2 %, 150/161) and well-defined margin (98.1 %, 158/161). Calcification within the tumour (11.2 %, 18/161), vascular invasion (9.3 %, 15/161), pancreatic duct dilatation (16.1 %, 26/161), and bile duct dilatation (5.0 %, 8/161) were infrequently observed. Lymph node enlargements and hepatic metastases were present in 9.9 % (16/161) and 6.2 % (10/161), respectively. The tumour size, arterial enhancement ratio, and portal enhancement ratio was 30.0 mm ± 20.8 (mean ± standard deviation), 1.476 ± 0.552, and 1.341 ± 0.358, respectively. Triphasic CT features of PanNENs are summarized in Table 3.
Survival outcomes
The median RFS in 157 patients with PanNENs who received R0 or R1 resection was 34.6 months (range, 23 days – 116.0 months). Thirty-one events occurred during the follow-up period; distant recurrences in 20 patients, local recurrence in one patient, both local recurrence and distant recurrence in five patients, and death from any cause in five patients. The locations for distant recurrences were liver (n = 21), distant lymph node (n = 2), liver and omentum (n = 1), and simultaneous recurrences in liver, distant lymph node, and lung (n = 1). The locations of local recurrences included operation site (n = 3) and regional lymph node (n = 3). The median OS in patients with PanNENs (n = 161) who received surgical resection was 48.4 months (range, 23 days – 123.3 months). There were 17 deaths from any cause during the follow-up period.
Survival analysis: univariate
The results of univariate Cox proportional hazard analysis of clinical-pathologic variables with survival outcomes are summarized in Table 4. Among the clinical-pathologic variables, symptoms at initial presentation (RFS HR, 2.138; OS HR, 4.218), high ENETS stage (RFS HR, 5.590 [stage III], 17.171 [stage IV]; OS HR, 9.755 [stage IV]), high tumour grade (RFS HR, 8.476 [G2], 38.405 [G3]; OS HR, 23.355 [G3]), and residual tumour (OS HR, 3.767 [R1]) were associated with worse survival outcomes.
The results of the univariate Cox proportional hazard analysis of the CT variables with survival outcomes are summarized in Table 5. Among the qualitative CT variables, a poorly-defined margin (RFS HR, 16.060; OS HR, 12.656), vascular invasion (RFS HR, 7.297; OS HR, 4.294), pancreatic duct dilatation (RFS HR, 3.126), bile duct dilatation (RFS HR, 8.215; OS HR, 8.644), lymph node enlargements (RFS HR, 6.211; OS HR, 4.002), and hepatic metastases (RFS HR, 8.196; OS HR, 6.958) were associated with worse survival outcomes. The results of the ROC analysis of the tumour size, arterial enhancement ratio, and portal enhancement ratio to determine the optimal cutoff value are summarized in Table 6. We set 3 cm as the optimal cutoff value of tumour size. We set 1.1 as the optimal cutoff value of RFS for arterial enhancement ratio, 0.9 as the optimal cutoff value of OS for arterial enhancement ratio, and 1.1 as the optimal cutoff value of RFS and OS for portal enhancement ratio. A tumour size (>3 cm) (RFS HR, 4.768; OS HR, 2.832), an arterial enhancement ratio (≤1.1 for RFS and ≤ 0.9 for OS) (RFS HR, 2.085; OS HR, 6.090), and a portal enhancement ratio (≤1.1) (RFS HR, 3.325; OS HR, 7.112) were associated with worse survival outcomes (Figs. 1 and 2).
Pancreatic neuroendocrine carcinoma, grade 3 in 56-year-old man. Transverse portal venous phase CT shows a hypo-attenuating tumour (arrow) in the pancreas tail and splenic vein thrombus in splenic hilum (black arrowhead) and splenoportal junction (white arrowhead). Distal pancreatectomy, splenectomy, and portal vein resection were performed. Tumour recurrence was identified in liver on the follow-up CT, obtained 5 months later. This patient deceased at 13 months after operation
Survival analysis: multivariate
The results of the multivariate Cox proportional hazard analysis are detailed in Table 7. A tumour size (>3 cm) (HR, 3.314; p = 0.006), a portal enhancement ratio (≤1.1) (HR, 2.718; p = 0.006), and hepatic metastases (HR, 4.374; p = 0.003) were the independent variables found to be associated with RFS. A portal enhancement ratio (≤1.1) (HR, 5.951; p = 0.001) and hepatic metastases (HR, 4.122; p = 0.021) were the independent variables found to be associated with OS. The proportional hazard assumption was confirmed by examination of the log survival curves and by testing of the partial Schoenfeld residuals, and no relevant violations were found. The Kaplan-Meier curves (Fig. 3) were significantly different for a tumour size (>3 cm) (RFS, log-rank p < 0.001; OS, log-rank p = 0.033), a portal enhancement ratio (≤1.1) (RFS, log-rank P < 0.001; OS, log-rank p < 0.001), and metastasis (≤1.1) (RFS, log-rank P < 0.001; OS, log-rank p < 0.001).
Kaplan-Meier curves for recurrence-free survival (a) and overall survival (b) based on tumour size (>3 cm). Kaplan-Meier curves for recurrence-free survival (c) and overall survival (d) based on portal enhancement ratio (≤1.1). Kaplan-Meier curves for recurrence-free survival (e) and overall survival (f) based on hepatic metastases
Discussion
Our study found that imaging features on triphasic CT can predict RFS and OS in patients with PanNENs. The most compelling result is that portal enhancement ratio assessed on CT can be used as an independent prognostic factor of RFS and OS in patients with PanNENs. In this study, patients with PanNENs that had a low portal enhancement ratio (≤1.1) (i.e., an iso- attenuating or hypo-attenuating tumour during the portal venous phase) on CT showed increased recurrence and mortality risk compared with PanNENs with a high portal enhancement ratio (>1.1) (i.e., hyper-attenuating tumour during portal venous phase). This result is consistent with a previous study [7] in which hypo-attenuating PanNENs during pancreatic phase CT correlated with a decreased OS. Rodallec et al. [7] reported hypo-attenuating PanNENs on a pancreatic phase CT were correlated with poor differentiation. Tumour blood flow assessed with a perfusion CT in patients with PanNENs was also significantly lower in tumours with a high (>2 %) proliferative index [8]. Previous studies [20–22] also reported that a low intratumoural microvessel density could be an unfavourable histoprognostic factor. However, two other studies failed to show a correlation between the degree of tumour enhancement and the grade of PanNENs on CT [11] and MR [23]. This discrepancy might be explained by the cutoff point in pathology analysis. Those two earlier studies divided the PanNENs into benign diagnosis versus non-benign diagnosis [11] or G1 versus G2 [23].
Two interesting observations of this study are the association between survival outcome and tumour size and between survival outcome and lymph node enlargements. Our study showed that PanNENs larger than 3 cm were associated with a high rate of recurrence and worse survival on univariate analysis. A tumour larger than 3 cm was an independent variable of RFS, but not of OS in multivariate analysis. Lymph node enlargements were associated with high recurrence and worse survival in the univariate analysis, but not in the multivariate analysis. There was a suggestion that the importance of tumour size and lymph node metastases in the staging classification is questionable [24]. The survival discrimination seen in the staging classification might likely stem from the T-stage and N-stage serving as a proxy for other prognostic factors that have been shown to be significant for PanNENs such as tumour differentiation and functional status [24].
Among qualitative CT findings, a poorly defined margin, vascular invasion, and bile duct dilatation were found to be associated with high recurrence and worse survival on univariate Cox proportional hazard analysis. These findings were more frequently observed in G3 NEC than G1/2 NET [9], but the incidence of poorly defined margin, vascular invasion, and bile duct dilatation was 1.9 % (3/161), 9.3 % (15/161), and 5 % (8/161), respectively. These characteristics were present at a low incidence among all PanNENs, and were not included in the independent variables for RFS or OS in multivariate analysis.
One of the important changes in the revised 2010 WHO classification of PanNENs was the replacement of the hybrid grade-based and stage-based classification system with a purely grade-based classification system [1, 25]. Tumour stage should also be determined because it is also an independent prognostic factor. If there is a discrepancy between the tumour grade and stage, predicting the likely clinical outcomes in patients with PanNENs based on the revised 2010 WHO classification is difficult. In our study, we used various CT input variables for the multivariate Cox proportional hazard analysis. These input variables included the tumour size (CT T-stage), lymph node enlargements (CT N-stage), liver metastases (CT M-stage), and the portal enhancement ratio. Considering the fact that the portal enhancement ratio might be associated with the grade of PanNENs, the results of our multivariate analysis may represent a hybrid classification including both stage and grade of PanNENs.
Our study had several limitations. First, we did not obtain the interobserver variability of the qualitative image analysis due to the consensus review by two radiologists. However, image analyses were performed by experienced abdominal radiologists and disagreements were uncommon. Disagreements were present in CT parameters such as tumour shape, vascular invasion, and lymph node enlargements. Second, we used various CT scanners and parameters. The surgically confirmed PanNENs are not common. This limitation was due to the long study period and retrospective study design. Third, we limited our study population to patients who received surgical resection. If we extended our study population to cases diagnosed with PanNENs based on a biopsy or surgery, this may have introduced many confounders. In selected cases, observation may be considered for small PanNENs. In advanced cases, molecular therapy, such as everolimus or sunitinib, or cytotoxic chemotherapy may be considered without surgery. Fourth, we performed dichotomization for continuous variables and this may have caused information loss during statistical analysis. However, the cutoff values were determined based on clinical and practical rationale.
In conclusion, a tumour size larger than 3 cm, an iso-attenuating or hypo-attenuating tumour during the portal venous phase, and hepatic metastases are the CT parameters associated with worse RFS in patients with PanNENs. An iso-attenuating or hypo-attenuating tumour during the portal venous phase and hepatic metastases are the CT parameters associated with worse OS in patients with PanNENs. An iso-attenuating or hypo-attenuating tumour during the portal venous phase and hepatic metastases are the common CT parameters associated with a worse RFS and OS in patients with PanNENs.
Abbreviations
- PanNEN:
-
pancreatic neuroendocrine neoplasm
- NET:
-
neuroendocrine tumour
- NEC:
-
neuroendocrine carcinoma
- RFS:
-
recurrence-free survival
- OS:
-
overall survival
- G1:
-
grade 1
- G2:
-
grade 2
- G3:
-
grade 3
- HU:
-
Hounsfield unit
- HR:
-
hazard ratio
References
Bosman FT, Carneiro F, Hruban RH, Theise ND (2010) WHO classification of tumours of the digestive system, 4th edn. International Agency for Research on Cancer, Lyon
Basturk O, Tang L, Hruban RH et al (2014) Poorly differentiated neuroendocrine carcinomas of the pancreas: a clinicopathologic analysis of 44 cases. Am J Surg Pathol 38:437–447
Franko J, Feng W, Yip L, Genovese E, Moser AJ (2010) Non-functional neuroendocrine carcinoma of the pancreas: incidence, tumor biology, and outcomes in 2,158 patients. J Gastrointest Surg 14:541–548
Falconi M, Plockinger U, Kwekkeboom DJ et al (2006) Well-differentiated pancreatic nonfunctioning tumors/carcinoma. Neuroendocrinology 84:196–211
Hill JS, McPhee JT, McDade TP et al (2009) Pancreatic neuroendocrine tumors: the impact of surgical resection on survival. Cancer 115:741–751
Horton KM, Hruban RH, Yeo C, Fishman EK (2006) Multi–Detector Row CT of Pancreatic Islet Cell Tumors. Radiographics 26:453–464
Rodallec M, Vilgrain V, Couvelard A et al (2006) Endocrine pancreatic tumours and helical CT: contrast enhancement is correlated with microvascular density, histoprognostic factors and survival. Pancreatology 6:77–85
d'Assignies G, Couvelard A, Bahrami S et al (2009) Pancreatic endocrine tumors: tumor blood flow assessed with perfusion CT reflects angiogenesis and correlates with prognostic factors. Radiology 250:407–416
Kim DW, Kim HJ, Kim KW et al (2015) Neuroendocrine neoplasms of the pancreas at dynamic enhanced CT: comparison between grade 3 neuroendocrine carcinoma and grade 1/2 neuroendocrine tumour. Eur Radiol 25:1375–1383
Luo Y, Dong Z, Chen J et al (2014) Pancreatic neuroendocrine tumours: correlation between MSCT features and pathological classification. Eur Radiol 24:2945–2952
Gallotti A, Johnston RP, Bonaffini PA et al (2013) Incidental neuroendocrine tumors of the pancreas: MDCT findings and features of malignancy. AJR 200:355–362
Rindi G (2010) The ENETS guidelines: the new TNM classification system. Tumori 96:806–809
Kawamoto S, Johnson PT, Shi C et al (2013) Pancreatic Neuroendocrine Tumor With Cystlike Changes: Evaluation With MDCT. AJR 200:W283–W290
Al-Hawary MM, Francis IR, Chari ST et al (2014) Pancreatic ductal adenocarcinoma radiology reporting template: consensus statement of the Society of Abdominal Radiology and the American Pancreatic Association. Radiology 270:248–260
Lu DS, Reber HA, Krasny RM, Kadell BM, Sayre J (1997) Local staging of pancreatic cancer: criteria for unresectability of major vessels as revealed by pancreatic-phase, thin-section helical CT. AJR 168:1439–1443
d'Assignies G, Fina P, Bruno O et al (2013) High sensitivity of diffusion-weighted MR imaging for the detection of liver metastases from neuroendocrine tumors: comparison with T2-weighted and dynamic gadolinium-enhanced MR imaging. Radiology 268:390–399
Hudis CA, Barlow WE, Costantino JP et al (2007) Proposal for standardized definitions for efficacy end points in adjuvant breast cancer trials: the STEEP system. J Clin Oncol 25:2127–2132
Strosberg JR, Cheema A, Weber JM et al (2012) Relapse-free survival in patients with nonmetastatic, surgically resected pancreatic neuroendocrine tumors: an analysis of the AJCC and ENETS staging classifications. Ann Surg 256:321–325
Kim JH, Park SH, Yu ES et al (2010) Visually Isoattenuating Pancreatic Adenocarcinoma at Dynamic-Enhanced CT: Frequency, Clinical and Pathologic Characteristics, and Diagnosis at Imaging Examinations. Radiology 257:87–96
Takahashi Y, Akishima-Fukasawa Y, Kobayashi N et al (2007) Prognostic value of tumor architecture, tumor-associated vascular characteristics, and expression of angiogenic molecules in pancreatic endocrine tumors. Clin Cancer Res 13:187–196
Couvelard A, O'Toole D, Turley H et al (2005) Microvascular density and hypoxia-inducible factor pathway in pancreatic endocrine tumours: negative correlation of microvascular density and VEGF expression with tumour progression. Br J Cancer 92:94–101
Marion-Audibert AM, Barel C, Gouysse G et al (2003) Low microvessel density is an unfavorable histoprognostic factor in pancreatic endocrine tumors. Gastroenterology 125:1094–1104
Manfredi R, Bonatti M, Mantovani W et al (2013) Non-hyperfunctioning neuroendocrine tumours of the pancreas: MR imaging appearance and correlation with their biological behaviour. Eur Radiol 23:3029–3039
Edge SB, Byrd DR, Compton CC et al (2010) AJCC cancer staging manual, 7th edn. Springer, New York
Kim KW, Krajewski KM, Nishino M et al (2013) Update on the management of gastroenteropancreatic neuroendocrine tumors with emphasis on the role of imaging. AJR 201:811–824
Acknowledgments
The scientific guarantor of this publication is Hyoung Jung Kim. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding by the Ministry of Education, Science and Technology, South Korea (grant 2012R1A1A1012731). Min-Ju Kim (Department of Clinical Epidemiology and Biostatistics, Asan Medical Center) kindly provided statistical advice for this manuscript. One of the authors (KW Kim) has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board.
Some study subjects or cohorts have been previously reported in:
a. Kim DW, Kim HJ, Kim KW, et al (2015) Neuroendocrine neoplasms of the pancreas at dynamic enhanced CT: comparison between grade 3 neuroendocrine carcinoma and grade 1/2 neuroendocrine tumour. Eur Radiol 25:1375-1383.
b. Kim JY, Kim MS, Kim KS, et al (2015) Clinicopathologic and prognostic significance of multiple hormone expression in pancreatic neuroendocrine tumours. Am J Surg Pathol 39:592-601.
Methodology: retrospective, prognostic study / observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, D.W., Kim, H.J., Kim, K.W. et al. Prognostic value of CT findings to predict survival outcomes in patients with pancreatic neuroendocrine neoplasms: a single institutional study of 161 patients. Eur Radiol 26, 1320–1329 (2016). https://doi.org/10.1007/s00330-015-3943-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3943-5