Abstract
Objectives
To evaluate secretin-enhanced MRCP (S-MRCP) findings of patients with pancreas divisum and Santorinicele, before and after minor papilla sphincterotomy.
Methods
S-MRCP examinations of 519 patients with suspected pancreatic disease were included. Size of the main pancreatic duct, presence and calibre of Santorinicele were evaluated. Duodenal filling was assessed on dynamic images. After sphincterotomy the same parameters and the clinical findings were re-evaluated.
Results
Pancreas divisum was depicted in 55/519 patients (11 %) by MRCP and an additional 26/519 by S-MRCP (total 81/519, 16 %). Santorinicele was detected in 7/81 patients (8.6 %) with pancreas divisum by MRCP and an additional 20/81 by S-MRCP (total 27/81, 33 %). Dorsal duct in patients with Santorinicele was significantly larger in the head compared with patients with only pancreas divisum (p < 0.01), in basal conditions (average 2.4 versus 1.9 mm) and after secretin administration (average 3.0 versus 2.4 mm). Duodenal filling was impaired in 11/27 patients (41 %) with Santorinicele. After sphincterotomy significant reduction in size of Santorinicele (−33 %) and dorsal duct (−17 %), increase of pancreatic juice and symptoms improvement were observed.
Conclusion
Secretin administration increases the accuracy of MRCP in detecting Santorinicele and demonstrates the impaired duodenal filling. S-MRCP is useful to assess results of sphincterotomy.
Key Points
• Secretin-enhanced MRCP gives anatomical and functional information on pancreatic outflow dynamics.
• Santorinicele is a cystic dilatation of the termination of the Santorini duct.
• S-MRCP images are the most useful to recognize the presence of Santorinicele.
• Minor papilla sphincterotomy during ERCP is indicated in patients with Santorinicele.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pancreas divisum is the most frequent congenital variant of the pancreatic ductal configuration; its occurrence varies in different population; it is more common in Caucasian people, with a reported prevalence between 5 % and 14 % [1–5].
Pancreas divisum occurs when the embryological ventral and dorsal parts of the pancreas fail to fuse, so that pancreatic drainage is mainly through the Santorini duct and the accessory papilla [6, 7]. The majority of patients with pancreas divisum have no clinical disease, but there is a subset of patients who have either unexplained abdominal pain or recurrent episodes of acute pancreatitis [8]. In this subset of patients, it has been suggested that a relative obstruction of the minor papilla could intermittently impair the outflow of pancreatic juice within the duodenum, resulting in increased endoluminal pressure and obstructive pancreatitis [9].
Santorinicele has been defined as a focal cystic dilatation of the termination of the dorsal pancreatic duct at the minor papilla [10]. It occurs in patients with pancreas divisum, particularly in the subgroup who develop abdominal pain or acute pancreatitis [11].
In the past endoscopic retrograde cholangiopancreatography (ERCP) was considered the gold standard for the diagnosis of Santorinicele [10]. However, in recent years magnetic resonance cholangiopancreatography (MRCP) has been proposed as the most appropriate imaging technique for noninvasively investigating the pancreatic ductal configuration [12].
Secretin injection during MRCP (S-MRCP) enhances the visualization of the morphology of the main pancreatic duct and gives information on pancreatic outflow dynamics [13–15]; according to some authors, S-MRCP is effective in diagnosing the presence of Santorinicele in patients affected by unexplained recurrent episodes of acute pancreatitis and who might benefit from endoscopic treatment [16–18].
Our objective in this study was to assess the utility of S-MRCP in the diagnosis of pancreas divisum and Santorinicele; then we evaluated the morphological modifications of the Santorini duct by S-MRCP before and after endoscopic sphincterotomy of the minor papilla in patients with pancreas divisum and Santorinicele; we also compared pancreatic outflow dynamics by S-MRCP before and after sphincterotomy.
Method and materials
Patient population
This retrospective study was approved by the investigational review board, and the requirement for informed patient consent was waived. Data from secretin-enhanced MRCP (S-MRCP) of 519 consecutive patients (278 men, 241 women; age range 14–81 years; average age 59 years) were evaluated; 459/519 patients were Caucasian, 53/519 African and 7/519 Asian. They had a suspected inflammatory pancreatic disease because of recurrent pancreatic-like symptoms (upper abdominal or left upper quadrant burning pain radiating to the back, nausea and vomiting) with pancreatic hyperenzymemia (lipase greater than 150 U/L and/or amylase greater than 110 U/L in at least two blood tests) [19]. Every patient had previously undergone ultrasonography (US), which had not depicted signs of acute or chronic pancreatitis and had excluded the presence of gallstones and lesions occupying space within the pancreatic parenchyma. After collecting consensus, 141/519 patients (27 %) underwent ERCP with an average time interval between S-MRCP and ERCP of 18 days (range 3–71 days) for diagnostic or therapeutic purposes; minor papilla sphincterotomy was performed in 21/141 patients during ERCP. One month after the procedure these patients underwent new blood tests to assess lipase and amylase levels; they also underwent a clinical interview to assess the frequency of abdominal pain, nausea and vomiting.
Follow-up S-MRCP after minor papilla sphincterotomy was performed in 12/21 patients (average 188 days after ERCP; range 13–314 days).
S-MRCP findings were compared with the ERCP findings.
MR imaging
MR imaging was performed with a 1.5-T MR unit (Magnetom Symphony; Siemens, Erlangen, Germany) by using a four-channel phased array coil. The patients were asked to fast for 4–6 h before the MR examination and were given 50–150 ml of superparamagnetic iron oxide particles (ferumoxsil, Lumirem; Guerbet, Aulnay-sous-Bois, France) orally just before the examination to prevent the overlap of gastrointestinal fluid on the MR images.
Before MRCP, a series of MRI sequences were performed to study the upper abdominal organs. The following sequences were used: T1-weighted gradient echo sequences (GRE) with in-phase and out-of-phase time to echo (TE), with repetition time (TR)/TE, 107–160/2.4–4.8 ms; T2-weighted rapid acquisition with relaxation enhancement (RARE) sequences with TR/TE 4,950/102 ms; T1-weighted GRE with fat saturation with TR/TE 107/4.8 ms; T2-weighted half-Fourier single-shot turbo spin echo (HASTE) with TR/TE ∞/60–102 ms, slice thickness 4 mm.
MRCP examination was performed with T2-weighted HASTE two-dimensional sequences, with TR/TE ∞/1,100 ms and slice thickness of 40–60 mm, to include the entire biliary tree and pancreatic ductal system. The latter sequence was carried out with different angles (3–10 acquisitions; average, 6) relative to the pancreatic long axis so as to optimize the visualization of the ductal system. The sequence which best visualized the main pancreatic duct was selected to acquire a set of MRCP images after secretin administration.
Secretin (Secrelux; SanoChemia, Neuss, Germany) was injected intravenously at a dose of 1 CU/kg body weight. MRCP dynamic acquisitions were repeated every 30 s for the first 5 min and every 1 min for the second 5 min up to 10 min after the injection.
Image analysis
Images obtained before and after secretin stimulation were evaluated on a dedicated workstation separately and in a randomized fashion. The MR imaging parameters were assessed with qualitative and quantitative image analysis.
The qualitative MR image analysis was conducted by two radiologists (18 and 4 years of experience in abdominal radiology).
Images were evaluated for the presence of pancreas divisum and of Santorinicele, in basal conditions and after secretin administration. Pancreas divisum was defined, according to the literature, when the dorsal duct visible from the tail and body of the pancreas through the anterior aspect of the head and could be seen draining into the minor papilla [5, 6]. Pancreas divisum was divided into two categories: classical, in which there is no connection between dorsal and ventral ducts; and incomplete pancreas divisum, in which a rudimentary communication was observed between the ducts [20, 21].
Santorinicele was defined as cystic dilation of the distal dorsal duct, just proximal to the minor papilla [16]. Santorinicele was divided in two subtypes, as suggested by previous studies: “spindle type” in cases of ampullary shape; “saccular type” in cases of saccular shape [22].
The qualitative image analysis also included a semi-quantitative evaluation of duodenal filling, a function of pancreatic exocrine secretion, on MRCP images obtained 10 min after secretin administration. MRCP images were assessed as follows: grade 0 for absence of duodenal filling; grade 1 for fluid limited to the duodenal bulb; grade 2 for duodenal filling up to the genu inferius; grade 3 for filling beyond the genu inferius. In agreement with the literature, pancreatic exocrine function was considered reduced when duodenal filling was less than grade 3 [13]. Duodenal filling was evaluated before and after sphincterotomy. Differences in evaluation were resolved by consensus.
A third radiologist (5 years of experience), not involved in the qualitative analysis, performed a quantitative image analysis on a workstation by using an electronic caliper.
The quantitative analysis was performed on T2-weighted HASTE MRCP images using an electronic caliper on 200 % magnified images. This evaluation included the calibre of the dorsal duct in the pancreatic head (greatest segment, avoiding Santorinicele) in basal conditions and after secretin administration; calibre of Santorinicele (greatest segment) in basal conditions and after secretin administration. When Santorinicele was visible only after secretin injection, we compared its diameter with the diameter of the corresponding region of the dorsal duct in basal conditions.
We also calculated the average ratio between Santorinicele and dorsal duct calibre, before and after secretin administration.
After minor papilla sphincterotomy all parameters were re-evaluated.
Statistical analysis
A one-tailed Student t test was used to calculate the difference of the following parameters: diameter of the dorsal duct in the pancreatic head in the group of patients with pancreas divisum and Santorinicele versus the diameter in the group with pancreas divisum without Santorinicele; diameter of the dorsal duct in the pancreatic head before and after secretin administration; size of the Santorinicele before and after secretin administration; diameter of the dorsal duct in the pancreatic head before and after minor papilla sphincterotomy; duodenal filling with pancreatic juice before and after sphincterotomy.
These analyses were performed by using MedCalc Software for Windows and Microsoft Excel software for Windows; a p value less than 0.05 was considered statistically significant.
Results
Qualitative image analysis
Presence of pancreas divisum
Pancreas divisum was depicted on MRCP images in 55/519 patients (11 %) and in an additional 26/519 (5 %) after secretin administration; overall pancreas divisum was depicted in 81/519 patients (16 %) by S-MRCP. Sixty-four out of 81 patients with pancreas divisum (79 %) presented the classical form (complete pancreas divisum), 17/81 (21 %) presented incomplete pancreas divisum.
Eighty out of 81 patients with pancreas divisum were Caucasian, 1/81 was African. No Asian patient had pancreas divisum.
ERCP was performed in 57/81 patients (70 %) with pancreas divisum; in all these patients ERCP confirmed the presence of the anatomical variant. Whereas 24/81 patients (30 %) with pancreas divisum did not undergo ERCP: 14 because S-MRCP did not show signs of chronic pancreatitis or hydrodynamic conditions that would require therapeutic ERCP; four patients refused to undergo the procedure; ERCP was not performed in six patients because of failure to cannulate the minor papilla.
Patients without pancreas divisum (438/519, 84 %) were not evaluated further in the qualitative and quantitative image analysis.
Presence of Santorinicele
Presence of Santorinicele was depicted on MRCP images in basal conditions in 7/81 patients (8.6 %) with pancreas divisum and in an additional 20/81 (25 %) after secretin administration (Fig. 1). No Santorinicele was found in patients with a normally fused pancreas. Overall Santorinicele was depicted by S-MRCP in 27/81 patients (33 %) with pancreas divisum (13 men, 14 women; age range, 31–79 years; average age 57 years). “Spindle type” Santorinicele was depicted in 23/27 patients (85 %), “saccular type” in 4/27 patients (15 %).
Female 56-year-old patient with pancreas divisum and Santorinicele presenting abdominal pain and pancreatic hyperenzymemia. a Coronal MRCP image obtained by using T2-weighted HASTE sequence, TR/TE ∞/1,100 ms, slice thickness 60 mm. The main pancreatic duct is the dorsal duct and terminates in the minor papilla (arrowhead). A dilated side branch is visible (arrow). Ventral duct is not depicted. b Coronal MRCP image 1 min after secretin administration. Both dorsal and ventral duct are depicted (top and bottom arrow, respectively), with multiple dilated side branches. Santorinicele is clearly visible (arrowhead). Duodenal filling with pancreatic juice is not depicted, a sign of impaired outflow. c Coronal MRCP image 4 min after secretin administration. Santorinicele is still visible (arrowhead), and duodenal filling is depicted (arrow). d Coronal MRCP image 10 min after secretin administration. Main pancreatic duct (arrow) has not returned to the basal calibre, sign of increased intraductal pressure
Santorinicele was depicted only in patients with complete pancreas divisum.
Every patient with Santorinicele was Caucasian.
The diagnosis of Santorinicele was confirmed by ERCP in 21/27 patients (78 %); in 6/27 patients ERCP confirmation was not possible because of failure to cannulate the minor papilla or because they refused the procedure, respectively two and four patients (Fig. 2).
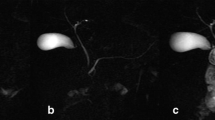
Female 61-year-old patient with pancreas divisum and Santorinicele presenting abdominal pain and pancreatic hyperenzymemia. a Coronal MRCP image obtained by using T2-weighted HASTE sequence, TR/TE ∞/1,100 ms, slice thickness 60 mm. Santorinicele is visible also in basal conditions (arrowhead). Dorsal duct is clearly visible (top arrow). Ventral duct is not depicted. A dilated side branch is visible (bottom arrow). b Coronal MRCP image 4 min after secretin administration. The calibre of main pancreatic duct is increased and Santorinicele is bigger than in basal conditions (3.0 mm versus 2.1 mm) (arrowhead). Duodenal filling is depicted (arrow). c Coronal MRCP image 10 min after secretin administration. Main pancreatic duct (arrow) and Santorinicele (arrowhead) have not returned to the basal calibre, sign of increased intraductal pressure. Duodenal filling (asterisk) is limited to duodenal bulb, sign of impaired outflow. d Endoscopic retrograde cholangiopancreatography (ERCP). The presence of Santorinicele is confirmed (arrowhead)
Clinical evaluation
The 21 patients with Santorinicele and ERCP confirmation underwent minor papilla sphincterotomy. One month after the procedure all patients reported a reduction in frequency and intensity of pancreatic-like abdominal pain and less occurrence of nausea and vomiting; in 16/21 patients (76 %) a normalization of blood levels of lipase and amylase was observed. Follow-up S-MRCP after sphincterotomy was performed in 12/21 patients (average 188 days after ERCP; range 13–314 days) (Fig. 3). Nine out of 21 patients who were totally asymptomatic after sphincterotomy refused to undergo further diagnostic procedures.
Female 49-year-old patient with Santorinicele before and after minor papilla sphincterotomy presenting abdominal pain and pancreatic hyperenzymemia. Before sphincterotomy: a Coronal MRCP image obtained by using T2-weighted HASTE sequence, TR/TE ∞/1,100 ms, slice thickness 60 mm. Main pancreatic duct (arrow) is not clearly depicted in basal conditions. b Coronal MRCP image 2 min after secretin administration. Both dorsal and ventral duct are depicted (top and bottom arrow, respectively). A small Santorinicele is visible (arrowhead). c Coronal MRCP image 8 min after secretin administration. Santorinicele is still visible, and duodenal filling with pancreatic juice (asterisk) is poor. d Endoscopic retrograde cholangiopancreatography (ERCP). The presence of Santorinicele is confirmed (arrowhead). Sphincterotomy of the minor papilla was performed during the ERCP. One month after sphincterotomy: e Coronal MRCP image 2 min after secretin administration. Santorinicele is not visible, and duodenal filling is clearly depicted (asterisk). f Coronal MRCP image 8 min after secretin administration. Duodenal filling is beyond duodenal genu inferius (asterisk), sign of normal pancreatic outflow; this demonstrates that sphincterotomy has resolved the situation of impaired pancreatic outflow
Duodenal filling with pancreatic juice
In the group with pancreas divisum without Santorinicele (54 patients) every patient had normal duodenal filling after secretin administration (grade 3). In the group with pancreas divisum and Santorinicele (27 patients), 16/27 (59 %) had normal duodenal filling; 10/27 (37 %) had slightly reduced filling (grade 2); 1/27 (3.7 %) had markedly reduced duodenal filling (grade 1). All the patients with duodenal filling of grade 1 and grade 2 (11 patients), and 10 with normal duodenal filling but severe abdominal pain underwent minor papilla sphincterotomy (total 21/27 patients). After the procedure, 12 of these patients (11 with previously impaired filling and one with normal filling) underwent a new S-MRCP to assess functional changes; a normal amount of pancreatic juice was visible in every patient (Fig. 3, Table 1).
Quantitative image analysis
The diameter of the dorsal pancreatic duct at the level of the pancreatic head in the group of patients with pancreas divisum and Santorinicele was significantly larger compared with that in patients with only pancreas divisum (p < 0.01), both in basal conditions (average 2.4 versus 1.9 mm) and after secretin administration (average 3.0 versus 2.4 mm).
After secretin administration a significant increase was seen in the maximum diameter of the Santorinicele compared with basal conditions (average 3.9 versus 2.5 mm, +36 %, p < 0.01) (Figs. 1, 2 and 4; Table 1).
The average ratio between Santorinicele and dorsal duct calibre was 1.08 in basal conditions, whereas it was 1.41 after secretin administration (p < 0.01).
After minor papilla sphincterotomy, a significant decrease of the calibre of Santorinicele was visible compared to the values before sphincterotomy (p < 0.01), both in basal conditions (average 1.9 versus 2.5 mm, −24 %) and after secretin administration (average 2.6 versus 3.9 mm, −33 %) (Figs. 3 and 4; Table 1). Dorsal duct calibre after sphincterotomy was significantly reduced (p < 0.01), both in basal conditions (average 1.9 versus 2.4 mm, −21 %) and after secretin administration (average 2.5 versus 3.0 mm, −17 %), with values similar to the patients with pancreas divisum without Santorinicele.
Discussion
The role of pancreas divisum in acute recurrent pancreatitis has been debated since 1976 [23]. The majority of patients with pancreas divisum have no clinical disease, but there is a subset of patients who have either unexplained abdominal pain or recurrent episodes of acute pancreatitis [8]. It has been suggested that a relative obstruction of the minor papilla in this subset of patients could intermittently impair the flow of pancreatic juice, resulting in increased endoluminal pressure and obstructive pancreatitis [8, 9].
In the past ERCP was considered the gold standard for the diagnosis of pancreas divisum [24, 25]. In recent years MRCP has been proposed as the most appropriate imaging technique for noninvasively investigating the pancreatic ductal configuration [12]. Secretin injection during MRCP (S-MRCP) enhances the morphology of the main pancreatic duct and gives information on pancreatic outflow dynamics [13–15].
In our study, pancreas divisum was depicted on MRCP images in 55/519 patients (11 %) with suspected pancreatic disease; after secretin administration we found 26 (5 %) additional patients with pancreas divisum, so the total prevalence of pancreas divisum in our series was 81/519 (16 %) by S-MRCP. Previous studies reported a similar prevalence of this anatomical condition: Delhaye et al. in 1985 found pancreas divisum in 6 % of the general population and 7 % in symptomatic patients by ERCP [25]; Manfredi et al. in 2000 found the anatomical variant in 10 % of patients with suspected pancreatic disease by S-MRCP [16]. DiMagno et al. in 2007 presented a review of several previous studies and concluded that the prevalence of pancreas divisum was between 4 and 12 %, both in symptomatic and asymptomatic patients [26]. Gonoi et al. in 2011 reported a prevalence of greater than 30 % in patients with chronic/recurrent pancreatitis, 13 % in patients with acute pancreatitis and less than 3 % in the control group [5].
In our series the majority of patients with pancreas divisum (79 %) presented the classical form (complete pancreas divisum), while 21 % presented incomplete pancreas divisum.
These results confirm that complete pancreas divisum is more common than the incomplete form, as suggested by previous studies [20, 21].
Every patient with pancreas divisum but one was Caucasian; this indicates an higher prevalence of the anatomical variant in Caucasian people compared with African and Oriental, as reported in the literature [3]; however, further studies are necessary because of the small number of non-Caucasian patients in our group (53 African and 7 Asian).
The diagnosis was confirmed by ERCP for every patient in which the procedure could be performed (57/81, 70 %). These results are in agreement with those of the literature [1, 16, 27], and confirm the primary role of S-MRCP in the diagnosis of pancreas divisum.
Santorinicele has been defined as a focal cystic dilatation of the termination of the dorsal pancreatic duct at the minor papilla [10]. It occurs primarily in patients with pancreas divisum, particularly in the subgroup who develop abdominal pain or acute pancreatitis [11]. In the past the diagnosis of Santorinicele was achieved only with ERCP [10]; in recent years S-MRCP has been proposed as the most appropriate technique to recognize morphological and functional alterations of the dorsal duct [2].
In our study, S-MRCP contributed significantly to detect Santorinicele since it was depicted on basal MRCP images in only 7/81 patients (8.6 %) and in additional 20 (25 %) patient after secretin administration (Fig. 1). No Santorinicele was found in patients with a normally fused pancreas or in patients with incomplete pancreas divisum. Overall Santorinicele was depicted by S-MRCP in 27/81 patients (33 %) with pancreas divisum. The diagnosis was confirmed by ERCP for every patient in which the procedure could be performed (21/27, 78 %) (Fig. 2). These results support the importance of pharmacological stimulation during MRCP to diagnose morphological alterations of the Santorini duct, in agreement with the literature [2, 17].
Gonoi et al. reported the presence of Santorinicele in an Asian population even in patients without pancreas divisum [28]; however, in our study we never depicted this condition, so it should be considered extremely rare in Western countries and it is not possible to assess its clinical implications.
To date there are no data available as to whether Santorinicele is a congenital or acquired condition; however, because of its rarity, the relatively young age of patients in our series and the high correlation with pancreas divisum, in our experience Santorinicele should be considered a congenital condition, rather than an acquired disease.
The diameter of the dorsal pancreatic duct in the group of patients with pancreas divisum and Santorinicele was significantly larger compared with that in patients with only pancreas divisum, both in basal conditions and after secretin administration; this proves the presence of impeded pancreatic secretion outflow at the level of the minor papilla, with subsequent increased intraductal pressure.
After secretin administration a significant increase was seen in the maximum diameter of the Santorinicele compared with basal conditions (Fig. 4, Table 1). The ratio between Santorinicele and dorsal duct calibre was higher after secretin administration compared with basal conditions; this confirms that MRCP images during secretin stimulation are the most useful to recognize the presence of Santorinicele.
According to the literature, minor papilla sphincterotomy is indicated in patients with Santorinicele and recurrent pancreatic-like abdominal pain with pancreatic hyperenzymemia [17]. The purpose of this procedure is to reduce endoluminal pressure and to prevent the onset of chronic obstructive pancreatitis [18].
In our study, after sphincterotomy, a decrease of the size of Santorinicele was visible compared with values before the procedure (Figs. 3 and 4). We found that MRCP images after secretin administration are better to assess results of sphincterotomy compared with MRCP images in basal conditions. The dorsal duct calibre after sphincterotomy was similar to the calibre of patients with pancreas divisum without Santorinicele, demonstrating the normalization of fluid dynamics (Table 1).
In 11/27 patients (41 %) with Santorinicele, impaired filling of the duodenum with pancreatic juice as a result of the relative obstruction of the minor papilla was visible by S-MRCP.
After minor papilla sphincterotomy, normal duodenal filling was visible in every patient by S-MRCP (Fig. 3, Table 1); this proves the utility of secretin administration during MRCP to assess the results of sphincterotomy.
After the endoscopic treatment, all patients reported a reduction in the pancreatic-like abdominal pain and an increase in the quality of life, with a normalization of blood levels of lipase and amylase in most of our patients. So, minor papilla sphincterotomy has to be considered the best treatment in the presence of pancreas divisum with Santorinicele.
Our study was limited by the retrospective nature of the investigation. Also, most of the patient population was composed of Caucasian patients and therefore non-Caucasian patients were not well represented. Furthermore in 24/81 patients with radiological findings of pancreas divisum ERCP was not performed; however, in 57/81 patients ERCP was performed and it always confirmed the presence of pancreas divisum.
Conclusion
Secretin administration increases the accuracy of MRCP in detecting Santorinicele and demonstrates the impaired filling of the duodenum with pancreatic juice. Therefore S-MRCP is useful to select patients who may benefit from endoscopic minor papilla sphincterotomy. Furthermore, S-MRCP is useful to assess the results of the procedure.
References
Manfredi R, Brizi MG, Tancioni V, Vecchioli A, Marano P (2001) Magnetic resonance pancreatography (MRP): morphology and function. Rays 26:127–133
Manfredi R, Brizi MG, Costamagna G, Masselli G, Vecchioli Scaldazza A, Marano P (2002) Pancreas divisum and Santorinicele: assessment by dynamic magnetic resonance cholangiopancreatography during secretin stimulation. Radiol Med 103:55–64
Liao Z, Gao R, Wang W et al (2009) A systematic review on endoscopic detection rate, endotherapy, and surgery for pancreas divisum. Endoscopy 41:439–444
Lerner A, Branski D, Lebenthal E (1996) Pancreatic diseases in children. Pediatr Clin North Am 43:125–156
Gonoi W, Akai H, Hagiwara K et al (2011) Pancreas divisum as a predisposing factor for chronic and recurrent idiopathic pancreatitis: initial in vivo survey. Gut 60:1103–1108
Stern CD (1986) A historical perspective on the discovery of the accessory duct of the pancreas, the ampulla 'of Vater' and pancreas divisum. Gut 27:203–212
Griffin N, Charles-Edwards G, Grant LA (2012) Magnetic resonance cholangiopancreatography: the ABC of MRCP. Insights Imaging 3:11–21
Cotton PB (1980) Congenital anomaly of pancreas divisum as cause of obstructive pain and pancreatitis. Gut 21:105–114
Gregg JA (1977) Pancreas divisum: its association with pancreatitis. Am J Surg 134:539–543
Eisen G, Schutz S, Metzler D, Baillie J, Cotton PB (1994) Santorinicele: new evidence for obstruction in pancreas divisum. Gastrointest Endosc 40:73–76
Seibert DG, Matulis SR (1995) Santorinicele as a cause of chronic pancreatic pain. Am J Gastroenterol 90:121–123
Bret PM, Reinhold C, Taourel P, Guibaud L, Atri M, Barkun AN (1996) Pancreas divisum: evaluation with MR cholangiopancreatography. Radiology 199:99–103
Matos C, Metens T, Deviere J et al (1997) Pancreatic duct: morphologic and functional evaluation with dynamic MR pancreatography after secretin stimulation. Radiology 203:435–441
Manfredi R, Costamagna G, Vecchioli A, Colagrande C, Spina S, Marano P (1998) Dynamic pancreatography with magnetic resonance after functional stimulus with secretin in chronic pancreatitis. Radiol Med 96:226–231
Nicaise N, Pellet O, Metens T et al (1998) Magnetic resonance cholangiopancreatography: interest of IV secretin administration in the evaluation of pancreatic ducts. Eur Radiol 8:16–22
Manfredi R, Costamagna G, Brizi MG et al (2000) Pancreas divisum and "Santorinicele": diagnosis with dynamic MR cholangiopancreatography with secretin stimulation. Radiology 217:403–408
Costamagna G, Ingrosso M, Tringali A, Mutignani M, Manfredi R (2000) Santorinicele and recurrent acute pancreatitis in pancreas divisum: diagnosis with dynamic secretin-stimulated magnetic resonance pancreatography and endoscopic treatment. Gastrointest Endosc 52:262–267
Lutzak GD, Gluck M, Ross AS, Kozarek RA (2013) Endoscopic minor papilla sphincterotomy in patients with Santoriniceles reduces pain and improves quality of life. Dig Dis Sci 58:2075–2081
Frulloni L, Falconi M, Gabbrielli A et al (2010) Italian consensus guidelines for chronic pancreatitis. Dig Liver Dis 42(Suppl 6):S381–S406
Quest L, Lombard M (2000) Pancreas divisum: opinio divisa. Gut 47:317–319
Spicak J, Poulova P, Plucnarova J, Rehor M, Filipova H, Hucl T (2007) Pancreas divisum does not modify the natural course of chronic pancreatitis. J Gastroenterol 42:135–139
Kamisawa T, Yuyang T, Egawa N, Ishiwata J, Okamoto A (1998) Patency of the accessory pancreatic duct in relation to its course and shape: a dye-injection endoscopic retrograde pancreatography study. Am J Gastroenterol 93:2135–2140
Rosch W, Koch H, Schaffner O, Demling L (1976) The clinical significance of the pancreas divisum. Gastrointest Endosc 22:206–207
Benage D, McHenry R, Hawes RH, O'Connor KW, Lehman GA (1990) Minor papilla cannulation and dorsal ductography in pancreas divisum. Gastrointest Endosc 36:553–557
Delhaye M, Engelholm L, Cremer M (1985) Pancreas divisum: congenital anatomic variant or anomaly? Contribution of endoscopic retrograde dorsal pancreatography. Gastroenterology 89:951–958
DiMagno MJ, Wamsteker EJ (2011) Pancreas divisum. Curr Gastroenterol Rep 13:150–156
Fukukura Y, Fujiyoshi F, Sasaki M, Nakajo M (2002) Pancreatic duct: morphologic evaluation with MR cholangiopancreatography after secretin stimulation. Radiology 222:674–680
Gonoi W, Akai H, Hagiwara K et al (2013) Santorinicele without pancreas divisum pathophysiology: initial clinical and radiographic investigations. BMC Gastroenterol 13:62
Acknowledgments
The scientific guarantor of this publication is Roberto Pozzi Mucelli. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. The authors consulted a colleague (William Mantovani, MD, Department of Statistic, Policlinico G.B. Rossi, Verona) with significant statistical expertise. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boninsegna, E., Manfredi, R., Ventriglia, A. et al. Santorinicele: secretin-enhanced magnetic resonance cholangiopancreatography findings before and after minor papilla sphincterotomy. Eur Radiol 25, 2437–2444 (2015). https://doi.org/10.1007/s00330-015-3644-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3644-0