Abstract
The co-occurrence of IgA nephropathy (IgAN) and positive anti-neutrophil cytoplasmic autoantibodies (ANCA) serology is uncommon. In the present case series and literature review, we aimed to clarify the impact of ANCA on pathogenesis, clinical and histopathology presentation, and outcome in IgAN patients. We report four patients with an overlap lesion of IgAN–ANCA positive. Also, we performed a narrative review of all biopsy-proven published case series. Only 1.2% patients had ANCA in our 330-biopsy-proven IgAN cohort. We compared our data with previous reports—6 case series and 3 small retrospective studies—a total of 103 patients. All patients but one had eGFR below 15 mL/min at diagnosis. Besides rapidly decreasing eGFR, all presented with proteinuria around 1.5 g/day and dysmorphic microhematuria, suggesting glomerular inflammation. Systemic symptoms suggestive for ANCA vasculitis were seen in half of our patients, but only one patient had hemorrhagic alveolitis. Patients from our cohort responded to the intensive immunosuppressive regimens used in ANCA-positive vasculitis with renal involvement. However, in the follow-up, one patient had a relapse followed by septic shock related to immunosuppression and one patient started hemodialysis. In the review, we found that IgAN–ANCA -positive patients are characterized by vasculitis-like lesions and clinically by a rapidly progressive decline in kidney function, which was reversed by an aggressive induction immunosuppressive protocol used in ANCA vasculitis. Checking ANCA serology seems useful in patients with rapidly progressive IgAN for therapeutic and prognostic reasons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunoglobulin A nephropathy (IgAN), the most common primary glomerulonephritis, usually manifests as a stable or slowly progressive kidney disease, with 30% of patients reaching end stage kidney disease (ESKD) 20 years after diagnosis [1]. However, a subset of IgAN patients (< 10%) has an acute or a subacute, rapidly progressive, course [2].
A small proportion of patients with biopsy-proven IgAN, ranging between 0.2 and 2%, can have circulating anti-neutrophil cytoplasmic autoantibodies (ANCA). Data regarding pathogenesis, clinical presentation, pathologic features, and outcome of IgAN in these patients are limited and contradictory [2]. Moreover, ANCA serology is diagnostic for ANCA associated vasculitis only in the presence of a certain histopathologic and clinical phenotype [3]. As ANCA-seropositive IgAN patients share some histopathologic and clinical features with those with ANCA vasculitis, i.e., crescent formation and rapidly progressive nephritic syndrome, the relationship between IgAN and ANCA vasculitis is unclear. It may be either fortuitous, resulting from the high incidence of IgAN in the general population, or pathogenically linked.
In the present case series, we report four seropositive ANCA patients with IgAN and perform a narrative review of the literature on the topic; we aimed to clarify the impact of ANCA seropositivity on IgAN pathogenesis, clinical and histopathology presentation, and outcome.
Methods
Case selection
Clinical and histologic data from 330 patients diagnosed in our department with IgAN between 2010 and 2020 were retrospectively analyzed for the concomitant presence of ANCA associated vasculitis.
Four renal biopsy specimens were identified which met the following inclusion criteria: (i) an IgAN diagnosis based on light microscopic findings of mesangial proliferative changes, dominant or codominant mesangial IgA deposition (with variable IgG and C3) by immunofluorescence, and mesangial electron-dense deposits at electron microscopy; (ii) the presence of extracapillary proliferation, with or without segmental necrosis of glomerular capillaries; (iii) a positive serum test for anti-PR3 and/or anti-MPO by ELISA. ANCA seropositivity was defined as an ANCA titer higher than 10 U/mL.
We excluded patients with Henoch–Schönlein purpura, those with secondary glomerulonephritis, and those with insufficient clinical and pathologic data.
Pathologic analysis
For each biopsy specimen, light microscopy, immunofluorescence, and electron microscopy were routinely performed. One pathologist reviewed independently the slides without knowledge of the original biopsy diagnosis, typically several months after the original pathology report.
The histological analysis included an in-depth review of the glomerular, tubulointerstitial, and vascular compartments. Definitions of histologic variables used in our study were derived from the Mayo Clinic/Renal Pathology Society Consensus [4].
Immunofluorescence microscopy was performed using antibodies against IgA, IgG, IgM, C1q, C3c, kappa, and lambda. The staining intensity was rated from “+” (weak, trace) to “+ + +” (strong). The presence of dense deposits in the glomerulus was assessed by electron microscopy.
Search strategy
Case-based strategy was performed according to the recommendations of the Journal [5]. MEDLINE/PubMed, Scopus, and Web of Science databases were searched. The following keywords were used for searching strategy: IgAN (glomerulonephritides IgA, IgA glomerulonephritis, immunoglobulin A nephropathy, and Berges disease) and ANCA-associated vasculitis (anti-neutrophil cytoplasmic autoantibody, granulomatosis with polyangiitis, Wegener granulomatosis, ANCAc, proteinase 3 ANCA, PR3-ANCA, microscopic polyangiitis, ANCAp, myeloperoxidase ANCA, and MPO-ANCA).
Only case series published in English between 1982 and 2020 which reported on the clinical presentation, histopathology, and outcome of patients with ANCA-positive IgA crescentic nephropathy were included in the present review. We only included case series, since single patient case reports do not allow the estimation of an effect size and only provide descriptive or narrative results. Studies were excluded if they: did not meet to aforementioned criteria and were not written in English (Fig. 1 from supplementary material).
Results
Baseline clinical characteristics and response to treatment
Clinical data for the four patients with ANCA-positive crescentic IgAN are depicted in Table 1.
Median age at diagnosis was 61.5 years; three patients were men. All patients were positive for MPO-ANCA, while other test results for autoantibodies (i.e., antinuclear, anti-dsDNA, anti-glomerular basement membrane antibodies, PR3-ANCA, and cryoglobulins) were negative. Complement levels were in normal limits in all patients.
All patients had full-blown acute nephritic syndrome at diagnosis: microscopic hematuria with dysmorphic red blood cells (median 220 RBC/HPF) but not macroscopic hematuria, proteinuria (median 1.9 g/g creatinine, nephrotic range in one patient), high serum creatinine (median 3.8 mg/dL), and hypertension. Two patients had systemic symptoms such as fever and arthralgia. In one patient, the clinical presentation included pulmonary involvement with alveolar hemorrhage (hemoptysis and bilateral pulmonary infiltrates on a CT scan).
All patients received induction immunosuppressive therapy with corticosteroids (pulse methylprednisolone, 7–15 mg/kg-day for 3 days; followed by oral prednisone 0.5–1 mg/kg-day tapered to 0.25 mg/kg/day by 1 month, 15 mg/day at 3 months, 10 mg/day at 4 months and 5 mg/day from 5 to 12 months) and cyclophosphamide (cyclophosphamide, 500 mg/m2 every 4 weeks) for 6 months. Azathioprine (2.0 mg/kg per day, maximum dose 200 mg/day) was used as maintenance therapy in all patients for at least 12 months after remission. No patient required renal replacement therapy during the acute phase.
All patients except one responded to induction therapy. However, in patient 1, a relapse-renal limited vasculitis was observed 5 years after diagnosis. The flare was managed using the same induction protocol. Three months while on induction therapy, this patient developed septic shock due to Pseudomonas aeruginosa pneumonia and died.
Patient 2 had a stable although low kidney function and nephrotic proteinuria. Hemodialysis was started after 5 months, due to intractable extracellular volume overload.
Patients 3 and 4, which had similar severely altered kidney function at baseline, showed a rapid renal improvement, especially patient 4 (a decline in serum creatinine from 7.3 to 3.2 mg/dL in 1 week). Moreover, patient 3 had normal serum creatinine after 3 months.
Histologic features
The histopathology findings are summarized in Table 2.
The tissue submitted for light microscopy consisted of renal cortex with a number of glomeruli ranging from 4 to 32.
Glomeruli with cellular and fibrocellular crescent formation were observed in all cases (Fig. 1b). The percentages of the glomeruli with extracapillary hypercellularity ranged between 14 and 75% of the examined glomeruli. No fibrinoid glomerular tuft necrosis was noted in any case. In only one case, fibrinoid necrosis was observed in the wall of an interlobular sized artery.
a Immunofluorescence microscopy image shows intense (3 +) mesangial IgA staining with a granular pattern (200 ×); b light microscopy image shows a glomerulus with a segmental cellular crescent and a segment of tuft sclerosis (toluidine blue stain of plastic embedded tissue; 200 ×); c electron microscopy image demonstrating small dense deposits located in the paramesangial area with associated severe foot process effacement and podocyte activation; d electron microscopy image shows a large dense deposit located in the mesangium
Glomeruli which demonstrated global glomerulosclerosis were noted in all cases, ranging from 14 to 37% of the examined glomeruli. One case had mesangial hypercellularity and another had focal endocapillary hypercellularity. Two cases had glomeruli with focal and segmental capillary tuft sclerosis.
The degree of interstitial fibrosis and tubular atrophy was rated as mild in one case and as moderate in the other three cases. Focal red blood cells and red blood cells casts were noted in the lumen of some tubules, as well as protein casts.
All cases showed dominant IgA staining in the mesangium (Fig. 1a). The glomeruli were also positive for IgG, C3, kappa, and lambda. No staining in the capillary wall was noted in any case. None of the cases showed any staining for C1q.
Electron microscopy demonstrated immune complex type electron-dense deposits in the paramesangial area in all cases (Fig. 1c). Mesangial deposits were observed in 3 cases (Fig. 1d). Only one case had focal small subepithelial and intramembranous dense deposits. The degree of foot process effacement was rated as severe in all cases, with associated podocyte activation and microvillous transformation.
Narrative review of IgAN–ANCA -positive case series
We compared our data with previous reports—6 case series and 3 small retrospective studies—a total of 103 patients (Table 3). The reported proportion of patients IgAN–ANCA -positive ranges between 0.2 and 2% in IgAN kidney biopsies [2].
Most of the patients with IgAN–ANCA positive presented with rapidly declining kidney function and an active urinary sediment (Table 3). In a study which compared kidney parameters in IgAN–ANCA positive with IgAN, gross hematuria was more frequent and eGFR was lower in IgAN–ANCA positive, 67 vs. 23% and 21 vs. 47 mL/min [6, 7].
However, slowly progressive kidney failure, without extracapillary proliferation or focal necrosis, has been also described in IgAN–ANCA -positive patients. O’Donoghue et al. screened 100 patients with IgAN and found two patients who were positive for ANCA, but these patients had no crescents and a slowly decreasing kidney function, similar to ANCA seronegative IgAN patients [8].
Systemic symptoms suggestive for ANCA vasculitis were reported in more than half of the patients, and also lung involvement—hemorrhagic alveolitis—was reported in 43% of the patients (Tables 3 and 4).
The reported percentage of crescents found in patients with IgAN–ANCA positive is variable, ranging from 8 to 30% for cellular crescents and from 14 to 29% for fibrous crescents (Table 3). Haas et al. compared the ANCA positive and ANCA negative forms of crescentic IgAN and found no difference in the mean percentage of crescents estimated to occupy >50% of the glomerular cross-sectional area or in the mean percentage of crescentic glomeruli with breaks in Bowman’s capsule [9]. This finding may suggest that ANCA is an epiphenomenon, accompanying but not necessarily driving crescent formation in IgAN.
However, the ANCA-positive patients had limited mesangial and endocapillary hypercellularity (Table 4) [9].
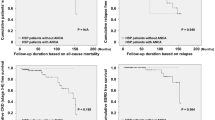
In a Chinese cohort of 1729 IgAN patients, Yang et al. found only 20 (1.2%) patients with a positive serology for ANCA. As compared to ANCA negative patients, they were older and had a more aggressive presentation—lower eGFR (21.2 versus 47.0 mL/min), higher gross hematuria (66.7 versus 22.5%), and more fibrinoid necrosis (35 versus 0%). IgAN–ANCA -positive patients were more responsive to immunosuppression, with a higher renal recovery from dialysis (75% versus 0%, p = 0.01) and a tendency to less ESKD after 6 months (0.77 versus 0.26 events/person/year, p = 0.09) [6].
In the largest series reported to date, Xie et al. found 35 (1.4%) IgAN patients with ANCA from 2390 Chinese patients with biopsy-proven IgAN. Among them, 14 (40%) had systemic symptoms. They showed lower levels of eGFR (24.2 versus 100.1 mL/min, p = 0.002), higher incidence of rapidly deteriorating kidney function (28.6 versus 0.0%, p = 0.039) and lower cumulative renal survival rate (7 versus 25 months, p < 0.001). These data suggest that systemic symptoms evaluated with Birmingham Vasculitis Activity Score (BVAS) are predictive for outcome in IgAN–ANCA patients, supporting a pathogenic role for ANCA. Regarding the renal histopathology, when compared with 40 randomly selected ANCA negative IgAN patients, there were no significant differences in cellular or fibrous crescents, global glomerulosclerosis, endocapillary hypercellularity, and tubular atrophy [10].
Discussion
In the present case series, we report the clinical and histologic features of four patients with crescentic IgAN coexisting with an ANCA-positive serology and compared them to previous reported case series. We found a proportion of 1.2% patients with ANCA positivity in our IgAN biopsy-proven cohort, similar to the one previous reported.
In our case series, all patients but one had eGFR below 15 mL/min at diagnosis. Besides rapidly decreasing eGFR, all patients presented with proteinuria around 1.5 g/day and dysmorphic microhematuria, suggesting glomerular inflammation. These results are in line with previous reports in which IgAN–ANCA -positive patients presented with acute nephritic syndrome.
Systemic symptoms suggestive for ANCA vasculitis were seen in half of our patients, but only one patient had hemorrhagic alveolitis, in contrast to reported series in which pulmonary involvement was reported in almost 40% of the patients [6]. Inflammation was also preeminent in our patients (Tables 1, 4). Moreover, in the single study which compared seropositive ANCA IgAN to rapidly progressive IgAN and to ANCA vasculitis, the clinical manifestations ANCA-positive IgAN were similar to those found in ANCA vasculitis [6]. Thus, the clinical phenotype of ANCA-seropositive IgAN—rapidly progressive nephritic syndrome and systemic symptoms with pulmonary involvement—seems distinctive from rapidly progressive IgAN and closer to ANCA vasculitis [2].
IgA deposits are commonly found in the general population, but only a few patients develop IgAN. Mesangial IgA deposits were reported in 5% of patients without known kidney disease in an autopsy study [11]. On the other hand, ANCA seropositivity was reported in variable proportion in conditions other than ANCA vasculitis, including IgAN and other glomerulonephritis [3, 12]. Thus, ANCA seropositivity in rapidly progressive IgAN could be either the superposition of an ANCA associated vasculitis on a preexistent IgAN or an increase in ANCA titer because of the pro-inflammatory environment generated by the glomerular lesions induced by IgA deposits. However, in both cases, a certain pathogenic link could exist.
It is also possible to look at ANCA seropositivity as a rare epiphenomenon of the immunologic abnormalities of IgAN. Interestingly, serum IgA ANCA autoantibodies with a relatively low affinity for the antigen or/and present in small amounts in the circulation have been reported in ANCA vasculitis. However, serum IgA ANCA are not useful for the diagnosis of IgA vasculitis (i.e., Henoch-Schönlein purpura) and their pathogenic role remains uncertain [13, 14].
While specificity and sensitivity of a positive ANCA test are high for ANCA vasculitis when the clinical manifestation is evocative, about 2.1% positive tests are false-positive [12]. However, the ANCA level of antibody detected in false-positive patients is towards the low end of the detectable range [15]. In our study, the ANCA titer was significantly increased in all the cases (Table 1). Moreover, the titer remained increased at follow-up.
On the other hand, the decision to order a test for ANCA may be hampered by the overlap in clinical presentation between ANCA vasculitis and IgAN. Therefore, the delay in diagnosis could be related to physician non-acquaintance with this clinical association, precluding earlier ANCA testing and efficient immunosuppressive treatment. Nevertheless, this could also explain the low frequency of reported rapidly progressive nephritic IgAN associated with ANCA vasculitis.
Another argument for ANCA being a culprit in rapidly progressive nephritic IgAN comes from response to treatment and outcome. All patients from our cohort and most patients reported by other investigators responded very well to the intensive immunosuppressive regimens used in ANCA-positive vasculitis with renal involvement [16], in contrast to rapidly progressive IgAN where the response to aggressive immunosuppression was poorer (ESKD after 6 months 0.26 vs. 0.77 events/patients-years) [6].
The simultaneous occurrence of two distinct pathological processes—IgAN and ANCA vasculitis—could be coincidental due to the increased prevalence of IgAN in the general population. However, the possibility that the presence of one condition may predispose to the other still exists. The pathological interplay between IgAN and ANCA-associated vasculitis is still a matter of debate. Some authors suggested that IgA transitory deposits are the first inflammatory step in the pathogenesis of ANCA-associated vasculitis. However, Bantis et al. reported IgA deposits in kidney biopsy specimens 6 months after treatment [16]. Moreover, the clinical features of IgAN–ANCA -positive patients resemble both IgAN and the ANCA associated vasculitis. Thus, ANCA could be “associated” with IgAN by playing a role in the acute phase of the disease [16].
Ma et al. studied complement activation in patients with IgAN and in those with ANCA-associated vasculitis with or without IgA deposition, and found that the complement was activated on the alternative pathway in all three groups [17]. However, in IgAN–ANCA -positive patients, the complement was activated also on the classic pathway, and serum C1q and IgA levels were directly correlated (Fig. 2, Table 4) [17].
ANCA vasculitis (red). A pro-inflammatory environment initiates the production of ANCA by plasma cells as well as neutrophils priming through cytokines. ANCA bind to myeloperoxidase (MPO) and proteinase 3 (PR3) on the surface of primed neutrophils causing the release of reactive oxygen species, and lytic enzymes, and excessive activation. Subsequent release of neutrophil extracellular traps (NETs) causes the development of ANCA vasculitis with vessel inflammation and hemorrhage. IgAN (green). The serum level of IgA1 bearing galactose-deficient O-glycans (Gd-IgA1) is increased. Gd-IgA1 are recognized as autoantigens by antiglycan autoantibodies (anti-Gd-IgA1), with the formation of circulating nephritogenic immune complexes. Some of these immune complexes deposit in the kidney and activate mesangial cells. In response, mesangial cells proliferate and produce in excess extracellular matrix, cytokines, and chemokines, leading to podocyte apoptosis and proteinuria. Alternative and lectin complement pathways are active in both diseases; however, patients with IgAN–ANCA vasculitis also had the activation of the classic complement pathway as reported by Ma et al. [17]
There are several limitations regarding the present case series and literature review. The ANCA positivity in IgAN patients being rare (probably because seldom checked), the studies reported heterogeneous clinical presentation, treatment, and outcome, explaining the lack of consensus on this topic. Moreover, we included only case series in our review, which might hamper the epidemiologic evaluation of IgAN–ANCA -positive patients. ANCA was determined in our case series only by ELISA; however, the ANCA titer was significantly increased in all the cases. While the induction therapy with corticosteroids and cyclophosphamide was efficient in the reported studies, the protocols, the follow-up period, and the definition of outcomes were highly different. Therefore, randomized clinical trials to evaluate the efficiency of immunosuppressive treatment in IgAN–ANCA-positive patients are needed.
In conclusion, we report a subset of patients with ANCA-positive crescentic IgAN characterized histopathologically by vasculitis-like lesions and clinically by a rapidly progressive decline in kidney function, which was reversed by an aggressive induction immunosuppressive protocol used in ANCA-positive vasculitis. Therefore, checking ANCA serology seems useful in patients with rapidly progressive IgAN for therapeutic and prognostic reasons.
Data availability
Data extracted from the included studies in this review are available on request from the corresponding author.
References
Lai KN, Tang SC, Schena FP, Novak J, Tomino Y, Fogo AB, Glassock RJ (2016) IgA nephropathy. Nat Rev Dis Primers 2:16001. https://doi.org/10.1038/nrdp.2016.1
Rojas-Rivera J, Fernandez-Juarez G, Praga M (2015) Rapidly progressive IgA nephropathy: a form of vasculitis or a complement-mediated disease? Clin Kidney J 8(5):477–481. https://doi.org/10.1093/ckj/sfv095
Savige J, Davies D, Falk RJ, Jennette JC, Wiik A (2000) Antineutrophil cytoplasmic antibodies and associated diseases: a review of the clinical and laboratory features. Kidney Int 57(3):846–862. https://doi.org/10.1046/j.1523-1755.2000.057003846.x
Sethi S, Haas M, Markowitz GS, D’Agati VD, Rennke HG, Jennette JC, Bajema IM, Alpers CE, Chang A, Cornell LD, Cosio FG, Fogo AB, Glassock RJ, Hariharan S, Kambham N, Lager DJ, Leung N, Mengel M, Nath KA, Roberts IS, Rovin BH, Seshan SV, Smith RJ, Walker PD, Winearls CG, Appel GB, Alexander MP, Cattran DC, Casado CA, Cook HT, De Vriese AS, Radhakrishnan J, Racusen LC, Ronco P, Fervenza FC (2016) Mayo Clinic/Renal Pathology Society consensus report on pathologic classification, diagnosis, and reporting of GN. J Am Soc Nephrol 27(5):1278–1287. https://doi.org/10.1681/ASN.2015060612
Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD (2011) Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int 31(11):1409–1417. https://doi.org/10.1007/s00296-011-1999-3
Yang YZ, Shi SF, Chen YQ, Chen M, Yang YH, Xie XF, Zou R, Lv JC, Liu LJ, Zhang H (2015) Clinical features of IgA nephropathy with serum ANCA positivity: a retrospective case-control study. Clin Kidney J 8(5):482–488. https://doi.org/10.1093/ckj/sfv078
Allmaras E, Nowack R, Andrassy K, Waldherr R, van der Woude F, Ritz E (1997) Rapidly progressive IgA nephropathy with anti-myeloperoxidase antibodies benefits from immunosuppression. Clin Nephrol 48(5):269–273
O’Donoghue DJ, Nusbaum P, Noel LH, Halbwachs-Mecarelli L, Lesavre P (1992) Antineutrophil cytoplasmic antibodies in IgA nephropathy and Henoch-Schonlein purpura. Nephrol Dial Transplant 7(6):534–538
Haas M, Jafri J, Bartosh SM, Karp SL, Adler SG, Meehan SM (2000) ANCA-associated crescentic glomerulonephritis with mesangial IgA deposits. Am J Kidney Dis 36(4):709–718. https://doi.org/10.1053/ajkd.2000.17615
Xie L, He J, Liu X, Tang S, Wang W, Li F, Zhang Y, Zhang J, Huang Y, Zhao J, Li Y, Zhang J (2018) Clinical value of systemic symptoms in IgA nephropathy with ANCA positivity. Clin Rheumatol 37(7):1953–1961. https://doi.org/10.1007/s10067-017-3931-z
Waldherr R, Rambausek M, Duncker WD, Ritz E (1989) Frequency of mesangial IgA deposits in a non-selected autopsy series. Nephrol Dial Transplant 4(11):943–946. https://doi.org/10.1093/ndt/4.11.943
Mandl LA, Solomon DH, Smith EL, Lew RA, Katz JN, Shmerling RH (2002) Using antineutrophil cytoplasmic antibody testing to diagnose vasculitis: can test-ordering guidelines improve diagnostic accuracy? Arch Intern Med 162(13):1509–1514. https://doi.org/10.1001/archinte.162.13.1509
Ronda N, Esnault VL, Layward L, Sepe V, Allen A, Feehally J, Lockwood CM (1994) Antineutrophil cytoplasm antibodies (ANCA) of IgA isotype in adult Henoch-Schonlein purpura. Clin Exp Immunol 95(1):49–55. https://doi.org/10.1111/j.1365-2249.1994.tb06013.x
Kelley JM, Monach PA, Ji C, Zhou Y, Wu J, Tanaka S, Mahr AD, Johnson S, McAlear C, Cuthbertson D, Carette S, Davis JC Jr, Dellaripa PF, Hoffman GS, Khalidi N, Langford CA, Seo P, St Clair EW, Specks U, Stone JH, Spiera RF, Ytterberg SR, Merkel PA, Edberg JC, Kimberly RP (2011) IgA and IgG antineutrophil cytoplasmic antibody engagement of Fc receptor genetic variants influences granulomatosis with polyangiitis. Proc Natl Acad Sci USA 108(51):20736–20741. https://doi.org/10.1073/pnas.1109227109
Deshpande P, Lucas M, Brunt S, Lucas A, Hollingsworth P, Bundell C (2016) Low level autoantibodies can be frequently detected in the general Australian population. Pathology 48(5):483–490. https://doi.org/10.1016/j.pathol.2016.03.014
Bantis C, Stangou M, Schlaugat C, Alexopoulos E, Pantzaki A, Memmos D, Ivens K, Heering PJ (2010) Is presence of ANCA in crescentic IgA nephropathy a coincidence or novel clinical entity? A case series. Am J Kidney Dis 55(2):259–268. https://doi.org/10.1053/j.ajkd.2009.09.031
Ma Y, Chen L, Xu Y, Han Q, Yu B, Zhao J, Hua Z, Yang Y, Chen J, Han F (2019) The clinicopathologic characteristics and complement activation of antineutrophil cytoplasmic antibody-associated vasculitides with glomerular IgA deposition. Appl Immunohistochem Mol Morphol. https://doi.org/10.1097/PAI.0000000000000819
Shimizu M, Wada T, Sakai N, Izumiya Y, Furuichi K, Misaki T, Kobayashi K-I, Goshima S, Takeda S-I, Yokoyama H (2000) Clinicopathological features of antineutrophil cytoplasmic antibodies- associated vasculitis in Japanese patients with IgA nephropathy. Clin Exp Nephrol 4:251–256
Funding
This study received no specific fund from any public, commercial, or not-for-profit agency.
Author information
Authors and Affiliations
Contributions
GS and GTB conceived and designed the protocol for this study and drafted the manuscript; SS and AZ did the search and reviewed completeness and validity of extracted data; MG and GM assisted with revision of the manuscript and methodological design of the study. All authors approved the final version of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest or competing interests.
Ethical approval
The study was approved by the institutional review board of Dr Carol Davila Teaching Hospital of Nephrology, Bucharest, Romania (approval number 2020–030).
Informed consent
Informed consent was not required in view of the retrospective study design and the anonymity of the patient records reviewed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ștefan, G., Terinte-Balcan, G., Stancu, S. et al. IgA nephropathy with serum ANCA positivity: case series and literature review. Rheumatol Int 41, 1347–1355 (2021). https://doi.org/10.1007/s00296-021-04888-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-021-04888-2