Abstract
To study the association of smoking status and the level of seropositivity in RA patients from COMORA Cohort. A post hoc analysis of COMORA database included 3439 RA patients was performed. Current smokers or recently quitted (< 3 years) were initially compared to those who never smoked or stopped > 3 years (Group I vs. II) regarding their seropositivity status (high positive, low positive and negative) for Rheumatoid Factor (RF) or Anti-citrullinated antibodies (ACPA). A further comparison was made between current smokers (Group III) and never smoked patients (Group IV). Analysis was also done on the individual country level for the 17 countries included in the COMORA study. Out of 3439 RA patients, 705 (20.5%) were smokers (group I), and 2734 (79.5%) were non-smokers (group II). Significantly more patients in group I, 442 (62.7%), had high levels of seropositivity than those in group II, 1556 (56.9%), [P = 0.006, OR 1.27 (95% CI, 1.07–1.5)]. More current smoker patients (group III—286 out of 456 “62.7%”) had high levels of seropositivity than never smoked patients (group IV—1236 out of 2191 “56.4%”), with significant difference [P = 0.013, OR 1.3 (95% CI, 1.06–1.6)]. In 11 countries, higher proportions of patients with high level of seropositivity in group I was found, with statistical significance in four countries. Smoking was associated with higher level of seropositivity in patients with RA in this post hoc analysis, both on a global level and in certain individual countries. As smoking is a modifiable risk factor, studying the effects of quitting smoking on level of seropositivity and other disease parameters is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Smoking is an environmental risk factor in several inflammatory diseases, including RA [1, 2]. In RA, studies connect smoking to several aspects of the disease including disease pathogenesis, prognosis, and response to treatment. Cigarette smoking was directly associated with the risk of developing RA [3, 4]. Kazantseva et al. [5] suggested that the effect of smoking on dendritic cell behavior in joints has relevance to both early and late phases of the disease pathogenesis. Smokers have an increased frequency of raised RF [6] and have an earlier onset of the disease [7] with an increased incidence of extra-articular manifestations including the development of rheumatoid nodules [8, 9]. They also have significantly higher radiological damage and Larsen’s score compared with nonsmokers [10]. Smoking was shown to be a risk factor for poor response to treatment in RA patients with disease-modifying anti-rheumatic drugs (DMARDs) and with tumor necrosis factor inhibitors (TNFi) [8]. Moreover, mortality rates in people with rheumatoid arthritis (RA) who smoke are significantly higher than those who have never smoked [11].
The association of smoking and RA is particularly strong for seropositive RA, defined as either rheumatoid factor [RF] and/or anti-citrullinated peptide antibody [ACPA] positive [12]. Smoking may contribute up to 35% of the attributable risk for seropositive RA [13]. In a large meta-analysis, the summary odds ratio (OR) for never, current and past smokers were 2.35 (1.64–3.35), 3.14 (1.70–5.82) and 2.35 (1.58–3.51) for RF-positive RA. On the contrary for RF-negative RA, the summary OR for never, current and past smokers were 0.90 (0.52–1.27), 1.31 (0.62–2.76) and 0.96 (0.61–1.51) [14]. Active smoking at the onset of the disease promotes the production of IgM and IgA RF regardless of whether smoking was stopped after RA discovery [7, 15]. Smoking acts as a trigger for anti-citrulline immunity and does so mainly in the context of certain HLA genes, and certain other genetic risk factors [16]. Studies in different cohorts of RA have revealed that tobacco exposure increases the risk of anti-citrullinated peptide antibodies (ACPAs) formation, especially in carriers of the shared epitope [17, 18]. The relation between smoking and seropositivity has been frequently addressed, but little is known about the relation of smoking to the level of seropositivity [19]. Furthermore, as previous studies in that context were conducted in restrictive parts of the world, and comorbidities of rheumatoid arthritis (COMORA) study has been conducted globally in different parts of the world involving several countries from 5 continents, therefore COMORA represented a good opportunity to check whether the previously reported association between smoking and seropositivity do exist in different parts of the world.
The aim of this study is to explore the association between smoking and the level of seropositivity in individuals with RA on the global COMORA cohort and on individual country level.
Patients and methods
This study is a post hoc analysis of COMORA data. COMORA is a cross-sectional, observational, multicenter, international study in which 3920 patients were recruited from several rheumatology centers that belong to 17 countries from 5 continents. The study was conducted in accordance with good clinical practice and approved by all local research ethical committees. Written informed consents were obtained from patients visiting the participating sites. Patients were enrolled when fulfilling COMORA inclusion criteria [20]. Data for this study were extracted from the COMORA database after approval of the COMORA scientific committee. The current study included 3439 patients that had a complete set of data with no missing or incomplete data, out of the full COMORA enrolled patients (3920 patients), as 481 patients with missing/incomplete data concerning smoking and/or seropositivity level were excluded with finally 3439 patients enrolled.
Smoking status in COMORA was recorded as one of four categories (current smokers, quitters < 3 years, quitters > 3 years, never smoked), while, seropositivity in COMORA dataset was recorded as serology negative (values < / = upper limit of Normal (ULN) for RF and ACPA); low positive (values > ULN and < / = 3 × ULN for RF and/or ACPA); and high positive (with values > 3 times ULN for RF and/or ACPA). In the present study, current smokers and those who stopped smoking for less than 3 years were grouped together as group I and their seropositivity were compared to group II that included never smoked RA patients and those who stopped smoking for more than 3 years. Next, current smokers (Group III) and never smoked (Group IV) were compared. After the global comparisons, data of individual countries of the COMORA study were analyzed in the same context for the association of smoking to the level of seropositivity. We further divided the countries into 5 regions namely North America, South America, Asia, North Africa, and Europe.
Statistical analysis
Data were statistically described in terms of mean, standard deviation (SD), median and range, or frequencies (number of cases) and percentages when appropriate. Comparison of numerical variables between the study groups was done using Student’s t test for independent samples when variables were normally distributed and Mann–Whitney U test for independent samples when not normally distributed. For comparing categorical data, Chi-square test was performed. Exact test was used instead when the expected frequency is less than 5. P values less than 0.05 was considered statistically significant. All statistical calculations were done using computer program SPSS (Statistical Package for the Social Science; SPSS Inc. Chicago, IL, USA) version 15 for Microsoft Windows.
Results
The demographic characteristics of the 3439 studied patients are shown in Table 1 and are comparable to the total COMORA cohort. Group I patients (current and quitters < 3 years) are 705 patients (20.5%), while 2734 (79.5%) comprised Group II (Never and quitters > 3 years). Distribution of RF and/or ACPA level of positivity showed that 58.1% were high positive, 23.4% were low positive and 18.5% were seronegative. Distribution of smoking and seropositivity status are shown in Table 2.
Regarding the level of positivity in the cohort, 442 out of 705 patients (62.7%) in Group I were highly positive, in comparison to 1556 patients (56.9%) in Group II, and the difference was statistically highly significant [OR = 1.27 (95% CI 1.07–1.5)], P = 0.006. Subsequently, more patients in group II (n = 666, 24.4%) had a low level of seropositivity when compared to group I (n = 139, 19.7%) and the difference was statistically significant [OR = 0.76 (95% CI 0.62–0.94), P = 0.009. Comparing Group III (current smokers—456 patients) to Group IV (never smoked—2191 patients), more patients with higher levels of seropositivity are found in group III (62.7%) compared to group IV (56.4%) and the difference was statistically significant [OR = 1.3 (95% CI 1.06–1.6), P = 0.013] (Table 3).
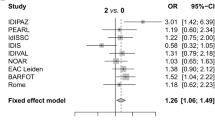
Looking at the individual country level, out of the 17 studied countries, 11 showed higher proportions of patients with a high level of seropositivity in group I compared to group II. The association achieved statistical significance in four countries, namely Italy, Egypt, Taiwan, and the United States of America (USA) Table 4 describes the association of high seropositivity level and smoking status in the individual countries included in the COMORA study. Testing the relationship between smoking and the level of seropositivity, in different regions of the world showed a statistically significant relationship in North America, Asia, and North Africa but not in South America, and Europe (Table: supplementary material).
Discussion
Seropositivity has diagnostic and prognostic importance in RA. Elevated level of RF/ACPA is important as well, and a high level had more weight in the most recent classification criteria [21]. In a study of patients with early inflammatory arthritis from Norway in 2010, Mjaavatten et al. [22], found that increasing levels of RF and ACPA were associated with persistent joint inflammation. Additionally, decreased level of seropositivity may be used for treatment success [23]. In this post-hoc analysis, more current smoker patients had high positive ACPA/RF than those never smoked, and the difference is statistically significant (P = 0.006). Leiden early arthritis clinic also found that levels of all isotypes of anti-CCP, except IgG3, were significantly higher (P < 0.05) in smokers [24]. Interestingly, Lee and colleagues [19] also found a significantly high level of seropositivity in RA patients with a history of smoking. This finding can mirror the pathogenic contribution of smoking to RA through citrullination of proteins; particularly in the context of the existence of genetic predisposition (the shared or rheumatoid epitope) that can reflect the importance of the level of seropositivity. Cigarette smoking can induce peptidyl arginine deiminase (PAD) expression in alveolar macrophages [25]. Enzymes then convert arginine to citrulline in the airway, thereby creating neoantigens that can be recognized by the adaptive immune system. Increased citrullination is not specific to RA and occurs with environmental stress. What is unique to RA is the propensity for immune reactivity to the neoepitopes created by protein citrullination with the production of anti-citrullinated protein antibodies (ACPAs). Citrullinated proteins were present in the bronchoalveolar lavage fluid from the lungs of cigarette smokers but were not demonstrated by immunostaining of fluid from nonsmokers [25, 26].
Smoking among carriers of the shared epitope was estimated to account for 36 percent of all RA that was associated with anticitrullinated peptide (ACPA). The Individuals who were homozygous for the shared epitope had an elevated risk of ACPA-positive RA but not ACPA-negative RA. The odds ratio (OR) for ACPA-positive RA was 17.8 (95% CI 11–29), and strong combined gene-environment effects were observed, with markedly increased risks of ACPA-positive RA among shared epitope homozygotes who were heavy smokers (OR 53, 95% CI 18–154), heavy coffee drinkers (OR 53, 95% CI 16–183), oral contraceptive users (OR 45, 95% CI 15–131) [27]. While obesity has been associated with the development of ACPA-negative RA (OR 3.5, 95% CI 1.7–6.9) [28]. The authors concluded that a distinction should be made between RA that is associated with and without ACPA because these subtypes are likely to represent disease entities with distinct etiologies. Moreover, the lack of an association between smoking and the risk of RA in those who are ACPA-negative suggests that these disease subsets (ACPA-positive versus ACPA-negative) differ in their pathogenesis [29]. Cigarette smoking may also be a risk factor for greater disease severity; patients with a 25 or more pack-year smoking history are more likely to be seropositive, have nodules, or have radiographically apparent erosions when compared with those who had never smoked [30]. In a large Swedish study, smokeless tobacco (e.g., moist snuff) did not increase the risk of chronic inflammatory diseases, suggesting that inhaled components of cigarette smoke other than nicotine may be more important than nicotine itself in etiology [31]. Also, a large collaborative study of Caucasian RA patients from North America confirmed a strong association between the presence of ACPA and the shared epitope; but found only a weak association between ACPA formation and smoking [32]. On the other hand, however, a moderately strong association between ACPA and tobacco exposure, irrespective of the presence of the shared epitope was demonstrated [24]. The most likely explanation for the propensity to form ACPAs in individuals with the shared epitope is the avid binding of the altered protein to the RA-associated MHC molecules. Interestingly, smoking cessation may help prevent the development of RA. This was suggested in a population-based study in the United States in which women who had stopped smoking more than ten years before entering the study did not share an increased risk of developing RA with their peers who were actively smoking [33].
A potential limitation of the current analysis might be the lack of separation of ACPA and RF as per COMORA dataset collection. Positive results of either (or both tests) are grouped. Despite that newer EULAR/ACR RA classification criteria had grouped and scored results of both or either tests similarly together [21], this post-hoc analysis would have provided distinct relationships between smoking on one hand and each of ACPA level and RF level of seropositivity, despite that the interaction between smoking and RF seropositivity had been also addressed. The disease risk of RF-positive RA associated with the classic genetic risk factors (e.g., the shared epitope) is strongly influenced by the presence of an environmental factor (smoking) in the population at risk [34]. Masdottir [15] confirmed a positive correlation between smoking and RF levels. Nevertheless, stratification of the results and studying ACPA and RF separately could have shown distinct results. Rasker and his colleagues [35] in their results showed an interaction between tobacco exposure and shared epitope for the presence of ACPA with OR for ACPA in patients having both tobacco exposure (TE) and shared epitope (SE) to be higher than the summed OR of patients having only tobacco exposure or shared epitope (OR: TE + /SE − , 1.07; TE − /SE + , 2.49; and TE + /SE + , 5.27; all relative to TE − /SE −). A similar effect was found for RF, but stratification showed that the interaction primarily associated with ACPA. Other studies found no discernable difference between RF titer and smoking [32]. Another important limitation of this analysis is the absence of data on the dose and the exact duration of smoking which could affect this association and may end up with dissimilar results.
A potential strength of this post-hoc analysis is the large sample size (> 3400), recruited from several countries from 5 continents of the globe with a different ethnic and genetic background which increases the external validity and the generalizability of the results. While earlier studies on the association of seropositivity and smoking were conducted in more restrictive world areas, COMORA data represented an opportunity to check if the previously reported association between smoking and seropositivity is pertinent to a particular geographic area or it exists in different parts of the world irrespective of the racial and ethnic background of the patients. The finding of a positive association between smoking and higher seropositivity level in 11 out of 17 countries, with variable OR reaching statistical significance in 4 different countries from Africa (Egypt), Asia (Taiwan), Europe (Italy) and North America (USA), supports the globalization of this association. Smoking in context to RA is a dynamic research field; given that smoking could be a modifiable risk factor, and that current smokers can have lower remission rate, altered treatment response [8], higher comorbidities (e.g., cardiovascular) and higher mortality rate [11]. Research addressing the effect of smoking cessation deems necessary. RA patients may consider smoking a calming mechanism to pain and may not be overly concerned with quitting smoking. Such research can have implications and give incentives to RA patients, particularly when proved that smoking cessation will make RA better.
References
Baka Z, Buzás E, Nagy G (2009) Rheumatoid arthritis and smoking: putting the pieces together. Arthritis Res Ther 11(4):238
Hammam N, Gheita TA (2017) Impact of secondhand smoking on disease activity in women with rheumatoid arthritis. Clin Rheumatol 36(11):2415–2420
Pedersen M, Jacobsen S, Klarlund M, Pedersen BV, Wiik A, Wohlfahrt J, Frisch M (2006) Environmental risk factors differ between rheumatoid arthritis with and without auto-antibodies against cyclic citrullinated peptides. Arthritis Res Ther 8(4):R133
Stolt P, Bengtsson C, Nordmark B, Lindblad S, Lundberg I, Klareskog L, Alfredsson L (2003) Quantification of the influence of cigarette smoking on rheumatoid arthritis: results from a population-based case-control study, using incident cases. Ann Rheum Dis 62(9):835–841
Kazantseva MG, Highton J, Stamp LK, Hessian PA (2012) Dendritic cells provide a potential link between smoking and inflammation in rheumatoid arthritis. Arthritis Res Ther 14(5):R208
Jónsson T, Thorsteinsson J, Valdimarsson H (1998) Does smoking stimulate rheumatoid factor production in non-rheumatic individuals? APMIS 106(10):970–974
Papadopoulos NG, Alamanos Y, Voulgari PV, Epagelis EK, Tsifetaki N, Drosos AA (2005) Does cigarette smoking influence disease expression, activity and severity in early rheumatoid arthritis patients? Clin Exp Rheumatol 23(6):861–866
Westhoff G, Rau R, Zink A (2008) Rheumatoid arthritis patients who smoke have a higher need for DMARDs and feel worse, but they do not have more joint damage than non-smokers of the same serological group. Rheumatology (Oxford) 47(6):849–854
Harrison BJ, Silman AJ, Wiles NJ, Scott DG, Symmons DP (2001) The association of cigarette smoking with disease outcome in patients with early inflammatory polyarthritis. Arthritis Rheum 44(2):323–330
Wolfe F (2000) The effect of smoking on clinical, laboratory, and radiographic status in rheumatoid arthritis. J Rheumatol 27(3):630–637
Joseph RM, Movahedi M, Dixon WG, Symmons DP (2016) Smoking-related mortality in patients with early rheumatoid arthritis: a retrospective cohort study using the clinical practice research datalink. Arthritis Care Res (Hoboken) 68(11):1598–1606
Lahiri M, Morgan C, Symmons DP, Bruce IN (2012) Modifiable risk factors for RA: prevention, better than cure? Rheumatology (Oxford) 51(3):499–512
Källberg H, Ding B, Padyukov L, Bengtsson C, Rönnelid J, Klareskog L, Alfredsson L; EIRA Study Group (2011) Smoking is a major preventable risk factor for rheumatoid arthritis: estimations of risks after various exposures to cigarette smoke. Ann Rheum Dis 70(3):508–511
Sugiyama D, Nishimura K, Tamaki K, Tsuji G, Nakazawa T, Morinobu A, Kumagai S (2010) Impact of smoking as a risk factor for developing rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis 69(1):70–81
Masdottir B, Jónsson T, Manfredsdottir V, Víkingsson A, Brekkan A, Valdimarsson H (2000) Smoking, rheumatoid factor isotypes and severity of rheumatoid arthritis. Rheumatology (Oxford) 39(11):1202–1205
Van Venrooij WJ, Pruijn GJ (2014) How citrullination invaded rheumatoid arthritis. Arthritis Res Ther 16(1):103
Lundberg K, Bengtsson C, Kharlamova N, Reed E, Jiang X, Kallberg H et al (2013) Genetic and environmental determinants for disease risk in subsets of rheumatoid arthritis is defined by the anticitrullinated protein/peptide antibody fine specificity profile. Ann Rheum Dis 72(5):652–658
Klareskog L, Stolt P, Lundberg K, Källberg H, Bengtsson C, Grunewald J et al (2006) A new model for an etiology of rheumatoid arthritis: smoking may trigger HLA-DR (shared epitope)-restricted immune reactions to autoantigens modified by citrullination. Arthritis Rheum 54(1):38–46
Lee DM, Phillips R, Hagan EM, Chibnik LB, Md CKH, Mph SPH (2009) Quantifying Anti-CCP titer: clinical utility and association with tobacco exposure in patients with rheumatoid arthritis. Ann Rheum Dis 68(2):201–208
Dougados M, Soubrier M, Antunez A, Balint P, Balsa A, Buch MH et al (2014) Prevalence of comorbidities in rheumatoid arthritis and evaluation of their monitoring: results of an international, cross-sectional study (COMORA). Ann Rheum Dis 73(1):62–68
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd et al (2010) Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62(9):2569–2581
Mjaavatten MD, van der Heijde D, Uhlig T, Haugen AJ, Nygaard H, Sidenvall G et al (2010) The likelihood of persistent arthritis increases with the level of anti-citrullinated peptide antibody and immunoglobulin M rheumatoid factor: a longitudinal study of 376 patients with very early undifferentiated arthritis. Arthritis Res Ther 12(3):R76
Chou C, Liao H, Chen Ch, Chen W, Wang H, Su K (2007) The clinical application of anti-CCP in rheumatoid arthritis and other rheumatic diseases. Biomark Insights 2:165–171
Verpoort KN, Papendrecht-van der Voort EA, van der Helm-van MAH, Jol-van der Zijde CM, van Tol MJ, Drijfhout JW et al (2007) Association of smoking with the constitution of the anti-cyclic citrullinated peptide response in the absence of HLA-DRB1 shared epitope alleles. Arthritis Rheum 56(9):2913–2918
Makrygiannakis D, Hermansson M, Ulfgren AK, Nicholas AP, Zendman AJ, Eklund A et al (2008) Smoking increases peptidylarginine deiminase 2 enzyme expression in human lungs and increases citrullination in BAL cells. Ann Rheum Dis 67(10):1488–1492
Damgaard D, Friberg Bruun Nielsen M, Quisgaard Gaunsbaek M, Palarasah Y, Svane-Knudsen V, Nielsen CH (2015) Smoking is associated with increased levels of extracellular peptidyl arginine deiminase 2 (PAD2) in the lungs. Clin Exp Rheumatol 33(3):405–408
Pedersen M, Jacobsen S, Garred P, Madsen HO, Klarlund M, Svejgaard A et al (2007) Strong combined gene-environment effects in anti-cyclic citrullinated peptide-positive rheumatoid arthritis: a nationwide case-control study in Denmark. Arthritis Rheum 56(5):1446–1453
Pedersen M, Jacobsen S, Klarlund M, Pedersen BV, Wiik A, Wohlfahrt J et al (2006) Environmental risk factors differ between rheumatoid arthritis with and without auto-antibodies against cyclic citrullinated peptides. Arthritis Res Ther 8(4):R133
Firestein GS, Schur PH, Romain PL (2019) Pathogenesis of rheumatoid arthritis. In Up To Date. Literature review current through
Saag KG, Cerhan JR, Kolluri S, Ohashi K, Hunninghake GW, Schwartz DA (1997) Cigarette smoking and rheumatoid arthritis severity. Ann Rheum Dis 56(8):463–469
Carlens C, Hergens MP, Grunewald J, Ekbom A, Eklund A, Höglund CO et al (2010) Smoking, use of moist snuff, and risk of chronic inflammatory diseases. Am J Respir Crit Care Med 181(11):1217–1222
Lee HS, Irigoyen P, Kern M, Lee A, Batliwalla F, Khalili H et al (2007) Interaction between smoking, the shared epitope, and anti-cyclic citrullinated peptide: a mixed picture in three large North American rheumatoid arthritis cohorts. Arthritis Rheum 56(6):1745–1753
Criswell LA, Merlino LA, Cerhan JR, Mikuls TR, Mudano AS, Burma M et al (2002) Cigarette smoking and the risk of rheumatoid arthritis among postmenopausal women: results from the Iowa Women’s Health Study. Am J Med 112(6):465–471
Padyukov L, Silva C, Stolt P, Alfredsson L, Klareskog L (2004) A gene-environment interaction between smoking and shared epitope genes in HLA-DR provides a high risk of seropositive rheumatoid arthritis. Arthritis Rheum 50(10):3085–3092
Linn-Rasker SP, van der Helm-van Mil AH, van Gaalen FA, Kloppenburg M, de Vries RR, le Cessie S et al (2006) Smoking is a risk factor for anti-CCP antibodies only in rheumatoid arthritis patients who carry HLA-DRB1 shared epitope alleles. Ann Rheum Dis 65(3):366–371
Acknowledgements
The authors thank all patients and investigators who participated in the COMORA study and all co-authors of the original COMORA manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Elzorkany, B., Mokbel, A., Gamal, S.M. et al. Does smoking affect level of seropositivity in RA? A post-HOC global and inter-country analysis of COMORA cohort. Rheumatol Int 41, 699–705 (2021). https://doi.org/10.1007/s00296-021-04791-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-021-04791-w