Abstract
Low back pain (LBP) is a major public health problem globally, resulting in a significant personal and societal burden. However, little is known about health-care utilisation for optimal management of LBP. The aim of this systematic review and meta-analysis was to determine the prevalence rate of health-care utilisation for LBP. The electronic databases MEDLINE, EMBASE via Ovid, CINAHL, and Scopus were searched for peer-reviewed articles published in English before March 2018. Meta-analysis was performed using Stata version 14 software. The reported summary statistics including the pooled prevalence rate of health-care utilisation were calculated using a random-effects model. Of 5801 identified records, 20 met the inclusion criteria and were reviewed. The prevalence rate of health-care utilisation for LBP varied regionally, the pooled prevalence rate was 67%, 95% confidence interval (CI) 50–84 in the USA, 47%, 95% CI 39–56 in the UK and 48%, 95% CI 33–63 in Europe. General practitioners, chiropractors and physical therapists were health-care providers commonly engaged in the management of LBP patients, while medication treatment, exercise, massage therapy and spinal manipulation were common prescriptions. A range of factors influencing the decision to seek and use health-care for LBP were also identified. Despite LBP being a common public health problem, a significant proportion of people with the pain fail to use health-care. It is apparent from this review that there is possibly skewed data, as the evidence to date is largely from developed countries. Therefore, it is warranted that future studies investigate the epidemiology of health-care utilisation for LBP in developing countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low back pain (LBP) is one of the major challenging public health problems globally [1, 2], resulting in a significant cause of negative social, psychological and economic consequences [3, 4]. Despite this LBP has been seen as a syndrome limited to developed countries until the past few decades, currently the literature [5,6,7] demonstrates that it is also a major public health problem in developing countries and that it is the leading cause of years lived with disability (YLDs) in every country in the world. When measured by disability-adjusted life years (DALYs), LBP is also one of the major contributors to the global burden of disease [8]. Evidence shows that individuals with LBP frequently present with comorbidities, such as psychological and somatoform disorders [9]. Furthermore, it has been argued that approximately 80% of individuals experience at least one episode of LBP during their lifetime [10]. The prevalence of LBP is estimated to be higher in older adults and increases after the age of 30 years [11]. Correspondingly, the population aged 60 years or over is projected to increase in the coming four decades [12]. Partly due to this philosophy, the global prevalence of LBP is suggested to increase significantly over the coming years [13], suggesting that there is a concomitant growing demand on health-care systems. Thus, evidence-based intervention planning is desirable to mitigate against the societal consequences of LBP. The investigation of the health-care needs of the population experiencing LBP and associated factors is important to plan appropriate intervention strategies [14]. In addition, having a clear understanding of the type of health-care preferred by LBP patients and the type of treatment most effective for management of the pain is imperative to integrate these choices in the provision of services [15]. In response to this, research interest in the area of health-care utilisation and factors influencing such behaviours has been increasing over the past three decades [14]. However, the reported results are divergent and often inconclusive, partly due to the variability of methods and the reference periods considered in estimating the prevalence of LBP and related prevalence rates of health-care utilisation. Due to this heterogeneity, the prevalence rate of health-care utilisation for LBP and type of health-care opted for by individuals with LBP remain unclear. This negates preventive strategies and management of LBP conditions. Therefore, it is essential to determine the prevalence rate of health-care utilisation for LBP.
Methods
This review was conducted following a protocol registered in PROSPERO [CRD42018086040]. The methods used in the review conformed to the established Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [16].
Inclusion criteria
This review was initially designed to focus on studies reporting health-care utilisation among people with non-specific LBP, which is the most prevalent form of LBP [11, 17]. However, the reviewed studies were observational studies with questionnaire-based data collection, indicating that none of the studies undertook diagnostic procedure to identify specific and non-specific LBP. Because of this, removing one of the inclusion criteria ‘the reported data were collected from people with non-specific LBP’, studies that met all of the following three criteria were included in the review: (1) studies reported the number of study participants with LBP and prevalence of health-care utilisation or if it is possible to determine number of people with LBP and prevalence of health-care utilisation from the reported data; (2) the study participants were 15 and above years old who reside in the general population; and (3) full text of the study was in English.
Exclusion criteria
Case reports, reviews, sex and/or age-specific studies, and studies addressing pregnant women and health-care-based patients were excluded.
Literature search strategy and sources
A computerised search of the electronic databases MEDLINE, EMBASE via Ovid, CINAHL, and Scopus was performed for peer-reviewed articles published in English before March 2018. The search engines Google and Google Scholar were also searched for grey literature. In addition, lists of references in the retrieved articles were searched. The search strategy was developed by GKB in consultation with SC and JOB. One expert librarian (LE) was consulted for guidance on how to undertake searching. The optimised search terms used were: “health-care use” OR “health-care seeking” OR “health service use” OR “health service seeking” OR “help seeking behaviour” OR “consultation” OR “health provider visit” AND “low back pain”.
Definitions
For the purpose of this review, health-care utilisation was defined as a consultation or a series of consultations of health-care provider(s) for LBP [18]. Similarly, LBP was defined as pain localised below the line of the 12th rib and above the inferior gluteal folds lasting more than 1 day [19].
Data extraction
The data were first extracted by one independent reviewer (GKB) using the Joanna Briggs Institute meta-analysis of statistics assessment and review instrument (JBI-MAStARI) data extraction tool [20]. The second reviewer (JOB) then repeated the procedure, and disagreements were resolved through discussion. The recorded information includes general characteristics of the study (name of authors, year of publication, country of the study, study design, study population, number of participants with LBP, data collection method, response rate, definition of LBP and related health-care utilisation). In addition, specific study information, such as prevalence of health-care utilisation, type of health-care professional consulted, type of treatment prescribed, and factors associated with health-care utilisation were extracted.
Assessment of risk of bias
The risk of bias in each included study was evaluated using a standard risk of bias tool [19]. Originally, the tool covers ten items that address four domains of bias and overall summary of risk of bias assessment. To best fit the tool to this review, adjustment was made by adding the definition of health-care utilisation for LBP (making 11 items). The first four items assess the external validity, selection and nonresponse bias domains of the study in particular. The next 5–11 items assess the internal validity of the study. Specifically, items 5–10 assess the measurement bias domain, and item 11 assesses the domain of bias related to the analysis. Each item 1–11 has a response option of either low or high risk of bias. However, the overall risk of bias of each study was rated as low, moderate or high risk of bias given the responses to the preceding 11 items. Studies scoring greater or equal to 9 low risk of bias out of 11 items were deemed low overall risk of bias, those scoring 6–8 were deemed of moderate overall risk of bias and those scoring less than 6 were deemed high overall risk of bias. The tool demonstrated high interrater agreement, overall agreement 91% and the Kappa statistic 0.82, 95% confidence interval (CI) 0.76–0.86 in assessing risk of bias [19].
Data synthesis
For each included study, health-care utilisation was determined as a prevalence rate and the 95% CI. Meta-analysis was performed using Stata version 14 software. The literature indicates that health-care utilisation data could vary between studies according to geographic location [21, 22], study population, reference period over which health-care utilisation was measured [23] and how the concept of health-care utilisation was defined [18]. For this reason, subgroup meta-analyses were performed based on these factors, and a random-effects model was used to pool the prevalence of health-care utilisation for LBP across studies. Heterogeneity among the studies was assessed using the I2 statistics, which reflects the percentage of variation not because of sampling error across studies [24]. Publication bias was graphically assessed using funnel plot and Egger’s test.
To identify factors associated with health-care utilisation for LBP, textual narrative analysis was performed following tabulation of the key significant factors of all studies. This method of analysis was chosen because of heterogeneity among studies in terms of variables categorisation and the reported summary measures of association among the covariates and health-care utilisation for LBP.
Results
Search results
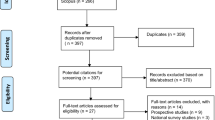
The electronic database and other sources search strategy identified 5801 potentially relevant records. After duplicates excluded, 4012 records remained to be eligible. Screening for title and abstract resulted in a further exclusion of 3901 records. The application of inclusion and exclusion criteria to the remaining 111 records deemed eligible for full text analysis led to the removal of 91 records. Thus, a total of 20 records met the inclusion criteria and were included in the review (Fig. 1).
Description of the included studies
The 20 included studies were reported from 11 countries. Specifically, while six studies [25,26,27,28,29,30] were conducted in the USA, three studies [31,32,33] were conducted in the UK. Of four other studies, two [34, 35] were carried out in the Netherlands and two [36, 37] in Greece. The remaining seven studies were carried out in Switzerland [38], Belgium [39], Ireland [40], Israel [41], Australia [42], Japan [43] and Turkey [44]. Almost all (n = 18) of the studies employed cross-sectional study design, while the two remaining studies used a prospective longitudinal follow-up study design (Table 1). The overall risk of bias was low in three studies [38, 42, 43] and high in two studies [33, 40]. Seven studies [26, 27, 33, 38, 39, 42, 44] included more than 1000 people with LBP, and the total number of people with LBP who participated in all studies were 19,086. All of the studies collected their data directly from the study participants as opposed to proxy. As demonstrated by the funnel plot symmetry (Fig. 2) and insignificant Egger test (p = 0.139), there was no evidence of small study bias and publication bias.
Health-care utilisation for LBP
All of the 20 reviewed studies reported the prevalence rate of health-care utilisation among people with LBP. The prevalence rate of health-care utilisation for LBP was found to vary among studies from 28% [38] to 92% [26]. Considering heterogeneity among studies, subgroup meta-analyses were performed based on a priori decisions, to disaggregate the effect of factors such as geographic region, study population, reference period and the way that health-care utilisation for LBP was conceptualised.
When health-care utilisation was disaggregated according to geographic region, the pooled prevalence rate of health-care utilisation was 67%, 95% CI 50–84 in the USA, 47%, 95% CI 39–56 in the UK and 48%, 95% CI 33–63 in Europe (Fig. 3). Alternatively, a subgroup meta-analysis referring to the study population demonstrated that the prevalence rate of health-care utilisation in the general population and workers was 56%, 95% CI 45–67 and 50%, 95% CI 26–75, respectively (Fig. 4).
The reference period over which the health-care utilisation was measured also varied across studies. Some studies measured health-care utilisation in the past 1 year, whilst others measured the history of health-care utilisation in the past 6 months, 4 months or 4 weeks prior to commencement of the study. The 1-month prevalence rate of health-care utilisation was 30%, 95% CI 28–33, while the annual prevalence was 51%, 95% CI 40–62 (Fig. 5).
Health-care utilisation for LBP was also conceptualised differently in different studies. Specifically, two studies [31, 33] limited the concept of health-care utilisation for LBP to consulting a general practitioner alone in contrast to the majority of the studies that defined the concept broadly as consulting any health-care provider for LBP. The highest prevalence (58%, 95% CI 45–72) was observed in those studies that measured health-care utilisation as seeking consultation from any health-care provider. When health-care utilisation was limited to seeking consultation from a general practitioner alone, the prevalence rate decreased to 51%, 95% CI 50–52 (Fig. 6).
Health-care provider commonly consulted, and treatment prescribed for the optimal management of LBP
Of the total reviewed articles, nine studies provided information on the type of health-care providers consulted for LBP condition [26, 27, 29, 30, 35, 38, 40,41,42]. Different categories of health-care providers were engaged in treating individuals with LBP. Consulting multiple health-care providers for the episode of LBP was also considerably noted. The type of health-care providers involved in the management of LBP patients varied among the studies. However, chiropractors in six studies [26, 27, 29, 30, 40, 42] and general practitioners in five studies [27, 35, 38, 40, 42] were reported. In addition, physical therapists and orthopaedic surgeons were noted in five studies [26, 29, 30, 35, 42] and three studies [29, 30, 41], respectively. It is noteworthy that in all the five studies [27, 35, 38, 40, 42], general practitioners were reported as health-care providers accounting for the highest number of consultations, and thus this group of health-care professionals play a significant role in the management of LBP patients. Regarding the common type of treatments prescribed, six studies [27, 29, 30, 41, 42, 44] provided the information, and all of them indicated medication treatment while exercise was noted in four studies [27, 29, 30, 42]. Massage therapy and spinal manipulation were both used in three studies [29, 30, 42], and bed rest in three studies [27, 30, 42] was also revealed as common prescriptions. In addition, transcutaneous electrical nerve stimulation (TENS), ultrasound [29, 30] and hot/cold packs [27, 30] were prescribed (Table 2).
Factors associated with health-care utilisation for LBP
A range of factors influencing health-care utilisation for LBP were reported by 13 studies. Eleven of these studies [26, 30,31,32, 34, 36,37,38,39, 42, 43] conducted logistic regression analyses and computed odds ratio (OR) with 95% CI to determine the statistical significance of the association between the covariates and health-care utilisation. The remaining two studies reported the association of different factors with health-care utilisation based on Chi square test [41] and p value [25]. In general, the identified factors can be categorised into socio-demographic factors, health behaviours and beliefs about the pain, pain and health-related factors as discussed below (Table S1).
Socio-demographic factors
Of the 13 studies that determined factors influencing health-care utilisation for LBP, 4 studies [26, 31, 38, 42] revealed statistically significant association between gender and health-care utilisation. Four of them consistently reported that females were more likely to utilise health-care for their LBP symptoms than males. However, this finding was not further observed in the other eight studies [25, 30, 32, 34, 36, 39, 41, 43] that reported statistically no significant association between gender and health-care utilisation. Further, the authors of one study [34] concluded that there was no association between the individual characteristics and health-care utilisation for LBP.
A positive association between increasing age and prevalence of health-care utilisation for LBP was observed in three studies [39, 41, 43]. Notably, in two of the studies [41, 43], being ≥ 60 years of age raised the history of reporting health-care utilisation for LBP. Further, in the other study [39], increasing age from 20 years showed a dose–response relationship with health-care utilisation to optimise the pain. Alternatively, the other nine studies [25, 26, 30,31,32, 34, 36,37,38] did not find a statistically significant association between age and health-care utilisation for LBP, while one of the studies [42] did not provide evidence in this regard.
The only two studies [42, 43] that presented the information about marital status of individuals and history of health-care utilisation for LBP reported different results. While one of the studies [42] presented an inverse association between being never married and health-care utilisation, the other study [43] showed no statistically significant association between marital status and health-care utilisation for LBP. Similarly, the findings reported on the influence of employment status and ethnic group on health-care utilisation for LBP lack consistency. While a higher prevalence rate of health-care utilisation for LBP was observed among unemployed or retired [32] and ‘black ethnic group’ [25] in the respective two studies, the other three studies [30, 38, 43] presented that the association between employment/working status and health-care utilisation was statistically not significant. No statistically significant association between race and health-care utilisation for LBP management was also seen in one study [30].
Surprisingly, those living in metropolitan cities were 21% less likely to utilise health-care compared to their counterparts in rural areas (AOR = 0.79, 95% CI 0.64–0.97) [39]. However, the finding of another study [25] showed that there was no statistically significant association between residential area and health-care utilisation. The evidence documented on educational status [25, 36, 38, 43] and income level [25, 38] as socioeconomic factors associated with health-care utilisation for LBP was also statistically not significant.
Health behaviours and beliefs about the pain
Under this category of factors influencing health-care utilisation for LBP, only few were studied. Specifically, being fearful that LBP could impair capacity to work [38, 42], having externalised locus of control for pain management [32] and having the belief that LBP would be a lifelong problem [39] were indicated to increase the odds of utilising health-care for the condition. Smoking status [43], drinking status [43] and body mass index (BMI) [36, 43] were identified as factors that have no association with history of health-care utilisation for LBP.
Pain-related factors
Higher pain score/higher intensity of pain [25, 32, 34, 38, 41, 43] and functional limitation [26, 38] were demonstrated as the most common factors increasing the prevalence rate of health-care utilisation for LBP. Similarly, five studies [30, 31, 34, 41, 42] ascertained that higher severity/disabling LBP was a significant factor leading people with LBP to utilise health-care. As opposed to this notion, only one study [26] reported that individuals with higher severity of LBP were 14% less likely to utilise health-care compared to their counterparts (AOR = 0.86, 95% CI 0.77–0.96). On episodes of pain, two studies [38, 42] provided the evidence that frequent LBP increases history of health-care utilisation. However, one study reported that individuals with greater number of LBP episodes were less likely to use health-care [25]. Alternatively, Côté et al. [26] documented that there was no statistically significant association between episodes of pain and health-care utilisation. The influence of history of back surgery [25] on health-care utilisation for the current LBP was not statistically significant.
Longer duration of the pain was also noted as a factor that has positive association with health-care utilisation [25, 32, 41]. In particular, the association between chronicity of LBP and health-care utilisation demonstrated a dose-dependent relationship [32, 36]. Thus, as the duration of pain increases from acute to chronic phase, the odds of utilising health-care to optimise the pain was noted to rise.
Health-related factors
Two studies [26, 37] presented a statistically significant association between general health status and health-care utilisation. The studies showed that being in a better health status reduces the history to report seeking health-care for LBP (AOR = 0.46, 95% CI 0.31–0.68) [26]; or moderate/bad perceived general health increases the likelihood to use health-care (AOR = 3.45, 95% CI 1.94–6.12) [37]. However, this concept was not further supported in three studies [30, 36, 38] reporting that there was no association between general/overall health status and health-care utilisation for LBP. The associations of factors such as comorbidity [43] and depression/anxiety [38, 43] with health-care utilisation for LBP management were also statistically not significant.
Discussion
An increasing amount of evidence has demonstrated that LBP is a considerable public health problem [11, 45,46,47] and that it has a significant impact on health-related quality of life [48,49,50]. The data on health-care utilisation for LBP is helpful to design appropriate intervention strategies. However, there is no comprehensive estimate of the prevalence rate of health-care utilisation among people with LBP. For this reason, this comprehensive systematic review and meta-analysis was undertaken to generate evidence that can be used for designing and implementing preventive strategies.
Utilisation of health-care for LBP requires appropriate medical diagnosis and management of the pain to reduce the subsequent social and economic burden. However, this review reflected that the prevalence rate of health-care utilisation for optimal management of LBP significantly varies between geographic regions. The highest prevalence rate was observed in the USA. This geographical variation in prevalence of health-care utilisation for LBP could be attributed to a number of factors. Firstly, the differences in health-care systems [51, 52] including health-care capacity, the approaches for reimbursing costs of health-care services and financial incentives contribute differently [21]. Secondly, the insurance system and the distribution of uninsured population across regions considerably influence the prevalence rate of health-care utilisation. The distribution of uninsured population is not homogeneous across regions and even within a region. However, evidence demonstrates that uninsured people have limited access to health-care needs in societies with high uninsured rates than do they in societies with comparatively low rates [53]. Thirdly, availability and accessibility of health-care services including skilled and experienced health-care providers, appropriate diagnostic testing and treatment could also largely explain the observed variation in prevalence rate of health-care utilisation for LBP. Finally, there is evidence arguing that individual factors such as age, level of education, income and the socioeconomic differences between geographic regions have different predictive power on explaining differences in prevalence of health-care utilisation [54, 55].
In this review, the overall prevalence rate of health-care utilisation in the general population and in the workers is comparable. However, the reported prevalence of health-care utilisation for worker groups largely varies in reference to whether the workers are entitled to claim workers’ compensation. The prevalence rate of health-care utilisation is considerably higher in workers entitled to claim workers’ compensation, which may be due to workers’ compensation health-care coverage. There is evidence demonstrating that after seeking the required health-care, workers entitled to claim workers’ compensation were significantly associated with greater overall adherence to health-care compared to workers who were not entitled to claim workers’ compensation [56]. This is because workers entitled to claim workers’ compensation are covered for health-care for work-related injuries including work-related LBP, and thus, the so-called cost-sharing methods used by the health insurers to limit health-care utilisation do not apply [26].
This review showed that general practitioners were the health-care providers that had a considerable involvement in the management of LBP patients, which is consistently reported within the literature [57, 58]. In addition, many individuals with LBP consulted and received treatment from a number of health-care providers, including physical therapists, chiropractors, massage therapists and orthopaedic surgeons. This finding is in accordance with the concept that the provision of health-care for individuals with LBP is characterised by the diversity of health-care providers offering a range of therapies [59] including pain medications or muscle relaxants, back exercise, bed rest, massage therapy and application of hot/cold packs. Such a multidisciplinary LBP management approach is argued to be linked with two main conditions [60]. First, LBP care is often fragmented [61]. Because of this, health-care professionals from different specialities are involved and often work independently, assess patients on the basis of their own experience and field of expertise, and design treatment plans accordingly. Second, LBP care is rarely provided in a consistent manner due to the differences in the clinical guidelines [60, 62]. Despite that several guidelines have been established by the involved disciplines, these guidelines have variations and are not accepted or followed universally [63]. Therefore, it is not surprising that patients may receive different recommendations and prescriptions based on the experience and field of the treating clinician.
This review demonstrated that the findings of most studies on factors associated with health-care utilisation for LBP are divergent, particularly with regard to social factors. The overall findings of this review support a previous study that concluded the inadequacy of evidence to support the common wisdom that socio-demographic characteristics of individuals impact on health-care utilisation for LBP management [14]. In those studies investigating social factors influencing health-care utilisation, few of them noted that being female and in an older age group significantly led to report a higher history of health-care utilisation for LBP. Freburger et al. [64] argued that the frequency of health-care utilisation for LBP could be a function of the prevalence of LBP condition. Consistent with this concept, there is an increasing amount of evidence [65,66,67,68] demonstrating that the prevalence of musculoskeletal pain including LBP is higher in females than males, which possibly raises the odds of health-care utilisation to optimise subsequent impact of the pain. There is also little evidence to argue that women are more enthusiastic to seek health-care for their problems than men [23, 69]. Alternatively, the finding that the older age groups use health-care more than younger people is not in concordance with previous evidence that describes older people as reluctant to seek health-care and to use treatment for their complaints [70], due to normalisation of their symptoms in relation to their age [71]. However, the authors of a study conducted in Norway documented that the use of health-care for musculoskeletal disorders (MSDs) is higher among older men and women [65].
The fear-avoidance model indicates that fear is an emotional reaction that leads towards an avoidance goal [72]. This may explain how individuals perceive, evaluate and respond to the conditions of LBP. A previous study also argued that health locus of control is associated with treatment benefit for LBP patients [73]. In this review, however, a limited number of studies provided information regarding the association between beliefs about LBP and health-care utilisation for the pain, suggesting the need for further investigation.
A higher intensity of pain and limitation in activities of daily living were determined as major pain related factors strongly associated with a higher frequency of health-care utilisation for LBP. Moreover, duration/chronicity of the pain that demonstrated a dose–response relationship with history of health-care utilisation is an important finding which calls for attention. Other than the direct health consequences, health-care costs attributed to chronic LBP management are also significantly high [9], and thus this finding shows a need for prompt intervention to prevent the transition of pain condition from the acute to the chronic phase. Unlike the case of social factors, the majority of the reviewed studies consistently showed that pain-related factors themselves are major factors associated with health-care utilisation for the optimal management of LBP. Therefore, it is worth noting that the overall evidence of this review is in concordance with the general view in the body of literature that pain-related factors are the main drivers of health-care utilisation to optimise the consequences of LBP [15, 74].
In another back pain study, depressive symptoms were found to be significantly associated with increased use of health-care providers, such as general and specialist physician services and physiotherapist services [75]. Similarly, the authors of a study in Japan concluded that depression was associated with higher frequency of health-care utilisation, higher degree of pain, poorer health-related quality of life and reduced labour productivity in chronic LBP patients [76]. However, the results of this systematic review do not support the presence of a statistically significant association among most of the health-related factors including comorbidity, anxiety, depression and health-care utilisation for LBP symptoms.
Strengths and limitations
The strengths of this systematic review and meta-analysis lie in its methods such as a comprehensive search of the electronic databases including search engines Google, Google Scholar and searching of lists of references in the retrieved articles. However, the estimates of factors associated with health-care utilisation for LBP were not pooled due to heterogeneity among studies in terms of variables categorisation and the reported summary measures of association among the covariates and health-care utilisation for LBP. In addition, due to the heterogeneity of the studies, the pooled prevalence rates of health-care utilisation for LBP need to be interpreted with caution.
Conclusions
Despite a growing body of evidence demonstrating that LBP is a common public health problem globally, a significant number of individuals with the condition fail to seek and use health-care for optimal management. The prevalence rate of health-care utilisation varies between geographic regions, study population, reference periods over which health-care utilisation was measured and definitions of health-care utilisation for LBP. The decision to seek and use health-care for LBP also depends upon an array of factors such as higher intensity of the pain, limitation in activities of daily living and chronicity of the pain. It is apparent from this review that there is possibly skewed data, as the evidence to date are largely from developed countries. Therefore, it is warranted that future studies investigate the epidemiology of health-care utilisation for low back pain in developing countries.
References
Buchbinder R, van Tulder M, Öberg B et al (2018) Low back pain: a call for action. Lancet 391(10137):2384–2388
Joergensen AC, Hestbaek L, Andersen PK, Andersen A-MN (2019) Epidemiology of spinal pain in children: a study within the Danish National Birth Cohort. Eur J Pediatr 178(5):695–706
Doualla M, Aminde J, Aminde LN et al (2019) Factors influencing disability in patients with chronic low back pain attending a tertiary hospital in sub-Saharan Africa. BMC Musculoskelet Disord 20(1):25
Bento TPF, dos Santos Genebra CV, Maciel NM et al (2019) Low back pain and some associated factors: is there any difference between genders? Braz J Phys Ther. https://doi.org/10.1016/j.bjpt.2019.01.012
Vos T, Flaxman AD, Naghavi M et al (2013) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2163–2196
Hartvigsen J, Hancock MJ, Kongsted A et al (2018) What low back pain is and why we need to pay attention. Lancet 391(10137):2356–2367
Hurwitz EL, Randhawa K, Yu H, Côté P, Haldeman S (2018) The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J 27(6):796–801
Murray CJ, Vos T, Lozano R et al (2012) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2197–2223
Gore M, Sadosky A, Stacey BR, Tai K-S, Leslie D (2012) The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine 37(11):E668–E677
Balagué F, Mannion AF, Pellisé F, Cedraschi C (2012) Non-specific low back pain. Lancet 379(9814):482–491
Hoy D, Brooks P, Blyth F, Buchbinder R (2010) The epidemiology of low back pain. Best Pract Res Clin Rheumatol 24(6):769–781
United Nations (2006) World population prospects: the 2006 revision. United Nations, New York
Hoy D, March L, Brooks P et al (2014) The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 73(6):968–974
Adamson J, Hunt K, Nazareth I (2011) The influence of socio-demographic characteristics on consultation for back pain—a review of the literature. Fam Pract 28(2):163–171
Woodhouse A, Pape K, Romundstad PR, Vasseljen O (2016) Health care contact following a new incident neck or low back pain episode in the general population; the HUNT study. BMC Health Serv Res 16:81
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Maher C, Underwood M, Buchbinder R (2017) Non-specific low back pain. Lancet 389(10070):736–747
de Vet HC, Heymans MW, Dunn KM et al (2002) Episodes of low back pain: a proposal for uniform definitions to be used in research. Spine 27(21):2409–2416
Hoy D, Brooks P, Woolf A et al (2012) Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 65(9):934–939
The Joanna Briggs Institute (2014) Joanna Briggs Institute Reviewers’ manual, 2014th edn. Australia The Joanna Briggs Institute, Adelaide
Buchan HA, Duggan A, Hargreaves J, Scott IA, Slawomirski L (2016) Health care variation: time to act. Med J Aust 205(S10):S30–S33
Traeger AC, Buchbinder R, Elshaug AG, Croft PR, Maher CG (2019) Care for low back pain: can health systems deliver? Bull World Health Organ 97(6):423–433
Kent PM, Keating JL (2005) The epidemiology of low back pain in primary care. Chiropract Osteopat 13(1):13
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J (2006) Assessing heterogeneity in meta-analysis: q statistic or I2 index? Psychol Methods 11(2):193–206
Carey TS, Evans AT, Hadler NM et al (1996) Acute severe low back pain: a population-based study of prevalence and care-seeking. Spine 21(3):339–344
Côté P, Baldwin ML, Johnson WG (2005) Early patterns of care for occupational back pain. Spine 30(5):581–587
Deyo RA, Tsui-Wu Y-J (1987) Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine 12(3):264–268
Merlino LA, Rosecrance JC, Anton D, Cook TM (2003) Symptoms of musculoskeletal disorders among apprentice construction workers. Appl Occup Environ Hyg 18(1):57–64
Carey T, Freburger JK, Holmes GM et al (2009) A long way to go: practice patterns and evidence in chronic low back pain care. Spine 34(7):718
Carey T, Evans A, Hadler N et al (1995) Care-seeking among individuals with chronic low back pain. Spine 20(3):312–317
Walsh K, Cruddas M, Coggon D (1992) Low back pain in eight areas of Britain. J Epidemiol Community Health 46(3):227–230
Waxman R, Tennant A, Helliwell P (1998) Community survey of factors associated with consultation for low back pain. BMJ 317(7172):1564–1567
Macfarlane GJ, Beasley M, Jones EA et al (2012) The prevalence and management of low back pain across adulthood: results from a population-based cross-sectional study (the MUSICIAN study). Pain (03043959) 153(1):27–32
Ijzelenberg W, Burdorf A (2004) Impact of musculoskeletal co-morbidity of neck and upper extremities on healthcare utilisation and sickness absence for low back pain. Occup Environ Med 61(10):806–810
Ijzelenberg W, Burdorf A (2004) Patterns of care for low back pain in a working population. Spine 29(12):1362–1368
Alexopoulos EC, Tanagra D, Konstantinou E, Burdorf A (2006) Musculoskeletal disorders in shipyard industry: prevalence, health care use, and absenteeism. BMC Musculoskelet Disord 7(1):88
Alexopoulos EC, Tanagra D, Detorakis I et al (2011) Knee and low back complaints in professional hospital nurses: occurrence, chronicity, care seeking and absenteeism. Work 38(4):329–335
Mannion AF, Wieser S, Elfering A (2013) Association between beliefs and care-seeking behavior for low back pain. Spine 38(12):1016–1025
Szpalski M, Nordin M, Skovron M, Melot C, Cukier D (1995) Health care utilization for low back pain in Belgium: influence of sociocultural factors and health beliefs. Spine 20(4):431–442
O’Sullivan D, Cunningham C, Blake C (2009) Low back pain among Irish farmers. Occup Med 59(1):59–61
Jacob T, Zeev A, Epstein L (2003) Low back pain—a community-based study of care-seeking and therapeutic effectiveness. Disabil Rehabil 25(2):67–76
Walker BF, Muller R, Grant WD (2004) Low back pain in Australian adults: health provider utilization and care seeking. J Manip Physiol Ther 27(5):327–335
Ono R, Yamazaki S, Takegami M et al (2015) Patient-reported disability in the general Japanese population was associated with medical care visits for low back pain, regardless of pain intensity. J Orthop Sci 20(4):742–749
Karahan A, Kav S, Abbasoglu A, Dogan N (2009) Low back pain: prevalence and associated risk factors among hospital staff. J Adv Nurs 65(3):516–524
Paul NS, Vicki KL, Pierre C, Linda CJ, David CJ (2015) Is low back pain associated with worse health-related quality of life 6 months later? Eur Spine J 24(3):458–466
Strudwick K, McPhee M, Bell A, Martin-Khan M, Russell T (2018) Best practice management of low back pain in the emergency department (part 1 of the musculoskeletal injuries rapid review series). Emerg Med Australas 30(1):18–35
Geurts JW, Willems PC, Kallewaard J-W, van Kleef M, Dirksen C (2018) The impact of chronic discogenic low back pain: costs and patients’ burden. Pain Res Manag. https://doi.org/10.1155/2018/4696180
Sadosky AB, DiBonaventura M, Cappelleri JC, Ebata N, Fujii K (2015) The association between lower back pain and health status, work productivity, and health care resource use in Japan. J Pain Res 8:119–130
Misiak B, Snarska KK (2014) Quality of life of patients with back pain. J Neurol Neurosurg Nurs 3(3):97–144
Sezgin M, Hasanefendioğlu EZ, Sungur MA et al (2015) Sleep quality in patients with chronic low back pain: a cross-sectional study assessing its relations with pain, functional status and quality of life. J Back Musculoskelet Rehabil 28(3):433–441
Zamanzadeh V, Ahmadi F, Foolady M, Behshid M, Irajpoor A (2017) The health seeking behaviors and perceptions of iranian patient with osteoarthritis about pain management: a qualitative study. J Caring Sci 6(1):81–93
Mikkelsson M (2012) Do we know enough about the health care use of adolescents with low back pain? Eur J Pain 16(10):1343–1344
Pagán JA, Pauly MV (2006) Community-level uninsurance and the unmet medical needs of insured and uninsured adults. Health Serv Res 41(3p1):788–803
Brezzi M, Luongo P (2016) Regional disparities in access to health care: a multilevel analysis in selected OECD countries. OECD regional development working papers 2016/04, Paris
Zhu D, Guo N, Wang J, Nicholas S, Chen L (2017) Socioeconomic inequalities of outpatient and inpatient service utilization in China: personal and regional perspectives. Int J Equity Health 16(1):210
Bier JD, Kamper SJ, Verhagen AP, Maher CG, Williams CM (2017) Patient nonadherence to guideline-recommended care in acute low back pain. Arch Phys Med Rehabil 98(12):2416–2421
Plénet A, Gourmelen J, Chastang J-F et al (2010) Seeking care for lower back pain in the French population aged from 30 to 69: the results of the 2002–2003 Decennale Sante survey. Ann Phys Rehabil Med 53(4):224–238
Picavet HSJ, Struijs JN, Westert GP (2008) Utilization of health resources due to low back pain: survey and registered data compared. Spine 33(4):436–444
Becker A, Held H, Redaelli M et al (2010) Low back pain in primary care: costs of care and prediction of future health care utilization. Spine 35(18):1714–1720
Namiranian K, Norris EJ, Jolissaint JG, Patel JB, Lombardi CM (2018) Impact of multidisciplinary spine conferences on surgical planning and perioperative care in elective lumbar spine surgeries. Asian Spine J 12(5):854–861
Harris SA, Rampersaud YR (2016) The importance of identifying and modifying unemployment predictor variables in the evolution of a novel model of care for low back pain in the general population. Spine J 16(1):16–22
Kirby ER, Broom AF, Adams J, Sibbritt DW, Refshauge KM (2014) A qualitative study of influences on older women’s practitioner choices for back pain care. BMC Health Serv Res 14(1):131
Koes BW, van Tulder M, Lin C-WC et al (2010) An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 19(12):2075–2094
Freburger JK, Holmes GM, Agans RP et al (2009) The rising prevalence of chronic low back pain. Arch Intern Med 169(3):251–258
Kinge JM, Knudsen AK, Skirbekk V, Vollset SE (2015) Musculoskeletal disorders in Norway: prevalence of chronicity and use of primary and specialist health care services. BMC Musculoskelet Disord 16(1):75
Noll M, de Avelar IS, Lehnen GC, Vieira MF (2016) Back pain prevalence and its associated factors in Brazilian athletes from public high schools: a cross-sectional study. PLoS One 11(3):e0150542
Meucci RD, Fassa AG, Faria NMX (2015) Prevalence of chronic low back pain: systematic review. Rev Saude Publica 49:73
Yang H, Haldeman S, Lu M-L, Baker D (2016) Low back pain prevalence and related workplace psychosocial risk factors: a study using data from the 2010 National Health Interview Survey. J Manipul Physiol Ther 39(7):459–472
Garg A, Kapellusch JM, Hegmann KT et al (2014) The NIOSH lifting equation and low-back pain, part 2: association with seeking care in the Backworks prospective cohort study. Hum Factors 56(1):44–57
Sanders C, Donovan J, Dieppe P (2004) Unmet need for joint replacement: a qualitative investigation of barriers to treatment among individuals with severe pain and disability of the hip and knee. Rheumatology 43(3):353–357
Walters K, Iliffe S, Orrell M (2001) An exploration of help-seeking behaviour in older people with unmet needs. Fam Pract 18(3):277–282
Vlaeyen JW, Linton SJ (2000) Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 85(3):317–332
Keedy NH, Keffala VJ, Altmaier EM, Chen JJ (2014) Health locus of control and self-efficacy predict back pain rehabilitation outcomes. Iowa Orthop J 34:158–165
Vasseljen O, Woodhouse A, Bjørngaard JH, Leivseth L (2013) Natural course of acute neck and low back pain in the general population: the HUNT study. Pain 154(8):1237–1244
Lim K-L, Jacobs P, Klarenbach S (2006) A population-based analysis of healthcare utilization of persons with back disorders: results from the Canadian Community Health Survey 2000–2001. Spine 31(2):212–218
Tsuji T, Matsudaira K, Sato H, Vietri J (2016) The impact of depression among chronic low back pain patients in Japan. BMC Musculoskelet Disord 17(1):447
Funding
This study did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the formation of the research question. GKB conducted the search. GKB and JO’B extracted the data and SC revised the data. All authors contributed to the preparation and review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interests to declare.
Ethical approval
Because this study was a systematic review and meta-analysis, ethical approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Beyera, G.K., O’Brien, J. & Campbell, S. Health-care utilisation for low back pain: a systematic review and meta-analysis of population-based observational studies. Rheumatol Int 39, 1663–1679 (2019). https://doi.org/10.1007/s00296-019-04430-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-019-04430-5