Abstract
To describe the clinical and therapeutic management of rheumatoid arthritis (RA) patients with biological disease-modifying antirheumatic drugs (bDMARDs), alone or in combination with conventional synthetic DMARDs (csDMARDs), as well as analysing changes over time in bDMARD use. An observational, retrospective, multicentre study was conducted in the rheumatology departments of 10 public Spanish hospitals. Patients with RA treated with bDMARDs at baseline who had medical records available in the data collection period 2013–2016 were included. All visits to rheumatology departments recording any type of bDMARD modification (dose, etc.) were collected. Clinical characteristics, concomitant treatment, resource use, work productivity and quality of life (QoL) were recorded. 128 patients were included: 81 received first-line bDMARD treatment, 28 second-line bDMARD treatment and 19 received third or later lines. Mean study follow-up was 4.1 years. Assessment of DAS28 was available in 54.6% of visits. At baseline, 48.7% of patients had moderate–high disease activity. At final observation, 69.5% of patients continued with the first bDMARD. Tumour necrosis factor blockers were administered to 85.2% of patients in first line, 45.7% in second line and 18.1% in third or later lines. At final observation, 80.2% of patients still felt pain/discomfort. As expected, those with higher disease activity had higher loss of work productivity and lower QoL, as assessed by DAS28, than patients with lower disease activity. Drugs represented 82.6% of the total cost. In this Spanish cohort of 128 patients, most patients remained on the first prescribed bDMARD, despite remaining signs and symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is the most common immune-mediated inflammatory joint disorder and is characterized by joint inflammation, pain and damage, reducing patients’ functionality and quality of life (QoL) and increasing morbidity and mortality [1,2,3]. The prevalence in Spain among the adult population is estimated to be 0.5% [4], and it is higher in women, with an incidence of around 8.4 cases/100,000 inhabitants [5]. RA is a great economic burden (both direct and indirect costs) for society and the Spanish national health system (NHS) [6,7,8]. Better treatment regimens would increase patients’ QoL and may save resources and costs for the NHS [7, 9].
There are multiple therapeutic options for RA, predominantly targeting moderate–severe RA. The development of tumour necrosis factor (TNF) blockers has improved the treatment and prognosis of RA patients, reducing loss of joint function and pain [10, 11]. Monotherapy of biological disease-modifying antirheumatic drugs (bDMARDs) and their combination with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) can lead to clinical remission and delay or completely stop clinical and radiological progression of the disease, thereby improving patients’ QoL [12].
Clinical practice guidelines recommend starting RA treatment with a DMARD, usually methotrexate, in monotherapy or combined with other csDMARDs [13,14,15]. In 2002, the retrospective emAR study analysed the therapeutic management of RA patients, confirming significant variability in patients’ pharmacological treatment, as well as in other parameters such as consumption of social and health resources [16]. 10 years later, the emAR II study [17] updated these data to include treatment with bDMARDs, which was not evaluated in the first study. In emAR II, the variability in resource use (use of some resources decreased, while others increased) and in treatment patterns was still evident. The emAR II study found an increase in the use of csDMARDs and a significant decrease in time between the onset of symptoms and start of the first disease-modifying antirheumatic drug (DMARD). Regarding treatment with bDMARDs, a significant tendency to decrease their use as the patient’s age increased was detected, while longer time to disease progression, the presence of extra-articular manifestations and high RA activity (disease activity score (DAS) > 5.1) were associated with a higher probability of receiving bDMARDs [17].
The development and increasing availability of bDMARDs have changed the treatment of patients with rheumatic diseases, so it is important to gather updated data on changes in treatment and the impact of these new therapies on resource consumption. Since recent data on the clinical and therapeutic management of RA patients in routine clinical practice in Spain are scarce, the aim of this study was to describe the clinical and therapeutic management of RA patients with bDMARDs. This included therapeutic management with bDMARDs, alone or combined with csDMARDs, as well as analysing changes over time in these patterns. Resources associated with the management of moderate–severe RA patients were also recorded.
Materials and methods
Study design and patient population
Between December 2016 and July 2017, an observational, retrospective, multicentre study was conducted in the rheumatology departments of 10 regional public Spanish hospitals. The following were considered inclusion criteria: adult patients (≥ 18 years) with moderate–severe RA at diagnosis (according to the criteria of the American College of Rheumatology [ACR] of 1987 or ACR/European League Against Rheumatism [EULAR] classification of 2010 [18, 19]) treated with bDMARDs in 2013 and with computerized medical records. Investigators included consecutive patients who attend clinics and meet the study selection criteria previously described.
Only patients with retrospective data available through 2013 until 2016 were included. Patients were asked to consent to inclusion of their data in this retrospective chart review regardless of their current status or changes in treatment over recent years. Patients treated with DMARDs for an indication other than RA or those participating in any clinical trial during the study period were excluded.
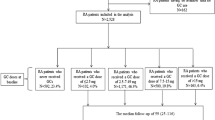
Data were retrospectively collected from visits to rheumatology departments from 2013 to the final observation date, including bDMARD treatment (dose, frequency, etc.) (observational period). Patients were categorised according to the bDMARD treatment line that they were receiving at baseline in 2013 (Fig. 1). In addition, patients completed the study questionnaires at final observation.
The study protocol was approved by the Ethics Committee of Hospital Parc Taulí, Sabadell, and classified by the Spanish Agency of Medicines and Medical Devices (AEMPS) as a non-prospective post-authorisation study (EPA-OD). The study was conducted in accordance with the principles of the Declaration of Helsinki of 1975/83.
Data collection
Patient information was retrieved from the patients’ clinical records and directly from patients through completed questionnaires. Demographic profiles and clinical characteristics were collected, including RA diagnosis and onset of symptom dates as well as first csDMARDs and bDMARDs treatment dates. If available, disease characteristics included the date and reason of every visit, 28 tender joint count (TJC), 28 swollen joint count (SJC), DAS28 (ESR and/or CRP), presence of morning stiffness, pain and disease assessment by the patient and clinician (visual analog scale, VAS), functional capacity measured by the health assessment questionnaire disability index (HAQ-DI) [20] and laboratory tests (rheumatoid factor and anti-citrullinated protein antibody [anti-CCP], acute-phase reactants [erythrocyte sedimentation rate, ESR, and C-reactive protein, CRP]). EuroQoL 5 dimensions 5 levels (EQ-5D-5L) [21] and work productivity and activity impairment questionnaire: general health (WPAI-GH) [22] questionnaires were also required.
Lines of bDMARD treatment at baseline (2013) were collected, taking into account the number of bDMARD treatments used for every patient before baseline. All changes in treatment with bDMARDs during the observational period were recorded. A change in bDMARD was defined as any dose increase/decrease, administration schedule modification and interruption/end or change to another bDMARD. The reasons for medication change at each observation, including dose and route of administration, were collected. Predefined lists for each treatment group were presented (non-steroidal anti-inflammatory drugs [NSAIDs], corticosteroids, csDMARDs or bDMARDs, or other).
The resources used since the last recorded visit were collected at each study visit. If available, direct resources included the number of visits to each department, hospitalisations related to RA, day hospital admissions, tests performed (blood, urine, imaging, etc.) and number of tests, purified protein derivative (PPD) test, vaccinations and the need for paid support from non-family members not financed by the NHS during the last year of observation. Given that data on domestic support are not likely to be recorded in the medical records, at final observation the patient was asked about her/his need for support from non-family members at the patient’s or relatives’ expense or funded by the NHS during the last year to date. As data pertaining to indirect resources were also not likely to be recorded in the medical records, the patient was asked at the final observation about loss of work productivity due to temporary disability in the last year (change of type of work or position and number of days on sick leave due to RA, or how RA affects work activity measured by the VAS score). Indirect costs were calculated according to the time of work absenteeism, the loss of labor productivity and applying the average interprofessional salary to them.
Study size and statistical analysis
The sample size should be sufficient to describe the therapeutic management of patients with RA. Due to the variability of the therapeutic changes and the absence of available data in the same population and in the same period of time, the sample size assumed that 50% of subjects would change treatment, which maximised the size of the sample needed. The target sample size was 151 patients, considering a precision of 0.08 and a significance level of 0.05.
Statistical analyses were performed using SAS version 9.2. For describing continuous variables, the mean, standard deviation, median, minimum and maximum were used and, depending on the distribution of the variable analysed quartiles would be also presented. For describing categorical variables, the number and percentage of patients per response category were used.
Statistical analysis of sociodemographic and clinical characteristics was performed in evaluable patients stratified in three treatment groups according to the treatment at baseline (2013); first, second or third or later lines of bDMARD treatment. The proportion of patients requiring a change of treatment, the reason for change and the mean time between consecutive bDMARD modifications were analysed. Clinical characteristics at the change of treatment visit were evaluated. A descriptive analysis of the biological treatment according to line, including bDMARD treatments prior to the study period, was performed.
The ANOVA test and Pearson’s correlation were used to evaluate the relationship between HAQ-DI, EQ-VAS and loss of productivity. The results were considered statistically significant at p < 0.05.
The cost data were obtained from national data sources [23, 24]. Historical costs were projected forwards to 2016 using the consumer price index published by the Spanish National Institute of Statistics (INE) [25]. Direct resources were not collected at final observation. Therefore, as data from previous follow-up observation to final observation were not recorded, to obtain the annual cost per patient, the total cost during patient follow-up was divided by the number of years between the previous follow-up observation and baseline (2013).
There was no imputation of data; only available data were analysed. In all descriptive analyses the number and percentage of missing values for each variable were recorded.
Results
A total of 128 patients were included in the study between December 2016 and July 2017. Demographic data and clinical characteristics stratified according to the line of treatment at baseline are given in Table 1. The mean age (standard deviation, SD) was 54.7 (10.7) years and mean disease duration was 13.2 (8.3) years. The mean time between diagnosis and the first csDMARD was 1.1 (2.9) years and the mean time between diagnosis and the first bDMARD was 8.0 (7.5) years. The elapsed time between the first csDMARD and the first bDMARD was 6.8 (7.7) years. The mean time on a bDMARD at baseline was 3.5 (3.2) years.
At baseline, 81 patients (63.3%) were receiving first-line bDMARD treatment, 28 (21.9%) second-line bDMARD treatment and 19 (14.8%) were receiving third or later lines bDMARD treatment. Table 2 shows the different bDMARDs at baseline, as well as whether they were administered alone or in combination with csDMARDs. At baseline, anti-TNF use was 85.2% in first line, decreasing to 45.7% in second line and to 18.1% in third or later lines (Fig. 2).
At final observation, a DAS28 score was available in 60.9% of patients. However, the TJC was available in 91.4% of cases and the SJC in 93.0%. Furthermore, the acute-phase reactants ESR and CRP were available in 85.9% and 86.7% of the patients, respectively.
At baseline, 33.3% of patients were in DAS28 remission (< 2.6); 17.9% had low disease activity (2.6–3.2); 37.2% moderate disease activity (3.2–5.1); and 11.5% high disease activity (> 5.1). Table 1 shows disease activity according to the line of treatment.
The mean observation time was 4.1 years. A total of 196 changes in bDMARDs (dose, etc.) were recorded during follow-up (median time between changes of 10.3 months) in 99 patients (77.3%). The most common bDMARD changes reported during follow-up were dose adjustments: 39.8% of all dose adjustments (35.7% changes in dosing interval and 4.1% changes in dose) were dose reductions (87.2% due to clinical remission) and 21.4% (17.9% changes in dosing interval and 3.6% changes in dose) were dose increases (57.1% due to a lack of response). 14 changes (7.1%) were interruption of the bDMARD treatment (42.9% due to adverse event) and 6 changes (3.1%) were discontinuation/end of the treatment (33.3% due to clinical remission). At the end of the observational period, 69.5% of patients were still receiving the same bDMARD as at baseline. In total, 30.5% of patients changed their bDMARD (76.7% due to a lack of response). By the time of the change, 85.7% of patients showed moderate to high disease activity according to DAS28 (although DAS28 was only available in 54.6% of the patients at the visits in which the bDMARD was changed). The mean joint count at this visit was 6.8 (6.2) TJC and 3.6 (3.2) SJC (Table 3).
Mean duration of treatment with the same bDMARD, only including treatments that ended during the observation period, was 5.5 years in first line, 2.8 in second line and 2.2 in third or later lines.
At the last observation, the percentage of patients who reported affected dimensions of the EQ-5D-5L descriptive system was 80.2% for pain/discomfort, 63.2% for usual activities, 55.6% for mobility, 50% for anxiety/depression and 40% for self-care dimensions. HAQ-DI scores for patients in first-line bDMARD treatment at baseline were lower than for patients in later lines, with a mean (SD) HAQ-DI score of 0.82 (0.69) for first-line patients, 0.99 (0.76) for second-line and 1.31 (0.55) for third or later lines. 34.7% of patients who did not change bDMARD had a HAQ-DI score of > 1 at baseline.
In the year prior to the final observation, 17.8% of employed patients took sick leave, with a mean of 146 sick leave days per year. Loss of productivity according to the WPAI-GH questionnaire was 30.6%, associated with an increase in HAQ-DI (r = 0.761, p = 0.003).
On average, patients had four ESR tests, four haematology and four clinical chemistry tests, as well as three rheumatology visits per year. In total, 28.9% of patients had a day admission for treatment administration and five patients (3.9%) were hospitalised due to RA. The total mean annual cost per patient was €16,549 (median €13,692), of which 94.9% (€15,709) were direct costs and 5.1% (€840) were indirect costs. The total annual cost was higher in patients treated with bDMARDs in second and third or later lines at baseline. The mean annual cost of RA medication in our study was €13,676 per patient (82.6% of the RA total cost) (Table 4).
Discussion
This study describes for the first time the clinical and therapeutic management of RA treated with bDMARDs during a retrospective period of about 4 years, based on data from 10 hospitals in Spain.
In the emAR II study, bDMARDs were used in combination with csDMARDs in 80.3% of subjects [17], while in this study only 70.3% of patients received a bDMARD and a csDMARD in combination (the most widely used csDMARDs were methotrexate [52.3%] and leflunomide [13.3%]). The observed difference in the percentage of patients treated with bDMARDs in monotherapy could be explained by the marketing of a new bDMARD indicated for monotherapy (tocilizumab) between both studies.
At baseline, the mean time between diagnosis and the first bDMARD was 8.0 (7.5) years. Compared to the emAR study, the time elapsed until our patients received their first csDMARD and their first bDMARD was longer [16]. In the emAR II study, the median time from diagnosis to administration of csDMARDs was 0 months (interquartile range of 0–2.9) [17]. However, it should be noted that in the emAR II study, 15% of patients started csDMARDs before diagnosis, 44% at the time of diagnosis and 48% after diagnosis [17].
ACR/EULAR treatment guidelines [15, 26] recommend that after the failure of first-line csDMARDs, other csDMARDs can be used in sequential or combination therapy, or combined with a bDMARD depending on patient characteristics and the presence of poor prognosis factors [13, 15]. The results of our study are aligned with these recommendations.
Most of the patients (85.2%) started treatment with an anti-TNF in first-line bDMARD therapy. The most widely used were those that have been on the market for longer and combination therapy was the most prescribed option. These findings are consistent with the treatment recommendations, which do not specify which is the best therapeutic option after the first bDMARD failure. Spanish clinical practice guidelines for RA management (GUIPCAR) indicate that after an inadequate response to csDMARDs, a personalised decision should be made according to individual patient characteristics and their medical histories and preferences [26, 27].
Although changing a bDMARD is indicated in various situations (failure to achieve the therapeutic objective, adverse events, etc.) [28], at the end of the follow-up period only a small percentage of patients changed baseline bDMARD (30.5%), despite 48.7% of patients reporting moderate to high disease activity. Missing data in medical records, especially DAS28 information (39.1% missing), could indicate that a “treat to target” strategy is not followed routinely and insufficiently treated [13, 15, 29, 30], leading to worse long-term outcomes.
Navarro Sarabia et al. [31] observed that there was a correlation between the functional capacity of the patient, the patients’ health-related QoL, loss of productivity and the cost of the disease. This study found that more than half of RA patients (63.2%) had difficulties performing activities of daily living according to EQ-5D-5L and there was a 30.6% loss of productivity according to the WPAI-GH questionnaire. This higher loss of productivity was associated with a decrease in physical function as assessed by the HAQ-DI.
RA is associated with high variability in the use of medical and non-medical resources regarding the disease and work disability. Ruiz-Montesinos et al. identified that direct costs were substantially higher than indirect costs (74% versus 26%), with drugs accounting for the main component of medical costs (56%) [7, 9]. This study also found direct costs to be higher than indirect costs (94.9% versus 5.1%), although indirect costs are lower than those identified by Ruiz-Montesinos et al., probably due to the low percentage of working patients (36.0%). In our study, the highest cost was associated with pharmacological treatment (82.6%), followed by loss of productivity (5.1%), and the average cost of RA increased from the first line of treatment.
Our study presents several limitations that are worth noting. The first limitation is the sample size (n = 128), which is less than the planned sample size (n = 151). While the planned sample size was calculated with a precision of 0.08, the final number of patients evaluated in the study had a precision of 0.087, with a difference between them of 0.7%, which is estimated not to influence in the results. Another limitation is the use of retrospective data for patients who initiated DMARDs 4 years previously. The retrospective nature prohibited the inclusion of more information, incorporating only the data collected by clinicians during the study period. At the beginning of the study, a feasibility study of the hospitals was performed to ensure that the necessary information was available. However, while the study included DAS28-ESR data for all patients, only eight of them were evaluated by DAS28-CRP. A second limitation is that the use of resources could be underestimated because in those patients whose treatment did not change (including at the final observation), use of resources was not recorded. Finally, as concomitant treatments were not collected between visits, it was assumed that the same patient received the same concomitant treatment until the next treatment change visit, suggesting a limitation in the calculation of costs. However, considering the high costs of bDMARDs, it is estimated that this assumption has a small impact on final costs.
In conclusion, this observational study has shown that most RA patients continued treatment with the first prescribed bDMARD, despite not achieving low disease activity or remission. Dose adjustments were required in a high percentage of patients for several reasons, mainly related to lack of response. Only a small percentage of patients changed bDMARD, primarily due to lack of efficacy. In this study, patient follow-up was hampered by a lack of recorded RA activity index data (DAS28). These real-world data could be of interest to understand and improve the management of RA patients and the importance of conducting more studies on this subject.
References
Fauci AS, Langford CA, Langford C (2013) Harrison’s rheumatology. McGraw-Hill Publishing, New York
O’Dell JR (2004) Therapeutic strategies for rheumatoid arthritis. N Engl J Med 350(25):2591–2602. https://doi.org/10.1056/NEJMra040226
Steiner M, Muñoz Fernández S (2010) Artritis reumatoide: fármacos modificadores de la enfermedad. Jano Med Humanid 1760:66
Carmona L, Villaverde V, Hernandez-Garcia C, Ballina J, Gabriel R, Laffon A (2002) The prevalence of rheumatoid arthritis in the general population of Spain. Rheumatol (Oxf Engl) 41(1):88–95. https://doi.org/10.1093/rheumatology/41.1.88
Carbonell J, Cobo T, Balsa A, Descalzo MA, Carmona L (2008) The incidence of rheumatoid arthritis in Spain: results from a nationwide primary care registry. Rheumatol (Oxf Engl) 47(7):1088–1092. https://doi.org/10.1093/rheumatology/ken205
Cross M, Smith E, Hoy D, Carmona L, Wolfe F, Vos T, Williams B, Gabriel S, Lassere M, Johns N, Buchbinder R, Woolf A, March L (2014) The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73(7):1316–1322. https://doi.org/10.1136/annrheumdis-2013-204627
Ruiz-Montesinos MD, Hernandez-Cruz B, Ariza-Ariza R, Carmona L, Ballina J, Navarro-Sarabia F (2005) Cost analysis in a cohort of rheumatoid arthritis patients managed in rheumatology units in Spain. Reumatol Clin 1(4):193–199. https://doi.org/10.1016/s1699-258x(05)72744-3
Mattila K, Buttgereit F, Tuominen R (2015) Influence of rheumatoid arthritis-related morning stiffness on productivity at work: results from a survey in 11 European countries. Rheumatol Int 35(11):1791–1797. https://doi.org/10.1007/s00296-015-3275-4
Ruiz-Montesinos MD, Hernandez-Cruz B, Ariza-Ariza R, Carmona L, Ballina J, Navarro-Sarabia F (2005) Resource utilization in a cohort of rheumatoid arthritis patients attended in rheumatology units in Spain. Reumatol Clin 1(3):142–149. https://doi.org/10.1016/s1699-258x(05)72733-9
Punzi L, Cimmino MA, Frizziero L, Gerloni V, Grassi W, Modena V, Montecucco C, Ramonda R, Schiavon F, Spadaro A, Trotta F (2007) Italian Society of Rheumatology (SIR) recommendations for performing arthrocentesis. Reumatismo 59(3):227–234
van Aken J, Lard LR, le Cessie S, Hazes JM, Breedveld FC, Huizinga TW (2004) Radiological outcome after four years of early versus delayed treatment strategy in patients with recent onset rheumatoid arthritis. Ann Rheum Dis 63(3):274–279. https://doi.org/10.1136/ard.2003.010298
Smolen JS, Landewe R, Breedveld FC, Buch M, Burmester G, Dougados M, Emery P, Gaujoux-Viala C, Gossec L, Nam J, Ramiro S, Winthrop K, de Wit M, Aletaha D, Betteridge N, Bijlsma JW, Boers M, Buttgereit F, Combe B, Cutolo M, Damjanov N, Hazes JM, Kouloumas M, Kvien TK, Mariette X, Pavelka K, van Riel PL, Rubbert-Roth A, Scholte-Voshaar M, Scott DL, Sokka-Isler T, Wong JB, van der Heijde D (2014) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis 73(3):492–509. https://doi.org/10.1136/annrheumdis-2013-204573
Smolen JS, Aletaha D, McInnes IB (2016) Rheumatoid arthritis. Lancet (Lond Engl) 388(10055):2023–2038. https://doi.org/10.1016/s0140-6736(16)30173-8
Sanmartí R, García-Rodríguez S, Álvaro-Gracia JM, Andreu JL, Balsa A, Cáliz R, Fernández-Nebro A, Ferraz-Amaro I, Gómez-Reino JJ, González-Álvaro I (2015) Actualización 2014 del Documento de Consenso de la Sociedad Española de Reumatología sobre el uso de terapias biológicas en la artritis reumatoide. Reumatol Clin 11(5):279–294
Smolen JS, Landewe R, Bijlsma J, Burmester G, Chatzidionysiou K, Dougados M, Nam J, Ramiro S, Voshaar M, van Vollenhoven R, Aletaha D, Aringer M, Boers M, Buckley CD, Buttgereit F, Bykerk V, Cardiel M, Combe B, Cutolo M, van Eijk-Hustings Y, Emery P, Finckh A, Gabay C, Gomez-Reino J, Gossec L, Gottenberg JE, Hazes JMW, Huizinga T, Jani M, Karateev D, Kouloumas M, Kvien T, Li Z, Mariette X, McInnes I, Mysler E, Nash P, Pavelka K, Poor G, Richez C, van Riel P, Rubbert-Roth A, Saag K, da Silva J, Stamm T, Takeuchi T, Westhovens R, de Wit M, van der Heijde D (2017) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis 76(6):960–977. https://doi.org/10.1136/annrheumdis-2016-210715
González-Álvaro I, Hernández-García C, Villaverde García V, Vargas E, Ortiz AM, emAR GdE (2002) Variabilidad en el tratamiento farmacológico de la artritis reumatoide en España. Med Clín 118(20):771–776
Lopez-Longo FJ, Seoane-Mato D, Martin-Martinez MA, Sanchez-Alonso F (2018) Variability in the prescription of biological drugs in rheumatoid arthritis in Spain: a multilevel analysis. Rheumatol Int 38(4):589–598. https://doi.org/10.1007/s00296-018-3933-4
Gómez-Reino JJ, Rodríguez-Lozano C, Campos-Fernández C, Montoro M, Descalzo MÁ, Carmona L (2012) Change in the discontinuation pattern of tumour necrosis factor antagonists in rheumatoid arthritis over 10 years: data from the Spanish registry BIOBADASER 2.0. Ann Rheumat Dis 71(3):382–385
Lapadula G, Ferraccioli G, Ferri C, Punzi L, Trotta F (2011) GISEA: an Italian biological agents registry in rheumatology. Reumatismo 63(3):155–164. https://doi.org/10.4081/reumatismo.2011.155
Gonzalez VM, Stewart A, Ritter PL, Lorig K (1995) Translation and validation of arthritis outcome measures into Spanish. Arthritis Rheum 38(10):1429–1446
Badia X, Roset M, Montserrat S, Herdman M, Segura A (1999) The Spanish version of EuroQol: a description and its applications. European Quality of Life Scale. Med Clin (Barc) 112(Suppl 1):79–85
Reilly MC, Zbrozek AS, Dukes EM (1993) The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics 4(5):353–365. https://doi.org/10.2165/00019053-199304050-00006
Oblikue consulting eSalud—Información económica del sector sanitario (2017) http://esalud.oblikue.com/. Accessed 10 Oct 2017
Consejo General de Colegios Oficiales de Farmacéuticos Bot PLUS (2017) https://botplusweb.portalfarma.com/. Accessed 10 Oct 2017
Instituto Nacional de Estadística (INE) (2017) Actualización de rentas con el IPC general (sistema IPC base 2016) para periodos anuales completos. http://www.ine.es/. Accessed 10 Oct 2017
Grupo de trabajo de la GUIPCAR (2011) Actualización de la Guía de Práctica Clínica para el manejo de la artritis reumatoide en España. 2011. Sociedad Española de Reumatología, Doyma ed, Madrid
Grupo de trabajo de la GUIPCAR (2018) Guía de práctica clínica para el manejo de pacientes con artritis reumatoide. Sociedad Española de Reumatología, Madrid
Carmona L (2008) Cambios entre anti-TNF,¿ están siempre justificados? Reumatol Clin 4(3):87–89
Balsa A (2011) Definiendo la remisión en la artritis reumatoide: nuevos criterios de la ACR/EULAR. Reumatol Clin 6:12–15
Villaverde V, Hernandez-Garcia C, Gonzalez-Alvaro I, Vargas E, Abasolo L, Morado I, emAR gde (2005) Evaluación clínica de los pacientes con artritis reumatoide en España. Rev Esp Reumatol 32(3):112–120
Navarro Sarabia F, Ballina García F, Hernández Cruz B, Hernández Mejía R, Ruiz Montesinos M, Fernández López J, Ariza Ariza R, Martín Lascuevas P, Carmona Ortell L (2004) Costes calidad de vida-artritis reumatoide. Estudio económico y de la calidad de vida de los pacientes con artritis reumatoide en España. Resultados preliminares. Rev Españ Reumatol 31(4):184–189
Funding
This study was supported by Sanofi Genzyme Spain.
Author information
Authors and Affiliations
Contributions
All the authors participated actively in the design of the work, the field work recruiting and collecting patient’s data, the analysis and later interpretation of data and in the writing of the present manuscript. In the same way, the final version of the manuscript has been reviewed and approved by all the authors. Also, this manuscript reflects honest, accurate and transparent information of the study and it has not been omitted key aspects of it.
Corresponding author
Ethics declarations
Conflict of interest
Dr Rubio reports speaker contributions for Lilly, Pfizer, Abbvie, Novartis, MSD, Celltrion, Sanofi, Roche, Gebro, Nordic, Grunenthal and UCB and was an advisor for Lilly, Sanofi, Biogen and Novartis. Dr Gómez-Centeno reportsspeaking fees from Pfizer, Lilly, Rubió, Abbvie, Sanofi, Roche, Janssen, travel expenses covered from Pfizer, Abbvie, Lilly, and was an advisor for Pfizer, Abbvie,Lilly, Sanofi, Rubió, Sandoz, Biogen and Gilead. Dr Gabriel Ovalles reports consultation and speaking fees from Abbvie, BMS, Celgene, Janssen, MSD, Novartis, Pfizer, Roche, Sanofi and UCB Pharma. Dr Manrique Arija reports speaking fees from Pfizer, Abbvie, MSD, UCB, Lilly, Novartis and Roche. Dr Marsal Barril was an advisor for Pfizer, Celgene, MSD, BMS, Abbvie, Sandoz, Novartis, Roche, UCB, Lilly, Sanofi and Janssen. Dr Amarelo Ramos reports speaking fees and consultancy from Sanofi and was an advisor for Novartis. Dr del Pino Montes reports consultancy from Amgen, Lilly, Pfizer, MSD, Abbvie, BMS, Novartis, Janssen and Sanofi. Dr Muñoz-Fernández reports speaking fees or was an advisor for MSD, Pfizer, Abbvie, Novartis, Janssen, UCB, Sanofi, Roche, Celgene and Gebro. Dr Bustabad was an advisor for Pfizer, AbbVie, Novartis, Sanofi, Roche, UCB and Janssen. Dr Barbazán Álvarez reports consultancy and expert testimony for Sanofi, Celgene, Novartis, Pfizer, Abbvie, Lilly, a grant from Janssen, speaker fees from Celgene, Sanofi, Novartis, Pfizer, Abbvie, Lilly and Roche, travel expenses covered from MSD, Abbvie, Lilly, Sanofi and Pfizer.
Ethical approval
The Ethics Committee of Hospital Parc Taulí, Sabadell, approved the study protocol (study code DIREGL08326) and allowed the retrospective analysis of available records of the patients between 2013 and 2016. The study was conducted in accordance with the principles of the Declaration of Helsinki of 1975/83.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gomez-Centeno, A., Rubio-Romero, E., Ovalles, J.G. et al. Clinical and therapeutic management of rheumatoid arthritis with biological disease-modifying antirheumatic drugs: RADAR study. Rheumatol Int 39, 2015–2024 (2019). https://doi.org/10.1007/s00296-019-04378-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-019-04378-6