Abstract
Rickettsia rickettsii, a tick borne disease, is the pathogen responsible for inducing Rocky Mountain Spotted Fever (RMSF), an illness that can progress to fulminant multiorgan failure and death. We present a case where R. rickettsii, acquired on a camping trip, precipitated a flare of peripheral arthritis and episcleritis in an HLA-B27 positive patient. Although Yersinia, Salmonella, Mycobacteria, Chlamydia, Shigella, Campylobacter, and Brucella have been previously associated with HLA-B27 spondyloarthritis, this unusual case demonstrates that obligate intracellular rickettsial organisms, and specifically, R. rickettsii, can also induce flares of HLA-B27 spondyloarthritis. Rickettsial infections in general can rapidly become fatal in both healthy and immunosuppressed patients, and thus, prompt diagnosis and therapy are required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spondyloarthritis refers to a group of inflammatory arthritides involving ligament/tendon insertion sites of the axial and, less frequently, the appendicular skeleton. Subsets of spondyloarthritis include both ankylosing spondylitis (AS) as well as reactive arthritis, among others [1,2,3]. The presence of the HLA-B27 genes confers a higher risk of developing ankylosing spondylitis, accounting for the preponderance in ethnic groups such as certain Native American tribes throughout the western United States [1]. Reactive arthritis is generally defined as a sterile, inflammatory mono- or oligoarthritis developing within 2–4 weeks after an enteric or urogenital infection. Like ankylosing spondylitis, reactive arthritis also has a frequent association with the presence of HLA-B27 [2].
Tick-borne illnesses have previously associated with both inflammatory and infectious arthritides; however, to this point, there has not been a documented case of Rickettsia-induced reactive arthritis flare in an individual who is HLA-B27 positive [4,5,6,7,8]. We present a case and literature review of the rickettsial tick-borne illness Rickettsia rickettsii, the causative agent of Rocky Mountain spotted fever (RMSF), precipitating a flare of HLA-B27 spondyloarthritis. This case emphasizes the importance of considering all possible precipitants of a reactive arthritis flare. Given the variable and potentially fatal course of rickettsial illnesses, those with even remote possibility of exposure should be evaluated for the presence of infection [4,5,6,7,8,9]. The need for awareness of Rickettsia species inducing reactive arthritis is of importance as the population of HLA-B27 positive individuals becomes increasingly immunosuppressed as a result of widespread use of biologic agents or chronic infections such as human immunodeficiency virus. In addition, we aim to understand the pathogenesis by which tick-borne illnesses induce reactive arthritis so as to improve diagnostic ease.
Patient information
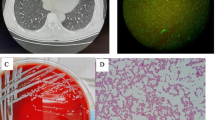
A 45-year-old female with a 19-year history HLA-B27-positive spondyloarthritis was well controlled for 4 years on the anti-tumor necrosis factor-alpha (anti-TNF) therapy (certolizumab pegol 400 mg subcutaneously every 4 weeks) (Fig. 1). She had failed multiple therapies prior to initiating certolizumab including: methotrexate, hydroxychloroquine, sulfasalazine, adalimumab, etanercept, and golimumab. Before being placed on certolizumab, approximately every 12 months, she would have a flare of spondyloarthritis with neck and low back pain, conjunctivitis, mild unilateral iritis, and effusive knee arthritis requiring aspiration and corticosteroid injection. However, these exacerbations resolved with certolizumab therapy. She presented to her primary care provider with a 5-day history of persistent frontal headache and fatigue without the other findings or symptoms. She related that she had gone camping in Southern New Mexico near a lake approximately 2 weeks previously, and admitted to receiving a number of mosquito bites, but denied any tick bites. She noted that she had a rash on her scalp and forehead that had resolved. She had self-administered her next certolizumab 400 mg injection 1 week after the camping trip.
Clinical findings
Physical examination was completely normal except for the presence of a resolving arthropod bite in the left occipital scalp that was interpreted as a resolving mosquito bite. The patient was told to return if her symptoms did not resolve. 2 days later, the patient had not improved and she consulted her rheumatologist. She complained of worsening frontal headache, stiff neck, fatigue, swollen glands, and arthralgias. Re-evaluation revealed persistent tender cervical lymphadenopathy, tenderness to the forehead above the orbits, and some stiffness in her neck, but the described rash and arthropod bite had resolved. The frontal headache in an immunosuppressed patient was thought to be due to sinusitis, and the patient was empirically treated with a 5-day course of azithromycin. However, over the next 13 days, the patient did not improve (at 21 days after her last certolizumab injection) and complained of an acute arthritis flare in her left knee (Fig. 2) and severe unilateral eye inflammation (Fig. 3) as well as worsening headache, lymphadenopathy, and stiff neck. The knee was aspirated, demonstrated inflammatory fluid with negative culture, and was subsequently injected with 60 mg triamcinolone acetonide. The eye was treated with combined antibiotic and corticosteroid drops, and the patient was referred to the eye clinic.
This photograph demonstrates monoarticular arthritis associated with a Rickettsia-induced flare in an HLA-B27-positive patient with spondyloarthritis. Note the dilated suprapatellar bursa superiorly and downward tilted patella due to extreme suprapatellar distention (Photograph Wilmer L. Sibbitt, Jr.)
Diagnostic assessment
Because of potential environmental exposure to arthropod-borne illnesses during her camping trip and the lack of clinical improvement, serologies were then obtained for Yersinia pestis, Lyme disease, Hanta virus, West Nile virus, and RMSF. However, 28 days had already elapsed, since the initial arthropod bite, suggesting that, if this was an arthropod-transmitted disease, it was resistant to azithromycin, already at an advanced stage, and at 4 weeks, these serologies would be considered the convalescent phase of an acute infection. Based on this exposure history and the lack of response to azithromycin, the patient was started empirically on doxycycline therapy at 100 mg orally twice per day for 14 days. It should be noted that the certolizumab was self-administered shortly after the tick bite (before any symptoms were noticed) and, thus, could not be discontinued in the setting of acute infection as per guidelines. The patient saw an ophthalmologist 1 week later and the inflamed eye had largely resolved, but the patient still had headache. 2 days after the eye examination, the patient progressed to severe headache, transient right-sided weakness, and an acute grand mal seizure and was admitted for evaluation. Cranial magnetic resonance imaging (MRI) with gadolinium contrast demonstrated enhancement of the leptomeninges and the cortical surfaces consistent with active meningoencephalitis (Fig. 4). Cerebrospinal fluid (CSF) findings were consistent with aseptic meningitis: minimally low glucose at 40 mg/dl (reference range 41–84 mg/dl), elevation of total nucleated cells to 96/mm3 (reference range 0–5/mm3) with lymphocytosis (7% neutrophils, 78% lymphocytes, and 18% monocytes), and mild elevation in total protein to 75 mg/dl with negative Gram stain and culture. CSF viral serologies were negative for West Nile Virus and Herpes Simplex I and II Virus. CSF bacterial cultures were finalized with no growth.
a Magnetic resonance (MR) T1 weighted image post-gadolinium contrast showing enhancement in the meninges (arrows) of the frontal lobe typical of Rickettsia-induced meningoencephalitis. b MR T1 weighted image post-gadolinium contrast in another slice showing enhancement consistent with meningoencephalitis (MRI Figures Wilmer L. Sibbitt, Jr.)
Serologies obtained 28 days after the arthropod bite were negative for Hanta virus, West Nile virus, Yersinia pestis, and Lyme disease, but were positive for R. rickettsii (1:256 IgG, normal < 1:64, low positive 1:64-1:128, high positive > 1:128), indicating recent, resolving, or chronic rickettsial infection based on Center for Disease Control guidelines [5].
Therapeutic intervention
Infectious disease consultation confirmed RMSF and recommended continuing the doxycycline 100 mg orally twice per day. She completed a 14-day course of doxycycline and had complete resolution of her symptoms and resumed her certolizumab therapy.
Follow-up and outcomes
A repeat cranial MRI obtained 28 days after the initial study demonstrated complete resolution of the meningoencephalitis. Convalescent serologies for R. rickettsii obtained 40 days after the arthropod bite continued to demonstrate an IgG titer of ≥ 1:256 (normal < 1:64, low positive 1:64-1:128, high positive > 1:128), confirming recent RMSF infection. At 1-year post-rickettsial infection, the patient occasionally complained of intermittent dizziness, memory problems, and difficulty concentrating. Cranial MRI obtained 1 year after the infection was normal.
Search methodology
We searched PubMed, Web of Science, and WorldCat using the keywords: spondylitis, ankylosing, rickettsia, reactive, and arthritis. We included that English sources, however, did not place time limits on the search given the unique scope of the paper (Rickettsia-induced arthritis flare) and the desire to be as inclusive of previous literature as possible. The bibliographies of the articles discovered based on the initial search were also evaluated for potential sources relevant to the topic.
Discussion
The rickettsiae are a diverse collection of obligately intracellular Gram-negative bacteria found in ticks, lice, fleas, mites, chiggers, and mammals, and include the genera Rickettsia, Ehrlichia, Orientia, and Coxiella [9]. Specific Rickettsia species induced intense and often fatal disease, including RMSF, rickettsial pox, other spotted fevers, epidemic typhus, and murine typhus [4,5,6,7,8,9]. Rickettsia species are found world-wide, including Europe, Asia, North and South American, and Africa, and are transmitted by a number of local arthropods including ticks, lice, fleas, and other biting arthropods [4,5,6,7,8,9]. R. rickettsii, the causative pathogen in RMSF, is a small, Gram-negative bacilli an obligate intracellular pathogen that is transmitted via the bite of several common ticks, including the American Dog Tick (Dermacentor variabilis), the Rocky Mountain Wood Tick (Dermacentor andersoni) (Fig. 5), and in parts of the southwestern United States and Mexico, the Brown Dog Tick (Rhipicephalus sanguineus) [4,5,6,7,8,9]. The American dog tick is most common in the eastern, central, and pacific coast United States, and the Rocky Mountain wood tick is encountered in the western states. The brown dog tick has been found throughout the United States. When taken in combination, these ticks (and R. rickettsii) can be encountered throughout almost the entire continental United States. That being said, areas with the greatest incidence of spotted fever Rickettsiosis include: Oklahoma, Arkansas, Missouri, Tennessee, North Carolina, Virginia, and parts of Arizona [4,5,6,7,8,9,10,11]. The percentage of infected ticks in North America with R. rickettsii are 0.26–1.5%, but this rate does vary considerably geographically with recent intense regional outbreaks [10, 11]. However, in certain areas of the world, local ticks are infected with endemic Rickettsia species at much higher rates, ranging from 22 to 100%, indicating considerable danger for immunosuppressed patients [10]. RMSP is frequently fatal even with therapy and is considered to be one of the most aggressive rickettsial diseases [4,5,6,7,8,9,10,11,12].
The Rocky Mountain wood tick (Dermacentor andersoni), a common vector of Rickettsia rickettsii in North America (Photographs: Adapted by Wilmer L. Sibbitt, Jr. from Disease Control and Prevention, Public Domain, James Gathany, https://phil.cdc.gov/Details.aspx?pid=10868, accessed November 24, 2018)
A recognized tick bite is reported in only 55–60% of cases, and thus, a high index of suspicion for environmental exposure and tick-borne illness is required for diagnosis [4]. In this case, the tick dropped off after feeding, leaving only the arthropod bite in the scalp. Following infection, R. rickettsii will invade vascular endothelial cells as well as underlying smooth muscle cells of the small and medium blood vessels. The resulting systemic vasculitis results in the distinctive petechial rash. In the later stages of disease, continued damage to vascular endothelial cells leads to increased permeability of capillaries, microhemorrhage, and consumption of platelets. Late-stage complications such as pulmonary and cerebral edema are the result of this increased vascular permeability [4, 12]. Early prodromal symptoms may include fever, headache, myalgias, gastrointestinal upset, abdominal pain, and a distinct petechial rash that often begins distally and spreads centrally. The rash characteristically appears 2–4 days after the development of fever and encompasses the palms and soles of the feet. Rash is observed in less than 50% of patients and, in some patients, may be atypically localized as in this case or may never develop. This early phase of RMSF in the first 1–5 days, if not treated, can rapidly progress in the following weeks to meningoencephalitis, seizures, coma, renal failure, acute respiratory failure, shock, and death, that occurs in 5% of those treated promptly and up to 40% who are treated late in the disease [4,5,6,7,8,9]. Of those cases of RMSF with abnormal neuroimaging findings as in this case, 17% die outright and 33% are left with chronic neurologic deficits emphasizing the gravity of neurologic rickettsial disease [12].
Ordinarily, acute serologies are obtained at the early phase (first 1–5 days) and convalescent serologies are obtaining 28 days later to demonstrate a fourfold rise in IgG levels; however, in this case, the diagnosis was delayed and serologies were obtained at 28 days and 40 days, and both were both high titer, indicating typical late-stage disease [4, 5]. IgM levels are not useful or reliable to diagnose rickettsial diseases [5]. It should be noted that R. rickettsii is resistant to azithromycin, and the present case did not respond to azithromycin [5,6,7]. However, our patient had complete resolution of symptoms with completion of doxycycline treatment for her rickettsial illness. R. rickettsii remains sensitive to doxycycline and chloramphenicol, and thus, the empiric switch of the patient from azithromycin to doxycycline before the serologies were available likely arrested disease progression and prevented any lethal complications as late-stage mortality from RMSF is typically 40% [4,5,6,7,8,9].
This patient developed acute arthritis and eye inflammation typical of HLA-B27-related disease (Figs. 2 and 3) [2]. The flare of HLA-B27-related disease was temporally related to the rickettsial infection with acute onset knee swelling accompanied by unilateral conjunctivitis/episcleritis in the weeks following the arthropod bite. This spondyloarthritis flare was unlikely to be due to withdrawal of the anti-TNF therapy, as the flare occurred 3 weeks after the last certolizumab injection and a week before the next planned certolizumab injection. Rickettsia species have not been previously associated with flares of reactive arthritis in a known HLA-B27-positive individual, in part because rickettsial infections are virulent and often fatal and because HLA B testing is not routinely performed after rickettsial infections [2,3,4].
Reactive arthritis associated with HLA-B27 is generally characterized by asymmetric, mono- or oligoarthritis that is typically preceded by an enteric or urogenital infection and is often associated with enthesitis/tendinitis, bursitis, eye disease (conjunctivitis, episcleritis, iritis, or uveitis), and rash [1,2,3, 13]. Reactive arthritis is known to be triggered by preceding specific bacterial infections, particularly of the genitourinary (Chlamydia trachomatis, Neisseria gonorrhea, and Ureaplasma urealyticum) or gastrointestinal (GI) tract (Salmonella enteritidis, Shigella, Yersinia enterocolitica, Campylobacter jejuni, and Clostridium difficile). Organisms that habitually survive intracellularly, including Yersinia, Salmonella, Mycobacteria, Chlamydia, Shigella, Campylobacter, and, potentially, Brucella, have all been previously associated with HLA-B27-induced disease, and thus, it is not surprising that the obligate intracellular rickettsial organism might have a similar effect [1,2,3, 13]. HLA-B27 may promote the invasion of implicated organisms into intestinal epithelial cells and then into the mesenteric lymph nodes instituting a complex pathologic immune response [14, 15].
Although the exact mechanism of association between ankylosing spondylitis HLA-B27 is unknown, it is believed that HLA-B27 leads to misfolding of intracellular proteins resulting in a unique peptide-major histocompatibility (MHC) complex that elicits an autoimmune response with AS as a consequence [15]. Intracellular organisms are then theorized to secrete antigens that “mimic” this unique peptide-MHC complex and trigger the self-reaction [13,14,15]. Recently, it has been demonstrated that HLA-B27-positive monocytic cells have decreased intracellular elimination and increased replication and trafficking of intracellular organisms [16, 17]. HLA-B27 positivity also has been shown to lead to lower levels of interferon-gamma (IFN-γ) leading to a more chronic course of arthritis and promoting latent forms of certain pathogens, most notably Chlamydia trachomatis [17]. Thus, HLA-B27-associated reactive arthritis is thought to be initiated by a primary extra-articular infection, but, because of the presence HLA-B27, there is persistence of viable but non-culturable bacteria, within the joint resulting in chronic arthritis [18]. Since Rickettsia are obligate intracellular organisms, it is not surprising that RMSF might provoke HLA-B27-associated spondyloarthritis in an manner similar to other implicated organisms [13, 14]. It is anticipated in the era of new antibiotics, treated and untreated human immunodeficiency virus, new immunosuppressant medications including biologics, and increasing travel of humans to environments with unusual organisms like Rickettsia, that new patterns and expression of HLA-B27 reactive arthritis will be increasingly recognized [19].
Despite the lack of previously documented Rickettsia-induced reactive arthritis and ocular flares in an HLA-B27-positive individual as reported here, there have been a number of previous reports of both infectious and non-infectious reactive arthritis and uveitis resulting from Rickettsia (Table 1). In 1996, Sundy et al. described the first known case of Rickettsia-associated monoarthritis [20]. This case a young male with RMSF had rash, fever, diarrhea, altered mental status, and monoarticular inflammatory arthritis of the right knee, although the HLA-B27 status was unknown [18]. Chaudhry et al. [21] reported a case of inflammatory polyarthritis resulting from R. rickettsii that was accompanied by classic prodromal symptoms. However, in contrast to our case, there was no history of spondyloarthritis, HLA-B27 positivity, or episcleritis. Premaratna and associates in Sri Lanka described four cases of polyarticular arthritis associated with concomitant Rickettsia conorii and Orientia tsutsugamushi infection with one of them suggestive of spondyloarthritis [22]. They reported a young male with erythema nodosum associated with swelling of the ankles, knees, and hips as well as pain of the sacroiliac joints and lumbar spine, but was not diagnosed with spondyloarthritis nor was reported to be HLA-B27 positive.
Rickettsia rickettsii has also been reported to induce anterior uveitis, retinitis, and iris nodules, but not episcleritis or scleritis—thus, the finding of episcleritis (Fig. 3) argues for a flare of the HLA-B27 disease rather than primary rickettsial eye involvement [23,24,25,26,27]. Rickettsial illnesses are difficult to diagnose, particularly in regions that are non-endemic for the classic vectors, and thus, the diagnosis as in this case is often delayed and morbidity is significant with mortality reported to be 40% at this late stage of diagnosis [4,5,6,7,8,9,10,11,12]. A high index of suspicion must be necessary to prevent life-threatening complications and death, particularly in immunosuppressed patients as in this case. Furthermore, immunosuppressed individuals in general should take measures to prevent arthropod bites, including avoiding arthropod environments and activity/swarm times, actively suppressing arthropod vectors, wearing hats, and long protective clothing, and using insect repellants [27, 28].
Conclusion
This case demonstrates that tick-borne R. rickettsii is another infectious agent that can trigger of flare of spondyloarthritis in an HLA-B27-positive patient. Although R. rickettsii is endemic to North America, similar arthropod-transmitted rickettsial organisms induce spotted fevers and other serious disease in Europe and world-wide, and thus, it is quite possible that that many of these other rickettsial organisms can also induce HLA-B27 reactive arthritis if the patient survives the initial infection [26]. Like many of the other organisms that can induce reactive arthritis, rickettsial infections can be fatal, especially in an immunosuppressed host, and thus, a high index of suspicion and a careful patient history, travel and arthropod exposure history, and physical are required to diagnose and promptly treat these individuals.
References
Kwas H (2019) Spondyloarthritis. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Spondyloarthritis. Accessed 15 Feb 2019
Hannu T (2011) Reactive arthritis. Best Pract Res Clin Rheumatol 25:347–357
Sheehan NJ (2004) The ramifications of HLA-B27. J R Soc Med 97:10–14
Biggs HM, Barton Behravesh C, Bradley KK et al (2016) Diagnosis and management of tickborne Rickettsial diseases: Rocky Mountain spotted fever and other spotted fever group rickettsioses, ehrlichioses, and anaplasmosis—United States. MMWR Recomm Rep 65:1–44
Center for Disease Control and Prevention (2019) Treatment, Rocky Mountain spotted fever (RMSF) CDC. https://www.cdc.gov/rmsf/healthcare-providers/treatment.html. Accessed 18 Feb 2019
Juckett G (2015) Arthropod-borne diseases: the Camper’s Uninvited Guests. Microbiology Spectrum. https://doi.org/10.1128/microbiolspec.iol5-0001-2014
Buckingham SC (2005) Tick-Borne infections in children: epidemiology, clinical manifestations, and optimal management strategies. Pediatric Drugs 7:163–176
Sexton DJ, Mclain MT (2017) Treatment of Rocky Mountain spotted fever. https://www.uptodate.com/contents/treatment-of-rocky-mountain-spotted-fever. Accessed February 8, 2019 (UpToDate 2018)
Walker DH (1996) Rickettsiae. In: Baron S (ed) Medical microbiology, chap 38, 4th edn. University of Texas Medical Branch at Galveston, Galveston
Socolovschi C, Mediannikov O, Raoult D, Parola P (2009) The relationship between spotted fever group Rickettsiae and Ixodid ticks. Vet Res. https://doi.org/10.1051/vetres/2009017
Center for Disease Control and Prevention (2019) Epidemiology and statistics, Rocky Mountain spotted fever (RMSF), CDC. https://www.cdc.gov/rmsf/stats/index.html. Accessed 24 Feb 2019
Bonawitz C, Castillo M, Mukherji SK (1997) Comparison of CT and MR features with clinical outcome in patients with rocky mountain spotted fever. AJNR Am J Neuroradiol 18:459–464
Saarinen M, Ekman P, Ikeda M, Virtala M, Grönberg A, Yu DTY, Arvilommi H, Granfors K (2002) Invasion of Salmonella into human intestinal epithelial cells is modulated by HLA-B27. Rheumatology (Oxford) 41:651–657
Chen B, Li J, He C, Li D, Tong W, Zou Y, Xu W (2017) Role of HLA-B27 in the pathogenesis of ankylosing spondylitis (review). Mol Med Rep 15:1943
Antoniou AN, Lenart I, Kriston-Vizi J et al (2019) Salmonella exploits HLA-B27 and host unfolded protein responses to promote intracellular replication. Ann Rheum Dis 78:74–82
Zhao Y, Tang H, Tan C, Zhao H, Liu Y (2017) HLA-B27 correlates with the intracellular elimination, replication, and trafficking of Salmonella Enteritidis collected from reactive arthritis patients. Med Sci Monit 23:5420–5429
Bas S, Kvien TK, Buchs N, Fulpius T, Gabay C (2003) Lower level of synovial fluid interferon-γ in HLA-B27-positive than in HLA-B27-negative patients with Chlamydia trachomatis reactive arthritis. Rheumatology (Oxford) 42:461–467
Rihl M, Klos A, Köhler L, Kuipers JG (2006) Reactive arthritis. Best Pract Res Clin Rheumatol 20:1119–1137
Misra R, Gupta L (2017) Time to revisit the concept of reactive arthritis. Nat Rev Rheumatol 13:327
Sundy JS, Allen NB, Sexton DJ (1996) Rocky mountain spotted fever presenting with acute monarticular arthritis. Arthritis Rheum 39:175–176
Chaudhry MA, Hal Scofield R (2013) Atypical Rocky Mountain spotted fever with polyarticular arthritis. Am J Med Sci 346:427–429
Premaratna R, Chandrasena TGAN, Rajapakse RPVJ, Eremeeva ME, Dasch GA, Bandara NKBKRGW, de Silva HJ (2009) Rickettsioses presenting as major joint arthritis and erythema nodosum: description of four patients. Clin Rheumatol 28:867–868
Vaphiades MS (2003) Rocky Mountain spotted fever as a cause of macular star figure. J Neuroophthalmol 23:276–278
Lam BL (2006) Rocky mountain spotted fever. Ann Ophthalmol (Skokie) 38:3–4
Raja H, Starr MR, Bakri SJ (2016) Ocular manifestations of tick-borne diseases. Surv Ophthalmol 61:726–744
Sathiamoorthi S, Smith W (2016) The eye and tick-borne disease in the United States. Curr Opin Ophthalmol 27:530–537
Koo S, Marty FM, Baden LR (2010) Infectious complications associated with immunomodulating biologic agents. Infect Dis Clin North Am 24:285–306
Nicholson WL, Paddock CD (2018) Rickettsial (spotted & typhus fevers) & related infections, including anaplasmosis & ehrlichiosis. Center for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2018/infectious-diseases-related-to-travel/rickettsial-spotted-and-typhus-fevers-and-related-infections-including-anaplasmosis-and-ehrlichiosis#5251. Accessed 8 Feb 2019
Funding
There was no funding for this report.
Author information
Authors and Affiliations
Contributions
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. Drs. AHR, JRT, and WLS collected the data, figures, and wrote the first manuscript draft; Dr. ADB, MF, and NSE, and Ms. SS help to organize the study, perform, and confirm citation searches, and revised the manuscript and figures.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have a conflict of interest.
Research involving human participants and/or animals
This was a case study exempted by the local Investigational Review Board (IRB). No animal studies were performed.
Informed consent
The subject gave informed consent to participate prior to all interventions and specifically provided permission for publication of this de-identified data, case report, and manuscript. All studies were carried out in accordance with the World Medical Association Declaration of Helsinki (JBJS 79A:1089-98, 1997). Patient confidentiality was protected according to the U.S. Health Insurance Portability and Accountability Act (HIPAA) and all data have been de-identified.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Redford, A.H., Trost, J.R., Sibbitt, W.L. et al. HLA-B27 spondyloarthritis and spotted fever rickettsiosis: case-based review. Rheumatol Int 39, 1643–1650 (2019). https://doi.org/10.1007/s00296-019-04330-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-019-04330-8