Abstract
The aim of this article was to critically assess the usefulness of hybrid molecular imaging (FDG PET/CT and FDG PET/MR) procedures in the evaluation of inflammatory activity in retroperitoneal fibrosis (RPF). A systematic review of the literature was performed using PubMed without timeline restriction and using the following keywords: retroperitoneal fibrosis, disease activity, diagnostic techniques, PET/CT, PET/MR. We evaluated full text articles written in the English language. Case reports, review articles or editorials and articles not in the field of interest of this review were excluded. Nine articles comprising a total of 186 patients met the inclusion criteria and were included and described in this systematic review. The new hybrid molecular imaging methods give promising results in the evaluation of the activity of the disease, quantification and prediction of therapeutic response and in tailoring medical therapy in RPF. FDG PET/CT can be a valuable tool in detecting disease activity, particularly in asymptomatic patients with RPF with acute phase reactant increase. Hybrid imaging can predict therapy response outcome and the best time for stent removal. Although PET/MR has potential advantage in small lesions and has reduced radiation exposure in comparison to PET/CT, PET quantification parameters have potentially higher diagnostic value over MR parameters in the evaluation of RPF. Acute phase reactants alone may not be reliable for the management and follow-up assessment of the disease. Hybrid imaging in RFP could be more comfortable, more accurate, with less radiation burden than different separate imaging studies acquired at different points in time.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Retroperitoneal fibrosis (RPF) is a rare collagen vascular disease with yet unknown etiology. It is characterized by a fibro-inflammatory reaction, usually starting around the retroperitoneal vascular structures and extending to the neighboring structures, first of all the ureters. RPF usually includes chronic periaortitis with inflammatory abdominal aortic aneurysms and with perianeurysmal retroperitoneal fibrosis. Nevertheless, additional fibrotic processes outside the retroperitoneum is not uncommon and is described in more than 15% of patients [1,2,3,4,5].
Though the true incidence of RPF is unknown, estimates range from 1 in 200,000 to 500,000 [1]. The condition occurs in men two to three times as much as in women, and peak incidence occurs in patients between 40 and 60 years of age.
Over two-thirds of RPF cases are considered idiopathic (Ormond’s disease) and one-third of cases of RPF occur secondary to other causes (infections, hemorrhage, trauma, radiotherapy, surgery, and use of certain drugs). Primary retroperitoneal neoplasms (such as lymphoma or sarcoma) and metastatic retroperitoneal tumors can also produce a desmoplastic reaction and mimic RPF. Malignant RPF is estimated to account for 8% of cases of RPF [6, 7]. Characterizing differentiating features of idiopathic RPF from underlying malignancy by radiographic evidence has proven challenging.
Patients with RPF typically present with dull abdominal and lumbar back pain that becomes acute. Physical examination is generally unremarkable with the exception of hypertension, probably of renal origin. Due to non-specific findings, patients can present with renal failure secondary to obstructive uropathy and long-standing hydronephrosis before the correct diagnosis is made. Ureteral involvement is reported in 80–100% of cases, and in the late stage of RPF it is characterized by progressive ureteral obstruction [8].
However, determining the presence of active inflammation is crucial for the management of patients with RPF and can be quite difficult, especially on the basis of only clinical parameters.
The gold standard for the diagnosis of RPF is still histopathology [9] with its typical presentation (inflammatory infiltrate characterized by mononuclear cells, chronic inflammation, fibroblast proliferation and excessive extracellular matrix) Fig. 1. Since its invasive nature, priority has been given to other less invasive procedures to obtain diagnosis as well as in monitoring therapy response.
Despite non-specific inflammatory indicators, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level, which are usually increased, no biochemical element can truly be considered as a specific marker of the disease in terms of severity, progression, or response [10].
Because laboratory tests are not often sufficiently specific, today preference is given to imaging techniques. The most commonly used imaging methods in this pathologic entity are multidetector computed tomography (MDCT) and magnetic resonance imaging (despite their difficulty in discriminating between active and fibrotic lesions and tumors). Nevertheless, MDCT may be useful in differentiating RPF from atherosclerosis or detecting morphological vascular alterations such as stenosis or aneurysms [2, 11]. Unfortunately, administration of intravenous contrast agents cannot be performed in many patients with renal impairment secondary to obstructive uropathy [12].
In this era, emphasis is placed on the use of noninvasive, safe, fast, informative and comfortable diagnostic procedures. For that reason, many clinicians pay more attention to the assessment of inflammatory activity in RPF with hybrid imaging (positron emission tomography with computed tomography—PET/CT; positron emission tomography with magnetic resonance imaging—PET/MR) using 18F-fluorodeoxyglucose (FDG). FDG is the glucose analog that identifies areas of high glucose metabolism, since inflammatory cells, such as neutrophils, lymphocytes and macrophages, have an increased glucose metabolism [13]. The main role of imaging in this field is not only its ability to diagnose the disease, but also to evaluate its extent, intensity, and most of all to assess therapy response, since the prognosis, treatment, and outcome of disease depends on it.
Several studies have evaluated the role of hybrid molecular imaging in diagnosing, assessing disease activity and monitoring RPF [10, 14,15,16,17,18,19,20,21]. Unfortunately, there is no consensus on which diagnostic procedures have the greatest impact on this issue. Since it is a rare clinical entity, insufficiently evaluated, the aim of this study is to systematically review relevant published articles on hybrid molecular imaging in the evaluation of RPF to add a more detailed and up-to-date analysis of this field.
Methodology
A comprehensive computer literature search of PubMed database was performed to identify relevant published articles on the role of FDG PET/CT and FDG PET/MRI in patients with RPF. We used a search algorithm based on the following keywords: retroperitoneal fibrosis, disease activity, diagnostic techniques, PET/CT, PET/MRI. Date limit was not used. Only full text papers, involving human population, written in English language were identified. We also searched the reference lists of identified articles to locate further papers. Two independent researchers reviewed articles to find all articles which can be included in this systematic review. Inclusion criteria for study selection were papers investigating the role of FDG PET/CT and FDG PET/MRI in patients with RPF. Case reports, review articles or editorials, and articles not in the field of interest of this review were excluded.
Results
Results of literature search
The comprehensive computer literature search from PubMed database revealed 18 articles. Revision of both the titles and the abstracts excluded 11 articles (3 were excluded as not within the field of interest of this review, 2 articles were excluded as reviews and 6 as case reports). Two additional studies were found by screening the references and passed inclusion criteria [14, 15] Fig. 2. Thus, nine articles [10, 14,15,16,17,18,19,20,21] were included in this systematic review (Tables 1, 2).
Nakajo et al. [14] evaluated the usefulness of FDG PET/CT in six male patients with RPF (five before steroid treatment and one during the treatment). They performed early and delayed imaging to examine change in the maximum standardized uptake value (SUVmax). Uptake was more intense on delayed images similar to the pattern observed in malignancies. Dual time point imaging was not useful to differentiate malignancy from RPF.
3 years after that, Piccoli et al. [15] reported seven patients with RPF who were prospectively studied to evaluate usefulness of FDG PET/CT in clinical management and ureteral stenting/stent removal. The authors noticed that CRP level was not uniformly related with severity and the clinical picture of RPF. After therapy, firstly clinical signs of disease remitted, and then the CRP level decreased. FDG PET/CT examination was mostly reliable as a therapeutic guide. The best time for stent removal was when there was no active disease on PET/CT examination.
Bertagna et al. [10] conducted a retrospective bicentric study in which they enrolled 25 patients with RPF (18 as initial evaluation, 3 during follow-up, 3 during steroid therapy, 1 for reevaluation of disease). The aim of the study was to assess the feasibility of PET/CT in patients affected by RPF for both an initial evaluation, during follow-up and for therapy response. Among the group of patients who performed an initial evaluation, 10/18 underwent a second PET/CT examination after steroid therapy. The authors suggested that FDG PET/CT is more sensible in early detection of therapy efficacy, since SUVmax values decreased statistically significantly in patients with complete metabolic response, while MDCT showed reduction of the mass or an unchanged scenario.
In the same year, Guignard et al. [16] reviewed ten patients suffering from RPF and observed clinical changes between baseline PET/CT scan and follow-up. Unlike biologic and CT parameters, FDG uptake was the most relevant parameter to measure the severity of inflammation, while CT was better in the delineation of periaortitis and its extension to adjacent structures.
Moroni et al. compared the levels of CT contrast enhancement (CE) and FDG uptake in the fibro-inflammatory mass and their relationship with the most common inflammatory markers (CRP, ESR). FDG PET/CT was performed in 7 newly diagnosed patients and in 15 patients with known disease (5 patients with relapse, 5 patients in remission without therapy and 5 patients still under therapy). Follow-up PET/CT was performed in nine patients. The CT CE level of the mass was determined in all patients 15 days before PET/CT. The CT CE status of RPF was scored as: 0 (CE < 20 HU, inactive disease); 1 (CE 20–30 HU, moderate disease activity); or 2 (CE > 30 HU, marked disease activity). All patients were split in two groups: A (active disease) and B (inactive disease). Patients with disease status score 1 or 2 with increased CRP and ESR value formed group A. Patients with disease status score 0 with normal CRP and ESR level were in group B. There was significant differences between the median SUVmax values of these groups (it was higher in A group). The ROC analysis showed that using SUV threshold greater than 2.76, active disease was detected with a sensitivity of 95.5% and inactive disease with a specificity of 90.9%. Significant agreement was found between visual assessment of FDG uptake and CE score (87.8%, p < 0.01) and between the SUVmax value and CE score (90.9%, p < 0.01). Significant correlations were observed between ESR and SUVmax value (rho = 0.55), SUVmax and CRP (rho = 0.56) and among inflammatory markers’ levels and CE score (p < 0.05) [17].
In 2015, Fofi et al. investigated the role of FDG PET/CT in the management of RPF at periodic follow-up examination and evaluated the correlations between biochemical markers and PET/CT parameters of disease activity. This retrospective study evaluated seven consecutive patients with RPF during 10 years. In PET-positive patients, they found elevated ESR in three patients, high CRP level in four and high BUN and serum creatinine in one, while there was one PET-positive patient with normal laboratory parameters. Stepwise regression showed that serum creatinine, blood urea nitrogen (BUN) and CRP if considered together were significantly correlated with SUVmax (p = 0.000003057). After medical therapy and progressive clinical remission, FDG PET/CT showed complete normalization of FDG uptake, while CT did not show any change [18].
In 2016, Ruhlmann et al. assessed RPF in 22 patients with FDG PET/CT examination, which was followed by abdominal PET/MR scan in 17 patients. The patient cohort was subdivided into two groups: 6 examinations in untreated and 16 in treated patients. FDG PET/CT analysis included assessment of SUVmax; MR analysis including evaluation of T2-weighted image signal intensity, contrast enhancement and diffusion restriction (ADC values). The differences in the hyperintense signal between the two patient groups were statistically significant only for the T2-W images (p = 0.0124). Quantitative analysis revealed significantly higher SUVmax in untreated patients on PET/CT and PET/MR (p = 0.0154). The mean values for ADC min and ADC mean were lower in the untreated group. Untreated patients showed statistically higher ESR and CRP values than the treated patients. There was significant inverse correlation between ADC min and SUVmax on PET/MR (r = –0.65, p = 0.0019) and moderate correlation between CRP and SUVmax on PET/MR (r = 0.45) [19].
Fernando et al. prospectively evaluated 78 patients who underwent PET/CT, CT and blood tests, to evaluate the potential of FDG PET/CT in clinical decision making and management of RPF. The median follow-up was 16 months, and 23 patients came to follow-up PET/CT. Of the 78 patients, 62 (79%) were prescribed steroids, of whom 47 (76%) underwent PET/CT examination. Response to steroids corresponded to the degree of initial FDG uptake on PET. Patients with high-grade FDG avidity were more likely to respond to steroids than patients with low-grade FDG avidity or negative PET. In 29% of scans, there was discordance between FDG PET/CT findings and inflammatory markers. In 19/38 scans, there was FDG uptake within the RPF despite normal marker levels, and ten patients with no FDG uptake had raised markers and had no response to steroids. The negative predictive value of FDG PET/CT was 100% (95% CI 0.95–0.97); the positive predictive value of atypical high-avidity FDG PET/CT for detecting malignancy was 50% (95% CI 0.12–0.43) [20].
Finally, Thuermel et al. evaluated the value of FDG PET/MR with regard to disease activity, extent and vascular involvement compared to clinical and laboratory parameters. They enrolled 14 patients who underwent PET/MR. Qualitative (visual 4-point scale) and quantitative image analysis (SUVmax, target–background ratio—TBR, RPF thickness and volume) was done. The laboratory parameters (ESR, CRP) did not correlate with PET/MR parameters. In 29% of patients with active disease seen on PET/MR, the laboratory parameters were in the normal range. SUVmax, TBR and volume of retroperitoneal mass differed significantly between therapy-naive patients and patients under therapy (SUVmax p = 0.004, TBR p = 0.015, volume p = 0.015) [21].
Discussion
Nowadays, there is a tendency to use molecular imaging in the diagnosis of various inflammatory diseases, including RPF. This hybrid model provides information of the precise anatomic localization of the disease and the functional changes at the cellular level. Also, one of the benefits of this examination is the assessment of the whole body, which is especially important to exclude malignancy/malignant RPF. It involves simultaneous scans instead of two consecutive scans that may be considered beneficial with regard to patient comfort.
Hybrid imaging is more expensive than CT scan. However, it has better performance and ability to semi-quantitatively evaluate and monitor the inflammatory activity in pathological focus that cannot be done with other morphologic examinations. Radiation exposure in PET/CT examination (about 25 mSv) comes from the radiation emitted by the radiopharmaceutical (one-third of the total value) and from the CT component. Using a low-dose CT protocol, the mean CT radiation dose can be reduced by 32%. Thus, the mean effective dose can be reduced without degradation of image quality. Reduced radiation exposure is even more pronounced in PET/MR examination, which is having radiation only from the use of a radiopharmaceutical [18, 19, 22, 23]. Hybrid imaging may replace the use of non-purposive laboratory and radiological procedures that are not sufficiently informative in assessing the activity of inflammatory disease in RPF. Thus a overall cost effectiveness of hybrid imaging can be considered better.
However, the exact usefulness of hybrid imaging in patients with RPF is unknown due to a small number of studies that evaluated this rare disease. Also, there are no established PET/CT or PET/MR criteria for the diagnosis of this pathological entity [11]. Comparative characteristics of these two diagnostic procedures are given in Table 3.
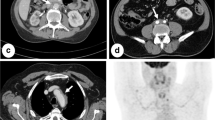
Regardless of the method of evaluation of disease activity, the majority of available studies suggest that FDG PET/CT could be useful in evaluating the disease extent and activity at the time of diagnosis. The evaluation of the metabolic activity of RPF on PET/CT can be done by visual analysis (Fig. 3). It is usually performed in four-point graded scale, based on the vessel-to-liver FDG uptake ratio (0: no uptake, 1: uptake less than that of the liver, 2: uptake equal to that of the liver, and 3: uptake greater than that of the liver); a visual score above 1 is usually considered a positive criterion for active RPF. Semiquantitative analysis is also used, based on the calculation of SUVmax, target–background ratio—TBR, RPF thickness and volume.
FDG PET/CT can be also useful in cases of exacerbation and progression of disease, highlighting new foci of inflammation not documented at morphological imaging [10, 20]. Nakajo et al. [14] suggested that FDG PET/CT could be helpful in assessing disease activity during or after treatment in patients with normal inflammatory marker levels and stable residual mass on repeated MDCT scans. Assessment of FDG uptake based on the calculation of the SUVmax can be useful for treatment response evaluation and follow-up of these patients [10, 15, 16]. The authors proposed that FDG PET/CT could be used in both diagnostic and follow-up workup, to tailor medical and surgical decisions [10, 15, 16, 18, 20]. In patients who have RPF with no FDG uptake, stent removal might be done earlier in the disease course and thus spared of potential complications of unnecessary treatment [15].
Fernando et al. stated that PET/CT was good in identifying patients at high or low risk of malignancy before biopsy. Their results indicate that patients with highly FDG-avid lesions, which are not perivascular, are highly suspicious for malignancy before biopsy with sensitivity of 100%. On the other hand, the positive predictive value of atypical high-avidity FDG PET lesions for detecting malignancy was 50%. This finding may have clinical value, because biopsy in these situations can be challenging owing to the risk of arterial injury [20].
According to Fernando et al., response to steroids corresponded to the degree of initial FDG uptake on PET/CT examination. The authors also have noticed that only patients with high-grade FDG avidity had good therapy response to steroid therapy.
On the other hand, patients with negative FDG PET/CT and others with low-grade FDG avidity on the PET/CT examination did not have a measurable response to steroid treatment. Thus, steroids may not be beneficial if PET/CT scans were negative [20]. Since, morbidity associated with oral steroids is considerable, with >80% complaining of one or more side effect, an individualized approach based on the prediction of response is desirable [24].
It seems that FDG uptake was in close relationship with the CE score. However, inconsistent PET results were obtained in patients with diffuse aortic calcifications and others who had FDG-inactive RPF, but elevated inflammatory markers. False increase of FDG uptake may be related to beam-hardening artifact, which should not be overlooked since many patients with RPF have vascular calcifications [17].
On the other hand, PET/MR has a different study analysis from PET/CT. PET/MR image analysis includes visual assessment of the signal intensity on T2-W images and relative contrast uptake in RPF lesions on the contrast-enhanced fat-saturated T1-W images. The findings were considered qualitatively positive if there was a high signal intensity on DWI images and low signal on the corresponding ADC map. Then these changes were quantitatively analyzed by rounding ellipsoid regions of interest with identical position and size on the DWI images and the ADC maps [19].
According to Ruhlmann et al., T2-W imaging can be helpful in differentiating between acute and non-acute stages of RPF. In the acute phase of disease, higher signal intensities are observed. They are probably caused by structural tissue changes due to edema and hypercellularity in the active phase of the disease. The authors also found significantly higher values for contrast enhancement, DWI and FDG uptake in active RPF than in patients treated with RPF. The advantage of using PET/MR in small lesions was also noted [19].
Current studies show that DWI is highly beneficial for functional assessment of acute stage of RPF, which can be useful since it is free of gadolinium-associated risk factors. This may be very useful in RPF patients, who are likely to suffer from renal insufficiency due to frequent ureteral compression. The benefits of PET/MR are also seen due to reduced radiation exposure [19].
However, the PET parameters (FDG uptake score and SUVmax) showed higher statistical significance than the MR parameters (DWI, T2 signal intensity and ADC values) in discrimination between the treated and untreated RPF patients. Thus, PET can have potentially higher diagnostic value over MR [19]. Other quantitative PET parameters (TBR and volume of retroperitoneal mass) differed significantly between treated and untreated patients [21].
Since the pathological characteristics of the infiltrate in retroperitoneal fibrosis do not differ significantly regardless of the type of retroperitoneal fibrosis (idiopathic, malignant, radiotherapy induced), additional data are necessary (anamnestic data on the use of certain drugs, radiation exposure and laboratory analysis).
Most authors agree that the laboratory parameters of inflammation have limited importance in RPF, due to their low specificity. Literature data show that inflammatory markers have a sensitivity of 71% and a specificity of 62% in detecting active or inflammatory RPF if FDG PET/CT is used as a proxy for inflammatory activity in RPF. Around 29% of patients had discordance between serum inflammatory markers and FDG PET/CT findings, raising questions about the validity of surveillance schedules based on serum markers alone [20].
Raised inflammatory markers and negative PET scans may be a reflection of systemic autoimmune diseases, infections, etc. [17]. Acute phase reactants alone may not be reliable for the management and follow-up assessment of disease. On the other hand, in patients with ureteral involvement, CRP together with BUN and serum creatinine has significant correlation with PET/CT results and can help the physicians in their therapeutic approach better than a single parameter [18].
Conclusion
Retroperitoneal fibrosis is a rare entity still not sufficiently clarified. The new hybrid molecular imaging methods give promising results in the evaluation of the activity of the disease, as they are more informative than standard radiology techniques. It seems that FDG PET/CT examination of RPF could be more comfortable and more accurate, with less radiation burden than different separate imaging studies acquired at different points in time. This could be important especially in patients with renal impairment in whom administration of i.v. contrast agents cannot be performed on MDCT.
FDG PET/CT can be a valuable tool in detecting disease activity, particularly in asymptomatic patients with RPF with acute phase reactant increase [17]. A special role of molecular imaging can be in the quantification and prediction of therapeutic response and in tailoring medical therapy [10, 15, 16, 20]. Hybrid imaging can predict therapy response outcome and predict the best time for stent removal [15, 20].
Inflammatory markers alone have limited correlation with PET parameters in the evaluation of RPF. However, in patients with ureteral involvement, CRP together with BUN and serum creatinine has a significant correlation with PET/CT results. PET/MR has a potential advantage in small lesions and has reduced radiation exposure in comparison to PET/CT. However, PET quantification parameters have potentially higher diagnostic value over MR parameters in the evaluation of RPF [19]. Further prospective multicenter studies are necessary to confirm these finding and this hypothesis and refine the clinical role of molecular imaging in retroperitoneal fibrosis.
References
VaglioA Salvarani C, Buzio C (2006) Retroperitoneal fibrosis. Lancet 367(9506):241–251
Palmisano A, Vaglio A (2009) Chronic periaortitis: a fibro-inflammatory disorder. Best Pract Res 23(3):339–353
Pipitone N, Salvarani C, Peter HH (2010) Chronic periaortitis. Internist 51:45–52
Otomi Y, Otsuka H, Terazawa K, Nose H, Kubo M, Yoneda K, Kitsukawa K, Harada M (2013) (18)F-2-fluoro-2-deoxyglucose uptake in or adjacent to blood vessel walls. J Med Invest 60(1–2):15–20
Yilmaz S, Tanb YZ, Ozhan M, Halac M, Asa S, Sönmezoglu K (2012) FDG PET/CT in monitoring treatment of retroperitoneal fibrosis. Rev Esp Med Nucl Imagen Mol 31(6):338–339
Lepor H, Walsh PC (1979) Idiopathic retroperitoneal fibrosis. J Urol 122(1):1–6
Mehta A, Blodgett MT (2011) Retroperitoneal Fibrosis as a cause of positive FDG PET/CT. J Radiol Case Reports 5(7):35–41
Van Bommel EF, Siemes C, Hak LE, van der Veer SJ, Hendriksz TR (2007) Long-term renal and patient outcome in idiopathic retroperitoneal fibrosis treated with prednisone. Am J Kidney Dis 49(5):615–625
Monev S (2002) Idiopathic retroperitoneal fibrosis:prompt diagnosis preserves organ function. Cleve Clin J Med 69:160–166
Bertagna F, Treglia G, Leccisotti L (2012) [18F]FDG-PET/CT in patients affected by retroperitoneal fibrosis: a bicentric experience. Jpn J Radiol 30:415–421
Kottra JJ, Dunnick NR (1996) Retroperitoneal fibrosis. Radiol Clin North Am 43:1259–1275
Talati SJ, Abghari R, Kochkodan JJ, Helmer SR (1995) Use of Ga-67 imaging in diagnosis and follow-up after steroid treatment of retroperitoneal fibrosis. Clin Nucl Med 20:995–997
Treglia G, Mattoli MV, Bertagna F, Giubbini R, Giordano A (2013) Emerging role of Fluorine-18-fluorodeoxy glucose positron emission tomography in patients with retroperitoneal fibrosis: a systematic review. Rheumatol Int 33:549–555
Nakajo M, Jinnouchi S, Tanabe H, Tateno R, Nakajo M (2007) 18F-fluoro deoxyglucose positron emission tomography features of idiopathic retroperitoneal fibrosis. J Comput Assist Tomogr 31(4):539–543
Piccoli GB, ConsiglioV Arena V, Pelosi E, Anastasios D, Ragni F, Fiori C, Cortese G, Deagostini MC, Porpiglia F, Scarpa RM (2010) Positron emission tomography as a tool for the‘tailored’management of retroperitoneal fibrosis: a nephro-urological experience. Nephrol Dial Transpl 25(8):2603–2610
Guignard R, Simukoniene M, Garibotto V, Ratib O (2012) 18F-FDG PET/CT and contrast-enhanced CT in a one-stop diagnostic procedure: a better strategy for management of patients suffering from retroperitoneal fibrosis? Clin Nucl Med 37(5):453–459
Moroni G, Castellani M, Balzani A, Dore R, Bonelli N, Longhi S, Martinelli I, Messa P, Gerundini P (2012) The value of 18FFDG PET/CT in the assessment of active idiopathic retroperitoneal fibrosis. Eur J Nucl Med Mol Imaging 39:1635–1642
Fofi C, Prosperi D, Pettorini L, Festuccia F, Pirisino R, Lanni V, Scopinaro F, Punzo G, Menè P (2016) Diagnosis and follow-up of idiopathic retroperitoneal fibrosis: role of (18)F-FDG-PET/CT and biochemical parameters in patients with renal involvement. Intern Emerg Med 11(6):809–816
Ruhlmann V, Poeppel TD, Brandt AS, Grüneisen J, Ruhlmann M, Theysohn JM, Forsting M, Bockisch A, Umutlu L (2016) (18)F-FDG PET/MRI evaluation of retroperitoneal fibrosis: a simultaneous multiparametric approach for diagnosing active disease. Eur J Nucl Med Mol Imaging. 43(9):1646–1652
Fernando A, Pattison J, Horsfield C, D’Cruz D, Cook G, O’Brien T (2016) [18F]-fluorodeoxyglucose positron emission tomography in the diagnosis, treatment stratification, and monitoring of patients with retroperitoneal fibrosis: a prospective clinical study. Eur Urol. doi:10.1016/j.eururo.2016.10.046
Thuermel K, Einspieler I, Wolfram S, Moog P, Meier R, Schwaiger M, Heemann U (2017) Disease activity and vascular involvement in retroperitoneal fibrosis: first experience with fully integrated 18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging compared to clinical and laboratory parameters. Clin Exp Rheumatol 35 Suppl 103(1):146–154
Brix G, Lechel U, Glatting G, Ziegler SI, Münzing W, Müller SP, Beyer T (2005) Radiation exposure of patients undergoing whole-body dual-modality 18F-FDG PET/CT examinations. J Nucl Med 46(4):608–613
Tonkopi E, Ross AA, MacDonald A (2013) Journal club: CT dose optimization for whole-body PET/CT examinations. AJR Am J Roentgenol 201(2):257–263
Veenstra DL, Best JH, Hornberger J, Sullivan SD, Hricik DE (1999) Incidence and long-term cost of steroid-related side effects after renal transplantation. Am J Kidney Dis 33(5):829–839
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the study.
Conflict of interest
Isidora T. Grozdic Milojevic, Bogomir Milojevic, Dragana P.Sobic-Saranovic and Vera M.Artiko declare that they have no conflict of interest.
Ethical approval
For this type of retrospective study formal consent is not required.
Rights and permissions
About this article
Cite this article
Grozdic Milojevic, I.T., Milojevic, B., Sobic-Saranovic, D.P. et al. Impact of hybrid molecular imaging in retroperitoneal fibrosis: a systematic review. Rheumatol Int 38, 179–187 (2018). https://doi.org/10.1007/s00296-017-3798-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-017-3798-y