Abstract
Ankylosing spondylitis (AS) is a chronic inflammatory disease of unknown origin, while both genetic and environmental factors have been demonstrated to be etiologically involved. Recent genome-wide association and replication studies have suggested that anthrax toxin receptor 2 (ANTXR2), interleukin-1 receptor 2 (IL1R2), caspase recruitment domain-containing protein 9 (CARD9), and small nuclear RNA-activating complex polypeptide 4 (SNAPC4) seem to be associated with AS pathogenesis. This case–control study was performed on 349 unrelated AS patients and 469 age- and gender-matched healthy controls, to investigate whether these non-MHC genes (IL1R2 rs2310173, ANTXR2 rs4333130, CARD9 rs4077515, and SNAPC4 rs3812571) influence the AS risk in Iranian population. ANTXR2 rs4333130 allele C (p = 0.0328; OR 0.744, 95 % CI 0.598–0.927) and genotype CC (p = 0.0108; OR 0.273, 95 % CI 0.123–0.605) were found to be significantly protective against AS. No other associations were found between AS and studied genes. The association between ANTXR2 rs4333130 and AS was independent of HLA-B27 status. Moreover, we found clinical disease severity scores (BASDAI and BASFI) and pain score were higher in ANTXR2 rs4333130 CT genotype. However, we observed that CARD9 allele C (p = 0.012) and genotype CC (p = 0.012) were significant protective factors against AS only in HLA-B27-negative patients, and IL1R2 rs2310173 genotype GT was mildly protective against AS only in HLA-B27-negative status. These findings support the role of non-MHC pathogenic pathways in susceptibility to AS and warrants more comprehensive studies focusing on these non-MHC pathways for developing novel therapeutic strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankylosing spondylitis (AS) belongs to the family of spondyloarthropathies and is a chronic inflammatory disease that primarily affects the sacroiliac joints and the axial skeleton [1]. AS patients have pain, stiffness, initial bone and joint erosion, and ultimately ankylosis and fibrosis [2, 3]. Inflammation may also involve extra-articular sites such as the uveal tract, tendon insertions, proximal aorta, and, rarely, lungs and kidneys [3].
The importance of genetic factors in AS susceptibility became clear after discovery of HLA-B27 as one major contributor to AS hereditability [4]. More exactly, genes within the MHC region influence nearly 25 % of AS hereditability, so that approximately 90 % of AS patients express the HLA-B27 antigen [4–6], but only about 73.5 % of Iranians patients [7] have HLA-B27. Moreover, minor contributions from genes outside of the MHC locus have been recognized to be associated in predisposing individuals to AS, which contribute up to 25.39 % of the overall heritability of AS [4]. To date, more than 14 susceptibility genes or genetic loci are identified to be associated with AS susceptibility based on genome-wide association studies regarding of individuals from the USA, UK, and Australia (the Australo–Anglo–American Spondylitis Consortium or TASC, in collaboration with the Wellcome Trust Case Control Consortium) [3, 8, 9].
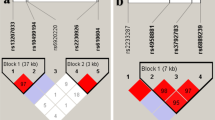
Endoplasmic reticulum aminopeptidase 1 (ERAP1) is determined as the strongest non-MHC gene associated with AS [4, 10]. The other genetic loci beyond MHC that contribute in AS susceptibility include IL 17–IL 23 axis genes, IL1 region genes including IL1R2, IL12B, and TNF pathway-associated genes, Anthrax toxin receptor 2 (ANTXR2), and caspase recruitment domain-containing protein 9 (CARD9) [4]. Also SNAPC4 (9q34.3) which is in linkage disequilibrium (LD) with CARD9 is shown to be associated with AS in Han Chinese population [11]. To the best of our knowledge, lots of these beyond MHC genes, such as ERAP1, are highly correlated with HLA-B27 [4].
Some major questions regarding heritability of AS remained to be answered, for example, whether or not these beyond MHC genes are correlated with AS. Thus, we performed this study to investigate whether these non-MHC genes (IL1 R2, ANTXR2, CARD9, and SNAPC4) affect the AS risk in Iranian population.
Patients and materials
Study population
The study group consists of 349 unrelated AS patients and 469 age- and gender-matched healthy controls. Diagnosis of AS patients was based on 1984 modified New York criteria. All patients were enrolled from Rheumatology Research Center of Tehran University of Medical Sciences, Shariati Hospital, and Iranian Association of AS. Ethics committee of Tehran University of Medical Sciences approved this study (according to the Declaration of Helsinki), and written informed consent was obtained from all individuals.
AS patients were examined for disease severity and functional capacities by a protocol based on the Assessment of Spondyloarthritis International Society (ASAS) core set [12], which include disease activity by Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) [13]; function by Bath Ankylosing Spondylitis functional Index (BASFI) [14]; damage or deformity of the spine by Bath Ankylosing Spondylitis Metrology Index (BASMI) [15]; Bath Ankylosing Spondylitis Global Index (BASG); and pain score. Validated Persian versions of BASDAI and BASFI questionnaires have been provided in our previous studies [16]. The Ankylosing Spondylitis Quality of Life (ASQoL) questionnaire was employed for the assessment of quality of life.
Genotyping
Genomic DNA was extracted from peripheral blood samples with standard phenol–chloroform–proteinase-K method [17]. Samples were genotyped for 4 selected SNPs including IL1 R2 (rs2310173), ANTXR2 (rs4333130), CARD9 (rs4077515), and SNAPC4 (rs3812571). Real-Time PCR allelic discrimination TaqMan genotyping assays (Applied Biosystems, Foster city, USA) were applied to genotyping each study participant, using ABI StepOne Plus Real-Time PCR system. Reactions were processed following standard protocols of Applied Biosystems. The allelic call was performed by the analysis of allelic discrimination plots, using ABI SDS version 1.4 software.
Statistical analysis
Data analysis was performed using IBM SPSS Software (version 20). Quantitative data with normal distribution are expressed as Mean ± SD, and non-normally distributed characteristics are shown as Median (interquartile range; IQR). The odds ratio (with 95 % CI) and p values were calculated for each allele and genotype. The genotype distributions of all selected SNPs were tested for deviation from the Hardy–Weinberg equilibrium in control group using Chi-square test. p value of less than 0.001 was considered statistically significant for HWE [18]. For investigating the associations between genetic markers (alleles, genotypes) and clinical status (AS vs. healthy controls), Chi-square test and logistic regression were performed. p values less than 0.05 were considered statistically significant after adjusting for false discovery rate (FDR) by Benjamini–Hochberg method [19]. In addition, Mantel–Haenszel test was performed to discover the possible epistasis/interactive effects of HLA-B27 with studied genes.
Results
Demographic information
The patients group included 285 men and 64 women, with median (IQR) age of 37 (14) years and disease duration of 15 (12) years. Most of AS patients (75.1 %) were HLA-B27-positive. The healthy controls included 387 men and 82 women, with the median (IQR) age of 36 (16) years. No significant differences were observed between AS patients and healthy controls regarding age (p = 0.082) and sex (p = 0.752). Control subjects and their family did not report to have any autoimmune and rheumatic diseases. Only 4.5 % of healthy controls were HLA-B27 -positive.
Association of AS with IL1 R2, ANTXR2, CARD9, and SNAPC4
The allelic and genotype frequencies of studied SNPs are demonstrated in Table 1. We did not observe any significant deviation from Hardy–Weinberg equilibrium in healthy controls. ANTXR2 (rs4333130) allele C (p = 0.0328; OR 0.744, 95 % CI 0.598–0.927) and genotype CC (p = 0.0108; OR 0.273, 95 % CI 0.123–0.605) were found to be significantly protective against AS. More exactly 31.3 % of healthy controls had allele C compared to 25.4 % of AS patients, and 7.2 % of healthy controls had genotype CC as compared to 2.3 % of AS patients. No significant associations were observed for other studied SNPs (Table 1).
Associations between HLA-B27 and IL1 R2, ANTXR2, CARD9, and SNAPC4
Interestingly, Mantel–Haenszel test (p = 0.012, Tables 2 and 3) showed that CARD9 allele C (p = 0.012; OR 0.624, 95 % CI 0.432–0.902) and genotype CC (p = 0.005; OR 0.477, 95 % CI 0.289–0.789) are significant protective factors against AS in HLA-B27-negative patients, while it is not meaningful in HLA-B27-positive ones. IL1R2 genotype GT showed to be mildly protective against AS in HLA-B27-negative patients (Table 3).
Clinical severity scores
In the whole patients' population, numeric rate scale of pain score (p = 0.006), ASQOL (p = 0.032), BASFI (p = 0.036), and BASDAI (p = 0.017) were significantly different between ANTXR2 rs4333130 genotypes. Interestingly, ANOVA followed by Tukey’s post hoc analysis revealed that ANTXR2 rs4333130 CT genotype has higher disease severity scores as compared to TT genotype. These findings were the same in AS patients (data not shown). Clinical characteristics of AS patients are compared between HLA-B27-positive and HLA-B27-negative patients (supplementary Table 1). We observed a slightly significant higher BASMI score and axial immobility in HLA-B27-positive individuals. Moreover, we observed that AS patients with positive HLA-B27 were significantly younger at the initiation of disease symptoms and at the time of diagnosis, as compared to HLA-B27-negative patients (p < 0.001; supplementary Table 1).
Discussion
Recently many genes outside MHC region have been investigated for AS susceptibility [4, 9]. Lots of minor contributions to the AS heritability have been discovered such as IL1 R2, ANTXR2, CARD9, and SNAPC4; however, the data have been mostly limited to Caucasian and East Asian ethnicities, with no replications in Iranian population.
IL1R2 gene is located at chromosome 2q12, which its product, IL1 receptor type 2, inhibits IL1 activity by acting as a decoy target for IL1 [4]. In the total of population, IL1 R2 SNP rs2310173 was not associated with AS, which is in line with the findings of Han Chinese population [20]. However, we found that IL1 R2 genotype GT was mildly protective in HLA-B27 status.
We observed that ANTXR2 (rs4333130) was significantly associated with AS risk in Iranian patients, which is in line with patients from the USA and UK [3]. However, it is different from the findings of Han Chinese population [3, 20]. ANTXR2 is located at chromosome 4q21 and encodes a receptor for anthrax toxin, and its protein binds to type IV collagen and laminin, which suggests the role of ANTXR2 in extracellular matrix adhesion. While the expression of ANTXR2 has been found to be non-different between AS patients and healthy controls [9], we observed that genotype CT of ANTXR2 rs4333130 exhibit significantly higher pain and disease activity scores. These findings have to be investigated in other molecular dimensions to provide sufficient evidence for the pathogenic role of ANTXR2.
We discovered that CARD9 is associated with AS only in HLA-B27-negative Iranian AS patients. These findings guide us toward the hypothesis that different immunologic pathways are operative in pathogenesis of AS in HLA-B27-negative patients in comparison with HLA-B27-positive ones. The product of CARD9 is an adaptor molecule that incorporates with other molecules and transduces signaling to the canonical NFκB pathway [4]. Actually CARD9 plays a key role in the IL17–IL23 pathway, signaling through NFκB to induce production of TNF, IL6 and IL23 (but not IL12), and differentiation of T cells secreting IL17 and IL23 [21]. CARD9 gene is located on chromosome 9q34, which its association with AS susceptibility was discovered in GWAS studies [3, 9] and was confirmed in replication study of UK population [22].
The mechanisms underlying relatively low HLA-B27 positivity of Iranian population is not exactly found. The differences in HLA-B27 frequencies in various ethnicities have been previously observed. For example, HLA-B27 does not exist in African blacks of unmixed ancestry and is present only in 8 % of white and 2–4 % of the American black population [23]. HLA-B27 is positive in healthy Iranian population to the extent 3.3 % (refer to Iran Royan Cord Blood Bank of 15,600 healthy blood donors, http://www.allelefrequencies.net/pop6001c.asp?pop_id=2813). Moreover, another study showed that only 3.95 % of normal Iranian individuals in Isfahan (a large city in central Iran) are positive for HLA-B27 [24]. Also less than 60 % of American black patients are positive for HLA-B27 [23]. It should be noted that variations in HLA-B27 subtypes and existence of race-specific HLA-B27 subtypes might be the other cause of these differences. Therefore, it is highly suggested for future studies to investigate the presence of specific HLA-B27 subtypes in Iranian population. Altogether, the fact that a higher percent of Iranian AS patients are HLA-B27 negative (≈25 %) [6, 25–27] as compared to other populations (≈10 %) warrants studying genes outside MHC as potentially attributed markers to AS pathogenesis. Our result regarding the association of CARD9 rs4077515 with HLA-B27-negative AS might intrigue the initiative molecular studies to better elucidate the enigmatic pathogenesis of AS.
Also we found no associations between SNAPC4 and AS, which is not in line with the findings of Han Chinese population [11]. Actually the associations of SNAPC4 and AS rests upon the hypothesis that CARD9 (associated with AS) is in LD with SNAPC4. However, because a different SNAPC4 SNP (rs11145835) is studied in Han Chinese AS patients, we cannot conclude these data are paradoxical.
Conclusion
In summary, we found significant associations between ANTXR2 (rs4333130) and AS, regardless of HLA-B27 status. Moreover, clinical disease severity scores (BASDAI and BASFI) and pain score were higher in ANTXR2 rs4333130 CT genotype. We observed that CARD9 and IL1 R2 SNPs are only associated with HLA-B27-negative AS. These findings support the role of non-MHC pathogenic pathways in susceptibility to AS and warrants more comprehensive molecular studies focusing on these non-MHC pathways for developing novel therapeutic strategies.
References
Dougados M, Baeten D (2011) Spondyloarthritis. Lancet 18(377):2127–2137
Huang J, Li C, Xu H, Gu J (2008) Novel non-HLA-susceptible regions determined by meta-analysis of four genomewide scans for ankylosing spondylitis. J Genet 87:75–81
Reveille JD, Sims AM, Danoy P et al (2010) Genome-wide association study of ankylosing spondylitis identifies non-MHC susceptibility loci. Nat Genet 42:123–127
Reveille JD (2012) Genetics of spondyloarthritis—beyond the MHC. Nat Rev Rheumatol 8:296–304
Chen B, Li D, Xu W (2013) Association of ankylosing spondylitis with HLA-B27 and ERAP1: pathogenic role of antigenic peptide. Med Hypotheses 80:36–38
Nicknam MH, Mahmoudi M, Amirzargar AA et al (2008) Determination of HLA-B27 subtypes in Iranian patients with ankylosing spondylitis. Iran J Allergy Asthma Immunol 7:19–24
Mahmoudi M, Jamshidi AR, Amirzargar AA et al (2012) Association between endoplasmic reticulum aminopeptidase-1 (ERAP-1) and susceptibility to ankylosing spondylitis in Iran. Iran J Allergy Asthma Immunol 11:294–300
Burton PR, Clayton DG, Cardon LR et al (2007) Association scan of 14,500 nonsynonymous SNPs in four diseases identifies autoimmunity variants. Nat Genet 39:1329–1337
Evans DM, Spencer CC, Pointon JJ et al (2011) Interaction between ERAP1 and HLA-B27 in ankylosing spondylitis implicates peptide handling in the mechanism for HLA-B27 in disease susceptibility. Nat Genet 43:761–767
Haroon N, Tsui FW, Chiu B, Tsui HW, Inman RD (2010) Serum cytokine receptors in ankylosing spondylitis: relationship to inflammatory markers and endoplasmic reticulum aminopeptidase polymorphisms. J Rheumatol 37:1907–1910
Ma X, Liu Y, Zhang H et al (2014) Evidence for genetic association of CARD9 and SNAPC4 with ankylosing spondylitis in a Chinese han population. J Rheumatol 41:318–324
van der Heijde D, van der Linden S, Bellamy N, Calin A, Dougados M, Khan MA (1999) Which domains should be included in a core set for endpoints in ankylosing spondylitis? Introduction to the ankylosing spondylitis module of OMERACT IV. J Rheumatol 26:945–947
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A (1994) A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 21:2286–2291
Calin A, Garrett S, Whitelock H et al (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 21:2281–2285
Jones SD, Porter J, Garrett SL, Kennedy LG, Whitelock H, Calin A (1995) A new scoring system for the Bath Ankylosing Spondylitis Metrology Index (BASMI). J Rheumatol 22:1609
Bidad K, Fallahi S, Mahmoudi M et al (2012) Evaluation of the Iranian versions of the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), the Bath Ankylosing Spondylitis Functional Index (BASFI) and the Patient Acceptable Symptom State (PASS) in patients with ankylosing spondylitis. Rheumatol Int 32:3613–3618
Roe BA, Crabtree JS, Khan AS (editors) (1995) Methods for DNA isolation. Part III. In: Protocols for recombinant DNA isolation, cloning, and sequencing [Internet edition], pp 2488–2498. University of Oklahoma, Norman, New York: Wiley; 1996. Available from: http://www.genome.ou.edu/protocol_book/protocol_index.html; also available in paper copy as: DNA isolation and sequencing
Balding DJ (2006) A tutorial on statistical methods for population association studies. Nat Rev Genet 7:781–791
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B (Methodol) 57:289–300
Chen C, Zhang X, Wang Y (2012) ANTXR2 and IL-1R2 polymorphisms are not associated with ankylosing spondylitis in Chinese Han population. Rheumatol Int 32:15–19
LeibundGut-Landmann S (2007) Syk- and CARD9-dependent coupling of innate immunity to the induction of T helper cells that produce interleukin 17. Nat Immunol 8:630–663
Pointon JJ, Harvey D, Karaderi T et al (2010) Elucidating the chromosome 9 association with AS; CARD9 is a candidate gene. Genes Immun 11:490–496
Khan MA (1978) Race-related differences in HLA association with ankylosing spondylitis and Reiter’s disease in American blacks and whites. J Natl Med Assoc 70:41–42
Fouladi S, Adib M, Salehi M, Karimzadeh H, Bakhshiani Z, Ostadi V (2009) Distribution of HLA-B*27 alleles in patients with ankylosing spondylitis in Iran. Irani J Immunol IJI 6:49–54
Nicknam MH, Mahmoudi M, Amirzargar AA, Jamshidi AR, Rezaei N, Nikbin B (2009) HLA-B27 subtypes and tumor necrosis factor α promoter region polymorphism in Iranian patients with ankylosing spondylitis. Eur Cytokine Netw 20:17–20
Nicknam M, Ganjalikhani Hakemi M, Jamshidi A, Khosravi F (2005) Association between HLA-B27 antigen and ankylosing spondylitis in Iranian patients. Hakim J 8:29–34
Fallahi S, Mahmoudi M, Nicknam MH et al (2013) Effect of HLA-B* 27 and its subtypes on clinical manifestations and severity of ankylosing spondylitis in Iranian patients. Iran J Allergy Asthma Immunol 12:321–330
Acknowledgments
This work was part of a Master of Science thesis and was generously supported by the grant (Grant No: 92-01-4121420) from the deputy of research of Tehran University of Medical Science (TUMS).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
There is no conflict of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Momenzadeh, P., Mahmoudi, M., Beigy, M. et al. Determination of IL1 R2, ANTXR2, CARD9, and SNAPC4 single nucleotide polymorphisms in Iranian patients with ankylosing spondylitis. Rheumatol Int 36, 429–435 (2016). https://doi.org/10.1007/s00296-015-3391-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-015-3391-1