Abstract
The aim of this study was to assess validity of the fibromyalgia survey questionnaire (FSQ) and polysymptomatic distress scale (PSD) in an Iranian population. We also sought to classify the severity levels of fibromyalgia (FM) symptoms according to the PSD scale. Participants were divided into FM and non-FM chronic pain disorder groups according to expert physician diagnosis. Patients in both groups answered to Persian-translated version of FSQ, fibromyalgia impact questionnaire (FIQ) and Short-Form-12 (SF-12). Both 1990 ACR criteria and FSDC were assessed in participates of two groups. Internal consistency and construct validity were evaluated. There was good internal consistency measured by Cronbach’s alpha (0.814 for FSQ). FSQ and its subscales correlated significantly with FIQ scores and SF-12 subscales, indicating acceptable construct validity. The concordance rates of FSQ with 1990 ACR criteria and expert diagnosis were 61.2 and 75.7, respectively (convergence validity). The mean score of PSD and its components in FM group were significantly more than in control groups (discriminative validity). Using lower PSD score cutoff (≥8.5) for the diagnosis of fibromyalgia appeared to be the most effective approach in our population. ROC analysis of the PSD scores revealed 8.5–11.5, 11.5–15 and more than 15, respectively, as a mild, moderate and severe FM. Persian version of FSQ was a valid instrument for application in survey research among Iranian patients with chronic pain disorders. The current study revealed that PSD could be used as a valid tool for assessment of symptoms intensity regardless of fibromyalgia diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of the 2010 American College of Rheumatology (ACR) fibromyalgia criteria and their modification for survey research presents an opportunity to conduct population-based research relating to fibromyalgia without the requirement for tender point ascertainment included in 1990 ACR criteria [1, 2]. The modified 2010 diagnostic criteria incorporate the locations of body pain as measured by the Widespread Pain Index (WPI) and the associated symptom severity (SS) score of fatigue, unrefreshing sleep, cognitive complaints and somatic symptoms [1, 3]. It, also called as fibromyalgia survey diagnostic criteria (FSDC), was developed in a longitudinal study of patients of the National Data Bank for Rheumatic Diseases by eliminating the physician’s estimate of the extent of somatic symptoms and substituting the sum of three specific self-reported symptoms. So, all the modified 2010 ACR items can be obtained by self-administration without requirement for an examiner. Fibromyalgia survey questionnaire (FSQ) which was derived from this criterion included 0–19 WPI and 0–12 symptom severity (SS) score. This questionnaire can be administered in survey research where the use of interviews and examination to evaluate the tender points or detailed somatic symptoms, which are as the parts of 1990 or 2010 ACR criteria, respectively, would be troublesome. Patients satisfy the FSDC if they meet the following two conditions: (1) WPI_7/19 pain sites and SS score_5/12 or WPI between 3 and 6/19 and SS score_9/12; and (2) symptoms have been present at a similar level for at least 3 months [3]. The patient does not have another disorder that would otherwise sufficiently explain the pain. The conditions 1 and 2 can be assessed by FSQ [1, 3].
Additionally, the sum of the WPI and SS score provides a 0–31 scale that is known as the “fibromyalgianess scale” or “polysymptomatic distress scale” (PSD). It was shown that the score more than 13 best separated criteria positive and criteria negative patients [1]. This scale can be applied directly to fibromyalgia severity within FM-diagnosed patients, and it also can be used in different rheumatic diseases as a measure of physical and psychological symptom intensity without regard to fibromyalgia diagnosis [1].
The FSQ and the PSD have been validated in various languages such as English, Japanese, Spanish, German and French [4–8]. It does not validate into Persian language thus far. The current study has three objectives: [1] to validate the Persian version of the FSQ and the PSD, (2) to assess concordance rates of the FSQ and the PSD with expert diagnosis and the 1990 ACR criteria and (3) to classify PSD scores of fibromyalgia patients into mild, moderate and severe levels of impacts of disease according to FIQ scores.
Methods
Design and subjects
Participates of the study were recruited from six clinics including two teaching hospital rheumatology clinics [Hazrat-e-Rasoul Akram General Hospital affiliated to Iran University of Medical sciences (IUMS) and Razi General Hospital affiliated to Guilan University of Medical Sciences (GUMS)], three private rheumatology clinics and Medical Laser Research Center, Iranian Center for Medical Laser (ICML) affiliated to Academic Center for Education, Culture and Research (ACECR). All of these locations were tertiary centers of care.
All consecutive subjects of study were enrolled from September 2011 to April 2012 and were divided into two groups: FM and non-FM chronic pain groups. For the sake of avoiding confounding factors, we selected only female patients in both groups. Patients with established or new diagnosis of fibromyalgia were eligible in FM group. Patients with non-FM chronic pain group were female patients with a painful non-inflammatory rheumatic condition such as osteoarthritis, periarthritis and regional pain syndromes, who had no concurrent diagnosis of FM at the time of enrollment.
The diagnosis of patients in both groups was made by three rheumatologists who had experience in diagnosis and management of chronic pain and fibromyalgia.
Individuals were excluded if they had the age under 18 years or greater than 65 years or they had systemic inflammatory rheumatic disease, cultural or educational barriers to cooperate, acute or known confounding medical illness (such as malignancy, pathologic fracture, disabling medical condition) at the time of enrollment, pregnancy and any non-rheumatic cause of pain.
All subjects were asked to fill out their demographic characteristics (including age, marital status and habitancy) and the study’s questionnaires which included three questionnaires: Short-Form-12 (SF-12), Fibromyalgia Impact Questionnaire (FIQ) and Persian-translated version of FSQ. All patients were observed by a study assistant. The assistant observed the participants to answer all questionnaires and offered help if persons did not understand the meaning of questions.
After documentation of the information, patients were assessed by dolorimeter for evaluation of tender point counts. Tender points were identified by applying dolorimeter (Force DialTM FDK20, Wagner, Instrument, EFFEGI, Italy) on each of known anatomical locations. Four assessors were trained to correctly perform dolorimetery assessment and satisfied inter-observer agreement level. Tenderness at any point was considered present if some involuntary reaction of patients to pain was observed when its pressure was lower than 4 kg/cm, the number of these tender points was considered as tender point count (TPC). So, all participants underwent both the 1990 ACR classification criteria and fibromyalgia survey diagnostic criteria (FSDC).
Written informed consent was obtained from all the patients. This study was approved by the Ethics Committee of Guilan University of Medical Sciences.
Questionnaires
Medical outcome survey: Short-Form-12 (SF-12)
Health status and quality of life were assessed by using the validated Persian version 1 of short-form health survey (SF-12) [9] that includes two main domains: the physical component score (PCS) and the mental component score (MCS), and eight scales for assessing eight dimensions: physical functioning, physical role, social role, emotional role, bodily pain, general health, vitality and mental health. Scores range from “0 to 100” where “0” indicates the worst condition and “100” indicates the best possible condition.
Fibromyalgia Impact Questionnaire (FIQ)
The validated version of FIQ [10] is a specific instrument assessing disease impact on daily living in fibromyalgia patients. This instrument measures “physical functioning,” “overall impact” (missed days of work and job difficulty) and “symptoms” (depression, anxiety, morning tiredness, pain, stiffness, fatigue and well-being over the past week). The maximum score for the FIQ is 100, with higher values indicating greater severity. In the severity analysis, a FIQ total score from 0 to <39 was found to represent a mild effect, ≥39 to <59 a moderate effect and ≥59–100 a severe effect [11].
Persian-translated version of fibromyalgia survey questionnaire (FSQ-P)
Two bilingual medical doctors included one rheumatologist and one internist translated original version of FSQ into Persian language. Afterward, the instrument was translated back into English by a bachelor of biological sciences. Finally, two English versions were compared in order to ensure the conceptual and linguistic equivalence.
FSQ consists of two components: WPI and symptom severity (SS) score. The WPI includes 19 pain sites (jaws, shoulders, upper arms, lower arms, hips, upper legs, lower legs, neck, chest, upper back, lower back and abdomen). It is also possible to determine from the WPI pain sites whether a patient satisfies the ACR 1990 widespread pain criterion.
The SS score included three major symptoms (fatigue, trouble thinking or remembering and waking up tired [unrefreshed]), which can be coded 0–3 (0_no problem; 1_slight or mild problems; 2_moderate, considerable problems; and 3_severe, continuous, life-disturbing problems), and three additional symptoms (pain or cramps in lower abdomen, depression, headache), which can be coded as present (1) or absent (0) (total subscore 0–3). These three items are surrogates for the somatic symptom burden item of the ACR 2010 criteria. The SS score ranges from 0–12.
Subjects satisfy the fibromyalgia survey diagnostic criteria if they meet the following three conditions: (1) WPI_7/19 pain sites and SS score_5/12 or WPI between 3–6/19 and SS score_9/12; (2) symptoms have been present at a similar level for at least 3 months; and (3) the patient does not have another disorder that would otherwise sufficiently explain the pain. The conditions 1 and 2 can be assessed by the FSQ in survey studies. In addition, sum of the WPI and the SS score constitutes the polysymptomatic distress scale or PSD scale, indicator of severity of disease symptoms [1, 3].
Validation methods and statistical analysis
Differences between groups in demographic and clinical characteristics were calculated with the Student’s t test and Chi-square test.
Reliability was analyzed by internal consistency. Internal consistency was assessed by Cronbach’s alpha coefficient. The coefficient value more than 0.7 was considered acceptable.
Construct validity was analyzed by convergent and discriminant validity. For assessing convergent validity, the PSD was compared with the FIQ, TPC, FIQ, fatigue scale, FIQ pain scale and the SF-12 domains by Spearman correlation coefficient analysis. It was a strong correlation if r was higher than 0.60; moderate correlation if r was between 0.30 and 0.60; and small correlation if r was lower than 0.30. P values less than 0.05 were considered significant.
For assessing discriminant validity, the PSD scores and its subscales were compared between FM group and no FM group by Mann–Whitney U test analysis.
Using receiver operator characteristic (ROC) analyses and area under the curve (AUC), we determined sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (PLR), negative likelihood ratio (NLR) and accuracy rate and a range of other cutoff points to see whether any other cutoff score would generate better test characteristics than the one defined by Wolfe et al. and to determine best cutoff for the FS scale in our patient population comparing the group of patients with FM and control subjects.
All statistical tests were two-tailed, and P values <0.05 were considered significant. Statistical analysis was performed using SPSS for Windows version 17.0; SPSS, Chicago, IL, USA.
Results
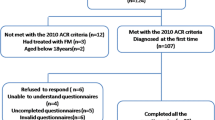
From a total of 269 subjects, six participates were excluded because of missing data. Remaining 263 patients consisting of 169 fibromyalgia (FM) patients and 94 non-fibromyalgia chronic pain (non-FM) patients were enrolled. All participates were female and aged 18–80 (mean 42 ± 11) in FM patients and 19–75 (mean 48 ± 11) in non-FM patients, with significant difference in two groups (P ≤ 0.05). No significant statistical difference was found between two groups with respect to marital status and habitancy (P ≤ 0.05).
In FM patients group, FIQ total, function, overall and symptom values represented as mean ± SD were 60.86 ± 17.72, 5.53 ± 5.12, 6.97 ± 3.04 and 2.90 ± 3.02, respectively, and the mean of TPC, fatigue FIQ scales and pain FIQ scales is 16 ± 3, 7 ± 2 and 7 ± 2, respectively.
In non-FM patients group, FIQ total, function, overall and symptom values represented as mean ± SD were 36.96 ± 15.97, 3.09 ± 1.78, 4.03 ± 3.49 and 2.24 ± 3.32, respectively, and the mean of TPC, fatigue FIQ scales and pain FIQ scales is 10 ± 4, 4 ± 3 and 6 ± 3, respectively.
The internal consistency was assessed. Cronbach’s alpha of FSQ-P components including SS score and PSD was 0.501 and 0.814, respectively.
Spearman’s correlation coefficients between subscales of the FSQ-P and other measures were calculated for testing of construct validity (Tables 1, 2). As could be seen, the FSQ-P and its subscales correlated significantly with all the FIQ scores (total, overall and symptom scores) and the SF-12 and its subscales except function domain of FIQ and TPC.
The diagnosis of fibromyalgia according to FSQ-P was established in 110 of 172 FM patients and three of 96 non-FM patients. In addition, 94.18 percentage of patients in FM group and 44.79 of patients in non-FM group (based on expert idea) met the 1990 ACR criteria. The concordance rates of the FSQ-P and the PSD scale with expert opinion were calculated (Table 3). Likewise, the concordance rates of the FSQ-P and the PSD with 1990 ACR criteria were 61.2 and 65.3 %, respectively.
The sensitivity, specificity, PPV, NPV, positive and negative likelihood ratio of FSQ-P or PSD as the diagnostic tools for comparison of the FM group with non-FM subjects are shown in Table 3.
The mean scores of WPI, SS score and PSD scale were 8.05 ± 4.08, 7.34 ± 2.12 and 15.39 ± 5.43, respectively, in FM patients group and were 2.21 ± 2.39, 3.32 ± 2.19 and 5.55 ± 3.63, respectively, in non-FM patients group. Mann–Whitney U test revealed that mean score of PSD and its components in FM group were significantly more than in control groups (significant at the 0.01 level). These findings indicated that the current scale had valuable discriminant validity.
Receiver operator characteristic (ROC) analysis showed that the best cutoff point of PSD scale with maximal AUC was 8.5 in Iranian patients, resulting in 91.2 % sensitivity and 85.3 % specificity. Using FIQ as the gold standard for illness severity index, ROC analysis also revealed 8.5–11.5, 11.5–15 and more than 15, respectively, as a mild, moderate and severe FM.
Discussion
Our study revealed that Persian version of FSQ was a valid instrument which could be applicable in survey research in Iranian population. Our result also showed that the PSD could be used as a valid tool for assessment of physical and psychological symptoms intensity in Iranian chronic pain patients regardless of fibromyalgia diagnosis. We defined mild, moderate and severe symptom intensity scales in fibromyalgia patients based on PSD for the first time from 2010 modified fibromyalgia criteria creation.
In developing the 2010 ACR criteria, the investigators sought to remove the tender points examination from the new criteria and incorporated associated fibromyalgia symptoms as somatic symptoms in this criteria beyond only body pain provided by 1990 ACR criteria [2, 12]. But, difficulty imposed by requirement of an interviewer for diagnostic purpose led to modification of 2010 ACR criteria. So, FSDC was developed for self-administration. It enables to be used in epidemiologic and clinical studies in different level of care [1]. FSDC and its related questionnaire, FSQ, have been validated in different languages [4–8], but up to the current study, there was no Persian version of this questionnaire.
The current study revealed that FSQ-P had a good level of internal consistency (0.814 and 0.501 for PSD and SS score, respectively) that was acceptable and comparable with other reports. There was not any level of internal consistency of FS (PSD) in Bidari et al. [13] study which validated Persian version of 2010 ACR criteria.
Correlation analysis between PSD, WPI and SS score with disease impact and health status measures was performed. Our findings showed that PSD and SS score correlated more strongly with the FIQ total scores and symptom domain scores rather than function domain scores. This is expected, because the FIQ contains nine physical function items and the PSD and SS scales by design do not contain any such items [14]. When we extracted FIQ pain and fatigue scales from the FIQ, we found the strongest correlation between SS score and FIQ fatigue scale. It is also acknowledged for neuropsychological base of SS score [1, 15]. Furthermore, the PSD scale and its components correlated negatively with mental and physical components of SF-12. This indicated that higher symptom intensity is associated with worse mental health and poor physical and social functioning. In general, PSD and SS score correlated most strongly with mental component of SF-12 (MCS), and correlation of WPI with physical component of SF-12 (PCS) was at least as strong as correlations of WPI with MCS. Although most of correlations are low-to-moderate levels, these findings supported the acceptable construct validity of Persian version of FSQ and PSD.
Notably, tender point count did not correlate with PSD, WPI and SS score. Although TPC was significantly higher in fibromyalgia patients than in non-FM group, the number of tender points did not relate to widespreadness of pain and somatic symptom intensity in our findings. It could be explained with given this fact that the items exploring FSQ do not have a similar nature than dolorimetry and differ from it. Additionally, it seems tenderness to touch can be affected by other various factors, not only pain perception or simple expression somatic symptoms [16]. It is still challenging that tenderness in FM can be explained in terms of a psychiatric condition or a psychosomatic reaction [17].
The current study also confirmed that FSQ-P was an accurate instrument for diagnosis of fibromyalgia in our population and it could separate accurately FM patients from non-FM patients. The percentage of patients meeting the FSQ-P in the fibromyalgia group was significantly higher than that in the non-fibromyalgia group (63.95 vs 3.12 %). The concordance rates of FSQ-P with expert opinion and 1990 ACR criteria were 75.7 and 61.2 %, respectively. Although they are mildly lower than those in Hauser et al. study, they are greater in Usui et al. study [7, 8].
The FSQ-P presented acceptable level of sensitivity and high level of specificity and positive likelihood ratio (63, 96.8 and 20 %) which were greater than in Japanese version of modified 2010 ACR criteria [7]. The high level of positive likelihood ratio indicated that positive FSQ-P occurred in fibromyalgia patients versus non-FM control subjects with the odds ratio equal to 20. Our data also showed that the FSQ-P seems to have lower sensitivity but higher specificity rather than those that found in some reports [5, 7]. It seems that improvement in the sensitivity without significant fall in specificity could be possible with using lower cutoff for satisfying the FSQ in Iranian patients, as had been studied in previous works [7, 13, 18].
The PSD scale was found to be useful and valid to assess severity of fibromyalgia. PSD scores and its related subscales including WPI and SS score were significantly different between FM and non-FM control groups. The PSD scale could differentiate fibromyalgia from other chronic pain disorders with good rates of sensitivity, specificity, PPV and NPV. Setting values ≥8.5 as the cutoff of the PSD scale (instead of 13 in the original study) for a diagnosis of fibromyalgia exhibited to be the most accurate approach, with improvement in sensitivity and without significant change in specificity (91.2 % sensitivity, 85.3 % specificity). In addition, the high concordance rate between PSD score and expert diagnosis (79.9 %) revealed convergence validity of this scale.
We also made use of the PSD scale to define and classify the severity of fibromyalgianess to mild, moderate and severe group, based on FIQ scores. This is the first study which has attempted to classify the fibromyalgia patients according to the PSD score. As we know, the more pain and somatic symptoms were experienced by patients, the higher PSD scores and the greater the disorder impact [1, 19]. But no study has defined the categories of severity of the PSD, previously. In our population, we defined 8.5–11.5, 11.5–15 and more than 15, respectively, as a mild, moderate and severe FM. Although the median score among modified ACR 2010 criteria positive patients in Wolf et al. [1] study was 19, a value that was suggested to be a benchmark for FM severity, Wolf study did not provide any level of severity of the PSD scale. It must be noted that lower median PSD score among our patients (15.4) and lower severity limits could be explained by cross-cultural differences in expression or the rating of symptoms. It remains to be clarified whether this severity level classification could be targeted in clinical or research setting to evaluation of the treatment response or outcome of the disorder.
There are some limitations in the current study. The patients in FM group were a little younger than the patients in non-FM group (42 ± 11 vs 48 ± 11) which does not seem to be clinically significant. Moreover, only female patients were recruited, and therefore, the results of this study cannot be generalized to men with FM. Additionally, we did not evaluate our patients in a primary care setting; thus, they probably do not reflect the general population of FM patients. Moreover, it also needs to be underscored that in this study, mood disorders were not evaluated in both groups, and they might have influenced PSD scores. It should be taken into account that virtually every type of psychiatric illness has been found to be more common in fibromyalgia than in other chronic pain disorders, and these disorders could be affected in the assessed measures. But this issue had not been provided in most previous validation studies including original modified 2010 ACR validation study. Furthermore, testing of the test–retest reproducibility was not performed in our study, and we used just internal consistency of FSQ components for reliability assessment.
We found several small-to-moderate-sized correlations of FSQ-P components with FIQ and SF-12 subscales. Although the amount of correlations was lower than in the original study [1], it is important to note that these correlations were comparable with French and Spanish studies [4, 6].
In summary, we found Persian version of FSQ as a valid instrument for application in survey research among Iranian patients with chronic pain disorders. Although this tool was validated in tertiary level of care, it has the potential to become the standard measure for fibromyalgia survey in epidemiologic study in Persian-speaking population. Furthermore, we showed the PSD as the representation of dimensional or continuum nature of fibromyalgia was a valid tool for assessing symptom severity both in Iranian FM and non-FM patients. Using lower PSD score cutoff (≥8.5) for the diagnosis of fibromyalgia appeared to be the most effective approach in our population. Additionally, for the first time from creation of modified 2010 ACR criteria, we defined the severity levels of the PSD scale with using FIQ scores. It remains to be found whether classifying the PSD severity could be considered as a useful method for assessing treatment response or outcome in clinical or research situations.
References
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Hauser W, Katz RS et al (2011) Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR preliminary diagnostic criteria for fibromyalgia. J Rheumatol 38(6):1113–1122
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P et al (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 62(5):600–610
Wolfe F, Brahler E, Hinz A, Hauser W (2013) Fibromyalgia prevalence, somatic symptom reporting, and the dimensionality of polysymptomatic distress: results from a survey of the general population. Arthritis Care Res 65(5):777–785
Carrillo-de-la-Peña MT, Triñanes Y, González-Villar A, Romero-Yuste S, Gómez-Perretta C, Arias M et al (2015) Convergence between the 1990 and 2010 ACR diagnostic criteria and validation of the Spanish version of the fibromyalgia survey questionnaire (FSQ). Rheumatol Int 35(1):141–151
Ferrari R, Russell AS (2013) A questionnaire using the modified 2010 American College of Rheumatology criteria for fibromyalgia: specificity and sensitivity in clinical practice. J Rheumatol 40(9):1590–1595
Fitzcharles MA, Ste-Marie PA, Panopalis P, Menard H, Shir Y, Wolfe F (2012) The 2010 American college of Rheumatology fibromyalgia survey diagnostic criteria and symptom severity scale is a valid and reliable tool in a French speaking fibromyalgia cohort. BMC Musculoskelet Disord 13:179
Usui C, Hatta K, Aratani S, Yagishita N, Nishioka K, Kanazawa T et al (2013) The Japanese version of the modified ACR preliminary diagnostic criteria for fibromyalgia and the fibromyalgia symptom scale: reliability and validity. Mod Rheumatol 23(5):846–850
Winfried H, Eva J, Brigitte E-M, Mechthild G, Hedi K-B, Franz P et al (2012) Validation of the fibromyalgia survey questionnaire within a cross-sectional survey. PLoS One 7(5):e37504
Montazeri A, Vahdaninia M, Mousavi SJ, Omidvari S (2009) The Iranian version of 12-item short form health survey (SF-12): factor structure, internal consistency and construct validity. BMC Public Health 9:341
Bidari A, Hassanzadeh M, Mohabat MF, Talachian E, Khoei EM (2014) Validation of a Persian version of the fibromyalgia impact questionnaire (FIQ-P). Rheumatol Int 34(2):181–189
Bennett RM, Bushmakin AG, Cappelleri JC, Zlateva G, Sadosky AB (2009) Minimal clinically important difference in the fibromyalgia impact questionnaire. J Rheumatol 36(6):1304–1311
Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL et al (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis Rheumatol 33(2):160–172
Bidari A, Hassanzadeh M, Ghavidel Parsa B, Kianmehr N, Kabir A, Pirhadi S et al (2013) Validation of the 2010 American College of Rheumatology preliminary diagnostic criteria for fibromyalgia in an Iranian population. Rheumatol Int 33(12):2999–3007
Bennett R (2005) The fibromyalgia impact questionnaire (FIQ): a review of its development, current version, operating characteristics and uses. Clin Exp Rheumatol 23(5 Suppl 39):S154–S162
Wolfe F (2010) New American College of Rheumatology criteria for fibromyalgia: a twenty-year journey. Arthritis Care Res 62(5):583–584
Bennett RM, Goldenberg DL (2011) Fibromyalgia, myofascial pain, tender points and trigger points: splitting or lumping? Arthritis Res Ther 13(3):117
Wolfe F (1997) The relation between tender points and fibromyalgia Symptom variables: evidence that fibromyalgia.Is not a discrete disorder in the clinic. Ann Rheum Dis 56:268–271
Katsuhiro T (2012) Difference of fibromyalgia symptom scale between the Japanese version of the 2010 ACR preliminary diagnostic criteria for fibromyalgia and the modification of the ACR preliminary diagnostic criteria for fibromyalgia. Mod Rheumatol 22:316
Wolfe F (2009) Fibromyalgianess [editorial]. Arthritis Rheum 61:715–716
Acknowledgments
The authors thank all the colleagues at the Guilan University of Medical Sciences, Rasht, Iran, who were coordinate in this research.
Funding
The source of Funding is Guilan University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bidari, A., Ghavidel-Parsa, B., Amir Maafi, A. et al. Validation of fibromyalgia survey questionnaire and polysymptomatic distress scale in a Persian population. Rheumatol Int 35, 2013–2019 (2015). https://doi.org/10.1007/s00296-015-3340-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-015-3340-z