Abstract
To evaluate initial glucocorticoid (GC) therapy in patients with rheumatoid arthritis (RA). Six hundred sixty-nine patients with early RA were followed for 2 years in the multicenter “Course And Prognosis of Early Arthritis” cohort. Treatment was applied according to routine care. Assessments included disease activity (DAS28), disability Hannover Functional Status Questionnaire (FFbH), and treatment details. Mixed models, ANCOVA, and logistic regression models were used for statistical analysis. In total, 518 patients (77 %) received oral GCs at baseline; 20 % received a low dose (<7.5 mg prednisolone/day), 22 % received a moderate (7.5–19 mg), and 35 % received a high dose (≥20 mg). In a multivariate logistic regression analysis, higher DAS28 values (OR 1.3) were associated with the use of higher GC doses at baseline (p < 0.001). After adjusting for age, sex, and baseline DAS28 and DMARDs, the patients who started with high-dose GCs had a greater improvement in DAS28 (month 3) and FFbH (month 6, p < 0.001 each). At 2 years, the mean DAS28 remission rates and FFbH values were similar. In all GC groups, the mean dose was tapered to 4 mg/day within 6 months. The reported comorbidities were not increased in patients with high-dose GC therapy. Starting treatment with high-dose GCs led to a better clinical response within 3 to 6 months compared to starting patients on lower dosages. Irrespective of the starting approach, rheumatologists tapered GCs down to a low dose within 6 months. With this strategy, clinical outcomes at 2 years did not differ relevantly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, early diagnosis and fast, effective therapy with the aim of remission are important goals in the treatment of patients with early rheumatoid arthritis (RA) [1]. In the past decade, it has become clear that there is a critical time period during which disease processes can be markedly slowed or even halted [1]. The significance of this “window of opportunity” led to multiple efforts to start medical treatment as soon as possible. A recent meta-analysis has confirmed that a prolonged symptom duration is associated with a radiographic progression and a lower chance of disease-modifying anti-rheumatic drug (DMARD)-free remission [2]. The recommended course of DMARDs in patients with RA has been outlined by the European League Against Rheumatism (EULAR) and in national guidelines that include a sequential therapeutic approach in accordance with the patient’s disease activity and progress [3–6]. Glucocorticoids (GC) are recommended in combination with the first DMARD strategy, but specific advice concerning dosage and duration of GCs is limited. In the update of the EULAR recommendations, the phrasing about GC usage was modified from “low to moderately high doses” to “a low dose for up to 6 months with tapering as rapidly as clinically feasible” [3]. The main reason for the controversial opinions on GC usage is the lack of randomized controlled trials (RCT) that evaluate dosage, duration, and tapering of GCs [7, 8]. Moreover, long-term data on the benefit of GCs as bridging therapy in relation to its toxicity are missing [9]. The differing GC approaches in the DMARD strategy trials range from the COBRA scheme (start with 60 mg prednisolone/day during the first 2 weeks, tapering down weekly to a dose of 7.5 mg/day) [10] to starting with low GC doses (≤10 mg/day) [11, 12]. A single initial intravenous GC dose of 250 mg methylprednisolone was administered in the IDEA trial [13], and repeating intra-articular GC injections were used in the CIMESTRA trial [14]. In the tREACH trial, intramuscular GC administration showed equal efficacy to tapering oral GCs in combination with triple DMARD therapy [15]. Various RCTs provide evidence for increased clinical, structural, and functional efficacy outcomes when low-dose oral prednisolone (≤10 mg/day) is added to methotrexate [11, 12, 16]. However, different oral GC starting doses have not been compared when using similar DMARD therapies [8]. Similar to the heterogeneity of GC starting doses in trial designs, different dosing schemes are used in routine rheumatologic care, depending on the institution, personal experiences, and national recommendations.
Early arthritis inception cohorts have been established to provide data on health care and clinical outcomes in regular rheumatologic settings. While different treatment strategies can only be compared in controlled clinical trials, observational cohorts provide information on the actual treatment patterns and on patient samples that are not limited to trial inclusion criteria. The German Course And Prognosis of Early Arthritis (CAPEA) inception cohort study was conducted to investigate the proportion of patients with early arthritis who achieve remission under the conditions of routine rheumatologic care and to determine the extent of the medical resources used.
The aim of our analysis was to evaluate observational data from the CAPEA cohort in which the GC starting doses are selected by rheumatologists for patients with early RA and to determine how rapidly the patients are tapered down during the first 2 years after symptom onset. The hypothesis of our analysis was that with high initial doses of GCs, more patients would achieve DAS28 remission and functional improvement in the first 2 years after the onset of symptoms.
Patients and methods
Course And Prognosis of Early Arthritis (CAPEA) cohort
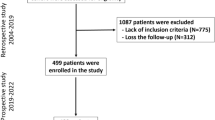
The CAPEA inception cohort study is a prospective, multicenter, non-interventional, observational study on the prognostic value of early symptoms for the development of a chronic course of disease in patients who have had arthritis for <6 months. Between 2010 and 2013, 1,301 patients were consecutively included in 118 rheumatologic institutions in Germany. The participating sites included private practices and outpatient departments of hospitals and university clinics. Patients with early inflammatory arthritis were included, provided that they were observed within 6 months of the first symptoms. They were followed at predetermined intervals (0, 3, 6, 12, 18, and 24 months) using a structured protocol of validated items reflecting treatment, disease activity, function, and treatment response. The patients completed a questionnaire reporting on overall health, function, and disease activity at 0, 6, 12, and 24 months. Medical treatment with DMARDs, GCs, and non-steroidal anti-rheumatic drugs (NSAIDs) was started and adjusted according to standard rheumatologic care and without predefined therapeutic strategies.
Study population
Patients who had arthritis in at least two joints or in one peripheral joint and morning stiffness >30 min for at least 6 weeks until a maximum period of 26 weeks and who gave written informed consent were consecutively included. Patients with confirmed bacterial joint inflammation or gout were excluded. A central ethics vote was obtained from the Ethics Committee of the Charité University Medicine, Berlin, in May 2009.
Data collection
The following items were documented by the rheumatologist at baseline and/or during follow-up: demographic data, laboratory tests, number of swollen and tender joints, disease activity score (DAS28), numerical rating scales (NRS 0–10) regarding disease activity, morning stiffness and functionality, suspected or confirmed diagnosis, comorbidities, current anti-rheumatic medication, and assessment of treatment response. The patients answered numerical rating scales (0–10) regarding global health, pain, morning stiffness, and the Rheumatoid Arthritis Impact of Disease (RAID) score [17]. Disability was reported as a percentage of full function (0–100) using the Hannover Functional Status Questionnaire (FFbH), which is comparable and highly correlated to the Health Assessment Questionnaire (HAQ). The FFbH is widely used in Germany, and FFbH values can be transformed into HAQ values [18]. The diagnosis of RA at 2 years was defined by the physician.
The primary endpoint of CAPEA was defined as the number of patients who achieved clinical remission (DAS28 <2.6) at 2 years. The secondary outcomes included time and use of resources to achieve remission.
Statistical analysis
Logistic regression models were used to determine the risk factors for dropout and comorbidities. Logistic regression analysis with stepwise model selection was used to determine variables associated with baseline GC use. Ordinal logistic regression with stepwise model selection was used to determine variables associated with the dosage of GC in patients who used GC at baseline. Parameters tested were the use of MTX, rheumatoid factor/ACPA positivity, type of practice (solo private practice, single-specialty group practice, multi-specialty group practice, or outpatient department), municipality size of practice site (5–20k, 20–100k, 100–1,000k, >1,000k inhabitants), DAS28, RAID, and the patients’ age and sex. ANCOVA was used to compare the outcome values at year 2 from the different GC doses adjusted for the baseline disease activity. To assess the influence of the initial GC dose on DAS28 and FFbH within 2 years, mixed models with an unstructured covariance structure were used. These models allow including repeated measurements and can handle missing data. Results with a p value of <0.05 were considered to be statistically significant. Statistical analysis was performed using SPSS software, version 19, and SAS, version 9.3.
Results
Of the 1,301 enrolled patients, 1,113 patients (86 %) had a suspected or confirmed diagnosis of RA at the baseline assessment, 7 % were diagnosed with undifferentiated arthritis, and 4 % had other rheumatic disease. Additionally, 46 % fulfilled the 1987 revised ACR, and 60 % fulfilled the 2010 ACR/EULAR criteria. The 2-year follow-up was completed with 773 patients. Of the 773 patients, 669 patients were diagnosed with RA as final diagnosis, but 323 patients with an indication of early RA dropped out during the follow-up. The patients who dropped out were comparable in age and sex to the patients completing the follow-up, but had lower mean erythrocyte sedimentation rates and used GCs less often. Patients with a low DAS28 at baseline, without DMARD therapy and without a probable diagnosis of RA, were significantly more likely to dropout.
For the following analysis, we included all patients who completed the 2-year follow-up and were diagnosed with definite RA at that time (n = 669, Table 1).
Glucocorticoids
Seventy-seven percent of the patients were treated with oral GCs at baseline. 7 % received intra-articular GC injections, primarily in the first year of the observation, and 2.4 % received modified-release GC.
The baseline characteristics by GC starting doses are presented in Table 1.
Practice variation
The frequency of prescribing GCs at baseline varied among the participating rheumatologists. Only rheumatologists with more than five patients were considered in this analysis. Nine (20 %) treated all patients with GCs, 11 (25 %) treated 1–20 % of patients without GCs, 18 (41 %) treated 21–50 % without GCs, and 6 (14 %) treated >50 % of patients without GCs. There was also a variation in the frequency of using high-dose GCs. Fourteen rheumatologists (32 %) treated >50 % of patients with high-dose, 22 (50 %) treated <50 % of patients with high-dose, and 8 (18 %) used no high-dose GCs.
Influencing factors of the GC starting approach
In a multivariate regression analysis, higher DAS28 values and MTX use were associated with the prescription of any GCs at baseline (Table 2). Patient-related factors (sex, age, rheumatoid factor/ACPA positivity, and RAID) were not associated. Variation among the rheumatologists was observed with regard to the practice type. Among the patients who were prescribed GCs at baseline, only DAS28 values (OR 1.3, p < 0.001) were associated with higher GC doses in the multivariate regression analysis.
GC tapering or increase
At 3 months, the mean prednisolone dose had decreased to 5.0 ± 5.8 mg/day in all GC users (median 5.0, IQR 5.0). The tapering of GCs in the CAPEA cohort is presented in Fig. 1. At 6 months, 10 % of the GC users remained on >7.5 mg/day. These patients had the same age, but higher values of ESR, CRP, DAS28, and RAID and lower FFbH values than patients with low-dose or no GCs. At 2 years, 52 % of the patients were GC-free, and 41 % were receiving a dose <5 mg/day; 7 % remained on >5 mg/day.
Of all patients without GC use at baseline, 57 % received GCs later. Thirteen percentage of those received a high dose (20 mg or more) at some visit after baseline. In patients who received ≤7.5 mg GC at baseline, the dosage was increased during follow-up in 19 % of the patients.
DMARD therapy
At 3 months, 82 % of patients were on methotrexate, either in monotherapy or in combination with conventional synthetic DMARDs (csDMARDs, 4 %). At 2 years, 406 patients (62 %) were still on methotrexate monotherapy and 65 (9.8 %) were treated with a combination of csDMARDs. Eighty patients (12 %) received biologics at 2 years, 60 patients in combination with csDMARDs, and 20 patients in monotherapy.
Influence of the GC starting dose on DAS28, FFbH, and morning stiffness
To analyze the clinical outcomes with respect to the GC starting dose, only GC-naïve patients at baseline who were followed for at least 6 months were included (n = 643). In the mixed models, dropouts within the 2 years were also included.
The use of high GC doses (≥20 mg prednisolone/day) was associated with higher DAS28, prolonged morning stiffness, and worse FFbH values at baseline (p < 0.001) (Table 3). Until month 3, the mean DAS28 values decreased significantly in all of the GC starting groups. The unadjusted changes in DAS28 (Δ − 2.5), FFbH (Δ + 15), and morning stiffness (Δ − 3.8 on NRS 0–10) within 6 months were most prominent in patients with the initial high-dose GCs.
Influence on remission
Irrespective of the initial GC dose, 40 % of patients achieved DAS28 <2.6 remission at month 6 and at 2 years. In a logistic regression model with age, sex, baseline DAS28, and MTX use as covariates, the initial GC dosage was not predictive for remission after 2 years, which was reached by 40 % of the patients. In this model, the OR to achieve remission was 1.3 (95 % CI 0.7, 2.4) for GC doses <7.5 mg; 1.1 (95 % CI 0.6, 2.2) for doses of 7.5–15 mg, and 1.3 (95 % CI 0.8, 2.2) for doses ≥20 mg GC, compared to no GC use at baseline.
Mixed model analysis
In a mixed model analysis, the influence of the GC starting dose on the DAS28 within the 2 years of observation was analyzed with adjustments for sex, age, baseline disease activity, and use of methotrexate and biologics (Fig. 2a). Regarding DAS28 values, there was a significant influence of the starting dose within 3 months (p < 0.001). At 2 years, patients in the ≥20 mg starting group had a mean DAS28 that was 0.2 points lower than in the other groups (p = 0.02).
In a similar analysis, patients with the baseline high-dose GCs had a significantly higher improvement in physical function between the baseline and month 6 (p < 0.001) (Fig. 2b). However, there was no influence of the GC starting dose on the FFbH after 2 years (p = 0.19).
GC-related comorbidities
The prevalence of physician-reported, potentially GC-related comorbidities, such as hypertension (33 %), cardiovascular disease (5 %), peptic ulcer disease (1 %), and renal dysfunction (1 %), did not increase over the 2 years of observation. Diabetes was prevalent in 7 % of all patients at baseline. Seventeen patients (2.6 %) had incident type 2 diabetes within the 2 years. There was no increased incidence in patients who started with high-dose GCs. Osteoporosis was not reported at baseline and unknown in 44 % of patients at 2 years. For the remaining patients with prevalent osteoporosis (22 %), logistic regression analysis revealed only the age at baseline as an independent predictor (p < 0.001).
Discussion
In the German CAPEA inception cohort, we observed a rapid improvement in functional ability and disease activity within the first 3–6 months after treatment initiation in patients with early RA. This is in agreement with findings from other early arthritis cohorts that also reported considerable functional and DAS28 improvement in the first 6 months after the disease onset [19, 20]. Our cohort is composed of patients from more than 100 rheumatologists in Germany, who performed routine RA therapy according to their preferences. Independent of the first-line DMARD strategy, predominantly methotrexate monotherapy, we noticed a high variability in the selection of the initial GC dose; 77 % of patients were initially treated with oral GCs, and one-third of them received initial doses ≥20 mg prednisolone/day. These findings differ from other cohorts where GCs are used less frequently. In the BARFOT study, 42 % of patients started on GCs [21]. In the CATCH cohort, 42 % were prescribed initial GCs, but only 48 % of them were on oral prednisolone, with 38 % receiving intra-articular or intramuscular GCs. Moreover, only ≤10 mg prednisolone/day was allowed [22]. In the ESPOIR cohort, 45 % received GCs during the first 6 months and 60 % received GCs at least once during a 5-year follow-up [20]. In a further inception cohort from Latin America (GLADAR), where treatment was also allowed according to the rheumatologists’ preferences, 64 % of patients received GCs, but 80 % of those were on ≤10 mg prednisolone/day [23].
In our cohort, the frequency of prescribing GCs at the onset of RA varied among the rheumatologists, both to using GCs in general and to using high-dose GCs. The multivariate analysis showed an influence of the type of rheumatologic facility, but we assume that the training of the rheumatologist may be the most decisive factor for differences in the GC starting approach. Irrespective of these findings, patients with high disease activity and disability at the disease onset were more frequently treated with high-dose GCs. Patients who started on MTX were also more frequently treated with GCs which can be explained by the bridging approach of GCs in patients with definite inflammatory arthritis. The impaired clinical status of these patients was stabilized within 6 months. Especially considering the functional response within the first 6 months, these patients appeared to benefit from starting with high-dose GCs. The results from ESPOIR showed a worse outcome at years 3 and 5 in patients with persistent moderate disease activity during the first year, indicating a possible advantage of early intensive intervention [20]. Regarding the outcomes at 2 years, we only found a clinically non-relevant impact of starting with high-dose GCs on DAS28 values and patients starting with low-dose GCs achieved equal DAS28 remission rates and functional capacity.
The current EULAR recommendations on the management of moderate to high GC doses in patients with rheumatic diseases report a lack of randomized trials to evaluate the selection of the appropriate GC starting dosage in patients with RA [7]. However, after debating this point, the current update of the EULAR recommendations on the management of RA advises starting with low doses (<7.5 mg/day) [3]. The current German guidelines adopted the previous recommendation to start at low to moderately high doses [4]. Our results indicate that German rheumatologists used their own discretion in GC-prescribing practices. This seems reasonable given that tapering was rapidly performed. In our cohort, a low dose was achieved within 6 months in most of the patients, irrespective of the initial GC dose. Half of all patients were completely GC-free at 2 years. It is a matter of debate whether very low doses (<3 mg/day) should be imperatively tapered or not. Although the current recommendation advises a 6-month period of low-dose GC concomitant therapy [3], evidence exists for a better radiographic outcome with ongoing low-dose therapy within 2 years [24]. As our radiologic data are incomplete, we did not discuss this topic in our study.
The frequency of GC-related comorbidities at baseline is similar to data from ESPOIR [20], except for one-third of patients with hypertension in our cohort (versus 17 % in ESPOIR). This can be explained in part by the mean age in the ESPOIR cohort (48 years), which is remarkably lower than in our cohort (56 years). We did not observe further increases during the first 2 years. The incident cases of type 2 diabetes showed no association with the initial GC dose. Our data on osteoporosis are limited, and we have no information on osteo-protective medication or on the frequency of infections.
The main limitations of our study are, first, that we have no data on the GC doses between the visits. We looked at the tapering dose during follow-up, but we cannot exclude temporal GC adaptation and, therefore, cannot provide precise cumulative GC doses. Second, as treatment adaptation was performed without predefined strategies, we could not compare GC strategies such as the COBRA scheme versus low-dose therapy. In general, observational data are limited at the point of analysis due to the variety of treatment adaptations. Third, our data on GC-related comorbidities lack sufficient power to exclude adverse effects of high-dose GCs. The strength of our study is that we provide detailed data on the initial use and tapering of GCs in real life from a broad range of rheumatologists in Germany, which is essential for the development of recommendations in the future.
Finally, we noticed that intra-articular GCs and modified-release prednisolone were not used frequently in the German routine rheumatologic care, although both have been successfully used with DMARD therapy in clinical trials [14, 25].
In summary, we observed a large variation in the GC starting doses in the patients with early RA in the German CAPEA cohort. This variation was, in part, explained by different baseline values of disease activity and function and, additionally, by a variation in the use among the rheumatologists. Patients with high initial disease activity and reduced functional status, who started with high-dose GCs, achieved comparably good outcomes. We found no delay in tapering and conclude that German rheumatologists follow the aim of tapering down the GC dose to <7.5 mg/day within 6 months, irrespective of the initial GC dose. With this strategy, clinical outcomes at 2 years did not differ relevantly.
References
Smolen JS, Aletaha D, Machold KP (2005) Therapeutic strategies in early rheumatoid arthritis. Best Pract Res Clin Rheumatol 19(1):163–177
van Nies JA, Krabben A, Schoones JW, Huizinga TW, Kloppenburg M, van der Helm-van Mil AH (2014) What is the evidence for the presence of a therapeutic window of opportunity in rheumatoid arthritis? A systematic literature review. Ann Rheum Dis 73(5):861–870
Smolen JS, Landewe R, Breedveld FC et al (2014) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis 73(3):492–509
Albrecht K, Kruger K, Wollenhaupt J et al (2014) German guidelines for the sequential medical treatment of rheumatoid arthritis with traditional and biologic disease-modifying antirheumatic drugs. Rheumatol Int 34(1):1–9
Singh JA, Furst DE, Bharat A et al (2012) 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 64(5):625–639
NICE (National Institute for Health And Care Excellence) (August 2013) Rheumatoid Arthritis. The management of rheumatoid arthritis in adults. http://www.nice.org.uk/nicemedia/live/12131/43327/43327.pdf. Accessed Aug 2013
Duru N, van der Goes MC, Jacobs JW et al (2013) EULAR evidence-based and consensus-based recommendations on the management of medium to high-dose glucocorticoid therapy in rheumatic diseases. Ann Rheum Dis 72(12):1905–1913
Gaujoux-Viala C, Nam J, Ramiro S et al (2014) Efficacy of conventional synthetic disease-modifying antirheumatic drugs, glucocorticoids and tofacitinib: a systematic literature review informing the 2013 update of the EULAR recommendations for management of rheumatoid arthritis. Ann Rheum Dis 73(3):510–515
Rau R (2014) Glucocorticoid treatment in rheumatoid arthritis. Expert Opin Pharmacother 15(11):1575–1583
Boers M, van Tuyl PJ, van den Broek M, Kostense PJ, Allaart CF (2013) Meta-analysis suggests that intensive non-biological combination therapy with step-down prednisolone (COBRA strategy) may also ‘disconnect’ disease activity and damage in rheumatoid arthritis. Ann Rheum Dis 72(3):406–409
Montecucco C, Todoerti M, Sakellariou G, Scire CA, Caporali R (2012) Low-dose oral prednisone improves clinical and ultrasonographic remission rates in early rheumatoid arthritis: results of a 12-month open-label randomised study. Arthritis Res Ther 14(3):R112
Svensson B, Hafstrom I (2011) Effects on joint destruction and remission, bone turnover and lack of influence on atherogenesis: a review of the BARFOT low-dose prednisolone studies on patients with early RA. Clin Exp Rheumatol 29(5 Suppl 68):S63–S67
Nam JL, Villeneuve E, Hensor EM et al (2014) Remission induction comparing infliximab and high-dose intravenous steroid, followed by treat-to-target: a double-blind, randomised, controlled trial in new-onset, treatment-naive, rheumatoid arthritis (the IDEA study). Ann Rheum Dis 73(1):75–85
Hetland ML, Horslev-Petersen K (2012) The CIMESTRA study: intra-articular glucocorticosteroids and synthetic DMARDs in a treat-to-target strategy in early rheumatoid arthritis. Clin Exp Rheumatol 30(4 Suppl 73):S44–S49
de Jong PH, Hazes JM, Barendregt PJ et al (2013) Induction therapy with a combination of DMARDs is better than methotrexate monotherapy: first results of the tREACH trial. Ann Rheum Dis 72(1):72–78
Bakker MF, Jacobs JW, Welsing PM et al (2012) Low-dose prednisone inclusion in a methotrexate-based, tight control strategy for early rheumatoid arthritis: a randomized trial. Ann Intern Med 156(5):329–339
Gossec L, Paternotte S, Aanerud GJ et al (2011) Finalisation and validation of the rheumatoid arthritis impact of disease score, a patient-derived composite measure of impact of rheumatoid arthritis: a EULAR initiative. Ann Rheum Dis 70(6):935–942
Lautenschlaeger J, Mau W, Kohlmann T et al (1997) [Comparative evaluation of a German version of the Health Assessment Questionnaire and the Hannover Functional Capacity Questionnaire] German. Z Rheumatol 56(3):144–155
Boyd TA, Bonner A, Thorne C et al (2013) The relationship between function and disease activity as measured by the HAQ and DAS28 varies over time and by Rheumatoid factor status in early inflammatory arthritis (EIA). Results from the CATCH Cohort. Open Rheumatol J 7:58–63
Combe B, Rincheval N, Benessiano J et al (2013) Five-year favorable outcome of patients with early rheumatoid arthritis in the 2000s: data from the ESPOIR cohort. J Rheumatol 40(10):1650–1657
Svensson B, Andersson ML, Bala SV, Forslind K, Hafstrom I (2013) Long-term sustained remission in a cohort study of patients with rheumatoid arthritis: choice of remission criteria. BMJ Open 3(9):e003554
McKeown E, Bykerk VP, De Leon F et al (2012) Quality assurance study of the use of preventative therapies in glucocorticoid-induced osteoporosis in early inflammatory arthritis: results from the CATCH cohort. Rheumatology (Oxford) 51(9):1662–1669
Cardiel MH, Pons-Estel BA, Sacnun MP et al (2012) Treatment of early rheumatoid arthritis in a multinational inception cohort of Latin American patients: the GLADAR experience. J Clin Rheumatol 18(7):327–335
Wassenberg S, Rau R, Zeidler H (2011) A dose of only 5 mg prednisolone daily retards radiographic progression in early rheumatoid arthritis-the low-dose prednisolone trial. Clin Exp Rheumatol 29(5 Suppl 68):S68–S72
Buttgereit F, Mehta D, Kirwan J et al (2013) Low-dose prednisone chronotherapy for rheumatoid arthritis: a randomised clinical trial (CAPRA-2). Ann Rheum Dis 72(2):204–210
Acknowledgments
The authors gratefully acknowledge the contribution of the participating patients and the consultant rheumatologists for recruiting and following the patients in the CAPEA cohort. The authors also acknowledge the support of Winicker Norimed in data collection and monitoring and the contributions of Edmund Edelmann, MD, Bad Aibling and Georg Schett, MD, Erlangen as members of the advisory board. Authors received the Support by an unconditional grant from Pfizer, Germany.
Conflict of interest
The authors report grants from Pfizer, Germany, during the conduct of the study; J Callhoff reports personal fees from Pfizer, Germany, outside the submitted work; M. Schneider has nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Albrecht, K., Callhoff, J., Schneider, M. et al. High variability in glucocorticoid starting doses in patients with rheumatoid arthritis: observational data from an early arthritis cohort. Rheumatol Int 35, 1377–1384 (2015). https://doi.org/10.1007/s00296-015-3229-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-015-3229-x