Abstract
Travel restrictions, while delaying the spread of an emerging disease from the source, could inflict substantial socioeconomic burden. Travel-related policies, such as quarantine and testing of travelers, may be considered as alternative strategies to mitigate the negative impact of travel bans. We developed a meta-population, delay-differential model to evaluate a strategy that combines testing of travelers prior to departure from the source of infection with quarantine and testing at exit from quarantine in the destination population. Our results, based on early parameter estimates of SARS-CoV-2 infection, indicate that testing travelers at exit from quarantine is more effective in delaying case importation than testing them before departure or upon arrival. We show that a 1-day quarantine with an exit test could outperform a longer, 3-day quarantine without testing in delaying the outbreak peak. Rapid, large-scale testing capacities with short turnaround times provide important means of detecting infectious cases and reducing case importation, while shortening quarantine duration for travelers at destination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
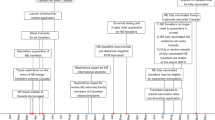
Emerging infectious diseases (EIDs) often render a potential for global spread, which can be facilitated by international transportation, especially by air travel (Findlater and Bogoch 2018). International Air Transport Association (IATA) data indicate that the connectivity of the six most populous countries in the world increased by 57% to 153% between 2009 and 2019 (IATA 2020). Although air travel and transportation have led to substantial gains in social and economic wealth, they have also raised significantly the risk of rapid dissemination of EIDs, particularly air-borne diseases like severe acute respiratory syndrome (SARS), influenza, and most recently SARS-CoV-2 that caused the COVID-19 pandemic (Brownstein et al. 2006; Hollingsworth et al. 2006; Germann et al. 2006). EIDs with serious public health concerns may trigger various interventions and restrictive measures that could interfere with connectivity and movement between populations in addition to measures implemented to quell outbreaks within populations. For example, during the early stages of the COVID-19 pandemic, many international airports implemented screening measures, and later, quarantine and testing strategies for travelers upon arrival. The intensity of these measures varied over time, from lockdowns of cities and countries to travel ban from and to affected regions (Wells et al. 2020, 2022; Vilches et al. 2021; Di Domenico et al. 2020; Alfano and Ercolano 2020; Chinazzi et al. 2020).
Although the effectiveness of travel-related policies may vary with time and geographic location, long-term use of restrictive measures can lead to enormous socioeconomic burdens (Nicola et al. 2020). Furthermore, travel policies would need to adapt over time as the EIDs enter different stages post emergence and their characteristics evolve (Leung et al. 2021). Combining travel restrictions with other public health measures may help minimize the movement disruption between populations. For instance, testing and quarantine were proposed during the COVID-19 pandemic in order to ameliorate transmission with lifting travel restrictions (Wells et al. 2022). However, the impact of travel-related policies depends on the effectiveness of other interventions. For example, low sensitivity of a test during some stages of infection may allow undetected infected individuals to travel and import the disease to another population. Furthermore, duration of quarantine and testing strategies (e.g., at the time of arrival for travelers) could influence the infection rates in a population (Wells et al. 2021, 2022), and may lead to the importation of new types of infection, such as different variants of an EID like SARS-CoV-2.
Understanding the interplay between these interventions and their impact on disease transmission dynamics between populations is critical to optimizing outbreak response policies. Integration of data into modelling frameworks can provide this understanding as demonstrated during the COVID-19 pandemic. For example, a mobility model for the spread of COVID-19 in a meta-population network of over 3200 subpopulations showed that the travel ban enacted in Wuhan in January 2020 had a more remarkable effect on decelerating the international spread than within-China spread (Chinazzi et al. 2020). Furthermore, sustained travel restrictions focusing only on the trips to and from China were suboptimal in the presence of uncontrolled within-community transmission. During the early stages of the pandemic, models demonstrated that there was a significant correlation between the international air connectivity of mainland China and the COVID-19 cases imported globally (Wells et al. 2020). For instance, travel restrictions and border control measures (i.e., screening upon arrival) were effective in averting over 70% of international cases during the first month (Wells et al. 2020), providing more time to devise and implement public health responses. However, airport screening alone was ineffective in controlling the importation due to asymptomatic infection in travelers.
Travel strategies may also be combined with other measures such as testing prior to departure and quarantine upon arrival (Dickens et al. 2020; Molero-Salinas et al. 2022). In this study, we aimed to evaluate the impact of travel-related policies between distinct populations, involving testing and quarantine, by developing a meta-population model that encapsulates the dynamics of disease transmission based on knowledge of SARS-CoV-2 infection. Within this theoretical framework, expressed as a system of delay differential equations, we consider the possibility of leaky quarantine with fixed duration, where infectious travelers can enter the destination population. To identify infectious individuals and reduce onward transmission through isolation, we also consider testing strategies within each population and prior to travel, as well as quarantine upon arrival and testing at exit from quarantine. In addition to discussing the theoretical foundation of the model, we perform simulations using parameter estimates specific to COVID-19 to compare the outcomes of different strategies.
2 The model
To develop our model, we first consider the dynamics of disease transmission within a population. We divide the population into several classes of individuals with epidemiological statuses, including susceptible (S), exposed and infected (E), infectious (I), and recovered (R). This structure is considered within two distinct populations (referred to as meta-population) that are connected only by dispersal (i.e., there is travel between populations). We use subscripts of A and B to represent the epidemiological classes within populations \(P_A\) and \(P_B\), respectively. Our model omits demographics of birth and natural death, and relies on the assumption that the duration of an outbreak is significantly shorter than the average lifespan of individuals. Within each population, we assume that the testing strategy is used to identify infectious individuals. In the context of COVID-19, infectious individuals have different characteristics from showing no symptoms to presenting mild or severe symptoms. To simplify the complexity of our model, we consider only one class of infectious individuals and assume that only a proportion of them may be tested. Those who are tested positive are isolated until recovery, with the assumption that isolation prevents further transmission. A schematic diagram of the model is illustrated in Fig. 1.
Given the introduction of the disease in \(P_A\), we evaluate the effect of travel-related policies on the importation of disease to \(P_B\). We assume that \(P_B\) has a quarantine policy with a fixed duration of \(\tau \) days for all individuals upon arrival. The model includes two discrete switch parameters. The first switch (\(\sigma _1\)), indicates whether there is a policy in \(P_A\) for testing travelers prior to departure for \(P_B\). Individuals who are identified as positive are isolated in \(P_A\) and prohibited from traveling to \(P_B\) until recovery. The second switch (\(\sigma _2\)) relates to the policy for testing travelers at exit from quarantine in \(P_B\). We include the parameter of diagnostic sensitivity for a test to determine the probability of identification (i.e., positive result) for an infected individual. A negative test result for infected individuals is referred to as false-negative, which allows them to travel from \(P_A\) to \(P_B\). A false-negative result for a test at exit from quarantine also provides an opportunity for infection to leak into \(P_B\), leading to further transmission.
2.1 Within-population disease dynamics
Transmission of disease occurs as a result of contacts between susceptible and infectious individuals at a rate denoted by \(\beta \). We assume that infected individuals experience an average duration of \(1/\alpha \) (referred to as the latent period) before becoming infectious. The average duration of infectious period is denoted by \(1/\gamma \), within which transmission can occur if individuals are not tested, or are tested but obtain false-negative results. We use \(\eta \) to represent the proportion of infectious individuals who are tested. This proportion may be affected by the manifestation of clinical disease as well as the testing capacity and prioritization in the population. The diagnostic sensitivity of a test varies over time with the stage of disease. Simplifying this temporal variation to an average, we denote the sensitivity of the test during the latent and infectious periods by \(\psi _{_E}\) and \(\psi _{_I}\), respectively, where \(0<\psi _{_E},\ \psi _{_I}\le 1\). Thus, the probabilities of a false-negative for an infected individual during the latent and infectious periods are \(1-\psi _{_E}\) and \(1-\psi _{_I}\), respectively. The term \(\eta \psi _{I}\) indicates the proportion of infectious individuals who are tested positive after the latent period has elapsed, and therefore isolated. The remaining proportion will continue their infectious period without isolation until recovery. Table 1 provides details of the model variables and parameters in each population.
2.2 Testing prior to travel in \(P_A\)
We consider dispersal rates of \(\delta _{_A}\) and \(\delta _{_B}\) for traveling between \(P_A\) and \(P_B\). In this model, the switch parameter \(\sigma _1=1\) indicates that \(P_B\) requires testing for incoming individuals prior to their departure from the origin (i.e., \(P_A\)), and only those with negative tests are allowed to travel. The control strategies in each population also mandate individuals with a positive test to isolate. Isolated individuals are not allowed to travel before recovery. Other individuals in \(P_A\) who test negative, regardless of their epidemiological status, can travel to \(P_B\).
2.3 Quarantine upon arrival in \(P_B\)
Travel-related policies in \(P_B\) may mandate incoming individuals to quarantine for a duration of \(\tau \) days upon arrival. During quarantine, epidemiological statuses of individuals may change (e.g., becoming infectious while being latent at the time of departure from \(P_A\)). Travelers may require to test before exiting the quarantine to limit the possibility of case importation. However, depending on various factors including testing capacity, an alternative strategy of quarantine with a longer duration may be implemented without testing at exit. We therefore use a switch parameter (\(\sigma _2=1\)) to implement a policy in \(P_B\) for testing individuals at exit from quarantine. Those with a positive test result are isolated and not allowed to freely interact with other individuals in \(P_B\) until recovery. In case of \(\sigma _2=0\) (i.e., no testing at exit from quarantine), or \(\sigma _2=1\) with false-negative test results, infectious individuals can enter \(P_B\) at the end of their quarantine period and may transmit the disease within \(P_B\). This scenario is referred to as the ‘leaky’ quarantine. For simplicity, we do not include specific compartments in the model for quarantine of susceptible or recovered individuals traveling from \(P_A\) to \(P_B\).
2.4 Leaky quarantine in \(P_B\)
There are three possible ways of leakage from quarantine (Fig. 1):
-
L1)
Travelers who enter quarantine in \(P_B\) as exposed and do not progress to the infectious state by the end of their quarantine may enter \(P_B\), either without exit testing or with a false-negative result of exit testing.
-
L2)
Infectious travelers who enter the quarantine with a false-negative test in \(P_A\) may enter \(P_B\) after \(\tau \) days of quarantine, while still being infectious. This includes both cases of no testing or a false-negative result of testing at exit from quarantine.
-
L3)
Travelers who enter quarantine in \(P_B\) as exposed, but become infectious during the quarantine period may enter \(P_B\) as infectious individuals at the end of quarantine if they have not yet recovered. This case also includes both scenarios of no testing, or a false-negative result of testing at exit from quarantine.
We note that individuals who enter quarantine during their infectious period and do not recover during quarantine, or those who exit quarantine while being still in the latent period do not have any change in their epidemiological status. Therefore, the key factors affecting their dynamics are the fixed duration of quarantine and testing at exit from quarantine. For those who have a change in epidemiological status (i.e., becoming infectious during quarantine), the dynamics is also affected by the amount of time elapsed since entering quarantine, which involves a continuous and, hence, distributed delay. We consider these cases to derive the relevant model equations.
2.4.1 Deriving equations in L1 and L2
We begin with the dynamics of travelers who enter quarantine during their latent period (\(E_{qB}\)) upon arrival in \(P_B\). The rate of incoming at time t is \(\delta _{_A}(1-\sigma _1\psi _{_E})E_A(t)\). With an average latent period of \(1/\alpha \), the progression to an infectious state in \(E_{qB}\) depends on the amount of time spent in \(E_A\) before traveling to \(P_B\) and the duration of quarantine. Let e(t, a) be the density of \(E_{qB}(t)\) (Alexander et al. 2008; Arino and Van Den Driessche 2006; Robertson et al. 2018) at time t with respect to a, representing the time since entering quarantine. Thus,
When \(a=\tau \), the quarantine ends and we have
with the boundary and initial conditions:
Using the method of characteristics and solving (1), we obtain
Thus, the dynamics of \(E_{qB}(t)\) can be expressed by
for \( t\ge \tau \). Similarly, one can derive the equation for the dynamics of those who enter quarantine during their infectious period \((I_{q1B}\)) as for \(t \ge \tau \),
2.4.2 Deriving equation in L3
With a fixed duration of quarantine, those who enter quarantine as exposed, \(E_{qB}(t)\), in \(P_B\) may become infectious, \(I_{q2B}(t)\), while still in quarantine at the rate \(\alpha \). Meanwhile, the infectious travelers recover at the rate \(\gamma \). From the time of entering quarantine, \(t_{start}\), to the time of exiting quarantine, \(t_{end}\), each traveler spends \(\tau \) units of time in quarantine, i.e., \(t_{end}-t_{start}=\tau \). It is worth noting that the disease state for part of individuals in \(E_{qB}(t)\) changes at an uncertain point in time during their quarantine. Denoting this time point by \(t_c\), we define the time interval between the start of quarantine and the change of disease state from exposed to infectious by \(\nu =t_c-t_{start}\). The remaining time in quarantine is therefore \(\omega =t_{end}-t_{c}\), with \(\tau =\nu +\omega \).
Let i(t, b) denote the density of \(I_{q2B}(t)\) at time t with respect to age (b) since the change in disease state during quarantine. Thus,
with the boundary and initial conditions:
Using the method of characteristics, we obtain
Denoting the probability density function of \(\omega \) by \(p_\omega \), we have
Taking the derivative of (2) with respect to t gives
We now determine the density function \(p_\omega \). Since quarantine has a fixed duration, the probability density function (\(p_\nu \)) for \(\nu \) can be considered as a “truncated" exponential distribution from 0 to \(\tau \). Thus, the cumulative distribution function for \(\nu \) is expressed by
which gives
Using \(\omega = \tau - \nu \), we obtain
Summarizing the above derivation, yields
where
2.5 Model equations
Here, we present the model as a system of delay differential equations, describing the dynamics of disease transmission in \(P_A\) and \(P_B\) with dispersal:
To further simplify the model for simulations, we convert the distributed delay to a constant delay. To do so, let \(s=t-\omega \). From (5), we get
Differentiating G(t) with respect to t gives:
which reduces to
2.6 Parameterization
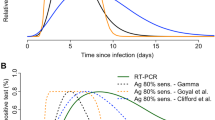
One of the key parameters in the model (6) is the transmission rate \(\beta \). In order to determine this parameter, we rely on estimates of the basic reproduction number (\(\mathcal {R}_0\)) for SARS-CoV-2, defined as the average number of secondary infections caused by an infectious individual in an entirely susceptible population (Diekmann and Heesterbeek 2000). Assuming other parameters are fixed, one can calculate \(\beta \) for a given \(\mathcal {R}_0\) (See Appendix). We consider \(\mathcal {R}_0=2.38\) (Li et al. 2020), with average latent and infectious periods of 2.2 and 5.5 days (Li et al. 2020; Moghadas et al. 2020). For the purpose of simulations, we consider 100,000 individuals in each population, and vary the proportion of infectious cases that are tested (\(\eta \)), the duration of quarantine (\(\tau \)) upon arrival in \(P_B\), in the absence and presence of testing before departure from \(P_A\) and at the exit from quarantine in \(P_B\). Using estimates associated with the temporal diagnostic sensitivity of various tests used during COVID-19 pandemic, we fix the test sensitivity to 5% and 90% during latent and infectious stages of the disease (Wells et al. 2022). Table 2 summarizes parameter values used for model simulations.
3 Results
To assess the effectiveness of travel-related policies on the timing and magnitude of the outbreaks, we assume that the disease is introduced in \(P_A\) and could be imported to \(P_B\) by travelers from \(P_A\) to \(P_B\). Thus, we are interested in quantifying the effect of testing and quarantine on the time and magnitude of the outbreak peak in \(P_B\) based on parameter values used for simulations (Table 2). The initial number of infections in \(P_A\) is 10 introduced in \(E_A\).
3.1 Effect of testing within each population
In the absence of travel-related policies, we simulate the model while varying the proportion (\(\eta \)) of infectious individuals being tested in each population. Not surprisingly, increasing this proportion decelerates the progression of outbreak with reduced magnitude and further delay in the peak (Fig. 2). For example, the peak of incidence in \(P_A\) occurs about 10 weeks into the outbreak with a magnitude of 2581 cases when only 10% (\(\eta =0.1\)) of infected individuals are tested (Fig. 2A). The peak of incidence is further delayed by 4 and 17 weeks when 30% (\(\eta =0.3\)) and 50% (\(\eta =0.5\)) of infected individuals are tested, respectively, with the corresponding magnitudes of 1446 and 397 cases. We observe a similar effect of testing on the number and timing of the outbreak peak in \(P_B\) when the disease is imported. However, we note that because the infection is initially introduced in \(P_A\), there is a delay in the occurrence of an outbreak in \(P_B\), and this delay reduces with increasing dispersal rate \(\delta _{_A}\) (Appendix, Fig. 6). The effect of testing prior to departure from \(P_A\) is negligible on changing the magnitude or timelines of the outbreak in \(P_A\) (Fig. 2B); however, it can further delay the surge of cases in \(P_B\) compared to no testing before travel depending on the proportion of infected individuals who are tested (Fig. 2C, D). For example, when \(\eta =0.5\), testing prior to departure from \(P_A\) delays the outbreak peak in \(P_B\) by 4 weeks compared to the scenario of no testing before travel.
3.2 Effect of quarantine and exit testing
Implementation of quarantine for travelers from \(P_A\) leads to a small delay in case importation and the ensuing outbreak (Fig. 3). However, a longer than 1-day duration of quarantine provides a negligible additional delay in the time of the outbreak peak with minimal change in its magnitude in \(P_B\) (Fig. 3). These characteristics are mainly affected by testing infectious individuals within \(P_B\). Testing prior to departure delays the surge of cases in \(P_B\) as shown in Fig. 2. Simulation show that testing at exit from quarantine results in the largest delay in case importation and the impending outbreak. This delay increases with higher \(\eta \). For example, in the absence of testing at exit from quarantine (i.e., \(\sigma _2=0\)) with a duration of 1 day, the outbreak peak in \(P_B\) occurs about 300 days after the introduction of infection in \(P_A\) with \(\eta =0.5\) (Fig. 3A). When testing at exit from quarantine is implemented (i.e., \(\sigma _2=1\)), the outbreak peak is further delayed by about 30 days (Fig. 3D). This observation remains consistent irrespective of the duration of quarantine. However, with testing at exit from quarantine, a longer quarantine contributes to an additional small delay (i.e., less than 3 weeks) in the outbreak peak (Fig. 3D–F). It is important to note that, despite deceleration of the outbreak and its peak in \(P_B\) using testing and quarantine, the overall attack rates (i.e., the proportion of the population that is infected throughout the outbreak) are the same in the corresponding scenarios (Appendix, Fig. 7).
Incidence of infection in \(P_B\) when quarantine of travelers is implemented upon arrival. Solid and dashed lines correspond to scenarios without and with testing before departure from \(P_A\). The duration of quarantine is A, D 1 day; B, E 2 days; and C, F 3 days, without testing at exit from quarantine (A, B, C), and with testing at exit from quarantine (D, E, F)
3.3 Comparison between quarantine strategies
We compare the performance of quarantine strategies with different durations, with and without exit testing. Simulations show that a 1-day quarantine upon arrival with an exit test outperforms a 3-day quarantine without testing at exit in terms of delaying the case importation and the outbreak peak (Fig. 4A). Similar to previous observations, the peak of outbreak occurs with a longer delay as \(\eta \) increases (i.e., a higher proportion of infected individuals are tested). Even with testing prior to travel in \(P_A\), a 1-day quarantine with testing at exit results in a longer delay of case importation and a later outbreak peak in \(P_B\) (Fig. 4B).
4 Discussion
At the onset of an emerging disease with pandemic potential, control strategies may rely on non-pharmaceutical measures such as lockdowns and travel restrictions between populations to limit case importation and decelerate global spread (Wells et al. 2020). However, prolonged use of these measures would result in substantial socioeconomic losses (Klinger et al. 2021). Furthermore, travel restrictions may be ineffective in preventing cases importation during some stages of the disease such as asymptomatic or pre-symptomatic (Russell et al. 2021). Travel-related policies, such as quarantine and testing of travelers, could provide alternative approaches to travel restrictions (Wells et al. 2022).
The effectiveness of quarantine and testing of travelers in preventing case importation and timelines of an outbreak depends on various factors, including the diagnostic sensitivity of the test, stage of disease at the time of testing, and the duration of quarantine (Wells et al. 2022; Molero-Salinas et al. 2022). Here, we constructed a meta-population compartmental model of disease transmission to include these factors and evaluate the effect of these travel-related policies. Our results show that within-population testing for the identification and isolation of infectious individuals is essential in flattening the outbreak. While testing of travelers prior to departure can delay the start of an outbreak in the destination population, the duration of quarantine upon arrival has negligible effects on timelines and the magnitude of an outbreak. We found that testing at exit from quarantine in destination has the largest effect on reducing case importation. For instance, a 1-day quarantine with testing at exit leads to comparable or superior effectiveness in delaying the outbreak in the destination population compared to a longer, 3-day quarantine without an exit test.
Incidence of infection in \(P_B\) when quarantine of travelers is implemented upon arrival with (dashed), or without (solid) testing at exit from quarantine. Dashed and solid lines correspond to quarantine durations of 1 and 3 days, respectively, without (A) and with (B) testing prior to departure from \(P_A\)
Consistent with previous work (Wells et al. 2022), our model shows that quarantine of travelers for a short duration combined with an exit test could be an effective alternative to an extended quarantine duration without testing. Furthermore, testing at departure is unlikely to eliminate case importation or to delay an outbreak in the destination population without control measures being implemented at arrival (Bou-Karroum et al. 2021). More importantly, our results indicate that in the absence of other measures (i.e., vaccination Lee et al. 2022), testing of travelers after quarantine in the destination is more effective than testing before quarantine (at the departure or upon arrival). We note that once the disease is introduced into the destination population, the overall attack rate depends mainly on the measures implemented within the population (e.g., isolation of infectious cases that reduces the reproduction number) to control the spread, and the effect of quarantine duration at arrival would be negligible.
Our findings should be interpreted within the context of study limitations. First, we developed our model in the absence of other non-pharmaceutical measures and vaccination, which could quantitatively affect our results. For simplicity, we made similar assumptions for both populations in the model, e.g., in terms of dispersal rates and testing of infectious individuals. However, these parameters would be affected by various population-specific factors and the internal healthcare system. Second, we simplified the model based on a susceptible-exposed-infectious-recovered structure, without considering other stages in the natural history of disease. For example, COVID-19 is known to have asymptomatic and presymptomatic stages, both of which are infectious with different durations and transmissibilities (Moghadas et al. 2020). Since manifestation of clinical symptoms may be a factor in testing and isolation, infectious individuals may not be identified during asymptomatic or presymptomatic stages. Although these are important considerations, the overall effect in our model could be captured in the proportion of infectious individuals tested, the sensitivity of the test, and the transmission rate that can be adjusted with the reproduction number (Vilches et al. 2022). Third, we assumed perfect isolation and quarantine, preventing disease transmission using these strategies. Fourth, we parameterized the model with early estimates of SARS-CoV-2 infection, which have changed over time as different variants have emerged. Finally, we did not account for turnaround times of test results, making the implicit assumption that timelines are short with consideration of rapid testing (Wells et al. 2022). Given these limitations that merit further investigation and the assumptions made in developing the model, we highlight the qualitative aspect of our findings.
5 Conclusion
Travel restrictions may be among measures considered as the first line of defense against the global spread of emerging diseases. Our study provides a theoretical framework for assessing alternative strategies, highlighting the benefits of exit testing in reducing the duration of quarantine and delaying outbreaks in destination populations. The exact parameters of implementing such travel-related policies (e.g., testing capacity, quarantine facility) depend on the epidemiology of disease and the population immunity, which may vary with time (Wells et al. 2022). Optimal quarantine and testing strategies could be a viable approach to socioeconomically burdensome travel restrictions in combating future diseases with pandemic potential.
References
Alexander ME, Moghadas SM, Röst G, Wu J (2008) A delay differential model for pandemic influenza with antiviral treatment. Bull Math Biol 70(2):382–397
Alfano V, Ercolano S (2020) The efficacy of lockdown against COVID-19: a cross-country panel analysis. Appl Health Econ Health Policy 18:509–517
Arino J, Van Den Driessche P (2006) Time delays in epidemic models: modeling and numerical considerations. In: Delay differential equations and applications. Springer, pp 539–578
Bou-Karroum L, Khabsa J, Jabbour M, Hilal N, Haidar Z, Abi Khalil P, Khalek RA, Assaf J, Honein-AbouHaidar G, Abou Samra C et al (2021) Public health effects of travel-related policies on the COVID-19 pandemic: a mixed-methods systematic review. J Infect 83(4):413–423
Brownstein JS, Wolfe CJ, Mandl KD (2006) Empirical evidence for the effect of airline travel on inter-regional influenza spread in the United States. PLoS Med 3(10):401
Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, Pastore y Piontti A, Mu K, Rossi L, Sun K et al (2020) The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 368(6489):395–400
Di Domenico L, Pullano G, Sabbatini CE, Boëlle P-Y, Colizza V (2020) Impact of lockdown on COVID-19 epidemic in Île-de-France and possible exit strategies. BMC Med. https://doi.org/10.1186/s12916-020-01698-4
Dickens BL, Koo JR, Lim JT, Sun H, Clapham HE, Wilder-Smith A, Cook AR (2020) Strategies at points of entry to reduce importation risk of COVID-19 cases and reopen travel. J Travel Med 27(8):141
Diekmann O, Heesterbeek JAP (2000) Mathematical epidemiology of infectious diseases: model building, analysis and interpretation, vol 5. Wiley, New York
Findlater A, Bogoch II (2018) Human mobility and the global spread of infectious diseases: a focus on air travel. Trends Parasitol 34(9):772–783
Germann TC, Kadau K, Longini IM, Macken CA (2006) Mitigation strategies for pandemic influenza in the United States. Proc Natl Acad Sci 103(15):5935–5940
Hollingsworth TD, Ferguson NM, Anderson RM (2006) Will travel restrictions control the international spread of pandemic influenza? Nat Med 12(5):497–499
International Air Transport Association (IATA) (2020) Air connectivity: measuring the connections that drive economic growth. Technical report
Klinger C, Burns J, Movsisyan A, Biallas R, Norris SL, Rabe JE, Stratil JM, Voss S, Wabnitz K, Rehfuess EA et al (2021) Unintended health and societal consequences of international travel measures during the COVID-19 pandemic: a scoping review. J Travel Med 28(7):123
Lee FW, Wang J, Wang CJ (2022) A testing and quarantine algorithm for individual international travelers using published data on WHO-approved vaccines and Bayes’ Theorem. Vaccines 10(6):902
Leung K, Wu JT, Leung GM (2021) Effects of adjusting public health, travel, and social measures during the roll-out of COVID-19 vaccination: a modelling study. Lancet Public Health 6(9):674–682
Li R, Pei S, Chen B, Song L, Zhang T, Yang W, Shaman J (2020) Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus. Science 368(6490):489–493
Moghadas SM, Fitzpatrick MC, Sah P, Pandey A, Shoukat A, Singer BH, Galvani AP (2020) The implications of silent transmission for the control of COVID-19 outbreaks. Proc Nal Acad Sci USA 117(30):17513–17515
Molero-Salinas A, Rico-Luna C, Losada C, Buenestado-Serrano S, de la Cueva García VM, Egido J, Adán-Jiménez J, Catalán P, Muñoz P, Pérez-Lago L et al (2022) High SARS-CoV-2 viral load in travellers arriving in Spain with a negative COVID-19 test prior to departure. J Travel Med 29(3):180
Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, Agha R (2020) The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg 78:185–193
Robertson SL, Henson SM, Robertson T, Cushing J (2018) A matter of maturity: to delay or not to delay? Continuous-time compartmental models of structured populations in the literature 2000–2016. Nat Resour Model 31(1):12160
Russell TW, Wu JT, Clifford S, Edmunds WJ, Kucharski AJ, Jit M et al (2021) Effect of internationally imported cases on internal spread of COVID-19: a mathematical modelling study. Lancet Public Health 6(1):12–20
Vilches TN, Sah P, Abdollahi E, Moghadas SM, Galvani AP (2021) Importance of non-pharmaceutical interventions in the COVID-19 vaccination era: a case study of the seychelles. J Glob Health 11:03104
Vilches TN, Rafferty E, Wells CR, Galvani AP, Moghadas SM (2022) Economic evaluation of COVID-19 rapid antigen screening programs in the workplace. BMC Med. https://doi.org/10.1186/s12916-022-02641-5
Wells CR, Pandey A, Fitzpatrick MC, Crystal WS, Singer BH, Moghadas SM, Galvani AP, Townsend JP (2022) Quarantine and testing strategies to ameliorate transmission due to travel during the COVID-19 pandemic: a modelling study. Lancet Reg Health-Europe 100304
Wells CR, Sah P, Moghadas SM, Pandey A, Shoukat A, Wang Y, Wang Z, Meyers LA, Singer BH, Galvani AP (2020) Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. Proc Natl Acad Sci 117(13):7504–7509
Wells CR, Townsend JP, Pandey A, Moghadas SM, Krieger G, Singer B, McDonald RH, Fitzpatrick MC, Galvani AP (2021) Optimal COVID-19 quarantine and testing strategies. Nat Commun 12(1):1–9
Wells CR, Pandey A, Moghadas SM, Singer BH, Krieger G, Heron RJL, Turner DE, Abshire JP, Phillips KM, Donoghue AM, Galvani AP, Townsend JP (2022) Comparative analyses of eighteen rapid antigen tests and RT-PCR for COVID-19 quarantine and surveillance-based isolation. Commun Med. https://doi.org/10.1038/s43856-022-00147-y
Wells CR, Pandey A, Gokcebel S, Krieger G, Donoghue AM, Singer BH, Moghadas SM, Galvani AP, Townsend JP (2022) Quarantine and serial testing for variants of SARS-Cov-2 with benefits of vaccination and boosting on consequent control of COVID-19. PNAS Nexus. https://doi.org/10.1093/pnasnexus/pgac100
Xu Z, Zhao X-Q (2012) A vector-bias malaria model with incubation period and diffusion. Discrete Contin Dyn Syst Ser B 17(7):2615–2634
Funding
The research was partially supported by the Natural Sciences and Engineering Research Council of Canada, Discovery Grant; Canadian Institutes of Health Research (OV4-170643, COVID-19 Rapid Research), and NSERC-MfPH Grant for Emerging Infectious Disease Modelling.
Author information
Authors and Affiliations
Contributions
JX, SMM: conceptualized the study; JX, ZW: designed the model and performed the analysis; JX, ZW, SMM: wrote the paper. All authors approve the content and final draft submitted for publication.
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
1.1 Reproduction numbers
To set a baseline for our analysis, we consider the two populations without any control measures, such as testing, isolation, or quarantine, and assume the same travel rate between \(P_A\) and \(P_B\). This simplifies our model into two populations with a susceptible-exposed-infectious-recovered structure, connected by dispersal. At the disease-free equilibrium (without any infection), all variables except \(S_A\) and \(S_B\) are zeros with \(\bar{S}_{A}=\bar{S}_{B}=N:= (N_A+N_B)/2\) when \(\delta _{_A}=\delta _{_B}\). The basic reproduction number is given by \( \mathcal {R}_0=\beta N/\gamma \).
When control measures are applied, \(\mathcal {R}_0\) may be reduced, which is characterized by the control reproduction number \(\mathcal {R}_c\). To calculate \(\mathcal {R}_c\) for model (6), we use the Next Generation Matrix (NGM) approach introduced in Xu and Zhao (2012). Let \(x_1, \ldots , x_{11}\) be the number of individuals in the \(E_A, E_{iA}, I_A, I_{iA}\), and \(E_B, E_{iB}, I_B, I_{iB}, I_{q1B}, E_{qB}, I_{q2B}\) classes, respectively. It then follows from the model (6) that the distribution of the remaining individuals at time \(t>0\) is
Thus, the total numbers of newly infected individuals in each class are
Similarly, we have
From the relationship between \((\bar{x}_1, \ldots , \bar{x}_{11})\) and \(x_1, \ldots , x_{11}\), we have the next generation operator \(\mathcal {M}\) (Matrix (9)), where
Since the reproduction number is defined as the spectral radius of \(\mathcal {M}\) (Xu and Zhao 2012), we obtain \(\mathcal {R}_c = (\rho (\mathcal {M}))^2\).
We note that the interventions of testing before departure from \(P_A\), quarantine and its duration upon arrival in \(P_B\), and testing at exit quarantine, have no significant effects on the control reproduction number (Fig. 5). However, the proportion of infectious individuals isolated within the population (\(\eta \)) reduces the reproduction number, leading to further delay in case importation and the outbreak within \(P_B\) with a lower peak and cumulative incidence.
1.2 Effect of dispersal rate on the reproduction number
See Fig. 5.
Control reproduction number as a function of dispersal rate. Solid and dashed lines (overlapped) correspond to scenarios without and with testing before departure from \(P_A\). The duration of quarantine is A, D 1 day; B, E 2 days; and C, F 3 days, without testing at exit from quarantine (A, B, C), and with testing at exit from quarantine (D, E, F) in \(P_B\)
1.3 Effect of dispersal rate on peak-time of the outbreak
See Fig. 6.
Range for the peak time of incidence in \(P_B\) when dispersal rate, \(\delta \), varies between 0.0001 and 0.001, with quarantine of travelers upon arrival. Solid and dashed lines correspond to scenarios without and with testing before departure from \(P_A\). The duration of quarantine is A, D 1 day; B, E 2 days; and C, F 3 days, without testing at exit from quarantine (A, B, C), and with testing at exit from quarantine (D, E, F)
1.4 Cumulative incidence
See Fig. 7.
Attack rate (i.e., the proportion of the population infected throughout the outbreak) in \(P_B\) when quarantine of travelers is implemented upon arrival. Solid and dashed lines correspond to scenarios without and with testing before departure from \(P_A\). The duration of quarantine is A, D 1 day; B, E 2 days; and C, F 3 days, without testing at exit from quarantine (A, B, C), and with testing at exit from quarantine (D, E, F)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, J., Wang, Z. & Moghadas, S.M. Modelling the effect of travel-related policies on disease control in a meta-population structure. J. Math. Biol. 87, 55 (2023). https://doi.org/10.1007/s00285-023-01990-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00285-023-01990-w