Abstract
Polymicrobial lung infections in individuals with Cystic Fibrosis (CF) contribute to the complexity of this disease and are a major cause of morbidity and mortality in the CF community. The microorganisms most commonly associated with severe airway infections in individuals with CF are the opportunistic pathogens S. aureus, P. aeruginosa and bacteria from the Burkholderia cepacia complex (Bcc), particularly B. cenocepacia and B. multivorans. Three Bcc strains, two S. aureus wild-type strains, and two derivative mutants were used to investigate the interplay between S. aureus and Bcc with a focus on the hemolytic activity of Bcc. Our results revealed that extracellular products from S. aureus potentiated the hemolysis of Bcc strains. Moreover, this effect was influenced by the composition of the medium in which S. aureus is grown. These findings contribute towards the understanding of the impact of interactions between S. aureus and Bcc and their possible implications in the context of co-infections by these pathogens in individuals with CF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cystic Fibrosis (CF) is an autosomal recessive genetic disorder linked to mutations in the CF transmembrane conductance regulator gene. CF is a multi-system disease with special impact on the airways. The cumulative presence of dense mucus in lungs, progressively leads to bronchiectasis and predisposes individuals to chronic infections that constitute the main cause of morbidity and early mortality among CF patients. These infections are usually difficult to eradicate due to failure of antibiotic therapies, representing a serious concern for the CF community, physicians and researchers.
Traditionally, Staphylococcus aureus, Pseudomonas aeruginosa, Haemophilus influenzae, and bacteria belonging to the Burkholderia cepacia complex (Bcc) are associated with chronic infections in the airways of CF patients [1, 2]. A large number of studies were focused on understanding the diverse mechanisms that promote virulence and antibiotic resistance in these pathogens, leading them to successfully establish persistent airway infections. S. aureus is the Gram-positive pathogen that most prevalently infects the CF lungs worldwide. Such high prevalence along with the emergence of different multi-drug resistant strains of S. aureus (e.g. methicillin-resistant –MRSA-, vancomycin-intermediate –VISA-, and vancomycin-resistant –VRSA- S. aureus), pose a very serious threat to public health [2,3,4]. In particular, the clinical prognosis of CF patients seriously worsens when they acquire MRSA infections [5, 6].
Bcc is composed of at least 20 related species that are naturally able to resist a wide range of antibiotics. As a consequence, Bcc-based infections in CF patients are usually very difficult to eradicate and lead to a progressive decline in lung function. In this context, patients may develop cepacia syndrome which is characterized by bacteremia and a rapid and uncontrollable deterioration in their health with often fatal consequences [7].
Despite the recognition that chronic airway infections in CF patients are commonly polymicrobial, most investigations have been focused on studying the pathogenesis of each microorganism individually [8]. Thus, relatively little is known about the interactions that occur between CF pathogens and the impact of their interactions on chronic infection. In this sense, in cases where polymicrobial interactions have been studied, relevant insights have been gained [2]. For instance, it was shown that peptidoglycan shed by Gram-positive bacteria enhances the virulence of P. aeruginosa by increasing the production of compounds with lytic activity [9]. Moreover, the α-toxin virulence factor from S. aureus was found to potentiate P. aeruginosa, Klebsiella pneumoniae and Acinetobacter baumannii proliferation, systemic spread, and lethality by preventing acidification of bacteria-containing macrophage phagosomes [10]. Of increasing relevance are the co-infections of S. aureus and Bcc, which are being reported in different CF centers all around the world (Dr. Benjamin Kopp, Nationwide Children´s Hospital, Ohio, USA; Dr. Pavel Drevinek, University Hospital Motol, Prague, Czech Republic; Dr. Laura Galanternik, Ricardo Gutierrez Children´s Hospital, Buenos Aires Argentina, personal communication). Despite the increasing awareness of these co-infections, very little is known regarding the interplay between S. aureus and Bcc. In fact, to the best of our knowledge, only one study, in which the interaction between S. aureus and Bcc was investigated, has been reported [11]. Interestingly, this study showed that products secreted by S. aureus are able to suppress the pro-inflammatory response of host cells induced by B. cenocepacia.
Acknowledging the need to increase our understanding of other clinically relevant aspects of the S. aureus-Bcc interaction, herein we studied the effects of their interactions on hemolysis. Our results showed that extracellular products from S. aureus potentiate the hemolysis of Bcc strains. This effect was found to be dependent on the composition of the culture medium in which S. aureus was grown and linked to the production of α-hemolysin by S. aureus. Overall, our results provide new insights into the interplay between S. aureus and Bcc and how it may impact Bcc virulence.
Materials and Methods
Bacterial Strains
Three Bcc strains, B. multivorans 249 (Bm249), B. contaminans (BcFFH2055) and B. cenocepacia J2315, two S. aureus wild-type strains, MSSA LS1 and MRSA USA300, and two derivative mutants, S. aureus LS1∆agr and USA300∆hla, were used throughout the study. All strains were stored in Tryptone Soy Broth (TSB) with 40%glycerol at -80 °C until use (Supplementary Table S1).
Cell-Free Conditioning Media (CFCM) Preparation
CFCM were prepared by inoculating the S. aureus strains in TSB, Luria–Bertani Broth (LB), Terrific Broth (TB) and Brain Heart Infusion (BHI). LB broth was prepared by mixing 10 g of peptone, 10 g of sodium chloride and 5 g of yeast extract, TB broth was prepared by mixing 12 g of tryptone, 24 g of yeast extract, 4 ml of glycerol and potassium phosphate buffer, and the BHI broth was prepared according to the manufacture recipe (Becton Dickinson, Germany). The cultures were incubated at 37 °C under shaking conditions for 48 h, centrifuged at 7000×g for 10 min and the supernatants were filtered using a Steriflip Vacuum Filtration System with Millipore Express PLUS Membrane (0.22 µm) (Millipore, #SCGP00525). The resulting CFCM was stored at − 80 °C.
Proximity Assay and Colony Removal Hemolysis Assay
Overnight cultures of S. aureus and Bcc strains were prepared by inoculating 5 mL of LB with a single colony of each strain independently and incubated for 18 h at 37 °C under shaking conditions. For pairwise interactions, blood agar plates (5% sheep blood in tryptic soy agar base, Hardy diagnostics, CA, USA) were inoculated with 2.5 µL of overnight cultures of single S. aureus and Bcc strains (OD600 = 1) at separation distances of 0.5, 1 or 5 cm. Plates were incubated at 37 °C and the hemolytic activity was recorded every 24 h for up to 120 h (Fig. S1A).
To determine if the presence of S. aureus cells was required to potentiate the hemolytic activity of Bcc strains, the colony removal hemolysis assay was carried out. Briefly, 2.5 µL and 10 µL of an overnight culture in LB medium of S. aureus LS1 were spotted on opposite sides of single blood agar plates. After 24 h of growth, S. aureus LS1 colonies were removed using a sterile tube and 2.5 μL of overnight cultures of Bcc strains were inoculated independently inside and outside the opaque halos formed by S. aureus that remained on the plate. All plates were then incubated at 37 °C and the hemolytic activity of Bcc strains was monitored after 24 h (Fig. S1B).
CFCM Interaction Hemolysis Assay
Aliquots of 5 and 10 µl of S. aureus CFCM were spotted onto blood agar plates and allowed to dry at room temperature for 1 h. Plates were then inoculated with 2.5 µl of overnight cultures of Bcc (OD600 = 1) inside and outside of the areas where the aliquots of S. aureus CFCM were spotted. Plates were again allowed to dry and then incubated at 37 °C in a static incubator. Hemolytic activities were registered after 24 h (Fig. S1C).
To evaluate whether Bcc and S. aureus release extracellular products that act alone or synergistically to cause hemolysis, 5 μL of CFCM from each species were inoculated together on the same spot of the plate. As controls, 5 μL of CFCM from each species were spotted separately on blood agar plates. Hemolytic activities were recorded after incubation of the plates at 37 °C for 24 h. All experiments were performed in triplicate by independent assays.
Quantitative Analysis of Hemolysis
In blood agar, hemolysis is visually manifested as the loss the red/orange color due to the destruction of the red blood cells. In blood agar images, such decrease of the red/orange color intensity directly correlates with a decrease in the pixel intensity values. Based on this correlation, hemolysis has been quantified by performing a densitometric analysis of blood agar images using Fiji (ImageJ) software. The Regions of interest for the analysis in the images were selected using the ROI manager and plots (pixel intensity vs distance) were generated using the Multi Plot command. Fiji-generated plots were scaled to the size of respective selected regions in images.
Results
S. aureus LS1 Enhances Bm249 and BcFFH2055 Hemolysis
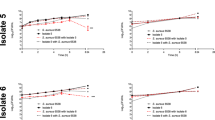
To determine if S. aureus and Bcc mutually influence their capabilities to cause hemolysis, pairwise interactions on blood agar plates were assayed. As shown in Fig. 1S. aureus LS1 forms an opaque halo of about 2 cm in diameter around its colonies. When this halo comes into contact with colonies of Bm249 and BcFFH2055, there is a marked increase in hemolytic activity of the Bcc strains clearly visualized as a decrease in the red color of the agar (Fig. 1). This effect appears to be associated with the halo produced by and surrounding the S. aureus colony, as when sectors of Bm249 and BcFFH2055 colonies remained outside of this area, such an increase in hemolysis by Bcc strains was not observed (Fig. 1c, d)., This enhanced hemolysis was more pronounced with Bm249 and not observed between S. aureus LS1 and BcJ2315 (data not shown), suggesting that this effect is likely restricted to some strains/species. Unfortunately, we were unable to detect enhancement of hemolysis of Bcc strains in the presence of the USA300 strain of S. aureus, essentially because this strain exhibited strong hemolysis itself, which made it impossible to distinguish USA300′s hemolytic activity from that of the Bcc strains (data not shown).
Proximity assay for bacterial interaction. a, b Full size images of blood agar plate exhibiting in the central part S. aureus LS1 colonies in close interaction with Bm249 (a) and BcFFH2055 (b) colonies. As control, the blood agar plates exhibit on the left and right-hand sides respective single colonies of Bcc and LS1 strains. c, d Enlarged view of pairs of S. aureus colonies interacting with Bm249 and BcFFH2055 shown in a and b, respectively. The images clearly show that S. aureus LS1 colonies form an opaque halo that when it comes in contact with Bm249 (c) and BcFFH2055 (d) colonies correlates with a marked increase in the hemolytic activity by Bcc strains. e–g Enlarged view of single S. aureus LS1 (e), Bm249 (f), BcFFH2055 (g) colonies shown in a and b. The spectral plots in (c–g) depict quantified patterns of color intensity (pixel intensity) of blood agar in respective selected (boxed) areas of the images
To determine if the hemolytic-potentiating effect of S. aureus LS1 is dependent on the presence of LS1 cells, we evaluated the hemolysis of Bcc strains in areas inside and outside halos that were pre-formed by S. aureus, but where S. aureus colonies were removed. Results showed that the hemolytic-potentiating effect on Bm249 on the blood agar occurred even in the absence of S. aureus LS1 colonies (Fig. 2), suggesting that this effect is mediated by diffusible extracellular molecules secreted by LS1.
Effect of S. aureus LS1 extracellular products on Bcc hemolysis after removal of LS1 colonies. a Full size image of blood agar plate showing Bm249 colonies grown outside (left and right) and inside (center) the area delimited by the opaque halo produced by S. aureus LS1 colonies. The halo remained after the entire LS1 colonies were removed. This image shows that in the absence of S. aureus LS1 cells, the extracellular products that remain in the region of the halo are able to stimulate the hemolytic activity of Bm249. b Magnified image of a Bm249 colony grown inside the region of the halo that remained after removal of the S. aureus LS1 colony. c Magnified image of a Bm249 colony grown outside the LS1 halo. The spectral plots in b and c depict quantified patterns of color intensity (pixel intensity) of blood agar or Bm249 colonies in the selected (boxed) areas of the images
The Growth Media Influence the Effect of S. aureus LS1 on Bcc Hemolysis
The type and amount of extracellular products that bacteria secrete can vary depending on the composition of the medium in which the bacteria are grown. Thus, we generated CFCM prepared from S. aureus LS1 cultures grown in four different media: LB, TB, TSB and BHI. As shown in Fig. 3a, CFCM prepared from LS1 cultures in LB, TSB, and BHI media caused an increase in hemolysis by Bm249 and especially by BcFFH2055. Particularly strong was the hemolytic activity of BcFFH2055 in the presence of CFCM from LS1 when grown in TSB and BHI media. Interestingly, the patterns of opaque halos associated with the CFCM also varied with the medium in which LS1 was grown. The CFCM from LS1 grown in LB and TB showed a single opaque halo, while those grown in TSB and BHI exhibited two to three halos which somehow correlated with variations in hemolysis by BcFFH2055. Unlike LB and TB, TSB and BHI contains glucose, suggesting that the presence of this carbon source may be important for the production of the extracellular products by S. aureus to stimulate Bcc hemolysis.
Effect of CFCMs prepared from S. aureus cultures grown in different media. a Bm249 and BcFFH2055 strains grown in the presence of CFCM from S. aureus LS1 prepared in LB, TB, TSB and BHI or grown alone in respective culture media. Spectral plots below the images depict quantified patterns of color intensity (pixel intensity) of blood agar and colonies in the images. b Effect on hemolysis of CFCM from Bm249 and S. aureus LS1 in LB medium that were spotted on blood agar either alone or combined
To determine if the extracellular products of both S. aureus and Bcc act together causing hemolysis of blood cells present in the agar plates, CFCM from both strains in different media were tested separately and combined. Either in isolation or when combined, the CFCM from LS1, Bm249 and BcFFH2055 did not cause robust hemolysis; minor hemolysis was observed with CFCM from LS1 alone (Fig. 3b). These results suggest that the enhanced hemolysis previously observed is the result of an active process that directly requires the cells of the Bcc strains. Notably, the CFCM from LS1 also forms an opaque halo as observed around LS1 colonies (Figs. 1 and 3b).
Agr-Deficient and α-Toxin-Deficient S. aureus Mutants Do Not Potentiate Bm249 and BcFFH2055 Hemolysis
Taking into account that as described in the literature [10] the α-toxin is one of the most prominent genes regulated by the Agr quorum sensing system, we hypothesized that they may be involved in enhancing Bcc hemolysis. To discern this we evaluated the effect of CFCM of an S. aureus LS1 derivative mutant deficient in agr (LS1∆agr) and from an USA300 derivative mutant deficient in α-toxin (USA300∆hla) on the hemolysis of the Bcc strains. CFCM prepared from LS1∆agr and USA300∆hla cultures in LB medium did not generate an increase in Bm249 hemolysis (Fig. 4). Similar results were observed for BcFFH2055, although we noticed that BcFFH2055 colonies themselves exhibited a more translucent border. Interestingly, we also observed that the opaque halos, characteristic of the CFCM from the LS1 wild-type strain, were absent in the CFCM from the LS1∆agr and USA300∆hla strains (Fig. 3b and Fig. 4). These results suggest that the Agr system and α-toxin are playing a role in the enhanced hemolytic activity of Bcc cells and that α-toxin and other Agr regulated products are associated with the opaque halo produced by S. aureus LS1.
Effect on Bcc hemolysis of CFCMs prepared from S. aureus LS1∆agr and USA300∆hla. Bm249 and BcFFH2055 strains grown alone or in the presence of CFCMs prepared from S. aureus LS1∆agr and USA300∆hla in LB medium (left and central panels). The right panel shows CFCM from LS1∆agr and USA300∆hla that were spotted on blood agar alone
Discussion
Despite the clinical relevance of S. aureus and the Bcc, little is known about their interactions. Previous research has shown that S. aureus α-toxin potentiates several virulence-related traits of various Gram-negative bacteria [10]. On the other hand, it has been shown that Bcc secretes hemolytic compounds that are correlated with increased virulence and the onset of the cepacia syndrome [12, 13]. Otherwise, prior to this work only one study reported how the interplay of these common CF pathogens by revealing their influences on the response of epithelial host cells [14].
Many biological phenomena that could lead to a better understanding of the S. aureus/Bcc co-infection remain unstudied. Here, we focused on the influence S. aureus on the hemolytic activity of three Bcc species.
Thomson et al. 2012, have demonstrated that the hemolytic activity of Bcc, which is mediated by a toxin, was associated with the virulence in these bacteria [13]. The effect of S. aureus in Bcc hemolytic activity observed in our work, suggests that this interaction is imparting changes in Bcc virulence.
Our data revealed that regarding hemolytic activity the interaction of S. aureus-Bcc depends on the S. aureus strain and the Bcc species. MSSA LS1 increased the Bcc hemolytic activity, while MRSA USA300′s activity could not be differentiated due to this strain’s intrinsic hemolysis. The impact of LS1 on hemolysis was observed with Bm249 and BcFFH2055 but not with BcJ2315. The effect of S. aureus LS1 on Bcc hemolytic activity adds a novel aspect to those reported by Ji et al.[11], who showed that S. aureus secreted products suppressed the pro-inflammatory response in host cells induced by B. cenocepacia.
On the other hand, it is widely known that extracellular products mediate communication between bacteria and this communication results in positive or negative interactions that modify different aspects of bacterial behavior like biofilm formation, antibiotic resistance profiles, expression of virulence factors, etc. [10, 15]. Using simple assays like colony removal and CFCM hemolysis assays, we have shown that S. aureus potentiates Bcc hemolytic activity by means extracellular products. We also found that this potentiation occurs when S. aureus is grown in enriched culture media like TSB or BHI suggesting that extracellular products involved in Bcc hemolytic potentiation are produced and released under specific growth conditions.
Probably the most studied and characterized extracellular compound produced by S. aureus is α-toxin [16,17,18,19]. This exoprotein is expressed in most S. aureus strains and is up-regulated by the agr regulatory locus. The inclusion of S. aureus mutants USA300∆hla and S. aureus LS1∆agr in the assays originally aimed to reveal if extracellular compounds involved in hemolytic Bcc potentiation are related to α-toxin. We observed that CFCM from S. aureus LS1∆agr and USA300∆hla, did not increase Bcc’s hemolytic activity Overall the results obtained allow us to propose that the increase in hemolytic activity of Bcc caused by S. aureus is mediated in part by extracellular compounds that are regulated by the agr regulatory locus.
The complexity of microbial infections in CF patients requires more research focusing on bacteria interactions for a better understanding of co-infections. Even though deeper studies are necessary, the finding that S. aureus extracellular compounds potentiate Bcc’s hemolytic activity contributes to the knowledge of the complex disease state in CF.
References
Surette MG (2014) The cystic fibrosis lung microbiome. Ann Am Thorac Soc 11(Suppl 1):S61-65. https://doi.org/10.1513/AnnalsATS.201306-159MG
Granchelli AM, Adler FR, Keogh RH, Kartsonaki C, Cox DR, Liou TG (2018) Microbial interactions in the cystic fibrosis airway. J Clin Microbiol. https://doi.org/10.1128/JCM.00354-18
Lyczak JB, Cannon CL, Pier GB (2002) Lung infections associated with cystic fibrosis. Clin Microbiol Rev 15(2):194–222
Chmiel JF, Aksamit TR, Chotirmall SH, Dasenbrook EC, Elborn JS, LiPuma JJ, Ranganathan SC, Waters VJ, Ratjen FA (2014) Antibiotic management of lung infections in cystic fibrosis. I. The microbiome, methicillin-resistant Staphylococcus aureus, Gram-negative bacteria, and multiple infections. Ann Am Thorac Soc 11(7):1120–1129. https://doi.org/10.1513/AnnalsATS.201402-050AS
Vanderhelst E, De Meirleir L, Verbanck S, Pierard D, Vincken W, Malfroot A (2012) Prevalence and impact on FEV(1) decline of chronic methicillin-resistant Staphylococcus aureus (MRSA) colonization in patients with cystic fibrosis. A single-center, case control study of 165 patients. J Cyst Fibros 11(1):2–7. https://doi.org/10.1016/j.jcf.2011.08.006
Dasenbrook EC, Checkley W, Merlo CA, Konstan MW, Lechtzin N, Boyle MP (2010) Association between respiratory tract methicillin-resistant Staphylococcus aureus and survival in cystic fibrosis. JAMA 303(23):2386–2392. https://doi.org/10.1001/jama.2010.791
Govan JR, Brown AR, Jones AM (2007) Evolving epidemiology of Pseudomonas aeruginosa and the Burkholderia cepacia complex in cystic fibrosis lung infection. Future Microbiol 2(2):153–164. https://doi.org/10.2217/17460913.2.2.153
Zemanick ET, Hoffman LR (2016) Cystic fibrosis: microbiology and host response. Pediatr Clin N Am 63(4):617–636. https://doi.org/10.1016/j.pcl.2016.04.003
Hotterbeekx A, Kumar-Singh S, Goossens H, Malhotra-Kumar S (2017) In vivo and In vitro Interactions between Pseudomonas aeruginosa and Staphylococcus spp. Front Cell Infect Microbiol 7:106. https://doi.org/10.3389/fcimb.2017.00106
Cohen TS, Hilliard JJ, Jones-Nelson O, Keller AE, O’Day T, Tkaczyk C, DiGiandomenico A, Hamilton M, Pelletier M, Wang Q, Diep BA, Le VT, Cheng L, Suzich J, Stover CK, Sellman BR (2016) Staphylococcus aureus alpha toxin potentiates opportunistic bacterial lung infections. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aad9922
Ji Y, Bolhuis A, Watson ML (2019) Staphylococcus aureus products subvert the Burkholderia cenocepacia-induced inflammatory response in airway epithelial cells. J Med Microbiol 68(12):1813–1822. https://doi.org/10.1099/jmm.0.001100
Hutchison ML, Poxton IR, Govan JR (1998) Burkholderia cepacia produces a hemolysin that is capable of inducing apoptosis and degranulation of mammalian phagocytes. Infect Immun 66(5):2033–2039
Thomson EL, Dennis JJ (2012) A Burkholderia cepacia complex non-ribosomal peptide-synthesized toxin is hemolytic and required for full virulence. Virulence 3(3):286–298. https://doi.org/10.4161/viru.19355
Limoli DH, Whitfield GB, Kitao T, Ivey ML, Davis MR Jr, Grahl N, Hogan DA, Rahme LG, Howell PL, O’Toole GA, Goldberg JB (2017) Pseudomonas aeruginosa alginate overproduction promotes coexistence with Staphylococcus aureus in a model of cystic fibrosis respiratory infection. MBio. https://doi.org/10.1128/mBio.00186-17
Vu B, Chen M, Crawford RJ, Ivanova EP (2009) Bacterial extracellular polysaccharides involved in biofilm formation. Molecules 14(7):2535–2554. https://doi.org/10.3390/molecules14072535
Bhakdi S, Tranum-Jensen J (1991) Alpha-toxin of Staphylococcus aureus. Microbiol Rev 55(4):733–751
Hildebrand A, Pohl M, Bhakdi S (1991) Staphylococcus aureus alpha-toxin. Dual mechanism of binding to target cells. J Biol Chem 266(26):17195–17200
Otto M (2014) Staphylococcus aureus toxins. Curr Opin Microbiol 17:32–37. https://doi.org/10.1016/j.mib.2013.11.004
Tam K, Torres VJ (2019) Staphylococcus aureus secreted toxins and extracellular enzymes. Microbiol Spectr. https://doi.org/10.1128/microbiolspec.GPP3-0039-2018
Acknowledgements
We want to thank Lorena Tuchscherr de Hauschopp for the mutant LS1 Δagr and Jovanka Voyich de Montana for the USA300 Δhla mutant.
Funding
Research reported in this publication was in part supported by the 2019–20 Junior/Senior Intramural Grant 0357019 to M.S.R. and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (NIH) to M.S.R under Award Numbers SC3GM125556 and to R.A.B. under Award Numbers R01AI100560, R01AI063517, and R01AI072219. This study was also supported in part by funds and/or facilities provided by the Cleveland Department of Veterans Affairs, Award Numbers 1I01BX002872 to K.M.P.-W. and 1I01BX001974 to R.A.B. from the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development, and the Geriatric Research Education and Clinical Center VISN 10. Cystic Fibrosis Foundation #691309 also support the laboratory of KMP-W. D.O.S is a member of the National Research Council of Argentina (CONICET). S.M is recipient of a postdoctoral fellowship from CONICET. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, the Department of Veterans Affairs or the United States Government.
Author information
Authors and Affiliations
Contributions
1) Conception and design of the study: AM, DS, JD, MSR; 2) Acquisition and analysis of data: AM, DS, AH, SM, JD, MSR; 3) Drafting and revision of manuscript: AM, DS, SM, JD, RB, KPW, MSR.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Moriano, A., Serra, D.O., Hoard, A. et al. Staphylococcus aureus Potentiates the Hemolytic Activity of Burkholderia cepacia Complex (Bcc) Bacteria. Curr Microbiol 78, 1864–1870 (2021). https://doi.org/10.1007/s00284-021-02458-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-021-02458-0