Abstract
Antibiotic resistance has brought into question the efficiency of clarithromycin which is a vital component of eradication therapy for Helicobacter pylori infection. The point mutations within the 23S rRNA sequence of H. pylori isolates which contribute to clarithromycin resistance have yet to be fully characterized. This study was aimed to detect clarithromycin resistance-associated mutations and assess the prevalence of key virulence factors of H. pylori among Iranian patients. Amplification of 16S rRNA and glmM genes were done to identify H. pylori. Minimal inhibitory concentration (MIC) of clarithromycin in 82 H. pylori clinical isolates was determined by agar dilution method. Subsequently, various virulence markers including cagA, vacA, sabA, babA, and dupA of H. pylori were identified by PCR. PCR-sequencing was applied to detect point mutations in the 23S rRNA gene. Based on MIC values, 43.9% of H. pylori isolates showed resistance to clarithromycin. The babA and cagA genes were detected in 92.7% and 82.9% of isolates, assigned to be higher than other virulence factors. No significant relationship was found between the H. pylori virulence genotypes and clarithromycin susceptibility (P > 0.05). Analyzing the 23S rRNA sequences revealed A2143G (4/48, 8.3%) and A2142G (3/48, 6.2%) as the most prevalent mutations in clarithromycin-resistant isolates. Additionally, several novel mutations including G2220T, C2248T, A2624C, G2287A, T2188C, G2710C, C2248T, G2269A, and G2224T were also detected among either resistant or susceptible isolates. Our findings revealed the presence of several point mutations in the 23S rRNA gene of H. pylori isolates which may be associated with resistance to clarithromycin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Helicobacter pylori (H. pylori) has been recognized as a Gram-negative, microaerophilic microorganism which affects a large number of people on a global scale, with an increasing trend in developing countries. Since the role of H. pylori as the most successful human pathogen in the progression of chronic gastritis, peptic ulcer, gastric cell carcinoma and gastric mucosa-associated lymphoid tissue (MALT) was discovered, research on H. pylori eradication therapy began [1,2,3]. Several lines of empirical evidence revealed the reduction of gastric cancer owing to eradication of H. pylori infection [4]. However, the efficiency of H. pylori infection treatment has drastically dwindled due to factors such as antibiotic resistance, poor adherence to the eradication regimen, drug dosage administered, and duration of therapy. Of these, antibiotic resistance plays the most important role in H. pylori treatment failure [5]. Investigating antibiotic resistance from the molecular perspective highlights the notion that point mutations in the genome of H. pylori remain a big reason behind this global public health challenge [6]. Clarithromycin is an acid-stable and the most common bacteriostatic antibiotic which belongs to the macrolide group. This agent is frequently used as a vital component of standard triple therapy in first-line eradication regimens for H. pylori infection. Though, the efficiency of clarithromycin has been brought into question mostly due to antibiotic resistance [4]. It is often argued that the existence of cross-resistance in each family of antibiotics is due to the same resistance mechanism. Hence, resistance to clarithromycin implies resistance to all macrolides [7]. It is conceived that three-point mutations in the region of domain V of 23S rRNA, including A2142G, A2142C, and A2143G, mediate > 80% of H. pylori clarithromycin resistance in the world and ~ 90% of resistance in developed nations [8, 9]. However, the occurrence of point mutation at other positions such as A2115G, G2141A, T2117C, T2182C, T2717C, A2144G, C2147G, T2190C, C2195T, A2223G, and C2694A should not be overlooked [10, 11]. In the light of Maastricht V/Florence Consensus report, it is rational to perform susceptibility testing prior to first-line eradication therapy in areas with high clarithromycin resistance rates, since the prevalence of H. pylori antibiotic resistance varies in one region of a country over time and significantly from country to country. Furthermore, prescription of triple therapy containing clarithromycin should be averted when the primary clarithromycin resistance rate is more than 15–20% [4, 12,13,14].
A growing body of literature has investigated the correlation of antibiotic resistance with bacterial genetic factors, since an increasing trend in clarithromycin resistance has become a global concern [10]. A series of recent studies has indicated that bacterial virulence factors are categorized into three major pathogenic groups based on their ability to promote the pathogenesis of H. pylori infection. The groups are as follows: colonization (babA, sabA), immune escape (cagA, vacA), and disease induction (cagA, vacA, babA, dupA) [15, 16]. There are controversial arguments over the role of these virulence factors and antibiotic susceptibility. While recent finding reported a significant association between clarithromycin resistance and vacA i1 genotype; this view has been refuted by others [17, 18]. As might be expected, genotyping of H. pylori strains opens a new window for understanding a better picture of clinical outcomes, post-treatment follow-up and human migration [19]. Herein, we aimed to assess H. pylori antibiotic susceptibility rate in response to clarithromycin among Iranian patients with various gastroduodenal diseases. Additionally, we reported H. pylori 23S rRNA point mutations linked to clarithromycin resistance among Iranian clinical isolates. The prevalence of H. pylori virulence factors including cagA, vacA, sabA, babA, and dupA was also investigated.
Materials and Methods
Gastric Biopsy Samples
Antral biopsy specimens were collected from 82 previously determined H. pylori-infected patients, who underwent upper gastroduodenal endoscopy at Taleghani Hospital in Tehran from June 2017 to October 2019. The H. pylori infection in these patients was confirmed through culture, histological observations and RUT test. The biopsy samples were kept in transport medium consisting of thioglycolate supplemented with 1.3 g/L agar (Merck, Germany) and 3% yeast extract (Oxoid) and immediately were sent to the Helicobacter research laboratory. The exclusion criteria were those patients who took eradication therapy for H. pylori including PPIs, or H2-receptor blockers, and any antibiotics used for other infections within two weeks prior to enrollment. The study protocol was approved by the Institutional Ethical Review Committee of the Research Institute for Gastroenterology and Liver Diseases at Shahid Beheshti University of Medical Sciences (Project No. IR.SBMU.RIGLD.REC.1395.878). All participants and/or their legal guardians signed written informed consent before enrollment in the study.
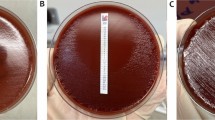
H. pylori Culture and Identification
The gastric biopsy specimens were completely homogenized and smeared on Brucella agar (Merck, Darmstadt, Germany) containing 7% horse blood (v/v), 10% fetal calf serum (FCS), and Campylobacter-selective supplement (vancomycin 2.0 mg/L, polymyxin B 0.05 mg/L, trimethoprim 1.0 mg/L). To prevent further fungal contamination, amphotericin B (2.5 mg/l) was added to the medium. The plates were incubated at 37 °C under microaerophilic atmosphere (5% O2, 10% CO2, and 85% N2) in a CO2 incubator (Innova CO-170; New Brunswick Scientific, USA) for 3–7 days. Bacterial colonies were identified as H. pylori on the basis of phenotypic and biochemical tests including positive reactions for urease, catalase, and oxidase, and confirmed by PCR (16S rRNA and glmM) as previously described [20, 21].
Antimicrobial Susceptibility Testing
The antibiotic susceptibility of the H. pylori strains was determined by the agar dilution method against clarithromycin purchased from Sigma-Aldrich (St. Louis, MO, USA). Briefly, H. pylori suspensions were prepared in sterile saline and adjusted to a density equal to McFarland standard No. 3. The bacterial inocula were inoculated directly onto Mueller–Hinton agar (Merck, Darmstadt, Germany) plates supplemented with 10% defibrinated horse blood containing clarithromycin dilutions ranging from 0.06 to 64 mg/L, and were incubated under microaerophilic conditions, as over-mentioned. The minimal inhibition concentration (MIC) was defined as the lowest concentration of antibiotic that thoroughly prevented the growth of the bacteria after 72 h of incubation. Clarithromycin MICs were interpreted based on the last guideline of European Committee on Antimicrobial Susceptibility Testing (EUCAST version 9.0, http://www.eucast.org/) [21]. Strains were considered to be susceptible for MIC of ≤ 0.25 mg/L, intermediate for MIC of 0.5 mg/L, and resistant for MIC of > 0.5 mg/L. A clarithromycin-susceptible H. pylori clinical isolate (strain HC114, NCBI/GenBank: MH040927.1) with previously identified MIC value served as a quality control strain [20].
Genotyping of H. pylori Virulence Determinants
DNA was extracted from single colonies from subcultures of each H. pylori strain using the QIAamp DNA extraction kit (QIAgen®, Hilden, Germany) according to the manufacturer’s instructions. The concentration and integrity of DNA samples were verified by NanoDrop ND‐1000 spectrophotometer (NanoDrop Technologies, Wilmington, DE, USA). The extracted DNA samples were stored at − 20 °C until further processing. PCR was used for virulence genotyping of H. pylori isolates. These virulence factors were as follows: cagA, vacA allelic types (s1/s2 and m1/m2), babA2, sabA, and dupA genes. The oligonucleotide sequences are presented in Table 1. PCR was performed in a final volume of 25 μl reaction mixture comprised of 2.5 µl 1X PCR buffer, 1 pmol of primers, 2 μl of DNA template (approximately 200 ng), 100 mM of dNTPs, 2 mM of MgCl2, and 1.5 U/μL SuperTaq™ DNA polymerase (HT Biotechnology Ltd., Cambridge, UK). PCR amplifications were performed based on the previously described cycling programs [20, 22].
Primer Design for Detection of 23S rRNA Point Mutations
The NCBI GenBank database (http://www.ncbi.nlm.nih.gov/genbank/) and the DNA Data Bank of Japan (http://www.ddbj.nig.ac.jp/) were used to access available complete 23S rRNA sequences of H. pylori strains. Based on sequence alignments of the 23S rRNA gene from various H. pylori strains and using the complete 23S rRNA sequence of H. pylori UA802 (U27270.1), specific primers for the conserved regions which cover all putative mutations associated with clarithromycin resistance were designed using CLC Sequence Viewer 8 (https://www.qiagenbioinformatics.com/), and Gene Runner Version 3.05 software. The expected size of the PCR amplicon was 1041 bp using primers 23S-F 5′-AGCACCGTAAGTTCGCGATAAG-3′ and 23S-R 5′-CTTTCAGCAGTTATCACATCC-3′. The primer specificity was checked in silico by the Basic Local Alignment Search Tool (http://blast.ncbi.nlm.nih.gov/Blast.cgi) analysis.
Direct Sequencing of 23S rRNA Gene
To detect specific mutations in the 23S rRNA gene of H. pylori strains, the direct PCR-based Sanger sequencing method was used for a selection of 50 susceptible and resistant strains. Briefly, PCR amplification was carried out in a final volume of 25 µl as over-mentioned under the cycling conditions: initial denaturation 94 °C for 4 min, followed by 30 cycles of 94 °C for 1 min, 56 °C for 45 s, and 72 °C for 1 min, with a final elongation step at 72 °C for 10 min. The PCR amplicons were purified using the Silica Bead DNA Gel Extraction Kit (Thermo Scientific, Fermentas, USA). Subsequently, both strands were sequenced by an automated sequencer (Macrogen, Seoul, Korea). DNA sequences were edited by Chromas Lite version 2.5.1 (Technelysium Pty Ltd, Australia) and BioEdit version 7.2.5 [23], and were aligned to the 23S rRNA sequence of H. pylori UA802 (U27270.1) as a reference sequence.
Phylogenetic Analysis
The edited 23S rRNA sequences of the H. pylori strains were aligned against reference sequence using ClustalW multiple alignment. A Maximum Likelihood tree was constructed by the Tamura 3-parameter model using Molecular Evolutionary Genetics Analysis version 7.0 (MEGA7) [24]. Bootstrap values were based on 1000 replicates.
Statistical Analysis
Statistical association between H. pylori resistance to clarithromycin and virulence genotypes was analyzed by the non-parametric Chi-square and Fisher’s exact tests using SPSS statistics version 23.0 for windows (IBM Corporation, Armonk, New York, USA). A P value of < 0.05 was regarded statistically significant.
Results
Patient Characteristics
The H. pylori-infected patients consisted of 52 (45.6%) men and 30 (54.4%) women, with an average age of 49.7 ± 3.33 years old (range 20–80 years). Regarding endoscopic and pathological findings, 52 patients had non-ulcer dyspepsia (NUD), 18 had peptic ulcer disease (PUD), 11 had intestinal metaplasia (IM), and 1 had gastric cancer (GC). Table 2 summarizes the demographic characteristics of the patients in different clinical diagnosis groups.
Clarithromycin Resistance of H. pylori Strains
The bacterial DNA samples were further used as a template for PCR reaction to identify H. pylori by amplification of 16S rRNA and glmM genes (Table 1). Accordingly, the clarithromycin resistance in 82 H. pylori strains was evaluated and their MIC values were recorded using the agar dilution method. By examining the MIC values, it can be inferred that 36 (43.9%) H. pylori strains were resistant to clarithromycin, whereas 42 (51.2%) strains showed susceptibility to this antimicrobial agent. Four (4.9%) strains were designated as intermediate ones. The MIC value of 16 mg/L was found as the most frequent breakpoint observed among the resistant strains, followed by MIC values of 1, 2, and 8 mg/L. The MIC values of 0.25 mg/L and 16 mg/L were determined as the MIC50 and MIC90 values, respectively. The frequency and distribution of MIC values for clarithromycin among H. pylori strains with respect to clinical diagnosis is presented in Table 3. The rate of resistance to clarithromycin was higher for the strains isolated from patients with PUD than NUD and IM patients. Frequency and distribution of clarithromycin resistance among H. pylori isolates in relation to different clinical diagnosis groups are shown in Table 4.
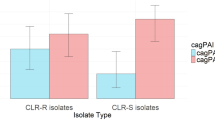
Association Between Virulence Genotypes and Clarithromycin Resistance
The resistant and susceptible clinical isolates were examined for the virulence factors of H. pylori including cagA, dupA, babA, sabA, and vacA (both allelic types: s and m regions). It can be seen clearly from the molecular results (Table 4) that the prevalence of babA and cagA genes were higher than others. In fact, these two genes were determined in 92.7% and 82.9% of the clinical isolates, respectively. When it comes to vacA, the prevalence of vacA s1m2 genotype was highest in the present study at 52.4%, while the least prevalent allelic combination was vacA s2m2 at 4.9%, and the vacA s1m1 combination was detected in 42.7% of the strains. sabA- and dupA-positive strains were found among 78% and 70.7% of the strains, respectively. Table 4 compares the data on the distribution of H. pylori genotypes among four groups of the patients. We failed to find a link between the prevalence of the virulence genotypes and clarithromycin susceptibility (P > 0.05). In addition, the statistical analysis from this study found no significant correlation between clarithromycin susceptibility rate and different age and sex groups with various clinical diagnoses (P > 0.05).
Sequence Analysis of 23S rRNA Gene Mutations
Regarding sequencing analysis in the present study, point mutations in the 23S rRNA gene were identified in 48 H. pylori isolates including 25 clarithromycin-resistant isolates, 22 clarithromycin-sensitive isolates, and one isolate with intermediate susceptibility. Moreover, the 23S rRNA gene was partially sequenced in two strains due to poor quality of sequence data or sequencing errors.
As shown in Supplementary Fig. 1, we observed 23 point mutations in the 23S rRNA gene sequence of the over-mentioned isolates. The list of point mutations in the 23S rRNA gene of H. pylori isolates is presented in Table 5. The type of mutations detected in the present study was not limited to A2142G and A2143G. Although the most prevalent mutations in clarithromycin-resistant isolates were A2143G (4/48, 8.3%) and A2142G (3/48, 6.2%), other point mutations including G2220T, T2221C, A2624C, C2248T, C2195T, T2182C, and C2288T were also detected with lower prevalence. In addition, some other single point mutations including G2287A, T2188C, G2710C, T2182C, C2248T, G2269A, G2224T, and C2694A were detected in clarithromycin-susceptible isolates. Apart from point mutations in the 23S rRNA gene, a transition T2244C and insertion of C nucleotide in position 2345 were observed in all clinical isolates including susceptible and resistant strains. Among the aforementioned point mutations, G2220T, C2248T, A2624C, G2287A, T2188C, G2710C, C2248T, G2269A, and G2224T were detected as novel point mutations.
Phylogenetic Analysis of 23S rRNA Gene
As might have been expected, the 23S rRNA gene is a highly conserved structure and no specific clustering in the phylogenetic tree was seen as a result. Figure 1 shows a clear illustration of similarities and discrepancies of 23S rRNA gene in different isolates based on the nucleotide sequence. However, strains with point mutations including A2142G and A2143G are classified in two separate clusters and the third branch implied to other point mutations in 23S rRNA gene sequence. The nucleic acid sequence of the 23S rRNA gene and the relevant point mutations were deposited with GenBank/NCBI database under accession numbers MH588172 to MH588219.
Phylogenetic tree of H. pylori clinical strains based on 23S rRNA nucleotide sequences (n = 43). Maximum likelihood tree of concatenated sequences was constructed using MEGA7 software with bootstrap method at 1000 replications. The evolutionary distances were computed using the Tamura 3-parameter model
Discussion
Clarithromycin is the main component of the first-line treatment regimens for H. pylori infection [25]. However, World Health Organization (WHO, 2017) presented clarithromycin-resistant H. pylori in the category of high priority which demands thoughtful and profound attention on eradication regimens for this problematic infection [26, 27]. Highlighting the importance of clarithromycin-resistant H. pylori, we decided to study the prevalence and the main mechanisms involved in clarithromycin resistance among clinical isolates of H. pylori. Regarding the Bangkok Consensus Report, the clarithromycin resistance rate is considered high when it exceeds 10–15%. Based on this statement, it can distinguish geographical regions into high- and low-resistance areas [28]. Thus, it can be inferred that region studied in present study is a high-resistance area with 43.9% clarithromycin-resistant strains, which showed an upward trend to our previous investigation with 33.8% of H. pylori resistance to clarithromycin [20].
With respect to a recent meta-analysis by Savoldi et al. [4], the high prevalence of primary clarithromycin resistance was observed in the Western Pacific Region (34%) and Eastern Mediterranean Region (33%). Regarding clarithromycin-resistant H. pylori in Europe, it was estimated to be more than 15%, whereas the lowest prevalence of clarithromycin resistance was assessed for Americas Region and the South-East Asia Region with similar primary resistant pattern (10%).
Increasing evidence supports a rising concern about the global resistance rate of clarithromycin among H. pylori strains. For instance, assessment of H. pylori primary antibiotic resistance in the Asia–Pacific region was performed by Kuo et al. [29]. This study revealed that the overall prevalence of resistance to clarithromycin was 17%, and total antibiotic resistance soared from 7% before 2000 to 21% in 2011–2015. With regards to studies from Iran, the overall prevalence of clarithromycin-resistant H. pylori strains has been reported to be 14.7%. The lowest and the highest resistance rates belonged to Rasht and Kashan with 5.5% to 33.7%, respectively [30]. A similar conclusion was reached by Hakemi Vala et al. [31] who reported that 21.7% of the H. pylori isolates were resistant to clarithromycin, whilst our findings in Tehran, the same city, revealed a notably higher resistance rate (43.9%). These findings extend our knowledge that clarithromycin resistance has been increasing during a period and as a consequence, the efficacy of clarithromycin-based treatment will be dramatically decreased. In the face of such an increasing trend, the third Maastricht consensus conference drew attention to the fact that the eradication rate of H. pylori should be more than 80% for an intention-to-treat analysis if a promising treatment is considered [25]. With reference to Hellenic consensus, treatment regimens for H. pylori should be based on regional antibiotic resistance rates and individual consumption of antibiotics [32].
When it comes to the point mutations responsible for clarithromycin resistance, frequent mutations in the gene encoding 23S rRNA have been discussed by a great number of authors in the literature. There is also accumulating evidence that single point mutations including A2143G (69.8%), A2142G (11.7%), and A2142C (2.6%) are the most common alterations seen in 23S rRNA sequence [32, 33], which is in line with our findings. In our study, seven isolates were found to harbor A2142G and A2143G mutations, whilst no A2142C mutation was seen among the resistant isolates. Furthermore, we identified a number of other mutations including G2220T, T2221C, A2624C, C2248T, C2195T, T2182C, and C2288T in addition to the most frequent ones. Matta et al. [33] reported the mutations A2144G, T2183C, and C2196T in clinical practice for the first time in Colombia, whereas none of those mutations were observed in the present study. Versalovic et al. [34] observed that 91.5% of clarithromycin-resistant isolates of H. pylori carried either the A2143G (formerly A2058G) or the A2144G (formerly A2059G) mutations in the gene encoding 23S rRNA. According to their findings, the majority of A2143G mutations were present in isolates with MICs more than 64 mg/L. On the contrary, the highest MIC in the present study was 16 mg/L. A similar pattern of results was obtained by Keshavarz Azizi Raftar et al. [35] who found A2143G with the prevalence of 66.7% among clarithromycin-resistant H. pylori. However, the high existence of A2143G may increase the concerns regarding treatment failure. In agreement with these studies, those sequences with mutations A2143G had the highest MIC (16 mg/L) among our clarithromycin-resistant strains. An interesting finding of our study was that several sequences of clarithromycin-resistant H. pylori were devoid of any mutations, indicating other potential mechanisms such as efflux pumps may be involved in clarithromycin resistance [36]. To the best of our knowledge, single point mutations including G2220T, A2624C, G2287A, T2188C, G2710C, C2248T, G2269A, and G2224T are considered as putative point mutations involved in clarithromycin resistance. Thus, further studies are required to assess the role of these mutations in the development of clarithromycin resistance among H. pylori strains.
Regarding the global prevalence of H. pylori and antibiotic resistance, a growing amount of resources are being devoted to analyses of virulence factors and antibiotic resistance between H. pylori strains. One of these main virulence factors is vacA, which carries two variable regions including the signal sequence (s) and middle region (m). The vacA s1 genotype is associated with PUD and the most virulent type of vacA s1m1 is related to gastric carcinoma, whereas inactive toxin is produced by the s2m2 allelic type [37]. Other findings provide evidence for the prevalence of vacA among H. pylori isolates as allelic combinations s1m1, s2m2, and s1m2 or s2m1 in 57.7%, 33.3%, and 4.4%, respectively [38]. It is interesting to note that the existence of s1m1 is more probable in patients with peptic ulcer in Western countries [39]. Conversely, in our study the allelic combination s1m2 had the highest prevalence and it was more common in those patients who suffered from NUD. Furthermore, H. pylori strains which are cagA-genopositive and carry vacA s1m1 concurrently, increase the risk of gastric precancerous lesions by roughly 4.8-fold in infected patients in comparison with those who were infected with cagA-negative/vacA s2m2 strains [15]. Although no significant correlation was found between antibiotic susceptibility and virulence factors in the present study, there exists a considerable body of literature on association of primary clarithromycin resistance with less virulent strains of H. pylori (cagA-negative and vacA s2) [40]. Additionally, Elviss et al. [41] argued that clarithromycin susceptibility in H. pylori was related with vacA s1m2 genotype. Intriguingly, Khani et al. [42] reported clarithromycin-susceptible H. pylori strains harbored the most virulent profile (cagA+/vacA s1m1+).
In a recent study by Farzi et al. [20], the vacA s1m2 genotype was the most common allelic type which was found to be correlated with PUD. Their results also showed that other vacA alleles including s1m1 and s2m2 genotypes were observed in 27.9% and 26.5% of the isolates, respectively. As might be reasonably expected, the concurrent expression of multiple virulence genes can escalate the risk of a severe gastric disorder [43]. Indeed, the decrease of babA expression can be contributed to higher incidence of gastrointestinal damages [3]. With reference to dupA, findings have shown a clear-cut positive correlation between the presence of dupA gene with increased risk of duodenal ulcer [15]. It follows the fact that clarithromycin resistance rate was ordinarily lower in the dupA-positive in contrast to dupA-negative group [44]. As for sabA, the frequency of this gene in H. pylori strains was 100%, 86.7%, and 83.3% in patients with gastric cancer, gastric ulcer, and both gastritis and duodenal ulcer, respectively [45]. There is still considerable controversy surrounding the association between H. pylori strains and clinical outcome. The recent data firmly established that no meaningful association was perceived among pathogenicity and antibiotic resistance or susceptibility which is completely in agreement with the present study [18, 46]. Despite the present study has successfully determined the prevalence of H. pylori virulence factors as well as molecular detection of clarithromycin resistance-associated mutations, it has some important limitations. First, a limited number of H. pylori 23S rRNA sequences were sequenced in this work. Thus, further investigations using a large cohort of isolates are necessary to determine additional mutations which are responsible for resistance to clarithromycin by themselves or in combination. Also, there could be other possible mechanisms involved in clarithromycin resistance that were not evaluated in the present study.
Conclusion
In summary, the prevalence of clarithromycin-resistant H. pylori isolates has been reaching a worrying level in Iran. Our findings revealed the presence of several point mutations in the 23S rRNA gene of H. pylori clinical isolates which may be associated with acquisition of resistance to clarithromycin. Additionally, the present data showed a high prevalence of H. pylori virulence factors among Iranian patients. Taken together, antimicrobial surveillance should be performed frequently to monitor the current susceptibility patterns and its alterations in each geographical region. Accordingly, it provides a strong empirical evidence for clinicians to replace clarithromycin or apply a potential combination of antibiotics to get the best results. Though, from the epidemiological point of view, it is important to be aware of the distribution of virulence factors in H. pylori isolates. Further studies using local surveillance networks are required to choose appropriate H. pylori eradication regimens for each region.
Data Availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
Kuo C-H, Hu H-M, Kuo F-C, Hsu P-I, Chen A, Yu F-J (2009) Efficacy of levofloxacin-based rescue therapy for Helicobacter pylori infection after standard triple therapy: a randomized controlled trial. J Antimicrob Chemother 63(5):1017–1024
Singh V, Mishra S, Maurya P, Rao G, Jain AK, Dixit VK (2009) Drug resistance pattern and clonality in H. pylori strains. J Infect Dev Countries 3(02):130–136
Ansari S, Yamaoka Y (2017) Helicobacter pylori BabA in adaptation for gastric colonization. World J Gastroenterol 23(23):4158
Savoldi A, Carrara E, Graham DY, Conti M, Tacconelli E (2018) Prevalence of antibiotic resistance in Helicobacter pylori: a systematic review and meta-analysis in World Health Organization regions. Gastroenterol 155(5):1372–1382
Arslan N, Yılmaz Ö, Demiray-Gürbüz E (2017) Importance of antimicrobial susceptibility testing for the management of eradication in Helicobacter pylori infection. World J Gastroenterol 23(16):2854
Vianna JS, Ramis IB, Ramos DF, Von Groll A, Silva PEAd (2016) Drug resistance in Helicobacter pylori. Arq Gastroenterol 53(4):215–223
Malfertheiner P, Megraud F, O’Morain CA, Atherton J, Axon AT, Bazzoli F (2012) Management of Helicobacter pylori infection: the Maastricht IV/Florence consensus report. Gut 61(5):646–664
Schmitt BH, Regner M, Mangold KA, Thomson RB Jr, Kaul KL (2013) PCR detection of clarithromycin-susceptible and-resistant Helicobacter pylori from formalin-fixed, paraffin-embedded gastric biopsies. Mod Pathol 26(9):1222–1227
Marques AT, Vítor JMB, Santos A, Oleastro M, Vale FF (2020) Trends in Helicobacter pylori resistance to clarithromycin: from phenotypic to genomic approaches. Microb Genom 6(3):e000344
Agudo S, Pérez-Pérez G, Alarcón T, López-Brea M (2010) High prevalence of clarithromycin-resistant Helicobacter pylori strains and risk factors associated with resistance in Madrid, Spain. J Clin Microbiol 48(10):3703–3707
Chen J, Ye L, Jin L, Xu X, Xu P, Wang X (2018) Application of next-generation sequencing to characterize novel mutations in clarithromycin-susceptible Helicobacter pylori strains with A2143G of 23S rRNA gene. Ann Clin Microbiol Antimicrob 17(1):10
Thung I, Aramin H, Vavinskaya V, Gupta S, Park J, Crowe S (2016) The global emergence of Helicobacter pylori antibiotic resistance. Aliment Pharm Ther 43(4):514–533
Lee JY, Kim N, Kim MS, Choi YJ, Lee JW, Yoon H (2014) Factors affecting first-line triple therapy of Helicobacter pylori including CYP2C19 genotype and antibiotic resistance. Dig Dis Sci 59(6):1235–1243
Malfertheiner P, Megraud F et al (2017) Management of Helicobacter pylori infection—the Maastricht V/Florence consensus report. Gut 66(1):6–30
Chang W-L, Yeh Y-C, Sheu B-S (2018) The impacts of H. pylori virulence factors on the development of gastroduodenal diseases. J Biomed Sci 25(1):1–9
Yadegar A, Mohabati Mobarez A, Zali MR (2019) Genetic diversity and amino acid sequence polymorphism in Helicobacter pylori CagL hypervariable motif and its association with virulence markers and gastroduodenal diseases. Cancer Med 8(4):1619–1632
Boyanova L, Markovska R, Yordanov D, Gergova G, Mitov I (2016) Clarithromycin resistance mutations in Helicobacter pylori in association with virulence factors and antibiotic susceptibility of the strains. Microb Drug Resist 22(3):227–232
Oktem-Okullu S, Cekic-Kipritci Z, Kilic E, Seymen N, Mansur-Ozen N, Sezerman U (2020) Analysis of correlation between the Seven Important Helicobacter pylori (H. pylori) Virulence Factors and Drug Resistance in Patients with Gastritis. Gastroenterol Res Prac. https://doi.org/10.1155/2020/3956838
Yadegar A, Mobarez AM, Alebouyeh M, Mirzaei T, Kwok T, Zali MR (2014) Clinical relevance of cagL gene and virulence genotypes with disease outcomes in a Helicobacter pylori infected population from Iran. World J Microbiol Biotechnol 30(9):2481–2490
Farzi N, Yadegar A, Sadeghi A, AsadzadehAghdaei H, MarianSmith S, Raymond J (2019) High prevalence of antibiotic resistance in Iranian Helicobacter pylori Isolates: importance of functional and mutational analysis of resistance genes and virulence genotyping. J Clin Med 8(11):2004
Yadegar A, Alebouyeh M, Lawson AJ, Mirzaei T, Mojarad EN, Zali MR (2014) Differentiation of non-pylori Helicobacter species based on PCR–restriction fragment length polymorphism of the 23S rRNA gene. World J Microbiol Biotechnol 30(6):1909–1917
Farzi N, Yadegar A, Aghdaei HA, Yamaoka Y, Zali MR (2018) Genetic diversity and functional analysis of oipA gene in association with other virulence factors among Helicobacter pylori isolates from Iranian patients with different gastric diseases. Infect Genet Evol 60:26–34
Hall TA (1999) editor BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic acids symposium series [London]: Information Retrieval Ltd., c1979-c2000.
Kumar S, Stecher G, Tamura K (2016) MEGA7: molecular evolutionary genetics analysis version 7.0 for bigger datasets. Mol Biol Evol 33(7):1870–1874
Sezgin O, Aydın MK, Özdemir AA, Kanık AE (2019) Standard triple therapy in Helicobacter pylori eradication in Turkey: systematic evaluation and meta-analysis of 10-year studies. Turk J Gastroenterol 30(5):420
Abadi ATB (2017) Resistance to clarithromycin and gastroenterologist’s persistence roles in nomination for Helicobacter pylori as high priority pathogen by World Health Organization. World J Gastroenterol 23(35):6379
Tacconelli E, Carrara E, Savoldi A, Harbarth S, Mendelson M, Monnet DL (2018) Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis 18(3):318–327
Graham D (2018) H. pylori Management in ASEAN: the Bangkok Consensus Report. J Gastroenterol Hepatol 33(1):37–56
Kuo Y-T, Liou J-M, El-Omar EM, Wu J-Y, Leow AHR, Goh KL (2017) Primary antibiotic resistance in Helicobacter pylori in the Asia-Pacific region: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2(10):707–715
Khademi F, Sahebkar AH, Vaez H, Arzanlou M, Peeridogaheh H (2017) Characterization of clarithromycin-resistant Helicobacter pylori strains in Iran: a systematic review and meta-analysis. J Glob Antimicrob Resist 10:171–178
Vala MH, Eyvazi S, Goudarzi H, Sarie HR, Gholami M (2016) Evaluation of clarithromycin resistance among Iranian Helicobacter pylori isolates by E-test and real-time polymerase chain reaction methods. Jundishapur J Microbiol 9(5):e60063
Georgopoulos SD, Michopoulos S, Rokkas T, Apostolopoulos P, Giamarellos E, Kamberoglou D (2020) Hellenic consensus on Helicobacter pylori infection. Ann Gastroenterol 33(2):105
Matta AJ, Zambrano DC, Pazos AJ (2018) Punctual mutations in 23S rRNA gene of clarithromycin-resistant Helicobacter pylori in Colombian populations. World J Gastroenterol 24(14):1531
Versalovic J, Osato MS, Spakovsky K, Dore MP, Reddy R, Stone GG (1997) Point mutations in the 23S rRNA gene of Helicobacter pylori associated with different levels of clarithromycin resistance. J Antimicrob Chemother 40(2):283–286
Keshavarz Azizi Raftar S, Moniri R, Saffari M, Razavi Zadeh M, Arj A, Mousavi SGA (2015) The Helicobacter pylori resistance rate to clarithromycin in Iran. Microb Drug Resist 21(1):69–73
Iwamoto A, Tanahashi T, Okada R, Yoshida Y, Kikuchi K, Keida Y (2014) Whole-genome sequencing of clarithromycin resistant Helicobacter pylori characterizes unidentified variants of multidrug resistant efflux pump genes. Gut Pathog 6(1):27
Taneike I, Nami A et al (2009) Analysis of drug resistance and virulence-factor genotype of Irish Helicobacter pylori strains: is there any relationship between resistance to metronidazole and cagA status? Aliment Pharmacol Ther 30(7):784–790
Garcia GT, Aranda KR, Gonçalves ME, Cardoso SR, Iriya K, Silva NP (2010) High prevalence of clarithromycin resistance and cagA, vacA, iceA2, and babA2 genotypes of Helicobacter pylori in Brazilian children. J Clin Microbiol 48(11):4266–4268
Feliciano O, Gutierrez O, Valdés L, Fragoso T, Calderin AM, Valdes AE (2015) Prevalence of Helicobacter pylori vacA, cagA, and iceA genotypes in Cuban patients with upper gastrointestinal diseases. BioMed Res Int. https://doi.org/10.1155/2015/753710
Brennan DE, Dowd C, O’Morain C, McNamara D, Smith SM (2018) Can bacterial virulence factors predict antibiotic resistant Helicobacter pylori infection? World J Gastroenterol 24(9):971
Karabiber H, Selimoglu MA, Otlu B, Yildirim O, Ozer A (2014) Virulence factors and antibiotic resistance in children with Helicobacter pylori gastritis. J Pediatr Gastr Nutr 58(5):608–612
Khani S, Abadi ATB, Mobarez AM (2019) Clarithromycin-susceptible but virulent Helicobacter pylori strains infecting Iranian patients’ stomachs. Infect Drug Resist 12:3415
Šterbenc A, Jarc E, Poljak M, Homan M (2019) Helicobacter pylori virulence genes. World J Gastroenterol 25(33):4870
Shiota S, Nguyen LT, Murakami K, Kuroda A, Mizukami K, Okimoto T (2012) Association of helicobacter pylori dupA with the failure of primary eradication. J Clin Gastroenterol 46(4):297
Pakbaz Z, Shirazi MH, Ranjbar R (2013) Frequency of sabA gene in Helicobacter pylori strains isolated from patients in Tehran, Iran. Iran Red Crescent Med J 15(9):767
Godoy APO, Ribeiro ML, Benvengo YHB, Vitiello L, Miranda MdCB, Mendonça S (2003) Analysis of antimicrobial susceptibility and virulence factors in Helicobacter pylori clinical isolates. BMC Gastroenterol 3(1):20
Acknowledgements
The authors would like to thank the sample collection team at Taleghani hospital and the staffs in Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Funding
This study was financially supported by a research grant (no. RIGLD 878) from Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Author information
Authors and Affiliations
Contributions
HA performed the susceptibility testing and PCR assay for H. pylori strains. NM provided the draft of the manuscript. AY worked on concept and design of the study, data analysis and interpretation, and writing of manuscript. AY and KB performed the sequence analysis. AY and SMS critically revised the manuscript. AS and MRZ provided clinical consultation for the study. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical Approval
The study protocol was approved by the Institutional Ethical Review Committee of the Research Institute for Gastroenterology and Liver Diseases at Shahid Beheshti University of Medical Sciences (Project No. IR.SBMU.RIGLD.REC.1395.878).
Consent to Participate
All participants and/or their legal guardians signed written informed consent before enrollment in the study.
Consent for Publication
All authors approved the final version of the manuscript and the authorship list.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the Supplementary Information.
Rights and permissions
About this article
Cite this article
Alavifard, H., Mirzaei, N., Yadegar, A. et al. Investigation of Clarithromycin Resistance-Associated Mutations and Virulence Genotypes of Helicobacter pylori Isolated from Iranian Population: A Cross-Sectional Study. Curr Microbiol 78, 244–254 (2021). https://doi.org/10.1007/s00284-020-02295-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-020-02295-7