Abstract
PPE68 is a Mycobacterium tuberculosis-specific protein which is absent from the vaccine strains of BCG. A panel of 14 PPE68-derived peptides predicted to bind to HLA-A*0201 was synthesized. The HLA-A*0201 restriction of these peptides was determined in T2 cell line and HLA-A*0201 transgenic mice. The specificity of peptides was assessed in pulmonary tuberculosis (TB) patients using IFN-γ enzyme-linked immunospot (ELISPOT) assay, and immunodominant peptides were further used to evaluate their diagnostic potential in HLA-A*0201-positive pulmonary TB patients. 13 out of 14 peptides were identified as high-affinity binders. Of these peptides, 12 peptides induced significant IFN-γ-secreting T cell response in transgenic mice and 9 peptides were efficiently recognized by peripheral blood mononuclear cells of 10 HLA-A*0201-positive TB patients. Four immunodominant HLA-A*0201-restricted epitopes (PPE68126–134, PPE68133–141, PPE68140–148, and PPE68148–156) were recognized by the most of 80 HLA-A*0201-positive TB patients (81, 86, 74, and 84 %, respectively). These epitopes may be used for a potential diagnosis of M. tuberculosis infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis (TB), caused by Mycobacterium tuberculosis (M. tuberculosis), is still a major public health problem [25]. At present, one-third of the world’s population has been infected with M. tuberculosis. In 2013, there were an estimated 9 million new cases of TB and 1.5 million people died from TB, including more than one million deaths among HIV-negative individuals and 360,000 among HIV-positive people [31]. In China, about one million new cases of active TB are reported each year according to the national wide TB survey in 2013 [31]. Although Bacille Calmette Guerin (BCG) has been used for almost a century, the protective efficacy of BCG is highly variable and limited. Currently, the main strategies pursued to improve TB control are accurate diagnosis, efficient drug treatment, and the development of a new effective TB vaccine. The traditional diagnostic methods for TB include sputum culture, polymerase chain reaction (PCR), tuberculin skin test (TST), etc. However, M. tuberculosis culture and PCR depend on a certain bacterial load. The most widely used TST is purified protein derivative (PPD) assay, which has been an important tool for detecting TB infection (both latent and active TB). However, because of cross reaction to proteins from BCG and nontuberculous mycobacteria, PPD assay has several drawbacks such as poor specificity and limited sensitivity in TB diagnosis [10, 12]. False-positive results are common because of environmental mycobacterial exposure and previous BCG vaccination. Therefore, the limitations of the TST indicate the need for an improved approach to the diagnosis of TB infection. Therefore, M. tuberculosis-specific antigens could be an alternative approach for the immunological diagnosis of TB.
Previous studies indicated that all clinical isolates of M. tuberculosis and M. bovis have a unique Region of difference 1 (RD-1) which is absent in all vaccine strains of BCG [3]. RD1 region contains genes encoding a specific number of proteins, including early secretory antigen target 6 (ESAT-6), culture-filtered protein 10 (CFP-10), PPE68, etc. [3, 18]. EAST-6 and CFP-10 have been intensively investigated and identificated as strong targets of the cellular immune response in TB patients and outstanding diagnostic targets for TB diagnosis [10, 19]. In addition, ESAT-6- and CFP-10-based diagnostic reagent such as T-SPOT.TB assay has been released to the market for clinical diagnosis of TB [17, 26]. However, the sensitivity obtained with these proteins is insufficient [17, 26]. Thus, it is necessary to find other antigens with diagnostic potential.
PPE68 (368 aa, encoded by Rv3873) is a membrane protein expressed on the surface of M. tuberculosis and M. tuberculosis-infected cells [8]. The ability of PPE68 inducing high levels of IFN-γ secretion by T cells of TB patients supports the usefulness of PPE68 as an antigen with diagnostic potential [15, 18, 19]. However, the cross reactivity between PPE68 and proteins from BCG and environmental mycobacterial strains may restrict its application in TB diagnosis [4, 15, 19]. The cross reaction would lead to false-positive reactions and may be resolved using highly specific PPE68-specific T cell epitopes.
HLA-A*0201 is a common HLA-A allele with a frequency of over 30 % in most populations irrespective of gender or ethnicity [5]. The study presented herein was designed to identify PPE68-derived HLA-A*0201-binding peptides and evaluate IFN-γ-secreting T cell responses to these peptides in HLA-A*0201 transgenic mice and TB patients. Fourteen putative PPE68-derived HLA-A*0201-binding peptides were selected and tested by ex vivo MHC-peptide complex stabilization assay and IFN-γ enzyme-linked immunospot (ELISPOT) assay. Four highly sensitive PPE68-specific HLA-A*0201-restricted epitopes were identified as a diagnostic candidates for human TB infection.
Materials and Methods
Prediction of T cell Epitopes in PPE68 Protein and Synthesis of Peptides
SYFPEITHI (http://www.syfpeithi.de/Scripts/MHCServer.dll/EpitopePrediction.htm) [23], a T cell epitope prediction algorithm, was used to predict HLA-A*0201-binding peptides within PPE68 protein of M. tuberculosis H37Rv strain (Genbank accession number: NP_857540). In addition, PAProc (http://www.paproc.de/) [14] was used to predict the potential human proteasomal cleavage sites within the predicted peptides. Epitope candidates were synthesized at ChinaPeptides Co., Ltd. (Shanghai, China) and purified to >95 % as confirmed by high-performance liquid chromatography and mass spectrometry. A universal Pan-DR Th epitope peptide (PADRE: AKFVAAWTLKAAA) was synthesized and used as a helper peptide. A dengue virus-derived HLA-A*0201-restricted CD8+ T cell epitope NS4b40–48(TLYAVATTI) was used as a positive control [30]. All peptides were dissolved in PBS to a concentration of 1 mM and stored at −20 °C until use.
Cell Line, Mice, and Study Subjects
The human transporter associated with antigen processing (TAP)-deficient T2 cell line was purchased from the American Type Culture Collection (Manassas, VA, USA). C57BL/6-Transgenic(HLA-A2.1)1Enge/J mice (HLA-A*0201 transgenic mice) were purchased from the Jackson Laboratory (Bar Harbor, ME, USA) and bred in specific pathogen-free conditions. One hundred sputum culture positive with PPD skin test and chest X-ray confirmed pulmonary TB patients (90 HLA-A*0201 positive, and 10 HLA-A*0201 negative, HLA-A*0201 was confirmed using the PCR sequence-specific primers [27]) (median age 48 ± 26 (22–76)) were recruited from the department of clinical laboratory, the third affiliated hospital of Wenzhou Medical University, China. Twenty healthy participants, BCG-vaccinated donors (median age 23 ± 2 (20–25)) with no known exposure to M. tuberculosis, were recruited from Wenzhou Medical University. All donors gave written informed consent before peripheral blood donation. Peripheral blood mononuclear cells (PBMCs) were isolated from heparinized blood using human lymphocyte density gradient centrifugation [11] and resuspended in RPMI-1640 medium supplemented with 2 Mm l-glutamine, 100 U/ml penicillin, 100 μg/ml streptomycin, and 10 % fetal bovine serum (FBS). The study was approved by the Human Research Ethics Board of Wenzhou Medical University.
MHC-Peptide Complex Stabilization Assay
To determine the affinity of peptides to HLA-A*0201 molecules, peptide-induced HLA-A*0201 up-regulation on T2 cells was measured as described previously [30]. Briefly, T2 cells (2 × 105 cells) were incubated in serum-free RPMI-1640 medium in the absence or presence of peptide (1, 10, 100 µM) for 1 h at 37 °C/5 % CO2 incubator. Cells were then incubated for 12 h at 26 °C, and returned to 37 °C for a 3 h incubation. Cells were stained with FITC-conjugated anti-HLA-A*0201 mAb (BD Pharmingen, CA, USA) for 40 min at 4 °C, and mean fluorescence intensity (MFI) was recorded with a FACS Calibur flow cytometer (BD bioscience, CA, USA). The fluorescence index (FI) was calculated as follows. Peptide with FI ≥1 (peptide concentration = 100 µM) was considered as high-affinity peptide [32], which means that this peptide could increase the expression of HLA-A*0201 molecules on T2 cells by at least 1-fold.
Immunization of HLA-A*0201 Transgenic Mice
Female HLA-A*0201 transgenic mice (6–8 weeks of age) were subdivided into 14 groups (4 mice/group). Mice were immunized subcutaneously with peptide (50 µg/mouse) and PADRE (50 µg/mouse) emulsified in complete Freund’s adjuvant (CFA). One week later, mice were boosted with the same peptide emulsified in Incomplete Freund’s adjuvant (IFA) for three additional times at weekly internals. In addition, control mice (mock-immunized mice) were immunized with CFA and IFA without peptide according to the same immunization protocol. One week after the fourth immunization, splenocytes and lymph node cells (from deltopectoral and popliteal lymph nodes) were prepared and tested using IFN-γ enzyme-linked immunospot (ELISPOT) assay. All animal experiments were performed following the Institutional Animal Care and Use Committee-approved protocols of Wenzhou Medical University.
Murine IFN-γ ELISPOT Assay
Murine IFN-γ ELISPOT assays were performed in pre-coated 96-well plates (U-CyTech Company, Utrecht, The Netherlands) according to the manufacture’s instructions. Firstly, splenocytes and lymph node cells were resuspended in RPMI-1640 medium, and adjusted to 5 × 106 cells/ml and 2 × 106 cells/ml, respectively. Splenocytes (5 × 105 cells/well) and lymph node cells (2 × 105 cells/well) were added to each well of the ELISPOT plates. Background control wells (without peptide) and test wells (with 10 µg/ml peptide) were set in duplicate wells. Subsequently, the plates were incubated for 24 h at 37 °C/5 % CO2 incubator and then incubated with biotinylated anti-mouse IFN-γ mAb for 1 h at 37 °C. Finally, plates were incubated with streptavidin-horseradish peroxidase, and developed using fresh ACE solution as a substrate. IFN-γ spots (Spot-forming cells, SFCs) were counted using an ELISPOT reader (Beijing SageCreation Science Co., Ltd. Beijing, China). Peptide-specific T cell frequency was expressed as IFN-γ SFCs/5 × 105 splenocytes or 2 × 105 lymph node cells.
Human IFN-γ ELISPOT Assay
Human IFN-γ ELISPOT kit (pre-coated 96-wells plates) was purchased from U-CyTech Company and the assay was performed as described above. In brief, PBMCs from 10 HLA-A*0201-positive TB patients, 10 HLA-A*0201-negative TB patients, and 20 healthy BCG-vaccinated donors were resuspended in RPMI-1640 medium and adjusted to 5 × 105 cells/ml. PBMCs (5 × 104 cells/well) were seeded into each well of the ELISPOT plates, and background control wells (without peptide) and test wells (with 10 µg/ml individual peptide) were set. After 24 h incubation at 37 °C, the plates were washed and processed as described above. IFN-γ SFCs were counted, and the frequency of peptide-specific T cells was expressed as IFN-γ SFCs/5 × 104 PBMCs. Responses to tested peptides were scored as positive if the number of IFN-γ spots was greater than 5 SFCs/5 × 104 PBMCs after subtraction of the background and this number also had to be at least twice the frequency found in the background wells [15].
Evaluation of the Sensitivity of Immunodominant PPE68-Derived Peptides
The sensitivity of 4 immunodominant PPE68-derived peptides (PPE68126–134, PPE68133–141, PPE68140–148, and PPE68148–156) was further evaluated in PBMCs of 80 additional HLA-A*0201-positive TB patients using human IFN-γ ELISPOT assay as described above (1 × 105 PBMCs/well). Meanwhile, the commercial ELISPOT-based T-SPOT.TB kit (containing ESAT-6 and CFP-10) was purchased from Oxford Immunotec Ltd. (Abingdon, UK) and used to detect the frequencies of ESAT-6- and CFP-10-specific IFN-γ-secreting T cells in PBMCs of 80 TB patients as described previously [17]. In brief, PBMCs (1 × 105 cells/well) were seeded into each well of the ELISPOT plates, background control wells (without proteins) and test wells (with ESAT-6 or CFP-10) were set in duplicate wells, and plates were incubated for 24 h at 37 °C/5 % CO2 incubator. The plates were washed and then incubated with alkaline phosphatase-conjugated anti-human IFN-γ mAb for 1 h at 37 °C. After a subsequent wash, the plates were developed using BCIP/NBT solution as a substrate. IFN-γ SFCs were counted using an ELISPOT reader and expressed as IFN-γ SFCs/1 × 105 PBMCs. Responses to tested peptides were scored as positive if the number of IFN-γ spots was greater than 5 SFCs/1 × 105 PBMCs after subtraction of the background and this number also had to be at least twice the frequency found in the background wells [15].
Statistical Analysis
Results were expressed as mean ± SEM. Student’s t test was used to determine the significant differences between the mean values of the experimental groups. P < 0.05 was considered significant.
Results
Affinity of Peptides to HLA-A*0201 Molecules
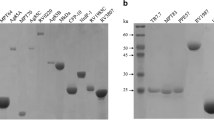
Epitope candidates were selected on the basis of the high predictive scores and proteasomal cleavage sites (C terminus). According to the prediction results, a panel of 14 peptides (each represents an epitope candidate) was synthesized (as shown in Table 1). BLAST results showed that PPE68126–134 is conserved in some PPE family proteins (PPE2, PPE3, PPE46, PPE47, and PPE66), while others have no sequence homology with any known mycobacterial proteins. Of 14 peptides, 8 peptides are nonapeptides, while other 6 peptides belong to decapeptides. Four overlapping peptides (PPE68126–134, PPE68133–141, PPE68140–149, and PPE68148–156) span a sequence (residues 126 to 156). MHC-peptide complex stabilization assay was used to measure the expression of HLA-A*0201 molecules on T2 cells induced by peptide exposure, with high-affinity peptides inducing HLA-A*0201 up-regulation more strongly than low-affinity peptides. FI ≥1 (peptide concentration = 100 μM) is a normally accepted threshold for high affinity [32]. As shown in Fig. 1 and Table 1, when peptide concentration reached 100 μM, of the 14 peptides, only PPE6826–34 was low-affinity peptide (FI = 0.65); other peptides and positive control peptide bound to HLA-A*0201 molecules with a FI ≥1.
The binding affinity of PPE68-derived peptides to HLA-A*0201 molecule. Based on T2 cells, MHC-peptide complex stabilization assay was used to evaluate the binding affinity of PPE68-derived CD8+ T cell epitope candidates and positive control (NS4b40–48) to HLA-A*0201 molecules as described in “Materials and Methods” section. T2 cells were incubated with individual peptides at the different concentrations [no peptide (red) or 1 μM (purple) or 10 μM (green) or 100 μM (blue)]. The mean fluorescence intensity of T2 cells was measured using flow cytometry and then the fluorescence index (FI) was calculated
Immunogenicity of Peptides in HLA-A*0201 Transgenic Mice
To test the potential immunogenicity of epitope candidates, HLA-A*0201 transgenic mice were immunized subcutaneously with individual peptides. Splenocytes and lymph node cells from immunized mice were restimulated in vitro with the corresponding peptide and the frequencies of peptide-specific IFN-γ-secreting cells were detected by IFN-γ ELISPOT assay. Positive control peptide elicited significant IFN-γ response. Of 13 high-affinity peptides, PPE6837–45 and PPE6844–52 did not elicit significant IFN-γ-secreting cells, while the other peptides induced high levels of IFN-γ-secreting cells in both spleen (Fig. 2a) and lymph nodes (Fig. 2b). Among 14 epitope candidates, PPE68299–308 immunization induced the highest frequency of IFN-γ-secreting cells in both spleen and lymph nodes (307 ± 23 SFCs/5 × 105 splenocytes; 174 ± 21 SFCs/2 × 105 lymph node cells) (Fig. 2a and b). In addition, there was no significant peptide-specific IFN-γ-secreting T cell response in mock-immunized transgenic mice (data not shown). Because HLA-A*0201 transgenic mice are produced on the basis of C57BL/6 mice, in order to determine if these fourteen epitope candidates could induce IFN-γ-secreting T cell response in C57BL/6 mice, the immunogenicity of fourteen peptides was evaluated in C57BL/6 mice and no significant IFN-γ responses were observed (data not shown).
Peptide-specific IFN-γ-secreting cells in splenocytes and lymph node cells of peptide-immunized HLA-A*0201 transgenic mice. Splenocytes and lymph node cells were isolated from peptide-immunized mice and were restimulated in vitro with no peptide or the same pepdide. The frequencies of IFN-γ SFCs/5 × 105 splenocytes (a) or IFN-γ SFCs/2 × 105 lymph node cells (b) were detected using ELISPOT assay and presented as mean ± SD (n = 4). Asterisk indicating the positive response to a pepdide
Identification of the Immunodominant PPE68-Specific HLA-A*0201-restricted Epitopes
To further determine whether these peptides are naturally processed and presented in human cells, PBMCs from 10 HLA-A*0201-positive TB patients were tested for their capacity to recognize peptide and secrete IFN-γ. PBMCs from each TB patients were stimulated with individual peptides, and the frequencies of peptide-specific IFN-γ-secreting cells were then detected by ELISPOT assay. As shown in Fig. 3b, the percentages of responding patients varied between 10 and 100 % for different peptides. Of 14 peptides, 9 peptides (PPE68148–156, PPE68133–141, PPE68166–174, PPE68126–134, PPE6864–73, PPE68200–209, PPE68105–114, PPE68140–149, and PPE68277–284) were recognized for at least 50 % of the TB patients. Notably, PPE68126–134, PPE68133–141, PPE68140–149, and PPE68148–156 were recognized by 100, 100, 80, and 90 % of the TB patients, respectively. The frequencies of peptide-specific IFN-γ-secreting cells specific for PPE68126–134, PPE68133–141, and PPE68148–156 were (median response and interquartile range) 18 (6–49), 18 (7–38), and 15 (1–37) per 5 × 104 PBMCs, respectively. Patients responded weakly to PPE68140–149 yielding relatively few spots (3–8 SFCs/5 × 104 PBMCs) (Fig. 3a). We next assessed the HLA-A*0201 restriction and specificity of PPE68-derived peptides by ELISPOT assay in 10 HLA-A*0201-negative TB patients and 20 HLA-A*0201-positive BCG-vaccinated donors. As shown in Fig. S1a, for HLA-A*0201-negative TB patients, the responders to PPE68-derived peptides, as well as the numbers of IFN-γ SFCs, were significantly lower than HLA-A*0201-positive TB patients. As expected, in the BCG-vaccinated individuals, the responses to peptides were absent (Fig. S1b). All of these results suggested that these four peptides (PPE68126–134, PPE68133–141, PPE68140–149, and PPE68148–156) represent the immunodominant PPE68-specific HLA-A*0201-restricted epitopes. These four peptides were then chosen as diagnostic peptides for subsequent experiments.
IFN-γ ELISPOT assay responses to peptides in PBMCs of HLA-A*0201-positive TB patients. a Frequencies of peptide-specific IFN-γ-secreting SFCs were enumerated by ELISPOT assay in 10 HLA-A*0201-positive TB patients. Each horizontal bar represents the median response for each peptide. The broken horizontal line represents the predefined cutoff point (5 SFCs/5 × 104 PBMCs). Points above the broken horizontal line represent individuals with a positive response to a give peptide, b Percentages of HLA-A*0201-positive TB patients who responded to each peptide
Diagnostic Potential of Immunodominant PPE68-Specific HLA-A*0201-restricted Epitopes
To test the diagnostic potential of the PPE68-specific HLA-A*0201-restricted epitopes, the immunodominant peptides including PPE68126–134, PPE68133–141, PPE68140–149, and PPE68148–156 were selected for diagnostic test in 80 HLA-A*0201-positive TB patients. To compare the relative sensitivity of above peptides in TB diagnosis, ESAT-6 and CFP-10 (components of T-SPOT.TB kit) were used as positive controls. The IFN-γ ELISPOT assay responses to 4 PPE68-derived peptides, ESAT-6 and CFP-10 are summarized in Fig. 4a. The percentages of responding patients for PPE68126–134, PPE68133–141, PPE68140–149, PPE68148–156, ESAT-6, and CFP-10 were 81, 86, 74, 84, 88, and 84 %, respectively (Fig. 4b). The frequencies of peptide-specific IFN-γ-secreting cells for all responding patients were (median response and interquartile range) 39 (7–132), 34 (7–111), 26 (5–88), 44 (6–142), 47 (5–128), and 51 (7–183) per 1 × 105 PBMCs, respectively (Fig. 4a).
IFN-γ ELISPOT assay responses to four peptides and two proteins in PBMCs of HLA-A*0201-positive TB patients. a The frequencies of four peptides (PPE68126–134, PPE68133–141, PPE68140–149, and PPE68148–156) and two proteins (ESAT-6 and CFP-10)-specific IFN-γ-secreting SFCs in 80 additional HLA-A*0201-positive TB patients were detected using ELISPOT assay and T-SPOT.TB assay, respectively. Each horizontal bar represents the median response for each peptide. The broken horizontal line represents the predefined cutoff point (5 SFCs/l × 105 PBMCs). Points above the broken horizontal line represent individuals with a positive response to a give peptide. b Percentages of HLA-A*0201-positive TB patients who responded to each peptide
Discussions
Mycobacterium tuberculosis infection is routinely being detected by TST against PPD, a crude extract from M. tuberculosis. This test has poor specificity, due to cross reaction with environmental mycobacteria and vaccination with BCG. New in vitro T cell-based interferon-γ release assays (IGRAs), which utilize M. tuberculosis-specific antigens, have been introduced into clinical diagnosis in recent years [22, 24]. At present, there are two available IGRAs: the QuantiFERON-TB Gold In-Tube test (QFT-GIT) and T-SPOT.TB test. T-SPOT.TB assay (ELISPOT-based IGRAs) contains a mixture of couples of epitopes derived from ESAT-6 and CFP-10, and determines the number of INF-γ-secreting cells with the use of an ELISPOT assay [16]. Although T-SPOT.TB improved the specificity for the diagnosis of TB, its sensitivity is insufficient [6, 17, 26]. Recent study indicated potentials for further improvement of this test [2]. Therefore, it has been of interest to search fine epitopes from other antigens and improve the diagnosis of TB.
In the present study, we sought out to identify a few immunodominant PPE68-derived HLA-A*0201-restricted epitopes that have both high specificity and sensitivity in TB diagnosis. 13 of 14 PPE68-derived epitope candidates bound to HLA-A*0201 molecules with high affinity, and 12 peptides induced IFN-γ-secreting cells in HLA-A*0201 transgenic mice. However, two high-affinity peptides, PPE6837–45 and PPE6844–52, did not induce significant IFN-γ-secreting cell response in transgenic mice. Conversely, one low-affinity peptide, PPE6826–34, elicited significant IFN-γ release. The possible explanations may be (1) neither PPE6837–45 nor PPE6844–52 is cross-presented to CD8+ T cells as for other antigens [21], so they could not induce IFN-γ response; (2) both PPE6837–45 and PPE6844–52 have higher dissociation rates from HLA-A*0201 molecules than other high-affinity peptides. In contrast, PPE6826–34 might has low dissociation rates from HLA-A*0201 molecules. Indeed, many studies have indicated that there is no strict correlation between functional activity of peptides and their HLA binding efficiency [1, 28]. High-affinity peptides did not always induce immune response [9, 13], whereas low-affinity peptides triggered CD8+ T cell response [29].
To know if these peptides could be processed and presented in human cells, 14 peptides were further tested in ex vivo IFN-γ ELISPOT assay in 10 HLA-A*0201-positive patients with active pulmonary TB. Nine PPE68-derived peptides were recognized by PBMCs from >50 % of the patients tested. 100, 100, 80, and 90 % of the TB patients responded to PPE68126–134, PPE68133–141, PPE68140–149, and PPE68148–156, respectively, identifying these overlapping peptides as immunodominant epitopes in humans. Although PPE68126–134 was recognized by one HLA-A*0201-negative individual, no significant IFN-γ T cell response to peptides could be detected in all BCG-vaccinated donors tested. Therefore, these peptides showed an excellent specificity for discrimination between HLA-A*0201-positive active TB patients and BCG-vaccinated donors. Subsequently, by the same approaches, we investigated the diagnostic performance of epitope-based ELISPOT assay for TB diagnosis and our study has highlighted the immunodominance of these four overlapping peptides in 80 HLA-A*0201-positive pulmonary TB patients. The sensitivities of 4 peptides each in TB diagnosis are 81, 86, 74, and 84 %, respectively. Given ESAT-6- and CFP-10-based diagnostic reagent (T-SPOT.TB assay) has been released to the market for clinical diagnosis of TB [17], we compared these four peptides with ESAT-6 and CFP-10 for the sensitivity in TB diagnosis. The sensitivity of epitope-based ELISPOT assay was similar to that of ESAT-6- and CFP-10-based T-SPOT.TB assay (88 and 84 %, respectively) in the present study. In total, the differences between these four peptides and ESAT-6 and CFP-10 are not so significant either in terms of proportion of responders or the frequencies of IFN-γ-secreting cells.
In the last decade, although some researchers have described some PPE68-derived peptides which could elicit IFN-γ-secreting cells and explored their potential diagnostic role in TB, no CD8+ T cell epitope has ever been reported. For example, PPE68118–135 (VLTATNFFGINTIPIALT) was identified as an immunodominant epitope which is recognized by both TB patients and BCG-vaccinated individuals [20]. Cockle et al. reported four immunodominant peptides, PPE6897–116(TQAMATTPSLPEIAANHITQ), PPE68105–124(SLPEIAANHITQAVLTATNF), PPE68121–140(ATNFFGINTIPIALTEMDYF), and PPE68129–148(TIPIALTEMDYFIRMWNQAA), in M. bovis-infected cattle [7]. Based on TB patients, Mustafa et al. identified an immunodominant peptide PPE68121–145(VLTATNFFGINTIPIALTEMDYFIR) and limited the promiscuous Th1 cell epitope region to the sequence 127-FFGINTIPIA-136 [19]. Although these studies demonstrated high levels of IFN-γ release and median percentages of responding patients specific for these peptides, they neither determined the minimal immunodominant peptides nor defined the HLA restriction of these peptides. Compared with the present identified epitopes, we can find that PPE6897–116, PPE68105–124, PPE68121–140, and PPE68129–148 contain the complete or partial sequences of PPE68105–114, PPE68126–134, PPE68133–141, and PPE68140–149, respectively. PPE68118–135 covers the sequence of PPE68126–134, while PPE68121–145 covers two epitopes (PPE68126–134 and PPE68133–141).
At present, the epitope-based diagnostic test is a convenient method for the diagnosis of active TB. Compared to TST, the main advantage of M. tuberculosis-specific T cell epitope as a TB diagnostic reagent is its sensitivity and specificity. Considering the high specificity and moderate sensitivity for the diagnosis of active TB, these four epitopes would provide a supplementary tool for screening this disease. It is possible to combine these epitopes as ingredients in a highly sensitive and specific ELISPOT-based or tetrameric HLA-A*0201-peptide complex (tetramer)-based diagnostic reagent. In addition, these four peptides span a peptide sequence (residues 126–156, GINTIPIALTEMDYFIRMWNQAALAMEVYQA), it is very likely that this long peptide could be used as a diagnostic reagent for TB.
Taken together, the present study described 13 PPE68-derived HLA-A*0201-binding peptides and 4 immunodominant epitopes (PPE68126–134, PPE68133–141, PPE68140–149, and PPE68148–156). To our knowledge, this is the first study reporting PPE68-specific HLA-A*0201-restricted epitopes, and using PPE68-derived epitope-based ELISPOT assay for TB diagnosis. These immunodominant PPE68-derived HLA-A*0201-restricted epitopes may represent a new diagnostic tool for TB. The population coverage rate of HLA-A*0201 (about 30 % in most populations) limits the broad application of above-mentioned immunodominant epitopes in TB diagnosis. Since the total population coverage rate of three HLA-A alleles (A*0201, A*1101 and A*2402) exceeds 80 % [5, 33], we next would identify HLA-A*1101-, A*2402-restricted epitopes in PPPE68. A number of such defined T cell epitopes would form the basis of universal T cell epitope-based in vitro diagnostic reagent for TB.
References
al-Ramadi BK, Jelonek MT, Boyd LF, Margulies DH, Bothwell AL (1995) Lack of strict correlation of functional sensitization with the apparent affinity of MHC/peptide complexes for the TCR. J Immunol 155:662
Arlehamn CS, Sidney J, Henderson R et al (2012) Dissecting mechanisms of immunodominance to the common tuberculosis antigens ESAT-6, CFP10, Rv2031c (hspX), Rv2654c (TB7.7), andRv1038c (EsxJ). J Immunol 188:5020
Behr MA, Wilson MA, Gill WP, Salamon H, Schoolnik GK, Rane S, Small PM (1999) Comparative genomics of BCG vaccines by whole-genome DNA microarray. Science 284:1520
Brock I, Weldingh K, Leyten EM, Arend SM, Ravn P, Andersen P (2004) Specific T-cell epitopes for immunoassay-based diagnosis of Mycobacterium tuberculosis infection. J Clin Microbiol 42:2379
Chang KM, Gruener NH, Southwood S, Sidney J, Pape GR, Chisari FV, Sette A (1999) Identification of HLA-A3 and-B7-restricted CTL response to hepatitis C virus in patients with acute and chronic hepatitis C. J Immunol 162:1156
Cockle PJ, Gordon SV, Lalvani A, Buddle BM, Hewinson RG, Vordermeier HM (2002) Identification of novel Mycobacterium tuberculosis antigens with potential as diagnostic reagents or subunit vaccine candidates by comparative genomics. Infect Immun 70:6996
Cockle PJ, Gordon SV, Hewinson RG, Vordermeier HM (2006) Field evaluation of a novel differential diagnostic reagent for detection of Mycobacterium bovis in Cattle. Clin Vaccine Immunol 13:1119
Demangel C, Brodin P, Cockle PJ, Brosch R, Majlessi L, Leclerc C, Cole ST (2004) Cell envelope protein PPE68 contributes to Mycobacterium tuberculosis RD1 immunogenicity independently of a 10-kilodalton culture filtrate protein and ESAT-6. Infect Immun 72:2170
Duan ZL, Wang ZB, Guo JL et al (2013) Two novel squamous cell cancer antigen-derived HLA-A*0201-binding peptides induced in vitro and in vivo CD8+ cytotoxic T lymphocyte responses. Int J Oncol 42:1482
Ewer K, Deeks J, Alvarez L, Bryant G, Waller S, Andersen P, Monk P, Lalvani A (2003) Comparison of T-cell-based assay with tuberculin skin test for diagnosis of Mycobacterium tuberculosis infection in a school tuberculosis outbreak. Lancet 361:1168
Fuss IJ, Kanof ME, Smith PD, Zola H (2009) Isolation of whole mononuclear cells from peripheral blood and cord blood. Curr Protoc Immunol. doi:10.1002/0471142735.im0701s85
Jasmer RM, Nahid P, Hopewell PC (2002) Clinical practice. Latent tuberculosis infection. N Engl J Med 347:1860
Khanna R (2004) Predictive algorithms and T cell epitope mapping. J Immunol 173:2895
Kuttler C, Nussbaum AK, Dick TP, Rammensee HG, Schild H, Hadeler KP (2000) An algorithm for the prediction of proteasomal cleavages. J Mol Biol 298:417
Liu XQ, Dosanjh D, Varia H, Ewer K, Cockle P, Pasvol G, Lalvani A (2004) Evaluation of T-cell responses to novel RD1- and RD2-encoded Mycobacterium tuberculosis gene products for specific detection of human tuberculosis infection. Infect Immun 72:2574
Mazurek GH, Jereb J, Vernon A, LoBue P, Goldberg S, Castro K, IGRA Expert Committee; Centers for Disease Control and Prevention (CDC) (2010) Updated guidelines for using interferon gamma release assays to detect Mycobacterium tuberculosis infection-United States, 2010. MMWR Recomm Rep 59:1
Meier T, Eulenbruch HP, Wrighton-Smith P, Enders G, Regnath T (2005) Sensitivity of a new commercial enzyme-linked immunospot assay (T SPOT-TB) for diagnosis of tuberculosis in clinical practice. Eur J Clin Microbiol Infect Dis 24:529
Mukhopadhyay S, Balaji KN (2011) The PE and PPE proteins of Mycobacterium tuberculosis. Tuberculosis 91:441
Mustafa AS, Al-Attiyah R, Hanif SN, Shaban FA (2008) Efficient testing of large pools of Mycobacterium tuberculosis RD1 peptides and identification of major antigens and immunodominant peptides recognized by human Th1 cells. Clin Vaccine Immunol 15:916
Okkels LM, Brock I, Follmann F et al (2003) PPE protein (Rv3873) from DNA segment RD1 of Mycobacterium tuberculosis: strong recognition of both specific T-cell epitopes and epitopes conserved within the PPE family. Infect Immun 71:6116
Otahal P, Hutchinson SC, Mylin LM, Tevethia MJ, Tevethia SS, Schell TD (2005) Inefficient cross-presentation limits the CD8+ T cell response to a subdominant tumor antigen epitope. J Immunol 175:700
Pai M, Zwerling A, Menzies D (2008) Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update. Ann Intern Med 149:177
Rammensee H, Bachmann J, Emmerich NP, Bachor OA, Stevanović S (1999) SYFPEITHI: database for MHC ligands and peptide motifs. Immunogenetics 50:213
Ramos JM, Robledano C, Masiá M, Belda S, Padilla S, Rodríguez JC, Gutierrez F (2012) Contribution of interferon gamma release assays testing to the diagnosis of latent tuberculosis infection in HIV-infected patients: a comparison of QuantiFERON-TB Gold In Tube, T-SPOT.TB and tuberculin skin test. BMC Infect Dis 12:169
Rustomjee R, Diacon AH, Allen J et al (2008) Early bactericidal activity and pharmacokinetics of the diarylquinoline TMC 207 in pulmonary tuberculosis. Antimicrob Agents Chemother 52:2831
Scarpellini P, Tasca S, Galli L, Beretta A, Lazzarin A, Fortis C (2004) Selected pool of peptides from ESAT-6 and CFP-10 proteins for detection of Mycobacterium tuberculosis infection. J Clin Microbiol 42:3469
Tan JM, Tang XD, Xie T et al (1998) DNA typing for HLA-A, B antigens by polymerase chain reaction with sequence-specific primers and clinical application. Natl Med J China 78:763
van der Burg SH, Visseren MJ, Brandt RM, Kast WM, Melief CJ (1996) Immunogenicity of peptides bound to MHC class I molecules depends on the MHC-peptide complex stability. J Immunol 156:3308
Wang Y, Sun M, He M et al (2012) Weak binder for MHC molecule is a potent Mycobacterium tuberculosis-specific CTL epitope in the context of HLA-A24 allele. Microb Pathog 53:162
Wen JS, Duan ZL, Jiang LF (2010) Identification of a dengue virus-specific HLA-A*0201-restricted CD8(+) T cell epitope. J Med Virol 82:642
World Health Organization (2014) Global tuberculosis report. World Health Organization, Geneva
Zhou M, Xu D, Li X et al (2006) Screening and identification of severe acute respiratory syndrome-associated coronavirus-specific CTL epitopes. J Immunol 177:2138
Zhu BF, Yang G, Shen CM et al (2010) Distributions of HLA-A and -B alleles and haplotypes in the Yi ethnic minority of Yunnan, China: relationship to other populations. J Zhejiang Univ Sci B 11:127
Acknowledgments
The work was funded by the National Natural Science Foundation of China (30972763, 81261160323, 81172811, 81171576 and 31070143), National Science and Technology Key Projects for Major Infectious Diseases (2013ZX10003001), the Natural Science Foundation of Zhejiang (LY13H160035 and LQ14C010006), the Planned Science and Technology Project of Ningbo (2012A610247), and the Planned Science and Technology Project of Zhejiang (2014C33261).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Zhi-liang Duan and Qiang Li have contributed equally to this work.
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Duan, Zl., Li, Q., Wang, S. et al. Identification of Mycobacterium tuberculosis PPE68-Specific HLA-A*0201-Restricted Epitopes for Tuberculosis Diagnosis. Curr Microbiol 70, 769–778 (2015). https://doi.org/10.1007/s00284-015-0786-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-015-0786-x