Abstract
Purpose
Cisplatin (DDP)-based chemotherapy is a standard strategy for cervical cancer, while chemoresistance remains a huge challenge. In the present study, we aimed to explore the effects of SPP1 on the proliferation and apoptosis rate of the HeLa cervical cancer cell line with cisplatin (DDP) resistance.
Methods
Microarray analysis was employed to select differentially expressed genes in cervical cancer tissues and adjacent tissues. Then, we established a DDP-resistant HeLa cell line (res-HeLa). Western blotting was used to detect SPP1 expression in both tissue and cells. After the transfection with si-SPP1 and pcDNA3.1-SPP1, colony formation and MTT assays were applied to detect cell proliferation changes. Flow cytometry was employed to detect the cell apoptosis rate. Western blotting was performed to verify the activation of PI3K/Akt signal pathway proteins related to DDP resistance.
Results
SPP1 was overexpressed in cervical cancer tissues and cell lines. Compared to normal HeLa cells, expression of SPP1 was significantly enhanced in res-HeLa cells. SPP1 knockdown resulted in repressed proliferation and enhanced apoptosis of res-HeLa cells, which could be reversed by SPP1 overexpression in HeLa cells. Additionally, downregulation of SPP1 improved the DDP sensitivity of HeLa by inhibiting the PI3K/Akt signaling pathway.
Conclusion
SPP1 inhibition could suppress proliferation, induce apoptosis and increase the DDP chemo-sensitivity of HeLa cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer, which is one of the most prevalent malignant neoplasms, affects approximately 529,800 new patients every year, and 275,100 of them are diagnosed with a deadly form of the cancer [1]. Among them, 30% of patients are aged less than 30 years [2]. To date, joint treatment of chemo-radiation (CRT) and neoadjuvant chemotherapy (NACT) followed by radical surgery (RS) have proven effective in cervical cancer overall survival [3], and over 20 chemotherapeutics are now available. However, the response rate remains low, which may be related to the resistance to chemotherapy of cervical cancer cells [4, 5]. Therefore, it is very important to explore the possible mechanisms of chemo-resistance in cervical cancer [6].
Cisplatin (DDP)-based chemo-radiotherapy is the standard therapy for locally advanced cervical cancer [7]. DDP crosslinks with purine bases in DNA molecules and interferes with DNA repair, which causes apoptosis and necrosis in cancer cells [8]. However, long-term treatment with DDP induces drug resistance in tumor cells although DDP is one of the most efficient agents for cervical cancer metastasis [9]. Studies have demonstrated that DDP resistance in res-HeLa cells is far more significant compared to wild-type HeLa cells [8]. Therefore, a key point for cervical cancer chemo-radiotherapy lies in overcoming the DDP resistance of tumor cells.
Secreted phosphoprotein 1 (SPP1), which is also known as osteopontin (OPN), controls the growth, proliferation, migration and apoptosis of cells. The association between the expression of SPP1 and chemo-resistance in tumorigenesis, such as prostate cancer, has also received attention from researchers [10]. It is widely accepted that OPN has certain functions, including the upregulation of cancer cell proliferation and apoptosis inhibition [11]. Studies have also revealed that in many malignancies, OPN expression level was upregulated [12]. For instance, SPP1 overexpression was observed in Leukemia [13], lung cancer [14] and glioblastoma [15]. However, the role of SPP1 in cervical cancer remains unclear and further research is needed. Therefore, the correlation between SPP1 and cervical cancer needs to be investigated further.
HeLa is an immortal cervical cancer cell line, and the phosphatidylinositol 3-kinase/Protein kinase B (PI3K/Akt) signaling pathway is a signal transduction network. Huan Chang et al. revealed that the PI3K/Akt signal pathway was involved in the autophagy of HeLa cells [16], and Shu XR et al. suggested that a PI3K/Akt-dependent pathway was involved in cisplatin resistance [17]. Therefore, we investigated the activation of the PI3K/Akt signal pathway in HeLa cells to explore a possible mechanism of DDP resistance.
In our study, we examined the role of SPP1 in a HeLa cell line and tested a possible mechanism by detecting cell proliferation and apoptosis in HeLa cells. Additionally, DDP sensitivity in HeLa cells influenced by SPP1 was investigated.
Materials and methods
Tissue samples
Sixteen cervical cancer and corresponding adjacent tissues were obtained from resected specimens collected during cervical cancer surgery in the General Hospital of Tianjin Medical University. Tissue samples were snap-frozen in liquid nitrogen and preserved at − 80 °C until RNA or protein extraction. This study and all the specimens involved were approved by the Ethics Committee of General Hospital of Tianjin Medical University.
Cell culture and reagents
Immortalized human epithelial cell line H8 and cervical cancer cell line C-33A (HeLa and CaSki) were purchased from BeNa Culture Collection (Beijing, China). The res-Hela cell line was obtained from HeLa cells that survived DDP screening. All cell lines were cultured in Dulbecco’s modified eagle medium (DMEM) with 10% fetal bovine serum (FBS) at 37 °C in 5% CO2.
SiRNA construction
Two siRNAs (Integrated Biotech Solutions, Shanghai, China) were synthesized and transfected into HeLa and res-HeLa cell lines using Lipofectamine RNAi MAX reagent (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions (siRNA: Lipofectamine = 10 nM:1 µL). The following siRNA sequences were used: si-SPP1-1, 5′-CGAUCGAUAGUGCCGAGAAGC-3′ and si-SPP1-2, 5′-AGCUAGUCCUAGACCCUAAGA-3′.
SPP1 overexpression plasmid construction
A polymerase chain reaction (PCR) was used to amplify the CDS region of SPP1 in the HeLa cell line. DNA fragments were separated from an agarose gel and collected using the small amount QIAquick Gel Extraction Kit (SBS Genetech Co., Ltd, Beijing, China). An enzyme digestion reaction was performed using plasmids and the collected DNAs. Then, the products were used for a ligase reaction with the pcDNA3.1 vector. Cells with stable SPP1 protein expression were selected and amplified.
Quantitative real-time polymerase chain reaction (qRT-PCR)
The total RNA was extracted using the Total RNA Kit (R6834; Omega, Norcross, GA, USA). The PrimeScript RT reagent Kit (DRR027A, TaKaRa, Dalian, China) was used for reverse transcription. Then, 2 µg of product for reverse transcription was obtained to perform a qRT-PCR reaction using specific primer sequences and to draw standard PCR reaction curves. GAPDH was used as an internal reference gene. The mRNA expression level was acquired using the 2− ΔΔCt method. All reactions were performed in triplicate. The following primers were used: SPP1 (forward: 5′-TTTGTTGTAAAGCTGCTTTTCCTC-3′, reverse: 3′-GAATTGCAGTGATTTGCTTTTGC-5′) and GAPDH (forward: 5′-AGTAGAGGCAGGGATGATG-3′, reverse: 3′-GGTATCGTGGAAGGACTC-5′).
Colony formation assay
Cells were digested, counted and used to make a 1 × 106/L cell suspension. Then 200 µL of the cell suspension and 10 mL complete medium were added to each 60 mm glass panel. After transfection, the cells were maintained at 37 °C in 5% CO2 for 14 days until visible colonies appeared. Then, the cells were washed with phosphate-buffered solution (PBS) and fixed with methanol for 15 min. After the cells were washed with running water, 1 mL 0.1% crystal violet solution (Beijing Dingguo Changsheng Biotech Co., Ltd, Beijing, China) was added to stain the cells for 30 min. Afterwards, the cells were washed with running water, dried and examined under a microscope.
MTT assay
Cells were cultured in serum-free medium for 10 h until they reached the logarithmic phase of growth. After digesting the cells with 0.25% trypsin, the concentration of single cell suspension was adjusted to 5 × 104 cells/mL. The cells were seeded into a 96-well plate with 100 µL/well along with a drug treatment. Next, MTT reagent (Sigma, St. Louis, MO, USA) was added to each well. After 4 h of incubation, Dimethyl sulfoxide (DMSO, Sigma, St. Louis, MO, USA) was added to remove the excess dye solution. Cell viability was detected after 24 h, 48 h and 72 h. The OD (optical density) value was measured at 490 nm. All reactions were performed in triplicate.
Cell apoptosis assay
Treated cells were washed with PBS twice and then suspended in binding buffer at 1 × 106 cells/mL. Next, 100 µL of the cell suspension was put into a 5-mL flow tube, and 5 µL of Annexin V/PE and 10 µL of 7-AAD (#YB40310ES20, ATCC, Manassas, VA, USA) were added. The cells were cultured at room temperature in darkness for 15 min. Afterwards, 400 µL 1 × binding buffer was added, mixed completely and then detected within 1 h. Three groups were involved in the experiment: viable cells with low-intensity background fluorescence, apoptotic cells at an early stage with stronger reddish orange fluorescence and apoptotic cells at a late stage with both reddish orange and red fluorescence.
Chemosensitivity assay
HeLa cells at the logarithmic growth phase were seeded into 96-well plates (180 µL/well, 1 × 105 cells/mL) and maintained at 37 °C in 5% CO2 for 24 h. Three parallel wells were set, and the cells in the treatment groups were treated with or without 10 µM DDP, whereas the negative control group received the same volume of physiological saline. After incubation for 48 h, 20 µL MTT (5 mg/mL) was added to each well. The cells were continually incubated at 37 °C for 4 h, centrifuged at 2,000 rpm for 10 min and then the supernatant was discarded. Next, 100 µL DMSO was added, and the solution was mixed until the precipitate was completely dissolved. The OD value was measured at 570 nm using an ELISA reader and a tumor cell inhibitory rate was calculated according to the following equation:
The dose–response curve was obtained by plotting the growth inhibitory rate of the tumor cells with different concentrations of drugs, and the half-inhibitory concentration IC50, which is the dose of the drug when the survival rate was reduced by 50%, was obtained. The fold-change in drug resistance was calculated according to the ratio of IC50 in each group to IC50 in sensitive groups.
Western blot
Cells were lysed using cell lysis buffer (78,501, Thermo Scientific, Rockford, IL, USA) to measure the protein concentration using a pierce BCA assay (23,225, Thermo Scientific, Rockford, IL, USA). Protein electrophoresis was performed using an SDS–PAGE and polyvinylidene (PVDE) membrane that was blocked at room temperature for 3 h. The primary antibodies anti-SPP1 (#H00006696-M01, 1:1000; Abnova, Heidelberg, Germany) and anti-GAPDH (#ab8245, 1:5000,Abcam, Heidelberg, Germany) were added and incubated at room temperature for 1 h and then washed with PBS three times. Immunoreactive bands were detected with a chemiluminescence system (32,209, Thermo Scientific, Rockford, IL, USA) and the data were measured using ImageJ. All reactions were performed in triplicate.
Statistical analysis
GSE9750 was used for gene analysis and selection of cervical cancer and adjacent tissues. A fold change < − 16 was considered to be downregulated. A fold change > 16 was considered to be overexpressed. A P value < 0.05 (adjusted by Benjamini-Hochberg (BH) method) was considered statistically significant. The data were analyzed using SPSS 24.0 software (SPSS Inc., Chicago, IL, USA) and GraphPad 7.0 software (GraphPad Inc., San Diego, CA, USA). The data were determined as the mean ± standard deviation (SD) and ANOVA was adopted for intergroup comparison.
Results
SPP1 was overexpressed in cervical cancer tissues and cell lines
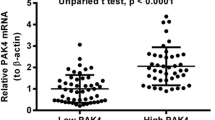
To reveal the differentially expressed mRNAs in the cervical cancer tissues, we used a microarray analysis, and the results are shown as a volcano plot and a heatmap. As seen in Fig. 1a, b, expression of SPP1 was significantly higher in cervical cancer tissues compared to adjacent tissues. The Western blot results of cervical cancer tissues from patients also showed that SPP1 was upregulated in cervical cancer (*P < 0.05, Fig. 1c). Additionally, expression of SPP1 was detected in cell lines. We set up five groups of cell lines. The Res-HeLa cell line was obtained from HeLa cells that survived DDP treatment. IC50 analysis showed that there was significant difference in DDP resistance between normal and DDP-resistant HeLa cells (***P < 0.001, Fig. 1d). The common cervical cancer cell lines C-33A, HeLa and CaSki were included. Human epithelial cell line H8 was used as a control. These results demonstrated that the SPP1 protein expression level significantly increased in the DDP-resistant cervical cancer cell line HeLa/DPP and common cervical cancer cell lines (C-33A/HeLa/CaSki). Compared to the HeLa cell lines, the res-HeLa cell lines significantly expressed more SPP1(**P < 0.01, ***P < 0.001, Fig. 1e). Overall, SPP1 was significantly overexpressed in cervical cancer tissues and cells. The expression of SPP1 in DDP-resistant HeLa cell lines was significantly improved compared to normal HeLa cells, which indicated that the aberrant overexpression of SPP1 might be closely linked to DDP resistance in cervical cancer.
SPP1 expression level in tissues and cells. a Volcano Plot: SPP1 was significantly overexpressed in cervical cancer tissues (P < 0.001). b Heat map: Among 20 genes, SPP1 was significantly and highly expressed in cervical cancer tissues compared with the adjacent tissues. c SPP1 expression in 16 cervical cancer tissues and adjacent tissues from a Western blot. d Continuous treatment of a HeLa cell line with the median-lethal dose of DDP to. The 1st generation of HeLa cells was the normal HeLa cell line, and the 8th generation was labeled as res-HeLa (DDP-resistant HeLa). The medium was changed every day. e SPP1 expression was analyzed by Western blot in H8, C-33A, HeLa, CaSki and res-HeLa cells (*P < 0.05, **P < 0.01, ***P < 0.001). Three repeated experiments were carried out for each assay
SPP1 promoted cervical cell line proliferation and inhibited apoptosis
Among the cell lines that were studied, SPP1 expression was the highest in the res-HeLa and HeLa cell lines. Therefore, res-Hela and HeLa were chosen for further study. qRT-PCR and Western blot results showed that siRNA1 and siRNA2 could both inhibit SPP1 mRNA and protein expression in the two cell lines (***P < 0.001, Fig. 2a, c). Further research displayed that SPP1 was overexpressed in the HeLa group transfected with a SPP1 plasmid (***P < 0.001, Fig. 2b, d). SPP1-differential-expression cell lines were established, and we detected cell proliferation and apoptosis potential. In the res-HeLa group, the colonies in the si-SPP1 group had significant downregulation, whereas the SPP1-overexpressed group in the HeLa cell line demonstrated a substantial increase increased obviously (***P < 0.001, Fig. 2e, f). The MTT assay results revealed that cell viability dropped in the si-SPP1 group and was enhanced in the SPP1 group in the res-HeLa or HeLa cell lines, respectively, with statistical significance observed after 48 h (**P < 0.01, ***P < 0.001, Fig. 2g). Additionally, after transfection with si-SPP1, the apoptotic rate of res-HeLa cell lines significantly increased. Nevertheless, the overexpression of SPP1 led to a significant reduction in HeLa (**P < 0.01, ***P < 0.001, Fig. 2h). Taken together, SPP1 protein could promote proliferation and inhibit apoptosis both in res-HeLa and HeLa cells.
SPP1 promoted proliferation and suppressed apoptosis of HeLa cells. a qRT-PCR results showed that the relative SPP1 expressions in the si-SPP1-1 and si-SPP1-2 groups were significantly lower compared to the Blank and si-ctrl groups. b The data of qRT-PCR revealed that the relative SPP1 mRNA expressions in the SPP1 overexpression groups were significantly higher compared to the Blank and ctrl groups. c SPP1 expression in the res-HeLa cell lines was analyzed with a Western blot. Si-SPP1 was transfected in res-HeLa cells. c SPP1 expression in HeLa cell lines was analyzed with a Western blot. The SPP1 plasmid was transfected into HeLa cells. d, e Colony formation in res-HeLa and HeLa cell lines. Si-SPP1 was transfected into res-HeLa cells, and the SPP1 plasmid was transfected into HeLa cells. Cell colony formation was reduced in the si-SPP1 group compared to the corresponding Blank and NC groups. While in the HeLa cell line, colony formation was promoted in the SPP1 overexpression group compared to the corresponding Blank and NC groups. f Cell viability was analyzed by MTT analysis in 96 h and was significantly enhanced in the HeLa + SPP1 group, whereas viability was repressed in the res-HeLa + si-SPP1 group compared to the NC group. g The cell apoptosis rate was significantly enhanced in the si-SPP1 group compared to the Blank and NC groups in the res-HeLa cell line, whereas an insignificant difference was revealed in the SPP1 group in HeLa cells *P < 0.05, **P < 0.01, ***P < 0.001. Three repeated experiments were carried out for each assay
SPP1 inhibition increased the DDP sensitivity of HeLa
To reveal the relationship between SPP1 expression and DDP resistance, we added 10 µM DDP to res-HeLa. The mRNA and protein expression of SPP1 were both induced by DDP, which indicates that the upregulation of SPP1 increased resistance to DDP (*P < 0.05, **P < 0.01, ***P < 0.001, Fig. 3a, b). Furthermore, we added PI3K signaling pathway inhibition LY294002 to analyze the relationship between DDP resistance and the PI3K signaling pathway. Colony formation and MTT assays revealed that an inhibitory effect of independent DDP on cell proliferation and viability was not evident, whereas independent SPP1 siRNA or cDNA reversed cell proliferation and viability remarkably. Moreover, in the res-HeLa cell line, combination of DDP and SPP1 siRNA had significantly more inhibition of cell proliferation compared to using DDP or SPP1 siRNA only (*P < 0.05, **P < 0.01, ***P < 0.001, Fig. 3c–e). Additionally, a cell apoptosis assay displayed that the transfection of SPP1 siRNA led to effective cell apoptosis in the res-HeLa cell line, and the highest cell apoptotic level occurred in the DDP + siRNA group (*P < 0.05, **P < 0.01, ***P < 0.001, Fig. 3f), which indicates that SPP1 suppressed the treatment of DDP in HeLa. Meanwhile, inhibition of PI3K signaling pathway significantly inhibited cell proliferation and anti-apoptosis.
SPP1 reversed the inhibition of DDP in the res-HeLa cell line. a qRT-PCR results showed that the relative SPP1 expressions in the DDP-treated group were significantly higher compared to the si-ctrl group, whereas the downregulation of SPP1 reversed this increase. b The Western blot data revealed that DDP increased SPP1 expression and si-SPP1 inhibited this upregulation. c, d Cell viability was analyzed with an MTT analysis in the res-HeLa cell line. Cell colony formation was reduced in the DDP-treatment group, whereas the decrease was more significant in the DDP + si-SPP1 group. e Cell viability was significantly reduced in the res-HeLa + SPP1 group supplemented with DDP. f The cell apoptosis rate was significantly promoted in the si-SPP1 + DDP group. *P < 0.05, **P < 0.01, ***P < 0.001. Three repeated experiments were carried out for each assay
Overexpression of SPP1 induced DDP resistance in HeLa
Furthermore, we established SPP1-overexpressed HeLa cell lines and added 10 µM DDP. Transfection was successful, and DDP had an ability to improve SPP1 expression (*P < 0.05, **P < 0.01, ***P < 0.001, Fig. 4a, b). Overexpression of SPP1 significantly improved colony formation, proliferation and anti-apoptosis ability in HeLa cell lines. DDP Treatment could not completely reverse the function of SPP1. PI3K signaling pathway inhibition significantly suppressed cell viability (*P < 0.05, **P < 0.01, ***P < 0.001, Fig. 4c–f).
Overexpressed SPP1 induced DDP resistance in the HeLa cell line. a qRT-PCR results showed that the relative SPP1 expressions in the DDP-treated group were significantly higher than the vector group and the upregulation of SPP1 enhanced this increase. b The data from a Western blot revealed that DDP increased SPP1 expression and SPP1 promoted this upregulation. c, d Cell viability was analyzed by MTT analysis in the HeLa cell line. Cell colony formation was significantly reduced in the DDP treatment group, whereas the decrease was reversed with transfection of SPP1. e Cell viability was less significantly reduced in the res-HeLa + SPP1 group supplemented with DDP. f The cell apoptosis rate was significantly enhanced in the si-SPP1 + DDP group. *P < 0.05, **P < 0.01, ***P < 0.001. Three repeated experiments were carried out for each assay
SPP1 siRNA increased HeLa DDP sensitivity by deactivating the PI3K/Akt signal pathway
Western blot results showed that in the res-HeLa cell line, SPP1 siRNA only or the combination of DDP and SPP1 siRNA repressed p-PI3K, p-Akt and p-ERK expression levels considerably (*P < 0.05, **P < 0.01, ***P < 0.001, Fig. 5a). The results verified that the PI3K/Akt signal pathway was suppressed effectively through the combination of DDP and SPP1 siRNA. From above, it was inferred that SPP1 siRNA could increase the DDP sensitivity of HeLa by inactivating the PI3K/Akt signal pathway.
The possible mechanism of DDP sensitivity improvement (i.e., the PI3K/Akt signal pathway). a Expression of the PI3K/Akt signaling pathway-related protein was analyzed by Western blot. P-PI3K, p-Akt and p-ERK expression levels declined significantly with si-SPP1 and DDP, respectively, and reached their lowest value in si-SPP1 + DDP groups. *P < 0.05, **P < 0.01, ***P < 0.001. Three repeated experiments were carried out for each assay
Discussion
Cervical cancer is a death-causing malignancy in gynecology, and DDP has been used as one of the most effective chemo-radiotherapy agents for treating this cancer [18]. However, therapeutic resistance has been found in cervical cancers cells, especially in patients with metastatic, recurrent and advanced disease [17]. In our study, we found that SPP1 was overexpressed in cervical cancer tissues and cells, and cell proliferation as well as viability in the cDNA group was notably increased while apoptosis decreased. The results for the SPP1 siRNA group showed the opposite result. Furthermore, we confirmed that SPP1 siRNA could repress DDP resistance by inhibiting the PI3K/Akt signal pathway in tumor cells.
A previous study indicated that SPP1 expression was significantly distinct in cervical cancer and normal cell lines [19]. Consistent with that study, we revealed that SPP1 mRNA and protein expression levels were remarkably higher in cervical cancer tissues compared to adjacent tissues. Additionally, it was widely maintained that HeLa cell proliferation and apoptosis were adjusted by SPP1 [20] and SPP1 downregulation, which were confirmed to be involved in tumor growth inhibition and anti-tumor activities [21]. For example, Cho et al. suggested that SPP1 could be regarded as a biomarker for cervical cancer [22] and Song et al. indicated that SPP1 upregulation was linked with the invasion of cervical cancer [23]. The present study witnessed the same phenomenon in that SPP1 induced HeLa growth. Nevertheless, when SPP1 was silenced by SPP1 siRNA, HeLa cell proliferation was obviously inhibited while the apoptosis rate increased dramatically. Therefore, our data supported the view that SPP1 promoted HeLa cell proliferation and inhibited apoptosis.
Until now, abundant research has been conducted to study miRNAs, proteins or genes that are potentially related to DDP resistance. Fang Li et al. have reported that DDP resistance in ovarian cancer can be reversed by the TNF-related apoptosis-inducing ligand (TRAIL) protein [24]. Hui Yang et al. also suggested that DDP sensitivity could be increased by deregulating miR-497 in cervical cancer HeLa cells [25]. Furthermore, SPP1 was found to contribute to DDP resistance in glioma [26] and small cell lung cancer [27]. In line with these findings, we discovered for the first time that DDP sensitivity was enhanced considerably in cervical cancer cells after SPP1 siRNA was added, and we found that SPP1 inhibition could reduce DDP resistance in HeLa cells.
Numerous experiments suggested that the PI3K/Akt signal pathway played an important role in cervical cancer. For example, Li et al. showed that activation of the PI3K/Akt signal pathway could promote cervical cancer cell proliferation [28], and Liao et al.’s research demonstrated that PI3K and Akt expression levels increased in cervical cancer tissues compared to adjacent tissues [29]. Additionally, SPP1 has been observed to promote the growth and proliferation of HeLa and suppress apoptosis by activating related signaling pathways [30]. Similarly, in our research, p-PI3K, p-Akt and p-ERK expression levels declined after SPP1 siRNA was added, which indicates that the PI3K/Akt signal pathway was positively related to SPP1 and could be inhibited by SPP1 siRNA. However, limitations, such as the small sample size and the absence of in vivo experiments, still exist in this study. To draw more convincing conclusions, larger samples should be investigated, and in vivo experiments should be carried out if conditions permit.
Conclusion
In the present study, SPP1 was used for the first time as a possible target for removing DDP resistance in cervical cancer treatment, and it was demonstrated that DDP sensitivity could be restored by inactivating the PI3K/Akt signaling pathway in cervical cancer. The exploration of the function of siRNAs in cancer chemo-resistance via particular pathways has great significance in human cancer therapy. Therefore, in future research, the actions of siRNAs in chemo-resistant processes and signaling pathways should be further investigated.
References
Zhang YH, Wang JJ, Li M, Zheng HX, Xu L, Chen YG (2016) Matrix metallopeptidase 14 plays an important role in regulating tumorigenic gene expression and invasion ability of HeLa cells. Int J Gynecol Cancer 26(3):600–606. https://doi.org/10.1097/IGC.0000000000000652
Sun XL, Wang HB, Wang ZQ, Cao TT, Yang X, Han JS, Wu YF, Reilly KH, Wang JL (2017) Effect of transcutaneous electrical stimulation treatment on lower urinary tract symptoms after class III radical hysterectomy in cervical cancer patients: study protocol for a multicentre, randomized controlled trial. BMC Cancer 17(1):416. https://doi.org/10.1186/s12885-017-3387-1
Marchetti C, De Felice F, Di Pinto A, Romito A, Musella A, Palaia I, Monti M, Tombolin V, Muzii L, Benedetti Panici P (2018) Survival nomograms after curative neoadjuvant chemotherapy and radical surgery for stage IB2-IIIB cervical cancer. Cancer Res Treat 50(3):768–776. https://doi.org/10.4143/crt.2017.141
Filippova M, Filippov V, Williams VM, Zhang K, Kokoza A, Bashkirova S, Duerksen-Hughes P (2014) Cellular levels of oxidative stress affect the response of cervical cancer cells to chemotherapeutic agents. Biomed Res Int 2014:574659. https://doi.org/10.1155/2014/574659
Gottesman MM (2002) Mechanisms of cancer drug resistance. Annu Rev Med 53:615–627. https://doi.org/10.1146/annurev.med.53.082901.103929
Pariente R, Pariente JA, Rodriguez AB, Espino J (2016) Melatonin sensitizes human cervical cancer HeLa cells to cisplatin-induced cytotoxicity and apoptosis: effects on oxidative stress and DNA fragmentation. J Pineal Res 60(1):55–64. https://doi.org/10.1111/jpi.12288
Agoni L, Basu I, Gupta S, Alfieri A, Gambino A, Goldberg GL, Reddy EP, Guha C (2014) Rigosertib is a more effective radiosensitizer than cisplatin in concurrent chemoradiation treatment of cervical carcinoma, in vitro and in vivo. Int J Radiat Oncol Biol Phys 88(5):1180–1187. https://doi.org/10.1016/j.ijrobp.2013.12.051
Wang B, Huang Z, Gao R, Zeng Z, Yang W, Sun Y, Wei W, Wu Z, Yu L, Li Q, Zhang S, Li F, Liu G, Liu B, Leng L, Zhan W, Yu Y, Yang G, Zhou S (2017) Expression of long noncoding RNA urothelial cancer associated 1 promotes cisplatin resistance in cervical cancer. Cancer Biother Radiopharm 32(3):101–110. https://doi.org/10.1089/cbr.2016.2156
Casagrande N, De Paoli M, Celegato M, Borghese C, Mongiat M, Colombatti A, Aldinucci D (2013) Preclinical evaluation of a new liposomal formulation of cisplatin, lipoplatin, to treat cisplatin-resistant cervical cancer. Gynecol Oncol 131(3):744–752. https://doi.org/10.1016/j.ygyno.2013.08.041
Liu G, Fan X, Tang M, Chen R, Wang H, Jia R, Zhou X, Jing W, Wang H, Yang Y, Yin F, Wei H, Li B, Zhao J (2016) Osteopontin induces autophagy to promote chemo-resistance in human hepatocellular carcinoma cells. Cancer Lett 383(2):171–182. https://doi.org/10.1016/j.canlet.2016.09.033
Qin H, Wang R, Wei G, Wang H, Pan G, Hu R, Wei Y, Tang R, Wang J (2018) Overexpression of osteopontin promotes cell proliferation and migration in human nasopharyngeal carcinoma and is associated with poor prognosis. Eur Arch Otorhinolaryngol 275(2):525–534. https://doi.org/10.1007/s00405-017-4827-x
Anborgh PH, Mutrie JC, Tuck AB, Chambers AF (2010) Role of the metastasis-promoting protein osteopontin in the tumour microenvironment. J Cell Mol Med 14(8):2037–2044. https://doi.org/10.1111/j.1582-4934.2010.01115.x
Ruberti S, Bianchi E, Guglielmelli P, Rontauroli S, Barbieri G, Tavernari L, Fanelli T, Norfo R, Pennucci V, Fattori GC, Mannarelli C, Bartalucci N, Mora B, Elli L, Avanzini MA, Rossi C, Salmoiraghi S, Zini R, Salati S, Prudente Z, Rosti V, Passamonti F, Rambaldi A, Ferrari S, Tagliafico E, Vannucchi AM, Manfredini R (2018) Involvement of MAF/SPP1 axis in the development of bone marrow fibrosis in PMF patients. Leukemia 32(2):438–449. https://doi.org/10.1038/leu.2017.220
Hao C, Cui Y, Hu MU, Zhi X, Zhang L, Li W, Wu W, Cheng S, Jiang WG (2017) OPN-a splicing variant expression in non-small cell lung cancer and its effects on the bone metastatic abilities of lung cancer cells in vitro. Anticancer Res 37(5):2245–2254. https://doi.org/10.21873/anticanres.11561
Kijewska M, Kocyk M, Kloss M, Stepniak K, Korwek Z, Polakowska R, Dabrowski M, Gieryng A, Wojtas B, Ciechomska IA, Kaminska B (2017) The embryonic type of SPP1 transcriptional regulation is re-activated in glioblastoma. Oncotarget 8(10):16340–16355. https://doi.org/10.18632/oncotarget.14092
Chang H, Li X, Cai Q, Li C, Tian L, Chen J, Xing X, Gan Y, Ouyang W, Yang Z (2017) The PI3K/Akt/mTOR pathway is involved in CVB3-induced autophagy of HeLa cells. Int J Mol Med 40(1):182–192. https://doi.org/10.3892/ijmm.2017.3008
Shu XR, Wu J, Sun H, Chi LQ, Wang JH (2015) PAK4 confers the malignance of cervical cancers and contributes to the cisplatin-resistance in cervical cancer cells via PI3K/AKT pathway. Diagn Pathol 10:177. https://doi.org/10.1186/s13000-015-0404-z
Song J, Li Y (2017) miR-25-3p reverses epithelial-mesenchymal transition via targeting Sema4C in cisplatin-resistance cervical cancer cells. Cancer Sci 108(1):23–31. https://doi.org/10.1111/cas.13104
Johanneson B, Chen D, Enroth S, Cui T, Gyllensten U (2014) Systematic validation of hypothesis-driven candidate genes for cervical cancer in a genome-wide association study. Carcinogenesis 35(9):2084–2088. https://doi.org/10.1093/carcin/bgu125
Giacopelli F, Marciano R, Pistorio A, Catarsi P, Canini S, Karsenty G, Ravazzolo R (2004) Polymorphisms in the osteopontin promoter affect its transcriptional activity. Physiol Genom 20(1):87–96. https://doi.org/10.1152/physiolgenomics.00138.2004
Sharma P, Kumar S, Kundu GC (2010) Transcriptional regulation of human osteopontin promoter by histone deacetylase inhibitor, trichostatin A in cervical cancer cells. Mol Cancer 9:178. https://doi.org/10.1186/1476-4598-9-178
Cho H, Hong SW, Oh YJ, Kim MA, Kang ES, Lee JM, Kim SW, Kim SH, Kim JH, Kim YT, Lee K (2008) Clinical significance of osteopontin expression in cervical cancer. J Cancer Res Clin Oncol 134(8):909–917. https://doi.org/10.1007/s00432-007-0351-5
Song JY, Lee JK, Lee NW, Jung HH, Kim SH, Lee KW (2008) Microarray analysis of normal cervix, carcinoma in situ, and invasive cervical cancer: identification of candidate genes in pathogenesis of invasion in cervical cancer. Int J Gynecol Cancer 18(5):1051–1059. https://doi.org/10.1111/j.1525-1438.2007.01164.x
Li F, Guo Y, Han L, Duan Y, Fang F, Niu S, Ba Q, Zhu H, Kong F, Lin C, Wen X (2012) In vitro and in vivo growth inhibition of drug-resistant ovarian carcinoma cells using a combination of cisplatin and a TRAIL-encoding retrovirus. Oncol Lett 4(6):1254–1258. https://doi.org/10.3892/ol.2012.926
Yang H, Wu XL, Wu KH, Zhang R, Ju LL, Ji Y, Zhang YW, Xue SL, Zhang YX, Yang YF, Yu MM (2016) MicroRNA-497 regulates cisplatin chemosensitivity of cervical cancer by targeting transketolase. Am J Cancer Res 6(11):2690–2699
Qian C, Li P, Yan W, Shi L, Zhang J, Wang Y, Liu H, You Y (2015) Downregulation of osteopontin enhances the sensitivity of glioma U251 cells to temozolomide and cisplatin by targeting the NF-kappaB/Bcl2 pathway. Mol Med Rep 11(3):1951–1955. https://doi.org/10.3892/mmr.2014.2951
Gu T, Ohashi R, Cui R, Tajima K, Yoshioka M, Iwakami S, Sasaki S, Shinohara A, Matsukawa T, Kobayashi J, Inaba Y, Takahashi K (2009) Osteopontin is involved in the development of acquired chemo-resistance of cisplatin in small cell lung cancer. Lung Cancer 66(2):176–183. https://doi.org/10.1016/j.lungcan.2009.02.004
Li Y, Cui N, Zheng PS, Yang WT (2017) BMX/Etk promotes cell proliferation and tumorigenicity of cervical cancer cells through PI3K/AKT/mTOR and STAT3 pathways. Oncotarget 8(30):49238–49252. https://doi.org/10.18632/oncotarget.17493
Liao S, Xiao S, Zhu G, Zheng D, He J, Pei Z, Li G, Zhou Y (2014) CD38 is highly expressed and affects the PI3K/Akt signaling pathway in cervical cancer. Oncol Rep 32(6):2703–2709. https://doi.org/10.3892/or.2014.3537
Kumar V, Behera R, Lohite K, Karnik S, Kundu GC (2010) p38 kinase is crucial for osteopontin-induced furin expression that supports cervical cancer progression. Cancer Res 70(24):10381–10391. https://doi.org/10.1158/0008-5472.CAN-10-1470
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no competing interests associated with the manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of General Hospital of Tianjin Medical University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Chen, X., Xiong, D., Ye, L. et al. SPP1 inhibition improves the cisplatin chemo-sensitivity of cervical cancer cell lines. Cancer Chemother Pharmacol 83, 603–613 (2019). https://doi.org/10.1007/s00280-018-3759-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-018-3759-5