Abstract
Purpose
The aim of this study was to determine the recommended dose (RD) for a docetaxel/oxaliplatin/S-1 (DOS) regimen in patients with unresectable gastric cancer and to preliminarily evaluate its efficacy.
Methods
Previously untreated patients with histologically proven unresectable metastatic gastric cancer were enrolled (n = 16). Docetaxel and oxaliplatin were administered intravenously on day 8 and S-1 was administered orally twice a day on days 1–14. Each cycle was repeated every 3 weeks. Dose-limiting toxicities (DLTs) were evaluated during the first treatment cycle. Three dose escalations of DOS were employed in this study: level 1 (50/100/80 mg/m2), level 2 (50/130/80 mg/m2), and level 3 (60/130/80 mg/m2).
Results
According to the 3 + 3 dose-escalating schedule, we determined that the RD and maximum tolerated dose for this regimen were level 1 and level 2, respectively. The DLTs were grade 3 diarrhea and febrile neutropenia. The overall response rate was 78% (7/9) for patients with measurable lesions and consisted of two complete responses and five partial responses. Five patients underwent conversion surgery. The median follow-up time was 19 months with median survival time and progression-free survival being 19.6 months and 7.6 months, respectively.
Conclusions
The results from this study demonstrated the safety and tolerability of DOS in unresectable metastatic gastric cancer patients and revealed promising preliminary efficacy with a high conversion rate. A phase II trial of DOS regimen using the identified RD is ongoing.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fifth most common cancer worldwide and the third leading cause of cancer death with the highest estimated mortality rates being in Eastern Asia [1]. Gastrectomy has improved the prognosis for localized gastric cancer, resulting in increased long-term disease-free survival [2]. However, many gastric cancer patients are diagnosed with distant metastasis and cannot undergo curative surgery, resulting in a poor prognosis [3]. For such patients, chemotherapy is the most appropriate treatment option. Until now, several promising cytotoxic agents for gastric cancer have been developed, including docetaxel, S-1, irinotecan, and oxaliplatin [4]. In western countries, the most frequently used chemotherapy for unresectable metastatic gastric cancer are combination regimens including fluoropyrimidine (intravenous 5-fluorouracil [5-FU] or an oral fluoropyrimidine) plus a platinum agent, with or without the addition of docetaxel or anthracyclines [5, 6]. In Japan, the combination of S-1 and cisplatin (CS) is considered the standard first-line regimen for unresectable metastatic gastric cancer, showing a 54% response rate and a median overall survival (OS) of 13.0 months in the SPIRITS trial [7].
Recent trials show that oxaliplatin is almost as active as cisplatin, and less toxic and can, therefore, be used to replace cisplatin [6]. In Japan, based on a phase III trial directly comparing S-1 plus oxaliplatin (SOX) with CS, SOX regimen is considered an alternative that is equal to a cisplatin regimen in terms of progression-free survival (PFS) [8]. In human epidermal growth factor receptor 2 (HER2)-positive gastroesophageal cancer, trastuzumab combined with fluoropyrimidine and cisplatin is the standard first-line therapy worldwide [9].
On the other hand, results from several studies demonstrate promising prognoses associated with conversion therapy, which involves radical surgery following down-staging that occurs in selective patients who received upfront systemic chemotherapy [10,11,12]. However, the regimens most likely to be appropriate for conversion therapy remain unclear. To accomplish down-staging and to proceed to conversion surgery, aggressive induction chemotherapy, such as a triplet regimen that may lead to a marked tumor regression could be a suitable candidate in this setting.
We previously reported the results from the clinical studies of a triplet-combination therapy including docetaxel, cisplatin, and S-1 (DCS) for the treatment of advanced gastric cancer [13,14,15,16,17,18]. A phase II clinical study revealed high clinical efficacy with an 87.1% overall response rate, including a complete response in 3.2% of patients and down-staging in 25.8% of patients, and with 22.6% of patients receiving curative adjuvant surgery [14]. Moreover, we have reported findings from a retrospective analysis of three consecutive DCS clinical studies and demonstrated that following DCS treatment (33.3% conversion rate), 84.8% of patients who received conversion therapy achieved an R0 resection, and 78.8% were confirmed to be chemotherapy responders, according to histological evaluation. Notably, prolonged survival is observed in the conversion cases (48 months) compared to that of patients who received DCS therapy alone (20 months) [10]. However, DCS therapy also shows a high incidence of grade 3/4 hematologic toxicities such as neutropenia (77.4%), and grade 3 non-hematologic toxicities such as anorexia (35.3%) and nausea (32.3%) [10]. Moreover, it is difficult to use cisplatin in an outpatient setting since cisplatin requires 1–2 L of hydration during its administration to prevent cisplatin-induced renal toxicity.
Recent studies suggest that in combination regimens for unresectable metastatic gastric cancer, oxaliplatin is almost as active as cisplatin, and less toxic, particularly regarding nephrotoxicity and gastrointestinal toxicities, and can, therefore, be used to replace cisplatin [6, 8]. Based on the above-described background, we hypothesized that a docetaxel/oxaliplatin/S-1 (DOS) regimen, with oxaliplatin in place of cisplatin from the DCS regimen, would reduce toxicity and be an effective treatment combination without compromising the feasibility or efficacy of treating unresectable gastric cancer. Therefore, the aim of this study was to conduct a dose-escalation analysis to determine the recommended dose (RD) for a DOS regimen used as the first-line treatment of patients with unresectable gastric cancer.
Materials and methods
Patient selection
Patients enrolled in the study were needed to meet the following eligibility criteria: histologic confirmation of adenocarcinoma of the stomach; unresectable distant metastatic disease with an M1 stage according to the Japanese Classification of Gastric Carcinoma (JGCA) version14 [19]; measurable lesion(s) or evaluable disease; age ≥ 20 years; an Eastern Cooperative Oncology Group (ECOG) performance status 0–1; no prior chemotherapy treatment except for adjuvant S-1 chemotherapy with an interval of ≥ 180 days; adequate bone marrow (leukocyte count 4.0 × 109/L or neutrophil count ≥ 1.5 × 109/L, hemoglobin ≥ 8.0 g/dL, platelet count ≥ 100 × 109/L), renal (serum creatinine ≤ 1.2 mg/dL), and hepatic functions (serum bilirubin ≤ 1.5 mg/dL, serum aspartate aminotransferase and alanine aminotransferase ≤ 5 times their respective normal upper limits); and an estimated life expectancy ≥ 3 months. Each patient gave written informed consent to participate prior to registration (trial registration ID: UMIN 000015849). The protocol was approved by the ethics committee of each participating facility and conducted in accordance with the Declaration of Helsinki.
Study design and treatment schedule
S-1 was administered at a dose of 40 mg/m2 twice daily on days 1–14 and docetaxel was administered via intravenous infusion over 60 min on day 8 followed by intravenous administration of oxaliplatin over a 2-h span on day 8 during each 3-week cycle. Three dose escalations of docetaxel, oxaliplatin, and S-1 were used; level 1 (50/100/80 mg/m2), level 2 (50/130/80 mg/m2), and level 3 (60/130/80 mg/m2), respectively. This treatment course was repeated every 3 weeks for a maximum of eight cycles and thereafter oxaliplatin was discontinued to avoid oxaliplatin-induced neurotoxicity. The treatment was repeated until evidence of disease progression, unacceptable toxicity, patient refusal, a secondary resection, or a physician’s decision to terminate. DLT was defined as the occurrence of any of the following events during the first cycle of treatment, in accordance with the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0: grade 4 neutropenia lasting more than 4 d, any febrile neutropenia (FN), grade 4 thrombocytopenia or other non-hematological grade 3–4 toxicities except for nausea, vomiting, and alopecia or any event leading to treatment discontinuation for longer than 2 weeks. This phase I study was carried out using the standard 3 + 3 dose-escalation design. The dose was escalated if no DLT occurred in the initial three patients or if DLT occurred in fewer than 2 of 6 patients. The maximum tolerated dose (MTD) was defined as the dose level associated with DLT in at least 2 of 3 or 2 of 6 patients. The RD was defined as the dose one level below the MTD.
On the planned day of docetaxel and oxaliplatin treatments (day 8), therapy was withheld if grade 3 or grade 4 hematological toxicity or grade 2–4 non-hematological toxicity (except for alopecia, nausea, and vomiting) was noted, and the treatment was not restarted until the adverse event had resolved. Doses of docetaxel, oxaliplatin, and S-1 were reduced if any of the following events occurred during the previous cycle: FN, grade 4 thrombocytopenia, or grade 3 or higher non-hematologic toxicities (except vomiting, nausea, anorexia, hypersensitivity, and fatigue). When indicated, the doses of docetaxel and oxaliplatin were reduced by 10% and the S-1 dose was reduced from 60 to 50 to 40 mg (minimal dose) twice daily. A treatment delay of > 4 weeks was considered a treatment failure (off treatment). When patients achieved down-staging and were judged capable of tolerating a curative surgical procedure, gastrectomy with lymph node dissection was performed.
Pretreatment evaluations
During the week preceding treatment, baseline evaluations were performed, which included a medical history, physical examination, ECOG performance status, routine blood analysis (hematology and chemistry), carcinoembryonic antigen measurement, urine analysis, chest X-ray, computed tomography (CT), and any other appropriate diagnostic procedures used to evaluate metastatic lesions.
Assessment of toxicity and tumor response
Routine blood analysis (hematology and chemistry), and urinalysis were performed twice weekly until the completion of the first treatment cycle and at least once every 3 weeks during treatment thereafter. Tumor response was evaluated with a CT scan every two cycles (6 weeks) according to the Response Evaluation Criteria in Solid Tumors (RECIST), version 1.1. PFS was defined as the time from study registration until objective tumor progression or death. OS was defined as the time from study registration until death from any cause. All statistical analyses were performed using Prism 5 (GraphPad Software, San Diego, CA).
Results
Patient characteristics
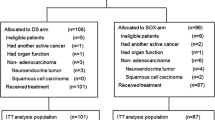
From January 2015 through June 2016, a total of 16 patients who met the inclusion criteria were enrolled in the study. The patient characteristics at baseline are listed in Table 1. The median age was 59.5 years (range 35–78), nine were male (56%), and the ECOG performance status was 0 in 14 patients (88%). 14 patients (88%) had diffuse-type cancers with the most common metastatic sites being the peritoneum (75%), distant lymph nodes (25%), and the liver (13%). The median number of metastatic sites was two (range 2–5). There were no patients with a history of prior gastrectomy and/or chemotherapy.
Dose-limiting toxicities and recommended dose
The number of patients receiving each dose level and the type of DLT observed during the first cycle (DLT window) are summarized in Table 2. At the level 1 dose, 1 of 3 patients developed DLTs (FN and diarrhea). Then, an additional three patients were treated at the level 1 dose with none demonstrating a DLT. Therefore, three patients were then entered into the level 2 dose. One patient developed FN during the first treatment cycle. However, the three subsequent patients in the second group of the level 2 dose did not present with any DLTs. Based on these results, dose-escalation proceeded to the level 3 dose and two patients experienced DLTs (FN and diarrhea). Then, additional two patients were entered into the study at the level 2 dose. Both of these patients subsequently exhibited DLTs (FN and diarrhea). Based on these results, the level 2 dose was defined as the MTD and thus the level 1 dose was defined as the RD for this regimen. In addition, the DLTs associated with the regimen were determined to be grade 3 diarrhea and FN.
Drug administration and toxicity
All 16 patients receiving DOS therapy were evaluated for toxicity during each cycle. A total of 98 treatment cycles were administered with the median number of cycles per patient being 6.5 (range 1–10 cycles). The maximum toxicities experienced by the patients throughout the entire course of treatment for each dose level are shown in Table 3. Neutropenia was the most frequent grade 4 toxicity, which was observed in 10 of 16 patients (63%) during the entire study and 3 of 6 patients (50%) that received the RD (level 1) as treatment. Grade 3 FN was observed in 6 of 16 patients (38%) during the entire study with only one of the patients (17%) presenting with grade 3 FN being from the RD treatment level. The most common grade 3 non-hematological toxicities in all dose levels were anorexia (19%), fatigue (19%), diarrhea (19%), and stomatitis (19%), with the exception of one grade 4 diarrhea observed in a patient being treated at the level 2 dose. At RD, non-hematological toxicities were generally tolerable and manageable. All treatment-related toxicities resolved with appropriate care and no treatment-related deaths occurred. The causes for discontinuation of therapy were disease progression in four patients (25%), conversion surgery in five patients (31%), unacceptable toxicity in two patients (13%), and reasons unrelated to treatment or diseases in five patients (31%). Dose reductions were implemented in 12 patients (75%). Most treatment cycles (78/98 cycles; 78%) were administered every 3 weeks, as per the protocol.
Efficacy
The overall response rate was 78% [95% confidence interval (CI), 46–100%] for the nine patients with measurable lesions, consisting of two complete responses and five partial responses. The disease control rate was 100% for these with no patient showing progression. The median number of cycles required to obtain a partial response was two (range 2–4). Five patients (31%) underwent conversion therapy (two patients for level 1, one patient for level 2, two patients for level 3); the metastatic lesions (three patients with para-aortic lymph node and two patients with peritoneal metastases) completely disappeared after 3–10 treatment courses and achieved R0 resection. All these patients showed pathological responses including two pathological complete responses of the para-aortic lymph node metastases. To date, four of these five conversion patients are still alive (730+, 887+, 891+, and 1135 days). With a median follow-up time of 19 months, the median survival time and progression-free survival were 19.6 months (95% CI 13.7–24.5 months) and 7.6 months (95% CI 6.4–17.9 months), respectively. The 1-year survival rate was 75%.
Discussion
To determine the potential benefit of an intensive triplet regimen without compromising the feasibility or efficacy of treatment, we conducted a dose-escalation trial using the combination of S-1, docetaxel, and oxaliplatin for treatment of patients with unresectable metastatic gastric cancer. We determined the RD for the DOS regimen was docetaxel, 50 mg/m2 (day 8); oxaliplatin, 100 mg/m2 (day 8); and S-1, 40 mg/m2 (twice daily, days 1–14). The DLTs were grade 3 FN and diarrhea.
Triplet therapy using DCS reported to be a promising treatment producing potent antitumor effects in several phase II trials against unresectable gastric cancer in a reproducible manner [14, 16, 20]. DCS shows high clinical efficacy with 79.1–87.1% overall response rates; however, it also shows a high grade 3/4 toxicity incidence, especially G3/4 neutropenia, which presents in 60–80% of the patients. Moreover, DCS regimen was not superior to CS doublet regimen in the JCOG1013 phase III trial, which has been recently published at the ASCO 2018 meeting [21]. However, this study was conducted using another DCS combination [20], which lacked dose intensity compared to our DSC regimen.
When compared to the results of the DCS studies [14, 16, 20], the toxicities observed in this study for DOS were mild. Neutropenia, the most common grade 3/4 toxicity, developed in 50% of the patients who received treatment at RD, showing a more favorable trend than that of DCS (72–79.1%). FN was present in 16.7% of patients who received DOS treatment at RD, compared to 14–34.9% for that in DCS-treated patients. Because both regimens contain triple agents with each of the drugs exerting a myelosuppressive effect to some extent, hematologic toxicity is clearly the limiting toxicity. However, neutropenia was generally short lasting and manageable, and its incidence was reduced through dose reduction or the prophylactic administration of granulocyte-colony stimulating factor (G-CSF). For non-hematological toxicities, there were comparable trends with DOS and DCS. At RD, grade 3/4 anorexia was observed in 16.7% of DOS-treated patients compared with 7–35.5% for that of DCS-treated patients, diarrhea was present in 16.7% of DOS-treated patients compared to 5–16.1% for that of DCS-treated patients, and nausea was observed in 0% of DOS-treated patients compared with 4.7–32.3% for that of DCS-treated patients. These results indicated that the substitution of oxaliplatin for cisplatin had a positive influence on relieving treatment-related toxicities.
Since the current study was a phase I trial and the number of participants was small, evaluation of the response rate was not the primary objective. However, DOS therapy showed a relatively high clinical efficacy of 79.1% for an objective response rate, including two cases showing complete responses and no disease progression cases, and a conversion therapy rate of 31.3% (5/16). It is worth noting that even though a relatively high proportion of patients in the current study had peritoneal metastasis (75%), which typically indicates poor prognosis for gastric cancer patients, promising survival rates were observed in this study (median OS and PFS were 19.5 and 7.6 months, respectively). These results are consistent with the results from the DCS study, which showed a relatively good OS of 16.8 months for patients with peritoneal metastasis [15].
Even though the current study was an initial phase I study, the efficacy and safety results were favorable and comparable to those obtained by Kim et al., using a previously reported Korean DOS regimen with an overall response rate of 54.5%, a median PFS of 7.6 months, and a median OS of 12.0 months [22]. The differences between the two DOS regimens can be summarized. First, the Korean DOS regimen consisted of docetaxel at 52.5 mg/m2 and oxaliplatin at 105 mg/m2 on day 1 plus S-1 at 40 mg/m2 on days 1–14, every 3 weeks. The dose of each of the three drugs is similar to the doses used in our DOS regimen. However, for our DOS regimen, both docetaxel and oxaliplatin were administered on day 8 compared to day 1 for that of the Korean DOS regimen. The rationale we used for the administration of docetaxel and oxaliplatin on day 8, and not on day 1, was based on results from a pilot study in which we observed severe neutropenia in patients on days 7–14 when both drugs were administered on day 1. In fact, findings from the Korean phase I study included the development of grade 4 neutropenia from days 6–10 on their schedule, which often resulted in the discontinuation of the administration of S-1. In our DOS regimen, myelosuppression developed primarily on days 15–20, which overlapped with the drug resting period, and therefore, in most cases there was no need to discontinue the administration of S-1, which could have resulted in an increase in treatment efficacy. Second, with the Korean DOS regimen, peripheral neuropathy of some grade was observed in most patients (88.4%) with grade 3 peripheral neuropathy being observed in 6 of the 11 patients who received nine or more cycles of chemotherapy [22]. In contrast, results from our study showed no grade 3/4 peripheral neuropathy, which may have been due to the fact that the administration of oxaliplatin was planned for up to eight cycles and, therefore, the accumulated dose of oxaliplatin in most patients was no more than 600–700 mg/m2, which is a threshold cumulative dose for the development of oxaliplatin-induced neurotoxicity [23].
Conversion therapy is defined as the adjuvant surgery aimed at achieving R0 resection post-chemotherapy for tumors initially considered unresectable for technical and/or oncological reasons. At present, conversion therapy is an option for unresectable metastatic gastric cancer when distant metastases are controlled by chemotherapy [12]. Aggressive induction chemotherapies such as triplet chemotherapy that may lead to a high response rate are necessary for conversion therapy. While most appropriate chemotherapy regimens remain to be determined, we reported that a DCS regimen is a suitable candidate since it shows a good conversion rate (33.3%) and contributes to a good prognosis with an MST of 48 months and 5-year OS of 42.4% in cases including conversion therapy [10]. In the current study, five patients (31.3%) underwent conversion therapy with R0 resection and their median survival time had not been reached with a median follow-up time of 19 months.
Overall, our findings suggested that DOS therapy may be exploited as a substitutional regimen for DCS and it was effective enough to allow for the attempt of conversion therapy. Moreover, our DOS regimen was more convenient for patients compared to that of the DCS regimen, which requires pre-hydration and post-hydration to prevent cisplatin-induced renal toxicity. Hence, the DOS regimen used in the current study was more feasible for use with patients receiving treatment in an outpatient setting.
In conclusion, the RD of the DOS regimen in patients with metastatic gastric cancer was docetaxel at 50 mg/m2 and oxaliplatin at 100 mg/m2 on day 8 with S-1 at 80 mg/m2 on days 1–14 of every 21-day cycle. This triplet combination, if used with proper monitoring and appropriate management for FN, was a tolerable and convenient therapeutic strategy for patients with advanced gastric cancer. The efficacy and ease of administration make the regimen a promising alternative to DCS, especially for potential candidates of conversion therapy. On the basis of the encouraging results of this Phase I study, we are currently conducting a phase II trial to better delineate the safety profile and to evaluate the efficacy of this triweekly DOS regimen.
References
Ferlay J, Soerjomataram I, Dikshit R et al (2014) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–E386
Saka M, Morita S, Fukagawa T, Katai H (2011) Present and future status of gastric cancer surgery. Jpn J Clin Oncol 41:307–313
Shah MA (2015) Update on metastatic gastric and esophageal cancers. J Clin Oncol 33:1760–1769
Ohtsu A (2008) Chemotherapy for metastatic gastric cancer: past, present, and future. J Gastroenterol 43:256–264
Van Cutsem E, Moiseyenko VM, Tjulandin S et al (2006) Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: a report of the V325 Study Group. J Clin Oncol 24:4991–4997
Cunningham D, Starling N, Rao S et al (2008) Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 358:36–46
Koizumi W, Narahara H, Hara T et al (2008) S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol 9:215–221
Yamada Y, Higuchi K, Nishikawa K et al (2015) Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naïve patients with advanced gastric cancer. Ann Oncol 26:141–148
Bang Y-J, Van Cutsem E, Feyereislova A et al (2010) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positiveadvanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376:687–697
Sato Y, Ohnuma H, Nobuoka T et al (2017) Conversion therapy for inoperable advanced gastric cancer patients by docetaxel, cisplatin, and S-1 (DCS) chemotherapy: a multi-institutional retrospective study. Gastric Cancer 20:517–526
Fukuchi M, Ishiguro T, Ogata K et al (2015) Prognostic role of conversion surgery for unresectable gastric cancer. Ann Surg Oncol 22:3618–3624
Yoshida K, Yamaguchi K, Okumura N et al (2015) Is conversion therapy possible in stage IV gastric cancer: the proposal of new biological categories of classification. Gastric Cancer 19:329–338
Takayama T, Sato Y, Sagawa T et al (2007) Phase I study of S-1, docetaxel and cisplatin combination chemotherapy in patients with unresectable metastatic gastric cancer. Br J Cancer 97:851–856
Sato Y, Takayama T, Sagawa T et al (2009) Phase II study of S-1, docetaxel and cisplatin combination chemotherapy in patients with unresectable metastatic gastric cancer. Cancer Chemother Pharmacol 66:721–728
Ohnuma H, Sato Y, Hirakawa M et al (2018) Docetaxel, cisplatin and S-1 (DCS) combination chemotherapy for gastric cancer patients with peritoneal metastasis: a retrospective study. Cancer Chemother Pharmacol 81:539–548
Uemura N, Kikuchi S, Sato Y et al (2017) A phase II study of modified docetaxel, cisplatin, and S-1 (mDCS) chemotherapy for unresectable advanced gastric cancer. Cancer Chemother Pharmacol 80:707–713
Mitsui Y, Sato Y, Miyamoto H et al (2015) Trastuzumab in combination with docetaxel/cisplatin/S-1 (DCS) for patients with HER2-positive metastatic gastric cancer: feasibility and preliminary efficacy. Cancer Chemother Pharmacol 76:375–382
Hirakawa M, Sato Y, Ohnuma H et al (2013) A phase II study of neoadjuvant combination chemotherapy with docetaxel, cisplatin, and S-1 for locally advanced resectable gastric cancer: nucleotide excision repair (NER) as potential chemoresistance marker. Cancer Chemother Pharmacol 71:789–797
Association JGC (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14:101–112
Koizumi W, Nakayama N, Tanabe S et al (2011) A multicenter phase II study of combined chemotherapy with docetaxel, cisplatin, and S-1 in patients with unresectable or recurrent gastric cancer (KDOG 0601). Cancer Chemother Pharmacol 69:407–413
Yamada Y, Boku N, Mizusawa J et al (2018) Phase III study comparing triplet chemotherapy with S-1 and cisplatin plus docetaxel versus doublet chemotherapy with S-1 and cisplatin for advanced gastric cancer (JCOG1013). J Clin Oncol 36(15_suppl):4009–4009
Kim HS, Ryu M-H, Zang DY et al (2015) Phase II study of docetaxel, oxaliplatin, and S-1 therapy in patients with metastatic gastric cancer. Gastric Cancer 19:579–585
Krishnan AV, Park SB (2014) Chemotherapy-induced peripheral neuropathy: the end of the beginning? J Neurol Neurosurg Psychiatry 85:359–359
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Sato, Y., Sagawa, T., Ohnuma, H. et al. A dose-escalation study of docetaxel, oxaliplatin, and S-1 (DOS) as a first-line therapy for patients with unresectable metastatic gastric cancer. Cancer Chemother Pharmacol 83, 161–167 (2019). https://doi.org/10.1007/s00280-018-3719-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-018-3719-0