Abstract
Purpose
We conducted a prospective study to evaluate the efficacy and safety of biweekly gemcitabine and carboplatin combination treatment in patients with resected non-small cell lung cancer (NSCLC).
Methods
Patients with completely resected stage IB to IIIA NSCLC were treated with four cycles of gemcitabine (1000 mg/m2, days 1 and 15) plus carboplatin [area under the time-concentration curve (AUC) 5 mg/mL/min, day 1] every 4 weeks as adjuvant chemotherapy.
Results
Forty-three patients were enrolled in this study. The median number of treatment cycles was four. The completion rate of chemotherapy was 79.1%. Major grade 3/4 hematological adverse events included leukocytopenia (27.9%) and neutropenia (53.5%), whereas non-hematological toxicities were generally mild. Ten patients (23.3%) required chemotherapy treatment schedule delay, and one patient required one dose level reduction because of drug fever. Median disease-free survival was 78.6 months [95% confidence interval (CI) 39.5–not reached (NA)] and median overall survival was not reached (95% CI 83.7–NA).
Conclusions
Biweekly administration of gemcitabine and carboplatin is effective and well tolerated for patients with completely resected NSCLC as an adjuvant chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the most common cause of cancer-related mortality worldwide, accounting for 27% of all cancer death in 2016 [1]. Non-small cell lung cancer (NSCLC) comprises 85% of all primary lung cancers [1]. Surgery is the best therapeutic strategy for patients with early-stage NSCLC; however, the prognosis after surgery remains unsatisfactory. As per the Lungscape study, 5-year relapse-free survival (RFS) rate was 52.8 months for all stages [2]. According to the pathological stage, RFS was 62.5% for stage IA, 57.8% for stage IB, 47.9% for stage IIA, 43.8% for stage IIIA, and 13.2% for stage IIIB.
To improve outcomes after complete resection, trials of adjuvant chemotherapy were conducted [3]. Pignon JP et al. authored a meta-analysis of the five largest trials, the lung adjuvant cisplatin evaluation (LACE), demonstrating that cisplatin-based adjuvant chemotherapy had a 5-year survival benefit of 5.4% and an overall hazard ratio of death of 0.89 [4]. Subgroup analyses in the LACE study indicated that the combination of cisplatin plus vinorelbine produced a significant survival benefit for the patients with stage II and stage III cancers [5]. Therefore, the cisplatin plus vinorelbine regimen is currently recommended as an adjuvant chemotherapy for patients with stage II and IIIA NSCLC. Meanwhile, carboplatin-based regimens were also tested as an adjuvant chemotherapy [6, 7] because the cisplatin-based adjuvant chemotherapy completion rate was low due to toxicities such as nausea, vomiting, and nephrotoxicity.
Gemcitabine (2′, 2′-difluoro-deoxycytidine) is a pyrimidine antimetabolite that is efficacious for NSCLC treatment [8]. The combination of cisplatin plus gemcitabine is used clinically for chemotherapy-naïve patients with advanced NSCLC [9]. As for a histology of squamous cell lung carcinoma, overall survival (OS) for patients receiving cisplatin plus gemcitabine was superior to those receiving cisplatin plus pemetrexed [10]. Additionally, a phase III randomized trial of cisplatin plus gemcitabine versus carboplatin plus gemcitabine, revealed that carboplatin plus gemcitabine had comparable antitumor efficacy with lower toxicity in patients with advanced NSCLC [11]. This regimen exhibits well-balanced efficacy and safety.
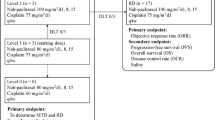
Recently, we reported a phase I dose escalation study of biweekly gemcitabine and carboplatin as adjuvant chemotherapy in patients with completely resected stage IB-IIIA NSCLC. In this study, the maximum-tolerated dose was not reached and the recommended dose for a phase II study was gemcitabine 1000 mg/m2 on days 1 and 15 and carboplatin area under the time-concentration curve (AUC) 5 on day 1, every 4 weeks. This protocol had acceptable toxicity in adjuvant settings [12]. Our adjuvant regimen was tolerable and feasible for patients with early-stage cancers who received complete resection. Based on the above findings, we conducted a phase II study to evaluate the efficacy and safety of biweekly gemcitabine and carboplatin as adjuvant chemotherapy in patients with completely resected NSCLC.
Materials and methods
Patient eligibility
To be eligible for this study, patients were required to have had complete resection pathologically documented stage IB, IIA, IIB, or IIIA NSCLC; only a single station of a resected mediastinal lymph nodule; no previous chemotherapy or radiotherapy; a performance status (PS) of 0–1; age over 20 years; a life expectancy of more than 12 weeks; adequate bone marrow reserves (leukocyte count ≥ 4000/mm3 and ≤ 12,000/mm3, neutrophil count ≥ 2000/mm3, platelet count ≤ 100,000/mm3, and hemoglobin ≥ 9.5 g/dL); normal liver function [total serum bilirubin ≤ 2.0 mg/dL, and aspartate transaminase (AST), alanine transaminase (ALT) ≤ 100 IU/L]; normal renal function (serum creatinine ≤ 1.5 mg/dL); and PaO2 ≥ 60 Torr. Patients with a concomitant malignancy, active infectious disease, or other serious medical problems were excluded. The local ethics committee approved the study and written informed consent was obtained from all patients. Patients with interstitial pneumonia detectable on chest radiography, uncontrolled pleural or pericardial effusions, superior vena cava syndrome, peripheral neuropathy ≥ grade 2, edema ≥ grade 2, uncontrolled diabetes, hypertension, liver dysfunction, unstable angina, myocardial infarction within the previous 3 months, clinically severe infections, symptomatic brain metastases, active double cancers, history of severe allergic reactions, severe disease complications, or new (before entry) lesions were ineligible.
Clinical evaluation
Patients were evaluated prior to treatment with a complete blood cell count, a differential count, routine chemistry measurements, a chest radiograph, chest computed tomography (CT) scan, abdominal CT scan, whole-brain magnetic resonance imaging or CT scan, and an isotope bone scan. Weekly evaluations included complete blood cell count, differential count, routine chemistry measurements, physical examination, and toxicity assessment. Toxicities were evaluated according to NCI-CTCAE version 4.0.
Treatment schedule
Patients received four cycles of gemcitabine 1000 mg/m2 on days 1 and 15 and carboplatin AUC 5 mg/mL/min on day 1, starting within 8 weeks of lung resection. The regimen was performed every 4 weeks. Before administration of the anticancer agent, each patient received antiemetic agents consisting of 5-HT3 antagonist and dexamethasone intravenously. Prophylactic administration of granulocyte-colony stimulating factor (G-CSF) was not permitted. Administration of G-CSF was permitted in patients with grade 4 neutropenia and/or grade 3 febrile neutropenia. Gemcitabine was delayed in case of leukocyte count ≤ 3,000/mm3, neutrophil count ≤ 1500/mm3, platelet count ≤ 100,000/mm3, fever with infections, liver and renal and lung toxicity, peripheral neuropathy ≥ grade 2, or non-hematological toxicity ≥ grade 3 on day 15. The maximum delay was 2 weeks. Subsequent courses of chemotherapy were initiated when the leukocyte counts were ≥ 3000/mm3, neutrophil counts were ≥ 1500/mm3, and platelet counts were ≥ 100,000/mm3, and there was no fever with infections, aspartate liver functions, peripheral neuropathy ≤ grade 1, edema ≤ grade 1, and liver and cardiac and lung toxicity ≤ grade 1 after day 29. If these criteria were unmet by day 1 of the next course of chemotherapy, both drugs were withheld until full recovery, with a maximum delay of 2 weeks. Dose reduction was performed on any patient who presented grade 4 leukopenia, grade 4 neutropenia for ≥ 4 days, febrile neutropenia, liver toxicity ≥ grade 2, or peripheral neuropathy ≥ grade 2. Any patient with these toxicities after dose reduction, reappearance of lesions, or ≥ 2 week delay before the subsequent chemotherapy course was withdrawn from the study. Treatment carried out four courses, unless unacceptable toxicity or disease progression occurred.
Statistical analysis
The primary end point of this study was the proportion of patients who were disease-free at 1 year. Secondary end points were safety and survival. Assuming 1 year disease-free survival of 70% in eligible patients would indicate potential usefulness, whereas a 1 year disease-free survival of 50% would constitute the lower limit of interest; with α = 0.05 and β = 0.20, the estimated accrual was 43 patients.
Results
Patient characteristics
Between August 2006 and June 2014, 43 patients were enrolled in this study. The patient characteristics are summarized in Table 1. The median age of the patients was 65 years with range of 49–74 years. Twenty-nine patients (67.4%) were male and all patients were PS of 0. Twenty-nine patients (67.4%) were diagnosed with adenocarcinoma. Ten patients (23.3%) had stage IIIA disease.
Safety
The toxicity of chemotherapy is summarized in Table 2. Major grade 3/4 hematological adverse events (AEs) included: leukocytopenia (27.9%), neutropenia (53.5%) and anemia (4.7%). Non-hematologic AEs were generally mild and grade 3/4 non-hematological toxicities included nausea (2.3%) and anorexia (2.3%). Interstitial lung disease (ILD) and treatment-related death were not observed in our study.
The median number of treatment cycles was four (1–4). Thirty-four patients received four cycles of chemotherapy, as planned, and the completion rate of chemotherapy was 79.1% [95% confidence interval (CI) = 0.64–0.90]. Nine patients received fewer than four cycles because of patient refusal (33.3%) and toxicities (66.7%). The completion rates in patients with stage IB, IIA, IIB and IIIA were 100, 80.9, 62.5 and 80.0%, respectively.
Treatment efficacy
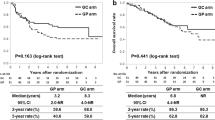
The 1-year disease-free survival rate was 86.0% (95% CI = 0.72–0.95); 1-year disease-free rates in patients with stage IB, IIA, IIB and IIIA were 100, 85.7, 100 and 70%, respectively. Median disease-free survival (DFS) was 78.6 months [95% CI = 39.5 to not reached (NA); Fig. 1]; median DFS in patients with stage IB, IIA, IIB and IIIA were 77.5 months (95% CI = 77.5–NA), 42.1 months (95% CI = 25.7–NA), not reached (95% CI = 63.0–NA) and 19.0 months (95% CI = 8.6–NA), respectively. Median OS was not reached (95% CI = 83.7–NA; Fig. 2); median OS in patients with stage IB, IIA, IIB and IIIA were 82.5 months (95% CI = 82.5–NA), not reached (95% CI = 44.4–NA), not reached (95% CI = 76.8–NA), and 84.4 months (95% CI = 32.2–NA), respectively.
The sites of disease recurrence are shown in Table 3. The rate of local and distant recurrence was 7.0 and 37.2%, respectively. The most frequent site of distant recurrence was pulmonary metastasis (20.9%), and pulmonary metastases alone were observed in 14.0% of patients with any recurrences. CNS metastasis (including meningitis carcinomatosa) and brain metastasis alone were 7.0 and 4.7%, respectively. Multiple distant metastases were only recognized in 14%.
Discussion
This phase II study evaluated the efficacy and safety of biweekly gemcitabine and carboplatin treatment in patients with completely-resected NSCLC. The results of our study demonstrated that the combination of biweekly gemcitabine and carboplatin as adjuvant chemotherapy had less toxicity and was associated with higher completion rates.
Carboplatin causes thrombocytopenia, but severe nausea, vomiting and nephrotoxicity are less frequent compared to cisplatin, in previous meta-analyses [13,14,15]. In our study, thrombocytopenia, nausea, and vomiting were recognized in 51.2, 41.9, and 11.6% of patients, respectively, but no grade 3/4 AE toxicities were observed. Gemcitabine causes thrombosis and induces ILD [16,17,18], but we did not observe these AEs in our study. Grade 4 toxicity, limited to neutropenia, was observed in 18.6% of patients with no treatment-related deaths. While severe toxicity was not observed in our schedule, ten patients (23.3%) required delay and one patient (2.3%) required one-level dose reduction. Because of the reduced toxicity, the completion rate of chemotherapy was 79.1% and only six patients (14.0%) received fewer than four cycles.
Previous adjuvant chemotherapy studies are summarized in Table 4. Compared to previous studies, the rate of overall grade 3/4 toxicities was 66% in four trials and the rate of overall grade 4 toxicities was 32% in five trials in the LACE meta-analysis [4]. In these trials, only 59% patients received at least 240 mg/m2 of cisplatin due to its high toxicity, and treatment-related deaths occurred in 19 patients (0.9%). Adjuvant chemotherapy completion rates were generally low; the rate was 48% in the JBR-10 trial, 50% in Adjuvant Navelbine International Trials Association (ANITA) and 76% in the LACE meta-analysis [4, 19, 20]. The major reasons for receiving fewer than the planned number of cycles included patient’s refusal (35%), toxicity (34%), and early death or progression (9%) in LACE meta-analysis [4]. Considering the frequency of toxicity profiled in adjuvant setting in previous studies, our regimen appears less toxic and possibly higher completion rates because of the carboplatin-based regimen and biweekly gemcitabine treatment schedule. A biweekly schedule of chemotherapy has been performed in the treatment of NSCLC since it maintains dose intensity with a better toxicity profile [21].
To date, two studies have reported the combination of gemcitabine and carboplatin in patients with completely resected NSCLC as adjuvant chemotherapy [22, 23]. Uramoto et al. and the CJLSG 0503 reported a 69 and 85% chemotherapy completion rate, respectively, similar to the completion rates in our study. Uramoto et al. observed greatest toxicity as neutropenia (80.6%), and grade 3/4 neutropenia was observed in 52.8% of patients, while thrombocytopenia was observed in only 25%, and no grade 3/4 thrombocytopenia was observed [22]. In the CJLSG 0503 trial, grade 3/4 neutropenia and thrombocytopenia were observed in 65 and 40% of patients, respectively [23]. In our study, the grade 3/4 neutropenia rate was 53.5%, and no grade 3/4 thrombocytopenia was observed. Such differences in these toxicity profiles might be due to therapeutic schedule differences, intervals, and the dose of carboplatin.
Disease recurrence after adjuvant chemotherapy is a serious problem, and contributes to shorter survival after surgical resection. Uramoto et al. reported that the most frequent distant recurrence was hematogenous metastasis; the rate of local and distant recurrence in both regimens of biweekly carboplatin plus gemcitabine and carboplatin plus paclitaxel was 8.0 and 25.3%, respectively [22]. In the ANITA study, local and distant recurrence rates were lower in the chemotherapy group than in the observation group (local relapse, 12 vs 18%, distant relapse, 25 vs 28%; Table 4). Pulmonary metastasis was the most common site of relapse (chemotherapy, 22% vs control, 28%) [20]. Bone metastasis was lower in the chemotherapy group than in the observation group (4 vs 11%), whereas brain metastasis was more frequent in the chemotherapy group than in the observation group (13 vs 10%); brain metastasis alone was 9, and 8% in the chemotherapy group and observation group, respectively [20]. While our relapse rate and recurrence sites were similar to the ANITA study, our regimen may suppress the occurrence of brain metastases, and multiple distant metastases, compared with other regimens.
In our study, median DFS was 78.6 months (95% CI 39.5–NA), and median OS was not reached (95% CI 83.7–NA). Median DFS and OS did not statistically differ by pathological stage (p = 0.138, 0.472, respectively). On the contrary, in the JBR-10 study, median DFS was not reached in the adjuvant chemotherapy group at the time of follow-up, ranging from 1.5 to 9.3 years (median, 5.1 years), and 46.7 months in the surgery-alone group; median OS was 94 months in the adjuvant chemotherapy group and 73 months in the surgery-alone group [19]. In the ANITA study, median DFS was 36.3 months in the adjuvant chemotherapy group and 20.7 months in the surgery-alone group; median OS was 65.7 months in the adjuvant chemotherapy group and 43.7 months in the surgery-alone group [20]. Median DFS and OS in our study were comparable with previous cisplatin-based studies (Table 4). Because of less toxicity and the suppression of brain metastases and multiple distant metastases, the patients could keep good PS, and receive subsequent treatment, which contributed to longer OS. It may be difficult to discuss the survival benefit of our regimen, because of the short follow-up period and small sample size. Nevertheless, we believe that our regimen is less toxic and suppresses CNS and multiple distant metastases so that patients with lung cancer after complete resection can receive adjuvant chemotherapy without deterioration of PS.
In conclusion, biweekly administration of gemcitabine and carboplatin is effective for disease control and is well tolerated by patients with completely resected NSCLC as adjuvant chemotherapy. Further study should include a randomized, phase III study to evaluate the practical significance of the biweekly gemcitabine and carboplatin combination regimen as adjuvant chemotherapy.
References
Siegel RL, Miller KD, Jemal A et al (2016) Cancer statistics, 2016. CA Cancer J Clin 66:7–30
Peters S, Weder W, Dafni U et al (2014) Lungscape: resected non-small-cell lung cancer outcome by clinical and pathological parameters. J Thorac Oncol 9:1675–1684
Buffoni L, Vavalà T, Novello S (2016) Adjuvant therapy of resected non-small cell lung cancer: can we move forward? Curr Treat Options Oncol 17:54
Pignon JP, Tribodet H, Scagliotti GV et al (2008) Lung adjuvant cisplatin evaluation: a pooled analysis by the LACE collaborative group. J Clin Oncol 26:3552–3559
Douillard JY, Tribodet H, Aubert D et al (2010) Adjuvant cisplatin and vinorelbine for completely resected non-small cell lung cancer. J Thorac Oncol 5:220–228
Okumura N, Sonobe M, Okabe K et al (2017) Feasibility of adjuvant chemotherapy with S-1 plus carboplatin followed by single-agent maintenance therapy with S-1 for completely resected non-small-cell lung cancer: results of the setouchi lung cancer group study 1001. Int J Clin Oncol 22:274–282
Schmid-Bindert G, Engel-Riedel W, Reck M et al (2015) A randomized phase 2 study of pemetrexed in combination with cisplatin or carboplatin as adjuvant chemotherapy in patinets with completely resected stage IB or II non-small-cell lung cancer. Lung Cancer 90:397–404
Barton-Burke M (1999) Gemcitabine: a pharmacologic and clinical overview. Cancer Nurs 22:176–183
Ohe Y, Ohashi Y, Kubota K et al (2007) Randomized phase III study of cisplatin plus irinotecan versus carboplatin plus paclitaxel, cisplatin plus gemcitabine, and cisplatin plus vinorelbine for advanced non-small-cell lung cancer: Four-arm cooperative study in Japan. Ann Oncol 18:317–323
Scagliotti GV, Parikh P, von Pawel J et al (2008) Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol 26:3543–3551
Zatloukal P, Petruzelka L, Zemanov M et al (2003) Gemcitabine plus cisplatin vs. gemcitabine plus carboplatin in stage IIIb and IV non-small cell lung cancer: a phase III randomized trial. Lung Cancer 41:321–331
Tomizawa Y, Ishihara S, Iijima H et al (2007) A phase I dose escalation study of biweekly gemcitbine and carbopatin in completely resected stage IB-IIIA nonsmall cell lung cancer. Am J Clin Oncol 30:498–502
Jiang J, Liang X, Zhou X et al (2007) A meta-analysis of randomized controlled trials comparing carboplatin-based to cisplatin-based chemotherapy in advanced non-small cell lung cancer. Lung Cancer 57:348–358
Ardizzoni A, Boni L, Tiseo M, CISCA (CISplatin versus CArboplatin) Meta-analysis Group et al (2007) Cisplatin versus carboplatin-based chemotherapy in first-line treatment of advanced non-small-cell lung cancer: an individual patient data meta-analysis. J Natl Cancer Inst 99:847–857
Hotta K, Matsuo K, Ueoka H et al (2004) Meta-analysis of randomized clinical trials comparing cisplatin to carboplatin in patients with advanced non-small-cell lung cancer. J Clin Oncol 22:3852–3859
Abratt RP, Bezwoda WR, Falkson G et al (1994) Efficacy and safety profile of gemcitabine in non-small-cell lung cancer: a phase II study. J Clin Oncol 12:1535–1540
Anderson H, Lund B, Bach F et al (1994) Single-agent activity of weekly gemcitabine in advanced non-small-cell lung cancer: a phase II study. J Clin Oncol 12:1821–1826
Gatzemeier U, Shepherd FA, Le Chevalier T et al (1996) Activity of gemcitabine in patients with non-small cell lung cancer: a multicenter, extended phase II study. Eur J Cancer 32A:243–248
Winton T, Livingston R, Johnson D et al (2005) Vinorelbine plus cisplatin vs observation in resected non-small-cell lung cancer. N Engl J Med 352:2589–2597
Douillard J, Rosell R, De Lena M et al (2006) Adjuvant vinorelbine plus cisplatin versus observation in patients with completely resected stage IB-IIIA non-small-cell lung cancer [Adjuvant Navelbine International Trialist Association (ANITA)]: a randomized controlled trial. Lancet Oncol 7:719–727
Lopez-Vivanco G, Viteri A, Barcelo R et al (2005) Biweekly administration of cisplatin/gemcitabine in advanced nonsmall cell lung cancer. Am J Clin Oncol 28:501–507
Uramoto H, Nakanishi R, Nagashima A et al (2010) A randomized phase II trial of adjuvant chemotherapy with bi-weekly carboplatin plus paclitaxel versus carboplatin plus gemcitabine in patients with completely resected non-small cell lung cancer. Anticancer Res 30:4695–4700
Usami N, Yokoi K, Hasegawa Y et al (2010) Phase II study of carboplatin and gemcitabine as adjuvant chemotherapy in patients with completely resected non-small cell lung cancer: a report from the Central Japan Lung Study Group, CJLSG 0503 trial. Int J Clin Oncol 15:583–587
Acknowledgements
We thank Dr. Kuniaki Suzuki and Dr. Yosuke Kamide for their help with the data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Reiko Sakurai declares that she has no conflict of interest. Author Yoshio Tomizawa declares that he has no conflict of interest. Author Akihiro Yoshii declares that he has no conflict of interest. Author Yosuke Miura declares that he has no conflict of interest. Author Hiroaki Tsurumaki declares that he has no conflict of interest. Author Kyoichi Kaira declares that he has no conflict of interest. Author Noriaki Sunaga declares that he has no conflict of interest. Author Osamu Kawashima declares that he has no conflict of interest. Author Takeshi Hisada declares that he has no conflict of interest. Author Masanobu Yamada declares that he has no conflict of interest. Author Ryusei Saito declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Yoshio Tomizawa—Deceased.
Rights and permissions
About this article
Cite this article
Sakurai, R., Tomizawa, Y., Yoshii, A. et al. A phase II study of biweekly gemcitabine and carboplatin in completely resected stage IB-IIIA non-small cell lung cancer. Cancer Chemother Pharmacol 81, 103–109 (2018). https://doi.org/10.1007/s00280-017-3439-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-017-3439-x