Abstract
Purpose
Triplet therapy using docetaxel, cisplatin, and S-1 (DCS) against unresectable gastric cancer as previously reported by us showed high clinical efficacy, with a 87.1% total response rate; however, it also showed a high incidence of grade 3/4 toxicity. With the aim of reducing toxicities, we conducted a phase II study of modified DCS (mDCS), using a reduced dose of docetaxel, and evaluated the clinical efficacy and adverse events of this regimen.
Methods
Patients with unresectable gastric cancer received chemotherapy with S-1 (40 mg/m2 b.i.d) on days 1–14, and docetaxel (50 mg/m2) plus cisplatin (60 mg/m2) on day 8 every 3 weeks. The primary endpoint was the response rate (RR). Overall (OS) and progression-free survival (PFS), and toxicities were also evaluated.
Results
Forty-nine patients were enrolled from November 2011 to April 2014, and 43 were eligible. The overall RR was 79.1%, including two cases of a complete response (4.7%), and 32 cases of a partial response (74.4%). Nine cases had stable disease (20.9%) but none showed progressive disease. Of the 43 cases, 15 cases (34.9%) underwent curative conversion surgery. The median PFS was 350 days (95% CI 240–416 days) and median OS was 722 days (95% CI 411 days–not reached). Grade 3/4 neutropenia developed in 79.1%, and febrile neutropenia in 34.9%, of patients. Non-hematological grade 3/4 adverse events were anorexia (25.6%), nausea (4.7%), and diarrhea (9.3%).
Conclusion
Modified DCS therapy showed high clinical efficacy sufficient enough to attempt conversion therapy against unresectable gastric cancer. Modified DCS showed fewer toxicities, but careful management of these is still essential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the incidence of gastric cancer has been decreasing, because of the prevalence of unresectable advanced disease at diagnosis, gastric cancer remains a major cause of cancer-related deaths worldwide [1]. Systemic chemotherapy is considered the principal treatment option for unresectable gastric cancer, with evidence of a survival benefit provided by a number of controlled phase III trials and meta-analyses [2,3,4,5]. In Japan, a S-1 plus cisplatin (CS) doublet regimen is considered the standard first-line regimen, showing a 54% response rate and a median overall survival (OS) of 13.0 months in the SPIRITS trial [6]. An S-1 plus oxaliplatin (SOX) regimen is also considered an alternative regimen, being non-inferior to CS in terms of progression-free survival (PFS) in a phase III trial directly comparing SOX with CS [7]. Adding a molecular targeting agent is expected to improve clinical outcomes. The ToGA trial showed improved efficacy in survival after the addition of the molecular targeting agent, Trastuzumab, in human epidermal growth factor receptor 2 (HER2)-positive gastric cancer compared to chemotherapy alone, but the median OS was 13.8 months, and never beyond 1.5 years, while the incidence of HER2-positive gastric cancer was limited [8]. Ramucirumab, a monoclonal antibody targeting vascular endothelial growth factor receptor 2 (VEGFR2), showed clinically better PFS and OS with monotherapy, or in combination with paclitaxel, compared with placebo control or paclitaxel alone in patients previously treated with fluoropyrimidine or platinum-containing chemotherapy [9, 10]. Ramucirumab is being evaluated for efficacy as a first-line therapy combined with capecitabine and cisplatin in the RAINFALL phase III trial. Although multiple agents have been active and multiple trials have been conducted, there is no globally accepted first-line therapy against unresectable gastric cancer. The main purpose of systemic chemotherapy remains the palliation of symptoms and the prolongation of survival, but its effect remains unsatisfactory.
“Conversion therapy” refers to combined therapy with systemic chemotherapy, followed by radical surgical treatment, after which down-staging occurs in selected patients who undergo systemic chemotherapy. R0 resection of conversion therapy is associated with longer survival in unresectable metastatic advanced gastric cancer, suggesting a curable capability that is not expected with chemotherapy alone [11,12,13,14,15]. To achieve down-staging and proceed to conversion therapy, aggressive induction chemotherapy, such as a triplet regimen that can lead to a high response rate, is considered essential. Triplet combination therapy would be a good candidate in this setting.
We previously reported the result of triplet combination therapy with docetaxel, cisplatin, and S-1 (DCS) for the treatment of gastric cancer [16,17,18]. A phase II study showed quite high clinical efficacy, with an 87.1% total response rate, including a 3.2% complete response, 25.8% of patients achieving down-staging, and 22.6% undergoing a conducted curative surgical treatment [17]. However, DCS therapy also showed a high incidence of grade 3/4 hematologic toxicities, such as 77.4% neutropenia, as well as grade 3 non-hematologic toxicities, such as 35.3% anorexia and 32.3% nausea. To reduce the incidence of such adverse events, we modified DCS therapy using a reduced dose of docetaxel.
We have subsequently conducted a phase II study of modified DCS (mDCS) for the treatment of unresectable advanced gastric cancer and evaluated the clinical efficacy and adverse events of this regimen. Furthermore, we analyzed the rate of achieving conversion therapy and the impact of conversion therapy on survival.
Materials and methods
Patient eligibility
Unresectable advanced gastric cancer patients were eligible for this study. Eligibility criteria included the following: histological diagnosis of adenocarcinoma; HER2 negative (IHC score of 0 or 1, or IHC score of 2 with FISH negative); aged between 20 and 80 years; PS of 0–1 on the Eastern Cooperative Oncology Group (ECOG) scale; no previous chemotherapy or radiotherapy treatment; adequate bone marrow function (WBC count >4.0 × 109/L; hemoglobin >8.0 g/dL; platelet count >100 × 109/L); adequate liver function (serum bilirubin level <1.5 mg/dL; serum transaminase level <100 IU/L); adequate renal function (serum creatinine level < upper normal limit; blood urea nitrogen level <25 mg/dL; creatinine clearance >60 mL/min); no other severe medical conditions; and the provision of written, informed consent. This study was approved by the ethics committee in each institution or hospital.
Treatment schedule
S-1 was administered orally twice daily on days 1–14 at a dose calculated according to the patient’s body surface area as follows: <1.25 m2, 40 mg; 1.25–1.5 m2, 50 mg; and >1.5 m2, 60 mg. Cisplatin was administered by intravenous infusion for 2 h at 60 mg/m2 in 5% glucose, followed by docetaxel at 50 mg/m2 in 5% glucose on day 8. To avoid cisplatin-induced renal dysfunction, adequate hydration of normally more than 2000 mL of normal saline on days 7–9 was administered. Antiemetic prophylactics were routinely used to prevent nausea and vomiting when cisplatin was administered according to American Society of Clinical Oncology (ASCO) guidelines [19]. Cycles were repeated every 3 weeks.
Assessment
Before treatment, each clinical stage was determined by physical examination, chest and gastrointestinal X-rays, upper gastrointestinal tract endoscopy, and abdominal computed tomography (CT). HER2 negative was determined by a IHC score of 0 or 1, or a IHC score of 2 with FISH negative. In the case of suspected bone metastasis, a bone scintigraphy study was added. Abdominal ascites puncture or diagnostic laparoscopic surgery was performed to confirm peritoneal metastasis by cytological or tissue diagnosis. Complete blood cell counts, liver function tests, and renal function tests were assessed at least once per week during treatment. CT scanning and imaging of measurable disease were performed once every cycle.
Tumor response was assessed according to the response evaluation criteria in solid tumors (RECIST) and Japanese Classification of Gastric Carcinoma 14th edition (3rd English edition) [20, 21]. Down-staging was defined as the disappearance of all lesions of distant metastases (M0 stage) for 4 weeks.
Toxicity was evaluated by the National Cancer Institute Common Toxicity Criteria Version 3.0. In the event of toxicity, the following treatment delays and dose reductions were planned. Cisplatin and docetaxel administration on day 8 was skipped in the case of a neutrophil count <1.5 × 109/L, platelet count <75 × 109/L, AST/ALT >100 IU/L, total bilirubin >1.5 mg/dL, serum creatinine > upper normal limit, fever >38.0 °C, grade 2 or higher diarrhea, or grade 2 or higher neuropathy. S-1 administration on day 1 in subsequent cycles was delayed in the case of a neutrophil count <1.5 × 109/L, platelet count <75 × 109/L, AST/ALT >100 IU/L, total bilirubin >1.5 mg/dL, serum creatinine > upper normal limit, ECOG PS 2 or 3, fever >38.0 °C, grade 2 or higher diarrhea, or grade 2 or higher neuropathy. If a patient developed one of the above adverse events during S-1 administration, S-1 was discontinued during that cycle. Doses of docetaxel, cisplatin, or S-1 were reduced if any of the following occurred during the previous cycle: febrile neutropenia, platelet count <50 × 109/L, or grade 3 or higher non-hematologic toxicities except nausea, vomiting, anorexia, fatigue, and hypersensitivity. Docetaxel and cisplatin were reduced by 10%. The S-1 dose was reduced as follows: 60–50, or 50–40 mg, twice daily, but the minimum daily dose was 40 mg twice daily. Treatment was continued until disease progression, unacceptable toxicity, the patient’s refusal, or the physician’s decision. When down-staging was achieved and patients were deemed able to tolerate a curative surgical operation, subsequent gastrectomy with lymph node dissection was performed.
Statistical methods
The primary endpoint of this study was the response rate (RR). Secondary endpoints were PFS, OS, and toxicities. The study design was based on a binominal distribution without planned interim analysis. Assuming a null hypothesis of 80% RR and an alternative hypothesis of 60% RR, with one-sided type I error = 0.05 and type II error = 0.1, it was necessary to enroll a minimum of 44 patients. PFS and OS were analyzed according to the Kaplan–Meier method using PRISM software. PFS was defined as the time from chemotherapy initiation until objective tumor progression or death. If the patient underwent conversion therapy, PFS was measured from initial treatment until the documentation of progression after surgery. OS was defined as the time from chemotherapy initiation until death from any cause.
Results
Patient characteristics
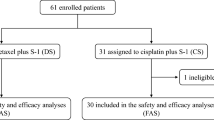
A total of 49 patients were enrolled, from November 2011 to April 2014, in this study. Six patients were excluded after enrolment as they did not meet the set eligibility criteria. Patient characteristics are outlined in Table 1. Patients included 27 males (62.8%) and 16 females (37.2%) with a median age of 59 years (range 31–79). Most patients were in good general condition with an ECOG PS of 0 (95.3%). Forty-one cases were unresectable because of distant metastasis and the other two patients were diagnosed as locally unresectable with direct invasion to an adjacent organ. The number of involved organs was one organ in 25 cases (58.1%), two in 13 cases (30.2%), and more than three organs in three cases (7.0%). The organs involved in distant metastasis included a lymph node in 22 cases (51.2%), peritoneum in 16 cases (37.2%), liver in 14 cases (32.6%), bone in four cases (9.3%), and lungs or adrenal glands in one case each (2.3%), respectively.
Efficacy
The median number of administrations was five courses (range 1–15). The overall response rate was 79.1%, including two cases of a complete response (4.7%), and 32 cases of a partial response (74.4%). Stable disease was observed in nine cases (20.9%) and progressive disease was not observed (Table 2). Of the 43 cases, 15 cases (34.9%) progressed to curative conversion surgery because of disappearing distant metastasis and/or down-staging. According to the number of involved metastatic organs, the one only involved organ group achieved conversion therapy (14 cases of 25, 56.0%; Table 3). With the regard to the lesion of the involved metastatic organ, the lymph node and peritoneum metastasis groups showed high conversion rates of 87.5 and 62.5%, respectively (Table 3). The median PFS as assessed by Kaplan–Meier analysis was 350 days (95% CI 240–416 days) and the median OS was 722 days (95% CI 411 days–not reached) in 429 days of the median follow-up time (range 100–1105 days; Fig. 1). The median survival time of cases with conversion therapy was not reached, compared to 413 days without conversion therapy (Fig. 2).
Toxicity
Toxicities during treatment are shown in Table 4. The most common grade 3/4 toxicities were leukopenia and neutropenia (79.1%), anorexia (25.6%), and anemia (18.6%). Febrile neutropenia was observed in 15 cases (34.9%). Cases developing febrile neutropenia were managed by the administration of the appropriate antibiotics and possibly also G-CSF administration. A dose reduction as planned prevented the recurrence of toxicities. In any case, such toxicities could be safely managed with proper treatment. No treatment associated death was observed.
Discussion
This study was conducted to investigate the clinical impact of primary dose modification for docetaxel in a DCS regimen. We previously reported phase I and II studies of DCS [oral S-1 (40 mg/m2 b.i.d.) on days 1–14 and intravenous cisplatin (60 mg/m2) and docetaxel (60 mg/m2) on day 8 every 3 weeks] [16, 17]. In the phase II study of DCS we undertook, we described the high clinical efficacy of a DCS regimen showing 87.1% of an objective response rate, including 3.2% of a complete response and good prolonged survival, with 226 days of PFS and 687 days of OS [17]. Notably, 25.8% of patients achieved down-staging as confirmed by disappearing distant metastasis, and 22.6% underwent conversion therapy. However, toxicities were also high, with incidences of 77.4% for neutropenia and 35.5% for anorexia, as the most common grade 3/4 hematologic and non-hematologic toxicities, respectively [17].
In this study, mDCS also showed a high clinical efficacy with 79.1% for an objective response rate including two cases of complete response and 34.9% for a conversion therapy rate. The median PFS (350 days) was not inferior to that of DCS (226 days). These findings suggest that mDCS therapy can act as a substitutional regimen for DCS, from the point of view of efficacy, and is effective enough to attempt conversion therapy. Toxicities observed for mDCS seemed not to be always remitted compared to DCS. Neutropenia and leukopenia, the most common grade 3/4 toxicities, were present in 79.1% of patients, similar to DCS (77.4%), and febrile neutropenia was present in 34.9% of patients (16.1% in DCS). These results were attributed to the shared myelosuppressive effect of each of the three drugs making up the mDCS regimen and it may be that to reduce hematological toxicities whole intensity reduction may be needed. In contrast to hematological toxicities, non-hematological toxicities showed a trend of reduced toxicity. Grade 3/4 anorexia was observed in 25.6% of patients (35.5% for DCS), nausea and vomiting in 4.7% of patients (32.3% for DCS), and diarrhea in 9.3% of patients (16.1% for DCS). These results came from the unshared non-hematologic toxicities that each drug could induce. A dose reduction for docetaxel had the positive result of alleviating non-hematologic toxicities. Taken together, mDCS therapy may be a promising triplet regimen, especially for potentially available conversion therapy candidates, showing equivalent efficacy and less non-hematological toxicity to DCS.
Triplet combination chemotherapy was developed as a regimen with high anti-tumor effect. Wagner et al. described the priority of a survival effect for triplet combination chemotherapy containing 5FU, anthracycline, and cisplatin in a meta-analysis [2]. Veer et al. reported that taxane within a triplet regimen (taxane, 5FU and cisplatin, or oxaliplatin) showed superior efficacy for PFS than a doublet regimen in a network meta-analysis [5]. In this analysis, an anthracycline-containing triplet regimen did not show statistical significance for both OS and PFS. Taxane may be a good partner for a triplet combination that includes 5FU and a platinum drug. Wang et al. reported in a randomized phase III trial that a triplet regimen with docetaxel, cisplatin, and 5FU (DCF) significantly prolonged PFS and OS (median PFS and OS: 7.2 and 10.2 months, respectively) compared with a doublet regimen with cisplatin and 5FU [CF; DCF vs. CF: median PFS; 7.2 months vs. 4.9 months (log-rank P = 0.0008): median OS, 10.2 months vs. 8.5 months (P = 0.0319)] [22]. Adding taxane is a reasonable choice for clinical efficacy and the un-sharing of non-hematological toxicities.
Similar to the phase II study of DCS, survival was prolonged in the conversion therapy group (Fig. 2). Conversion therapy combined with intensive chemotherapy is a strategy that looks promising as a possible cure for unresectable gastric cancer [23, 24]. Several studies have previously reported the prognostic role of combined surgery compared to chemotherapy alone for unresectable gastric cancer [12, 23, 25]. However, which regimen and patient group is most suitable for conversion therapy remains unclear. We have previously reported a retrospective analysis of three DCS studies that showed 84.8% of patients who achieved conversion therapy following DCS treatment (conversion rate was 33.3%) completed with an R0 resection, and 78.8% were confirmed as chemotherapeutic responders as determined by histological analysis [14]. Furthermore, our phase II study of DCS in a neoadjuvant setting for locally advanced resectable gastric cancer showed a 90.7% R0 resection rate and a 65.9% pathological response [18]. These findings suggest that a triplet combination regimen, with S-1, cisplatin, and docetaxel, is suitable for attempting conversion therapy with a high anti-tumor effect sufficient to eliminate distant metastasis, including micro-metastasis.
In this study, the only one involved organ group achieved conversion therapy, while the two or more involved organ groups did not achieve conversion therapy (Table 3). Similar to our study, Fukuchi et al. also reported that one non-curative factor was associated with a good prognosis after conversion therapy in an analysis of 40 patient conversion therapy cases of 151 unresectable gastric cancers treated with an S-1-based doublet regimen [12]. At a minimum, the only one involved organ group may be a promising candidate for conversion therapy. Furthermore, the number of involved organs was reported to be associated with the R0 resection rate, with 88.0% for one metastatic site and 44.4% for two or more metastatic sites [24]. Thus, to achieve down-staging by chemotherapy and a good prognosis after conversion therapy, the number of metastatic organs seems to be an important factor. This group could be further divided into two groups: potentially metastasis resectable or not. Even with resectable metastasis, induction chemotherapy prior to surgery may be necessary in order to eradicate micro-metastasis and achieve R0 surgery by tumor reduction. Yoshida et al. proposed to categorize stage IV gastric cancer into subgroups, based mainly on the presence or absence of peritoneal dissemination, and reported that longer survival could be expected in the category without peritoneal dissemination [13]. In our study, though distant metastasis with the peritoneum group achieved a similar conversion rate to that of the lymph node group, the prolonged survival seen with conversion therapy for the peritoneum group was limited compared to that of the lymph node group, which showed a dramatic and prolonged survival with conversion (Supplemental Figure). This result may come from the high relapse rate of the peritoneum after R0 surgery and can mainly be attributed to the difficulty of a precise diagnosis for a complete response against peritoneal metastasis. A special strategy for peritoneal metastasis, such as combined intra-peritoneal chemotherapy or developing a diagnostic technology such as repeated diagnostic laparoscopy, may be required.
In conclusion, modified DCS therapy, using a reduced dose of docetaxel, was effective enough to attempt conversion therapy against unresectable gastric cancer. Therapy with mDCS may be less toxic than DCS therapy but careful and proper monitoring and management of adverse events is essential, especially for hematological toxicities.
References
Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015. CA Cancer J Clin 65(1):5–29. doi:10.3322/caac.21254
Wagner AD, Grothe W, Haerting J, Kleber G, Grothey A, Fleig WE (2006) Chemotherapy in advanced gastric cancer: a systematic review and meta-analysis based on aggregate data. J Clin Oncol 24(18):2903–2909. doi:10.1200/JCO.2005.05.0245
Cunningham D, Starling N, Rao S, Iveson T, Nicolson M, Coxon F, Middleton G, Daniel F, Oates J, Norman AR (2008) Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 358(1):36–46. doi:10.1056/NEJMoa073149
Murad AM, Santiago FF, Petroianu A, Rocha PR, Rodrigues MA, Rausch M (1993) Modified therapy with 5-fluorouracil, doxorubicin, and methotrexate in advanced gastric cancer. Cancer 72(1):37–41
Ter Veer E, Haj Mohammad N, van Valkenhoef G, Ngai LL, Mali RM, Anderegg MC, van Oijen MG, van Laarhoven HW (2016) The efficacy and safety of first-line chemotherapy in advanced esophagogastric cancer: a network meta-analysis. J Natl Cancer Inst. doi:10.1093/jnci/djw166
Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, Miyashita K, Nishizaki T, Kobayashi O, Takiyama W, Toh Y, Nagaie T, Takagi S, Yamamura Y, Yanaoka K, Orita H, Takeuchi M (2008) S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol 9(3):215–221. doi:10.1016/S1470-2045(08)70035-4
Yamada Y, Higuchi K, Nishikawa K, Gotoh M, Fuse N, Sugimoto N, Nishina T, Amagai K, Chin K, Niwa Y, Tsuji A, Imamura H, Tsuda M, Yasui H, Fujii H, Yamaguchi K, Yasui H, Hironaka S, Shimada K, Miwa H, Hamada C, Hyodo I (2015) Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naive patients with advanced gastric cancer. Ann Oncol 26(1):141–148. doi:10.1093/annonc/mdu472
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T, Aprile G, Kulikov E, Hill J, Lehle M, Ruschoff J, Kang YK, To GATI (2010) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376(9742):687–697. doi:10.1016/S0140-6736(10)61121-X
Fuchs CS, Tomasek J, Yong CJ, Dumitru F, Passalacqua R, Goswami C, Safran H, dos Santos LV, Aprile G, Ferry DR, Melichar B, Tehfe M, Topuzov E, Zalcberg JR, Chau I, Campbell W, Sivanandan C, Pikiel J, Koshiji M, Hsu Y, Liepa AM, Gao L, Schwartz JD, Tabernero J, Investigators RT (2014) Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet 383(9911):31–39. doi:10.1016/S0140-6736(13)61719-5
Wilke H, Muro K, Van Cutsem E, Oh SC, Bodoky G, Shimada Y, Hironaka S, Sugimoto N, Lipatov O, Kim TY, Cunningham D, Rougier P, Komatsu Y, Ajani J, Emig M, Carlesi R, Ferry D, Chandrawansa K, Schwartz JD, Ohtsu A, Group RS (2014) Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol 15(11):1224–1235. doi:10.1016/S1470-2045(14)70420-6
Funaki H, Fujita J, Morioka E, Kaida D, Ohnishi T, Ohno Y, Tomita Y, Noguchi M, Fujita H, Kinami S, Nakano Y, Ueda N, Kosaka T (2013) Evaluation of conversion gastrectomy for treatment of Stage IV advanced gastric cancer. Gan To Kagaku Ryoho 40(12):1615–1617
Fukuchi M, Ishiguro T, Ogata K, Suzuki O, Kumagai Y, Ishibashi K, Ishida H, Kuwano H, Mochiki E (2015) Prognostic role of conversion surgery for unresectable gastric cancer. Ann Surg Oncol 22(11):3618–3624. doi:10.1245/s10434-015-4422-6
Yoshida K, Yamaguchi K, Okumura N, Tanahashi T, Kodera Y (2016) Is conversion therapy possible in stage IV gastric cancer: the proposal of new biological categories of classification. Gastric Cancer 19(2):329–338. doi:10.1007/s10120-015-0575-z
Sato Y, Ohnuma H, Nobuoka T, Hirakawa M, Sagawa T, Fujikawa K, Takahashi Y, Shinya M, Katsuki S, Takahashi M, Maeda M, Okagawa Y, Naoki U, Kikuch S, Okamoto K, Miyamoto H, Shimada M, Ichiro T, Kato J, Takayama T (2016) Conversion therapy for inoperable advanced gastric cancer patients by docetaxel, cisplatin, and S-1 (DCS) chemotherapy: a multi-institutional retrospective study. Gastric Cancer. doi:10.1007/s10120-016-0633-1
Kanda T, Yajima K, Kosugi S, Ishikawa T, Ajioka Y, Hatakeyama K (2012) Gastrectomy as a secondary surgery for stage IV gastric cancer patients who underwent S-1-based chemotherapy: a multi-institute retrospective study. Gastric Cancer 15(3):235–244. doi:10.1007/s10120-011-0100-y
Takayama T, Sato Y, Sagawa T, Okamoto T, Nagashima H, Takahashi Y, Ohnuma H, Kuroiwa G, Miyanishi K, Takimoto R, Matsunaga T, Kato J, Yamaguchi K, Hirata K, Niitsu Y (2007) Phase I study of S-1, docetaxel and cisplatin combination chemotherapy in patients with unresectable metastatic gastric cancer. Br J Cancer 97(7):851–856. doi:10.1038/sj.bjc.6603957
Sato Y, Takayama T, Sagawa T, Takahashi Y, Ohnuma H, Okubo S, Shintani N, Tanaka S, Kida M, Sato Y, Ohta H, Miyanishi K, Sato T, Takimoto R, Kobune M, Yamaguchi K, Hirata K, Niitsu Y, Kato J (2010) Phase II study of S-1, docetaxel and cisplatin combination chemotherapy in patients with unresectable metastatic gastric cancer. Cancer Chemother Pharmacol 66(4):721–728. doi:10.1007/s00280-009-1215-2
Hirakawa M, Sato Y, Ohnuma H, Takayama T, Sagawa T, Nobuoka T, Harada K, Miyamoto H, Sato Y, Takahashi Y, Katsuki S, Hirayama M, Takahashi M, Ono M, Maeda M, Takada K, Hayashi T, Sato T, Miyanishi K, Takimoto R, Kobune M, Hirata K, Kato J (2013) A phase II study of neoadjuvant combination chemotherapy with docetaxel, cisplatin, and S-1 for locally advanced resectable gastric cancer: nucleotide excision repair (NER) as potential chemoresistance marker. Cancer Chemother Pharmacol 71(3):789–797. doi:10.1007/s00280-013-2073-5
Basch E, Prestrud AA, Hesketh PJ, Kris MG, Feyer PC, Somerfield MR, Chesney M, Clark-Snow RA, Flaherty AM, Freundlich B, Morrow G, Rao KV, Schwartz RN, Lyman GH, American Society of Clinical O (2011) Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 29(31):4189–4198. doi:10.1200/JCO.2010.34.4614
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247. doi:10.1016/j.ejca.2008.10.026
Japanese Gastric Cancer A (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14(2):101–112. doi:10.1007/s10120-011-0041-5
Wang J, Xu R, Li J, Bai Y, Liu T, Jiao S, Dai G, Xu J, Liu Y, Fan N, Shu Y, Ba Y, Ma D, Qin S, Zheng L, Chen W, Shen L (2015) Randomized multicenter phase III study of a modified docetaxel and cisplatin plus fluorouracil regimen compared with cisplatin and fluorouracil as first-line therapy for advanced or locally recurrent gastric cancer. Gastric Cancer. doi:10.1007/s10120-015-0457-4
Okabe H, Ueda S, Obama K, Hosogi H, Sakai Y (2009) Induction chemotherapy with S-1 plus cisplatin followed by surgery for treatment of gastric cancer with peritoneal dissemination. Ann Surg Oncol 16(12):3227–3236. doi:10.1245/s10434-009-0706-z
Han DS, Suh YS, Kong SH, Lee HJ, Im SA, Bang YJ, Kim WH, Yang HK (2013) Outcomes of surgery aiming at curative resection in good responder to induction chemotherapy for gastric cancer with distant metastases. J Surg Oncol 107(5):511–516. doi:10.1002/jso.23284
Suzuki T, Tanabe K, Taomoto J, Yamamoto H, Tokumoto N, Yoshida K, Ohdan H (2010) Preliminary trial of adjuvant surgery for advanced gastric cancer. Oncol Lett 1(4):743–747. doi:10.3892/ol_00000130
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
This study was in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consents were obtained from all patients included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
280_2017_3404_MOESM1_ESM.pptx
Differences in survival between those who underwent conversion therapy (thick curve) and chemotherapy alone (dotted curve) in lymph node metastasis group (a) and peritoneum metastasis group (b) (PPTX 42 kb)
Rights and permissions
About this article
Cite this article
Uemura, N., Kikuchi, S., Sato, Y. et al. A phase II study of modified docetaxel, cisplatin, and S-1 (mDCS) chemotherapy for unresectable advanced gastric cancer. Cancer Chemother Pharmacol 80, 707–713 (2017). https://doi.org/10.1007/s00280-017-3404-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-017-3404-8