Abstract
Purpose
Aggressive chemotherapy protocols for non-metastatic limb osteosarcoma have improved histological response without affecting prognosis. This study evaluated the toxicity and outcome of a dose-intensive, high-dose 3- to 5-drug pilot protocol, SCOS 89.
Methods
The cohort included 26 patients (14 male; ages 6.5–22 years) with non-metastatic limb osteosarcoma treated at a tertiary pediatric medical center between 1989 and 2013. Preoperatively, patients received two courses of once-weekly pulses of high-dose methotrexate (12–30 g/m2) for 2 weeks; doxorubicin (90 mg/m2) with dexrazoxane, combined with cisplatin (200 mg/m2), was added in week 3. Following methotrexate, 760 mg/m2 of folinic acid was administered. Postoperative chemotherapy was continued to a total of 14 courses of methotrexate, doxorubicin (up to a total dose of 360 mg/m2), and cisplatin (up to a total dose of 560 mg/m2). If toxicity occurred or <90 % tumor necrosis, ifosfamide (12 g/m2) plus etoposide (500 mg/m2) was substituted for doxorubicin, cisplatin, or methotrexate. Toxicity and death rates were calculated.
Results
All patients underwent definitive limb salvage surgery. Six patients died of infection, recurrent disease, or secondary malignancy. Median follow-up was 100 months (range 2–290). Event-free and overall survival rates, respectively, were 88 and 96 % at 2 years, 80 and 87.6 % at 5 years, 80 and 78 % at 10 years. Eleven patients required ifosfamide/etoposide substitution. One patient had a transient decreased left ventricular ejection fraction. Two patients developed acute nephrotoxicity during therapy, but no neurotoxicity. Seven patients had hearing impairment.
Conclusions
The SCOS 89 yields a high event-free survival rate with reduced nephro-/neuro-/cardiotoxicity in patients with non-metastatic limb osteosarcoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma, the most common primary malignant bone tumor, occurs mostly in the 15- to 19-year age group in which it accounts for >10 % of all solid cancers (0.8/100,000–1.1/100,000). It frequently originates in the metaphyseal region of the long bones of the extremities. Most of the patients have localized disease [1].
Prior to the introduction of effective chemotherapy, osteosarcoma treated by surgical resection and/or radiotherapy had a 2-year survival rate of 15–25 % [2]. The first pharmacological agents with proven activity against osteosarcoma were high-dose methotrexate (MTX) and doxorubicin [3, 4] and cisplatin followed, in the late 1970s [5]. The addition of multi-agent chemotherapy to surgery dramatically improved the prognosis of non-metastatic osteosarcoma [6]. At present, MTX, doxorubicin cisplatin, and ifosfamide are considered the most effective drugs [2, 7]. However, the optimal dosage and drug combination remains unclear [6, 8–13]. From 1980 to 2013, no improvement in survival was shown in osteosarcoma studies. Intensive chemotherapy protocols have since improved histological response but not prognosis [14]. However, one study reported better survival in patients with localized extremity osteosarcoma who experienced chemotherapy-induced toxicity [15]. This could suggest that since serum drug levels differ among patients on the same dose regimen, those with higher (toxic) drug levels may be receiving more effective treatment.
The aim of the present study was to evaluate a dose-intensive, high-dose 3- to 5-drug pilot protocol, SCOS 89, designed to improve prognosis while reducing toxicity in patients with non-metastatic limb osteogenic sarcoma.
Patients and methods
Patients and setting
From April 1989 to July 2013, 73 patients with osteogenic sarcoma were diagnosed and treated at the Department of Pediatric Oncology of Schneider Children’s Medical Center of Israel, a tertiary university-affiliated hospital where an average of 14 new cases of primary bone tumors are seen each year. Those who presented with classical high-grade primary sarcoma without metastasis were identified for study inclusion. Forty-seven patients were excluded: metastasis at diagnosis (17 patients), non-limb primary disease (nine patients), lost to follow-up (eight patients), previous malignancy (four patients), treatment with another chemotherapy protocol (four patients), limb and adjacent joint involvement (three patients), gross protocol violation (one patient), and periosteal chondroblastic osteosarcoma (one patient).
The diagnosis was confirmed histologically in all cases, with subtyping based on the predominant cell type.
For this type of study, formal consent is not required by the local research ethics committee.
Pretreatment evaluation
Baseline laboratory studies consisted of complete blood count, serum glucose, electrolytes, serum alkaline phosphatase, lactate dehydrogenase, total bilirubin, aminotransferase, and cardiac function tests (including baseline left ventricular ejection fraction by MUGA scan). All patients underwent audiometry. The primary tumor was evaluated by plain radiograms, computed tomography scans, and/or magnetic resonance imaging scans. Bone scintigraphy and chest computed tomography were used to screen for metastases.
Chemotherapy protocol
The SCOS 89 protocol is shown in Table 1. Two courses of high-dose MTX in weeks 1 and 2 were followed by cisplatin and doxorubicin in week 3. The next course was started 3 weeks later. MTX was started at 12 g/m2, and subsequent doses were increased to a maximum of 20 g/m2 (and 30 g/m2 below the age of 10 years). The rational for this modification has been published by Saeter et al. [16]. In order to achieve a serum level of 2 × 10−5 mol/l at 24 h and 1 × 10−6 mol/l at 48 h. MTX was administered as a 6-h infusion in a hydration solution of 3.2 l/m2 of saline 0.3 % and glucose 5 % with 48 ml of sodium bicarbonate 7.5 % and 5 ml of potassium chloride 15 %/l. The dosage of bicarbonate was adjusted to alkalinize the urine to a pH above 7.0. Blood levels were measured at 24, 48, and 72 h, and the dose was adjusted in subsequent courses to achieve the required levels. Intravenous folinic acid 50 mg/m2 (maximal dose 50 mg) was given 30 h after the start of MTX and then eight times every 3 h. Oral folinic acid 45 mg/m2 (maximum dose 45 mg) was given 60 h after the start of MTX and then eight times every 6 h (total folinic acid dose 760 mg/m2, maximum dose 760 mg). Cisplatin (week 3) was given at a dose of 40 mg/m2/day × 5 days in 100–250 ml of 3 % sodium chloride for 21 h for 3 days and 24 h for the next 2 days. Doxorubicin, at a dose of 30 mg/m2/day × 3 days, was administered intravenously over 3 h concomitantly with dexrazoxane 300 mg/m2 on the first 3 days of the cisplatin treatment. Limb salvage surgery was scheduled 3 weeks after the two courses of MTX + cisplatin + doxorubicin therapy.
After definitive tumor resection, specimens were evaluated by an institutional pathologist. Necrosis was graded according by Huvos’s method, as modified by the Children’s Cancer Group [10]. Postoperatively, patients continued the 2-weekly treatments with MTX, followed by cisplatin (160 mg/m2) in the first course and doxorubicin in the first two courses. The total dose of doxorubicin was 360 mg/m2 (in the absence of cardiotoxicity); the total dose of cisplatin was 560 mg/m2 (in the absence of ototoxicity), with 14 doses of MTX. When cardiotoxicity, ototoxicity, or nephrotoxicity prevented continuing therapy, or <90 % tumor necrosis was seen on postoperative evaluation, ifosfamide 12 g/m2 (2.4 g/m2 × 5 days) combined with etoposide 500 mg/m2 (100 mg/m2 × 5 days) was substituted for doxorubicin, cisplatin, or MTX. Audiometry was repeated every two cycles of cisplatin therapy and after therapy completion.
Renal toxicity assessment was based on increased serum creatinine level above normal (age-adjusted) values. Serum creatinine and urea levels were measured on a daily basis when MTX or doxorubicin/cisplatin courses were given, and twice a week between chemotherapy courses. Renal toxicity that caused creatinine level of above 150 % of the baseline value was an indication to discontinue MTX.
MUGA scans were performed before initial therapy with doxorubicin and before every second therapy after completion of therapy. Patients had cardiac monitoring once a year or more frequently if cardiotoxicity was observed.
Data analysis
Descriptive statistics were used to analyze toxicities, necrosis, and death. Univariate analysis was used to determine the association between age, sex, ethnic origin, primary tumor site, histology and disease-free survival. Event-free survival was calculated from the first day of chemotherapy to recurrence (local or distant) or second malignancy, chemotherapy-related death, or last follow-up. Overall survival was calculated from the start of chemotherapy until death or the last follow-up. Survival curves were formulated according to the Kaplan–Meier method and compared using a log-rank test. A P value of <0.05 was considered significant.
Results
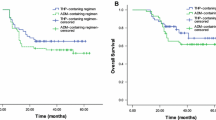
Twenty-six patients aged 6.5–22 years met the inclusion criteria. Their epidemiological, clinical, and pathological characteristics are summarized in Table 2. Univariate analysis showed no association to any of the background parameters evaluated with survival. Limb salvage was performed in all patients. Twelve patients required ifosfamide/etoposide substitution (eight due to poor response per pathology or continuation of severe local pain; two due to MTX toxicity; one for cisplatinum ototoxicity; and one for cardiomyopathy. Fourteen out of the 26 patients received maximum MTX doses higher than 12–12.5 g/m2. Four received 15 g/m2, two received 17.5 g/m2, five received 20 g/m2, 1 aged 7 years received 25 g/m2 and another aged 9 years received 27.5 g/m2. Six deaths were recorded: One patient treated during the learning period of this protocol had fever prior to the start of chemotherapy (2 months after diagnosis) and died of sepsis; three patients died of recurrent metastatic disease 3, 4, and 5 years after diagnosis; one patient developed treatment-related acute myelogenous leukemia and subsequently received stem cell transplantation, but died of persistent leukemia, 4.5 years after completion therapy for osteosarcoma; and one patient died of breast cancer 12.5 years after diagnosis. The median duration of follow-up was 100 months (range 2–290 months). On completion of the study, 20 patients (76.9 %) were alive in continuous complete remission. On Kaplan–Meier analysis, 2-year event-free survival was 88 %, and 2-year overall survival was 96 %; corresponding rates at 5 years were 79.8 and 87.6 %, and at 10 years were 79.8 and 77.8 % (Fig. 1).
Necrosis after induction chemotherapy
Five patients had <90 % necrosis, of whom four ultimately died: two patients with recurrent disease, one patient with secondary leukemia, and one patient with disseminated breast cancer. Both patients with secondary malignancies received ifosfamide etoposide because of poor chemotherapy response. The fifth patient, with chondroblastic osteosarcoma, is currently disease free, 8 years after diagnosis, despite only 25 % necrosis. Nineteen of the 21 patients who had more than 90 % necrosis on definitive surgery continue to be long-term disease-free survivors.
Toxicity
Acute MTX-induced nephrotoxicity was documented in two patients. The first was a 9-year-old boy in whom nephrotoxicity developed after four cycles of methotrexate 12 g/m2; maximum serum creatinine level was 3.5 mg% (upper normal limit in our laboratory, 1.1 mg%), and maximum serum methotrexate level (at 24 h) was 1.4 × 10−4 mol/l. The second patient was an 11-year-old girl in whom nephrotoxicity developed after two cycles of MTX 19.4 g/m2; maximum serum creatinine level was 3.5 mg%, and maximum serum MTX level (at 24 h) was 1.5 × 10−4 mol/l. Treatment in both cases consisted of hyperhydration and repeated doses of leucovorin. The girl was also treated with oral charcoal and intravenous thymidine. Thereafter, MTX levels decreased and blood creatinine level normalized. The next chemotherapy treatments (doxorubicin) were postponed for 9 and 13 days. The same dose of MTX was continued without event in both cases suggesting that inadvertent protocol violation had been the cause of the renal insufficiency.
A confusional state post-MTX therapy was recorded in one patient and resolved within one day. No other MTX-induced toxicity such as mucositis was recorded.
Eleven patients required ifosfamide/etoposide substitution. Ifosfamide (±etoposide) was substituted because of hearing impairment of >4 Hz caused by cisplatin in one patient; poor pathology response of <90 % tumor necrosis at tumor resection in four patients; suspected transient MTX neurotoxicity in one patient who did not occur with subsequent MTX treatments; MTX nephrotoxicity in two patients; poor clinical improvement (continuation of severe local pain) in two patients; and transient cardiotoxicity per MUGA in one patient.
This patient had a single episode of transient reduction of left ventricular ejection fraction, and doxorubicin was replaced with ifosfamide until recovery. Grade 3 hearing loss (>20 dB at ≤2000 Hz) was found in five patients, and grade 4 hearing loss (>40 dB at 200 Hz), in one patient. Azoospermia and impaired sperm function in the presence of a normal sperm count were found in two male patients. No female patient had fertility problems. Eight of the 20 survivors (three female, five male) married and have, collectively, 18 children to date. The remainder were <18 years old or unmarried.
Discussion
This study shows that the dose-intensive multi-agent SCOS 89 protocol improves prognosis of patients with non-metastatic limb osteosarcoma and reduces the toxicity associated with other protocols.
Development of the protocol to increase chemotherapy effectiveness was based on the concept that the administration of multiple non-cross-resistant drugs early in therapy prevents drug resistance [17]. Several classical studies in other malignancies have shown that survival is related to dose intensity [18, 19]; however, reducing the doses of each of the drugs may worsen prognosis and must be avoided [20]. Apparently, both the total dose and the dose intensity have a separate effect on cure [21]. In osteosarcoma, in particular, the cure rate has been correlated with the total doxorubicin dose [22]. Pre-operative chemotherapy was especially intensive since we were concerned that similar to breast cancer patients, tumor cells may disseminate into the blood stream during surgery [23], leading to metastatic spread.
Accordingly, following the successful use of an element of concomitant 200 mg/m2 cisplatin and 90 mg/m2 doxorubicin in a child in our center with osteosarcoma that progressed on MTX, this element was incorporated into the protocol. Since weekly MTX does not reduce the platelet and leukocyte count, it was given on weeks 1 and 2 followed by cisplatin and doxorubicin in week 3. Surgery was performed after two such cycles. Ifosfamide, when used, was administered as 2-h pulses every 12 h, shown to improve the chemotherapy effect [24] instead of by continuous infusion.
Seventy-seven percent of the 26 patients were alive in continuous complete remission, a mean follow-up was 100 months, the 10-year event-free survival rate is 79.8 %, and the overall survival rate is 77.8 %.
Although high-dose MTX, cisplatin, and doxorubicin are effective in osteosarcoma, they pose a significant risk of toxicity. All may cause neutropenia and mucositis [25]. However, studies have shown that a number of drugs may be given simultaneously without necessarily causing additive toxicity [24]. In the SCOS 89, to prevent renal shutdown due to crystallization of the MTX in the renal tubules [26], all patients received adequate fluids with sufficient bicarbonate. MTX was administered with high folinic acid based on the findings that inadequate doses of folinic acid or a delay of more than 36 h in the start of folinic acid rescue results in systemic toxicity [27, 28], and that neurotoxicity may be prevented by the use of appropriate high-dose folinic rescue without a loss in MTX efficacy [28–30]. Indeed, some of our patients had already participated in an earlier study showing that this protocol is associated with a reduction in 11 of 18 parameters of neuropsychological damage (P < 0.025) [28].
Cisplatin is known to be associated with nephrotoxicity, especially glomerular damage [31]. To reduce this risk, we administered cisplatin together with hypertonic saline [32], rather than mannitol, as suggested by Ozols et al. [33].
A high total dose of cisplatin has been found to cause hearing loss. In one study, 15.7 % of patients given a platinum dose of >490 mg/m2 cisplatin had deafness [34]. In the present study, the dose of cisplatin was limited to 560 mg/m2, and it was administered as a continuous infusion, shown to reduce the risk of neurotoxicity [35]. We found that only six patients (23.1 %) had hearing loss at 4000–8000 Hz, and none required a hearing aid.
The effect of cisplatin on male fertility has been studied mostly in patients with testicular cancer [36]. However, men with testicular cancer have a potential predisposition to infertility. In one study of 32 cisplatin-treated patients with osteosarcoma, nearly all were rendered azoospermic during treatment, although sperm production resumed in 30 patients 2 years later. The rate of normal sperm production was lower in the patients receiving cisplatin dosages of 600 mg/m2 or more [37]. The present protocol, using continuous infusion of cisplatin, was associated with azoospermia in one patient and poor sperm function in one patient. As in other studies of female survivors of osteogenic sarcoma [38], none of our female patients had fertility problems.
Anthracyclines exert cardiotoxic and anticancer effects through different mechanisms. Although increased doses of doxorubicin have been found to be associated with a higher cure rate in osteosarcoma, Silber and Kaizer [22] showed that in patients treated with higher doses, the increase in mortality due to cardiac failure eventually supersedes the increase in cure rate. Cardioprotection is imperative because the dose reduction of doxorubicin needed to prevent the 5 % of deaths due to cardiotoxicity will result in 20 % more patients dying from their primary disease [22]. In the present study, doxorubicin cardiotoxicity was prevented by limiting the total dose to 360 mg/m2 and administering concomitant dexrazoxane, an FDA-approved cardioprotective agent [39]. In children, clinical evidence of the cardioprotective action of dexrazoxane is limited. The available data support both short- and long-term effects in patients with acute leukemia. Although concerns were raised following a study in children with Hodgkin lymphoma [40] that dexrazoxane may pose a risk of secondary malignant neoplasms [41], others found that of 553 dexrazoxane-treated patients with acute lymphoblastic leukemia, only one (with a mixed-lineage leukemia gene rearrangement) developed acute myelogenous leukemia [42].
Several other chemotherapy protocols for non-metastatic limb osteosarcoma are presented in Table 3 [6, 8, 11–13, 43–45], and their outcomes are compared to the present study in Table 4. The only other study with results comparable to ours was reported by Kudawara et al. [45]. Their cohort consisted of 40 patients treated with doxorubicin, cisplatin, and ifosfamide before surgery and doxorubicin, cisplatin, ifosfamide, and MTX as adjuvant therapy. Their patients received less MTX and cisplatin than our patients, with the same dose of doxorubicin and a much higher dose of ifosfamide (without etoposide). Owing to short-term toxicity, only 2.5 % of the patients received the planned ifosfamide dose, and <20 % received the planned doxorubicin dose. There were no treatment-related deaths, cardiotoxicity events, or second cancers [45]. Although the 10-year event-free survival of 80 % was similar to the present study, the toxicity pattern differed. Our MTX-based protocol prevented long-term nephrotoxicity despite larger doses of cisplatin, and ifosfamide was used only as second-line therapy (with etoposide), owing to its known nephrotoxicity, especially when given with cisplatin. At the time of this study, etoposide was thought to be an active drug in osteosarcoma; subsequently, the EURAMOS-1 study and other studies have shown that adding ifosfamide and etoposide to MAP as postoperative chemotherapy in patients with a poor response to preoperative chemotherapy for newly diagnosed osteosarcoma is associated with additional morbidity and has no effect on survival outcomes [46, 47].
In conclusion, the SCOS 89 pilot study in patients with non-metastatic limb osteosarcoma leads to a high event-free survival rate with reduced toxicity relative to existing protocols.
References
ESMO/European Sarcoma Network Working Group (2012) Bone sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 23:vii100–vii109
Marina N, Gebhardt M, Teot L, Gorlick R (2004) Biology and therapeutic advances for pediatric osteosarcoma. Oncologist 9:422–441
Cortes EP, Holland JF, Wang JJ, Sinks LF (1972) Doxorubicin in disseminated osteosarcoma. JAMA 221:1132–1138
Jaffe N, Frei E 3rd, Traggis D, Bishop Y (1974) Adjuvant methotrexate and citrovorum-factor treatment of osteogenic sarcoma. N Engl J Med 291:994–997
Baum ES, Gaynon P, Greenberg L, Krivit W, Hammond D (1979) Phase II study of cis-dichlorodiammineplatinum(II) in childhood osteosarcoma: Children’s Cancer Study Group Report. Cancer Treat Rep 63:1621–1627
Ferrari S, Smeland S, Mercuri M, Italian and Scandinavian Sarcoma Groups et al (2005) Neoadjuvant chemotherapy with high-dose ifosfamide, high-dose methotrexate, cisplatin, and doxorubicin for patients with localized osteosarcoma of the extremity: a joint study by the Italian and Scandinavian Sarcoma Groups. J Clin Oncol 23:8845–8852
Bielack SS, Kempf-Bielack B, Delling G et al (2002) Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol 20:776–790
Bramwell VH, Burgers M, Sneath R et al (1992) A comparison of two short intensive adjuvant chemotherapy regimens in operable osteosarcoma of limbs in children and young adults: the first study of the European Osteosarcoma Intergroup. J Clin Oncol 10:1579–1591
Souhami RL, Craft AW, Van der Eijken JW et al (1997) Randomised trial of two regimens of chemotherapy in operable osteosarcoma: a study of the European Osteosarcoma Intergroup. Lancet 350:911–917
Provisor AJ, Ettinger LJ, Nachman JB et al (1997) Treatment of nonmetastatic osteosarcoma of the extremity with preoperative and postoperative chemotherapy: a report from the Children’s Cancer Group. J Clin Oncol 15:76–84
Fuchs N, Bielack SS, Epler D et al (1998) Long-term results of the co-operative German–Austrian–Swiss osteosarcoma study group’s protocol COSS-86 of intensive multidrug chemotherapy and surgery for osteosarcoma of the limbs. Ann Oncol 9:893–899
Ferrari S, Mercuri M, Picci P et al (1999) Nonmetastatic osteosarcoma of the extremity: results of a neoadjuvant chemotherapy protocol (IOR/OS-3) with high-dose methotrexate, intraarterial or intravenous cisplatin, doxorubicin, and salvage chemotherapy based on histologic tumor response. Tumori 85:458–464
Bacci G, Ferrari S, Bertoni F et al (2000) Long-term outcome for patients with nonmetastatic osteosarcoma of the extremity treated at the istituto ortopedico rizzoli according to the istituto ortopedico rizzoli/osteosarcoma-2 protocol: an updated report. J Clin Oncol 18:4016–4027
Lewis IJ, Nooij MA, Whelan J, MRC BO06 and EORTC 80931 collaborators, European Osteosarcoma Intergroup et al (2007) Improvement in histologic response but not survival in osteosarcoma patients treated with intensified chemotherapy: a randomized phase III trial of the European Osteosarcoma Intergroup. J Natl Cancer Inst 99:112–128
McTiernan A, Jinks RC, Sydes MR et al (2012) Presence of chemotherapy-induced toxicity predicts improved survival in patients with localized extremity osteosarcoma treated with doxorubicin and cisplatinum: a report from the European osteosarcoma study group. Eur J Cancer 48:703–712
Saeter G, Alvegård TA, Elomaa I, Stenwig AE et al (1991) Treatment of osteosarcoma of the extremities with the T-10 protocol, with emphasis on the effects of preoperative chemotherapy with single-agent high-dose methotrexate: a Scandinavian Sarcoma Group study. J Clin Oncol 9(10):1766–1775
Goldie JH, Coldman AJ (1979) A mathematic model for relating the drug sensitivity of tumors to their spontaneous mutation rate. Cancer Treat Rep 63:1727–1733
Bonadonna G, Valagussa P (1981) Dose response effect of adjuvant chemotherapy in breast-cancer. New Engl J Med 304:10–15
De Vita VT (1986) Dose-response is alive and well. J Clin Oncol 4:1157–1159
Winkler K, Beron G, Delling G et al (1988) Neoadjuvant chemotherapy of osteosarcoma: results of a randomized cooperative trial (COSS-82) with salvage chemotherapy based on histological tumor response. J Clin Oncol 6:329–337
Coldman AJ, Goldie JH (1987) Impact of dose-intense chemotherapy on the development of permanent drug resistance. Semin Oncol 14:29–33
Silber JH, Kaizer H (1988) Marginal analysis applied to the dose-response curve. Med Pediatr Oncol 16:344–348
Brown DC, Purushotham AD, Birnie GD, George WD (1995) Detection of intraoperative tumor cell dissemination in patients with breast cancer by use of reverse transcription and polymerase chain reaction. Surgery 1:96–101
Benjamin RS (1997) Freidreich’s laws in the treatment of sarcomas. Clin Cancer Res 3:2648–2654
Price LA, Hill BT (1981) Safe and effective combination chemotherapy without cis-platinum for squamous cell carcinomas of the head and neck. Cancer Treat Rep 65(Suppl 1):149S–154S
Cohen IJ (2009) High dose methotrexate is effective in osteosarcoma so what is the problem? J Pediatr Hematol Oncol 31:892–893
Cohen IJ, Wolff JE (2014) How long can folinic acid rescue be delayed after high-dose methotrexate without toxicity? Pediatr Blood Cancer 61:7–10
Bonda-Shkedi E, Arush MW, Kaplinsky C et al (2013) The correlation between dose of folinic acid and neurotoxicity in children and adolescents treated for osteosarcoma with high-dose methotrexate (HDMTX): a neuropsychological and psychosocial study. J Pediatr Hematol Oncol 35:271–275
Cohen IJ (2013) Challenging the clinical relevance of folinic acid over rescue after high dose methotrexate (HDMTX). Med Hypotheses 81:942–947
Cohen IJ (2004) Defining the appropriate dosage of folinic acid after high-dose methotrexate for childhood acute lymphatic leukemia that will prevent neurotoxicity without rescuing malignant cells in the central nervous system. J Pediatr Hematol Oncol 26:156–163
Janeway KA, Grier HE (2010) Sequelae of osteosarcoma medical therapy: a review of rare acute toxicities and late effects. Lancet Oncol 11:670–678
Ozols RF, Corden BJ, Jacob J, Wesley MN, Ostchega Y, Young RC (1984) High-dose cisplatin in hypertonic saline. Ann Intern Med 100:19–24
Ozols DF, Deisseroth AB, Javadpour N, Barlock A, Messerschmidt GL, Young RC (1983) Treatment of poor prognosis nonseminomatous testicular cancer with a “high-dose” platinum combination chemotherapy regimen. Cancer 51:1803–1807
Nagarajan R, Kamruzzaman A, Ness KK et al (2011) Twenty years of follow-up of survivors of childhood osteosarcoma: a report from the Childhood Cancer Survivor Study. Cancer 117:625–634
Gupta AA, Capra M, Papaioannou V et al (2006) Low incidence of ototoxicity with continuous infusion of cisplatin in the treatment of pediatric germ cell tumors. J Pediatr Hematol Oncol 28:91–94
Petersen PM, Hansen SW, Giwercman A, Rørth M, Skakkebaek NE (1994) Dose-dependent impairment of testicular function in patients treated with cisplatin-based chemotherapy for germ cell cancer. Ann Oncol 5:355–358
Meistrich ML, Chawla SP, Da Cunha MF et al (1989) Recovery of sperm production after chemotherapy for osteosarcoma. Cancer 63:2115–2123
Ash BS, Cohen I, Goshen Y et al (2009) Fertility in female survivors of nonmetastatic osteosarcoma. ESMO (Abstract). J Bone Joint Surg Br Proceedings 10.1302. http://www.bjj.boneandjoint.org.uk/. Accessed 1 Dec 2014
Walker DM, Fisher BT, Seif AE et al (2013) Dexrazoxane use in pediatric patients with acute lymphoblastic or myeloid leukemia from 1999 and 2009: analysis of a national cohort of patients in the Pediatric Health Information Systems database. Pediatr Blood Cancer 60:616–620
Vrooman LM, Neuberg DS, Stevenson KE et al (2011) The low incidence of secondary acute myelogenous leukaemia in children and adolescents treated with dexrazoxane for acute lymphoblastic leukaemia: a report from the Dana-Farber Cancer Institute ALL Consortium. Eur J Cancer 47:1373–1379
Tebbi CK, London WB, Friedman D et al (2007) Dexrazoxane-associated risk for acute myeloid leukemia/myelodysplastic syndrome and other secondary malignancies in pediatric Hodgkin’s disease. J Clin Oncol 25:493–500
Crews KR, Liu T, Rodriguez-Galindo C et al (2004) High-dose methotrexate pharmacokinetics and outcome of children and young adults with osteosarcoma. Cancer 100:1724–1733
Meyers PA, Schwartz CL, Krailo M et al (2005) Osteosarcoma: a randomized, prospective trial of the addition of ifosfamide and/or muramyl tripeptide to cisplatin, doxorubicin, and high-dose methotrexate. J Clin Oncol 23:2004–2011
Ferrari S, Ruggieri P, Cefalo G et al (2012) Neoadjuvant chemotherapy with methotrexate, cisplatin, and doxorubicin with or without ifosfamide in nonmetastatic osteosarcoma of the extremity: an Italian sarcoma group trial ISG/OS-1. J Clin Oncol 30:2112–2118
Kudawara I, Aoki Y, Ueda T et al (2013) Neoadjuvant and adjuvant chemotherapy with high-dose ifosfamide, doxorubicin, cisplatin and high-dose methotrexate in non-metastatic osteosarcoma of the extremities: a phase II trial in Japan. J Chemother 25:41–48
Marina N, Smeland S, Bielack SS, Bernstein M, Jovic G, Hook JM, Krailo MD (2014) MAPIE vs MAP as postoperative chemotherapy in patients with a poor response to preoperative chemotherapy for newly diagnosed osteosarcoma: results from EURAMOS-1 (Paper 032). Presented at: 19th annual Connective Tissue Oncology Meeting, October 15–18, 2014, Berlin, Germany
Allison DC, Carney SC, Ahlmann ER et al (2012) A meta-analysis of osteosarcoma outcomes in modern medical era. Sarcoma 2012:10. doi:10.1155/2012/704872
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional local ethics committee and the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Shkalim-Zemer, V., Ash, S., Toledano, H. et al. Highly effective reduced toxicity dose-intensive pilot protocol for non-metastatic limb osteogenic sarcoma (SCOS 89). Cancer Chemother Pharmacol 76, 909–916 (2015). https://doi.org/10.1007/s00280-015-2865-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2865-x